Abstract
Introduction:
Management of emergencies is an integral part of primary care. Being first contact care providers general practitioners may encounter any type of emergency. Acute attacks of asthma, myocardial infarction, anaphylactic shock, hypoglycemic coma, convulsions, head injuries and trauma are some of the common emergencies encountered by GPs. Updated knowledge, communication and procedural skills, trained paramedical staff, necessary equipment and medications and appropriate practice organization are vital to provide optimum care which may even save lives of patients. The wide range of problems and the rarity of the problems make it difficult for primary care doctors to be updated and competent in providing emergency care.
Role of GP:
Some of the emergencies can be managed completely at a general practice while others should be referred to hospital after initial management. The extent to which a patient should be managed may be determined by the degree of severity of the condition, expertise of the doctor and distance to the nearest hospital. Apart from pharmacological management, explanation about the condition and the need for admission and appropriate advice on care prior to admission are also vital components of management. Writing an appropriate referral, arranging transport facilities, informing the hospital about the referral are also important steps in the process as these measures could prevent crucial delays.
Conclusion:
Emergency care is a responsibility of primary care doctors and they should be knowledgeable and skilled and organize their practices to provide prompt and effective management whenever the need arises.
Keywords: Emergency care, primary care, general practice
Introduction
A medical emergency is an injury or illness that is acute and poses an immediate risk to a person's life or long-term health and it's extremely important to attend to these patients immediately. The early identification of a medical emergency and subsequent management will be helpful to save the patient's life[1] and prevent irreversible consequences. Acute attacks of asthma, myocardial infarction, anaphylactic shock, hypoglycemic coma, convulsions, head injuries and trauma are some of the common emergencies[1,2,3] encountered by general practitioners (GPs)/primary care doctors. The airway, breathing, circulation, disability, exposure approach which is widely accepted by experts in emergency medicine is applicable in primary care settings as well for immediate assessment and treatment of critically ill patients.[4]
It's a Responsibility of GPs
Provision of emergency care is an integral part of general practice[1,2,3,5] and GPs play a crucial role in the management of medical emergencies. Being first contact care providers, primary care physicians could come across any type of emergency at any time. Availability and accessibility at the community level make them the ideal first contact point for emergency care. The provision of timely, effective, proper and compassionate care require knowledge, proper training, confidence, experience, trained supportive staff, equipment and medications.[4,6,7]
Competencies Required
Knowledge and skills
The top most requirement for emergency management is the updated knowledge of the doctor that aids in the early diagnosis and management. It is a challenge for a primary care doctor to be updated and competent in every emergency that he may come across. One reason is the wide spectrum of problems and the other reason is the rarity of some of the emergencies encountered.[2] It has been revealed that GPs are less comfortable in managing emergencies which they encounter less frequently.[3] They should be able to suspect or diagnose that a patient is having a serious problem and be able to carry out at least initial pre-hospital management. GPs should also know the indications to admit patients having conditions which can be managed in an outpatient set up such as acute attack of asthma and febrile convulsion. They should be competent in therapeutic and diagnostic procedures[2] such as nebulization and electrocardiography (ECG). Exposure into emergency care through training programs, continuous medical education sessions and case discussions with peers could help them to enhance their knowledge, competence and confidence.[3] Accessibility to guidelines[8] and protocols are vital to update the knowledge of GPs[7,9] and algorithms for the management of different medical emergencies can be displayed in the emergency management room for quick reference.
Communication skills
GPs should be skilled to gather accurate and essential information from all sources including history, physical examination, family members, witnesses to the incident, medical records etc.[10] They need to have excellent interpersonal skills and communication skills that result in information exchange as well as teaming with patients, family members and paramedical staff.[10] It's extremely important to be calm in these situations and lead the staff to carry out what is expected. While practicing emergency care GPs should demonstrate caring attitude, respect, compassion, integrity and also should be sensitive and responsive to the needs of patient and family as well. They should understand that these are situations where patients and family are extremely worried and concerned. GPs should try to avoid even a slight delay since that may not be tolerated by carers and could even lead to hostile reactions. Prompt attention, explanation and reassurance would help to alleviate their fears and concerns and gain confidence of patient and carers.
Trained paramedical staff
The presence of trained paramedical staff is also essential to attend to emergencies promptly. The staff at the reception should be educated about the medical emergencies and they should be advised to give priority to patients who present with medical emergencies. The staff should also be trained to detect patients needing prompt attention such as wheezing, unsteadiness and pain as they enter the premises. Some patients are unaware that they are having a life-threatening condition despite having these symptoms and some patients are reluctant to break the queue and trouble the staff and the doctor. Paramedical staff in the practice should be competent in basic procedures such as obtaining intravenous access, stabilizing and maintaining the airway, breathing and circulation and nebulization. They need proper training, regular update of knowledge, encouragement and admiration.
Practice organization
The location and the layout of the medical center play a major role in providing emergency care. It should ideally be situated in the center of the community, with an easy access to it by any mode of transport; therefore, care should be taken when a location is being selected for a general practice. It should be spacious and have electricity, water, telephone and toilet facilities and ample parking space. It should have broad entrance and wheel chair access so a patient could be carried or wheeled in if the need arises. There should be an emergency care room close to the entrance and it should be accessible from the consultation room of the doctor [Figure 1]. This kind of arrangement will help the doctor to attend to the patient immediately and review the patient while attending to other patients.
Figure 1.
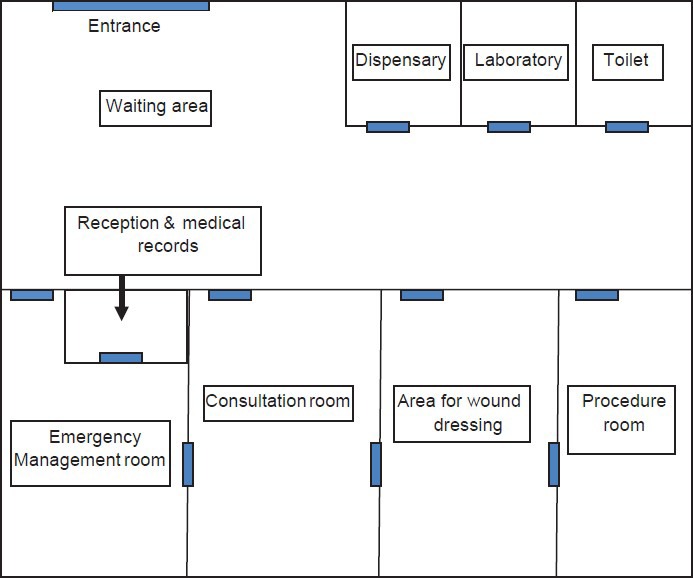
Appropriate practice layout to provide emergency care
Medications and equipment
Emergency treatment room should be equipped with equipments [Box 1] and a suitable range of medications[11,12,13] [Box 2] which reflect the anticipated emergencies in the patient populations, the practitioners’ skills and the distance to the nearest emergency department.[9]
Box 1.
Necessary equipment

Box 2.
Essential medications
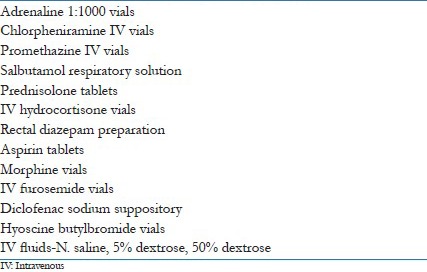
Medications, intravenous fluids and equipment which are essential for emergency management should be stored in a separate place and labeled properly for easy access. The availability of stocks and expiry dates of the medications and intravenous fluids should be checked regularly by an appointed person.[6] At the same time, the sterility of the equipments used during emergencies should also be maintained.
GP's Role
Even though conditions such as acute attacks of asthma, febrile convulsions and hypoglycemia could be managed entirely in a general practice, most of the emergencies such as acute myocardial infarction, ectopic pregnancy and torsion of the testis need to be transferred following initial management. The extent to which the emergency should be managed may depend on the condition of the patient, expertise of the doctor and distance to the nearest emergency department and a GP in a rural setting may need to do more than just stabilize a critically ill patient.[8]
The primary care medical center can be patient friendly by having contact details of available ambulance services and other vehicles. This would help to minimize the delay in transferring a patient to the hospital. The primary care physicians can co-ordinate care by informing the hospital about the condition of the patient. Then the hospital would be ready to receive the patient and crucial delays could be avoided. It's important to write a referral letter mentioning the essential items of information such as the probable diagnosis (myocardial infarction), present status (blood pressure, pulse rate and rhythm), investigation findings (ECG changes), treatment administered (aspirin), co-morbidities (asthma, diabetes mellitus), treatment for co-morbidities, drug allergies and other relevant information which would be vital for the assessment, diagnosis and the management of the patient.
It is extremely important to make the family and care givers aware why patient is referred and the need for prompt admission to avoid undue delays such as seeking second opinion from another doctor or neglecting the problem such as mild discomfort in the chest due to myocardial infarction by a diabetic patient. Advising patients not to take anything orally in situations such as torsion of the testis, ectopic pregnancy and to minimize physical exertion such as walking in patients having myocardial infarction are also important part of pre-hospital care.
GPs can carry out opportunistic health promotion by displaying posters regarding symptoms of medical emergencies, features of early recognition and first aid measures that should be practiced. Doctors should educate patients who are susceptible to emergencies such as hypoglycemic and hyperglycemic attacks about prevention, early detection of impending attacks and measures to be adopted in such situations.
Attending to emergency medical problems is a responsibility of primary care doctors and they should be armed with knowledge, skills, staff, practice organization, equipment and medications to manage patients effectively which may even be lifesaving.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Johnston CL, Coulthard MG, Schluter PJ, Dick ML. Medical emergencies in general practice in south-east Queensland: Prevalence and practice preparedness. Med J Aust. 2001;175:99–103. doi: 10.5694/j.1326-5377.2001.tb143540.x. [DOI] [PubMed] [Google Scholar]
- 2.Bury G, Prunty H, Egan M, Sharpe B. Experience of prehospital emergency care among general practitioners in Ireland. Emerg Med J. 2008;25:450–4. doi: 10.1136/emj.2007.052910. [DOI] [PubMed] [Google Scholar]
- 3.Dick ML, Schluter P, Johnston C, Coulthard M. GPs’ perceived competence and comfort in managing medical emergencies in southeast Queensland. Aust Fam Physician. 2002;31:870–5. [PubMed] [Google Scholar]
- 4.Wardrope J, Mackenzie R. The ABC of community emergency care: The system of assessment and care of the primary survey positive patient. Emerg Med J. 2004;21:216–25. doi: 10.1136/emj.2003.013524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liddy C, Dreise H, Gaboury I. Frequency of in-office emergencies in primary care. Can Fam Physician. 2009;55:1004–51. [PMC free article] [PubMed] [Google Scholar]
- 6.Brittain C, Eaton CJ, Steggles BG, Holden PJ, Fairhurst RJ. Emergency care in general practice. Should be properly recognised. BMJ. 1995;310:736. doi: 10.1136/bmj.310.6981.736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Avery A, Pringle M. Emergency care in general practice. BMJ. 1995;310:6. doi: 10.1136/bmj.310.6971.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bouma M, Rutten FH, Wiersma T, Burgers JS. Revised Dutch College of General Practitioners’ practice guideline ‘Acute coronary syndrome’. Ned Tijdschr Geneeskd. 2013;157:A6006. [PubMed] [Google Scholar]
- 9.Toback SL. Medical emergency preparedness in office practice. Am Fam Physician. 2007;75:1679–84. [PubMed] [Google Scholar]
- 10.Chapman DM, Hayden S, Sanders AB, Binder LS, Chinnis A, Corrigan K, et al. Integrating the accreditation council for graduate medical education core competencies into the model of the clinical practice of emergency medicine. Acad Emerg Med. 2004;11:674–85. [PubMed] [Google Scholar]
- 11.Drugs for the doctor's bag 1989. Drug Ther Bull. 1989;27:17–9. [PubMed] [Google Scholar]
- 12.Hiramanek N, O'shea C, Lee C, Speechly C, Cavanagh K. What's in the doctor's bag? Aust Fam Physician. 2004;33:714, 716–20. [PubMed] [Google Scholar]
- 13.Murtagh J. The doctor's bag. What do you really need? Aust Fam Physician. 2000;29:25–9. [PubMed] [Google Scholar]


