Abstract
Fractures of distal radius account for up to 20% of all fractures treated in emergency department. Initial assessment includes a history of mechanism of injury, associated injury and appropriate radiological evaluation. Treatment options include conservative management, internal fixation with pins, bridging and non-bridging external fixation, dorsal or volar plating with/without arthroscopy assistance. However, many questions regarding these fractures remain unanswered and good prospective randomized trials are needed.
Keywords: Barton, Colles’ fracture, distal radius fracture, volar, volar barton
Introduction
Distal radius fractures are one of the most common injuries encountered in orthopedic practice. They make up 8%−15% of all bony injuries in adults.[1] Abraham Colles is credited with description of the most common fracture pattern affecting distal end radius in 1814, and is classically named after him.[2] Colles’ fracture specifically is defined as metaphyseal injury of cortico-cancellous junction (within 2−3 cm of articular surface) of the distal radius with characteristic dorsal tilt, dorsal shift, radial tilt, radial shift, supination and impaction. Smith's fractures, also referred to as reverse Colles’ fracture, have palmar tilt of the distal fragment. Barton's fracture is the displaced intra-articular coronal plane fracture-subluxation of dorsal lip of the distal radius with displacement of carpus with the fragment. Reverse Barton's occurs with wrist in palmar-flexion and involves the volar lip. Chauffer's fracture was described as originally occurring due to backfire of the car starter handles in older models. It involves an intra-articular fracture of radial styloid of variable size.
Intra-articular component in distal radius fractures usually signifies high-energy trauma occurring in young adults. High-energy injuries frequently cause shear and impacted fractures of the articular surface of the distal aspect of the radius with displacement of the fracture fragments. The fracture pattern most commonly observed in geriatric age group is extra-articular while the high-energy intra-articular type is most frequent in young adult patients.
Every family care physician see this fracture day in and day out and must have a basic knowledge regarding this fracture so as to provide effective treatment when appropriate.
Mechanism of Fracture
Most of the fractures are caused by a fall on the outstretched hand with the wrist in dorsiflexion. The form and severity of fracture of distal radius as well as the concomitant injury of disco-ligamentary structures of the wrist also depend on the position of the wrist at the moment of hitting the ground. The width of this angle influences the localization of the fracture. Pronation, supination and abduction determine the direction of the force and the compression of carpus and different appearances of ligamentary injuries.[3]
The radius initially fails in tension on the volar aspect, with the fracture progressing dorsally where bending forces induce compressive stresses, resulting in dorsal comminution. Cancellous impaction of the metaphysis further compromises dorsal stability. Additional shearing forces influence the injury pattern, resulting in articular surface involvement.[4]
Anatomy of articular interface of distal radius[5]
The articular surface of the distal aspect of the radius tilts 21 degrees in the antero-posterior plane and 5 to 11 degrees in the lateral plane.[5] The dorsal cortical surface of radius thickens to form the Lister tubercle as well as osseous prominences that support the extensors of the wrist in second dorsal compartment. A central ridge divides the articular surface of the radius into a scaphoid facet and a lunate facet. The triangular fibrocartilage extends from the rim of the sigmoid notch of the radius to the ulnar styloid process. Only the brachioradialis tendon inserts onto the distal aspect of the radius; the other tendons of the wrist pass across the distal aspect of the radius to insert onto the carpal bones or the bases of the metacarpals.
In addition to the extrinsic ligaments of the wrist, the scapholunate interosseous and lunotriquetral interosseous ligaments maintain the scaphoid, lunate and triquetrum in a smooth articular unit that comes into contact with the distal aspect of the radius and the triangular fibrocartilage complex. Because of the different areas of bone thickness and density, the fracture patterns tend to propagate between the scaphoid and lunate facets of the distal aspect of the radius. The degree, direction and extent of the applied load may cause coronal or sagittal splits within the lunate or scaphoid facet.[5,6,7]
Classification of Fracture
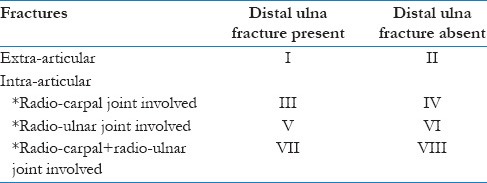
Classifying the distal radius fractures and suggesting best treatment protocols has been a herculean task as evidenced by the number of classification systems put forth and their relative acceptance. Earliest attempts at classification were made during the 1930s, foremost being by Nissen-lie.[8] Gartland and Werley[9] in 1951 and Lidstrom[10] in 1959 developed systems of classification that were based on the presence of, not extent of, displacement at the site of fracture and involvement of radio-carpal joint. Frykman established a system of classification that identified involvement of radio-ulnar and radio-carpal joints along with the presence or absence of the fracture of ulnar styloid process.[11] Although many authors have accepted this classification, this system does not include the extent or direction of initial displacements and comminution [Table 1].
Table 1.
Frykman classification of distal radius fractures
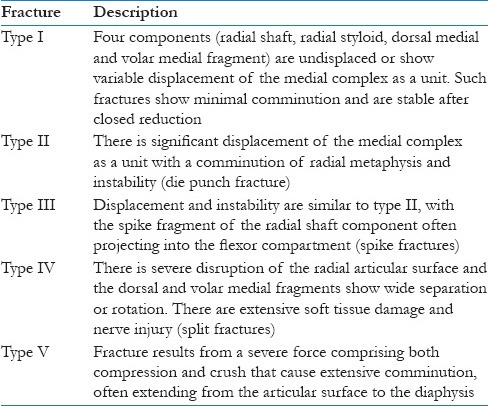
Recent systems of classification have focused on the mechanism of injury. Melone reflected on both the mechanism and degree of injury to distal radius (excluding distal ulna) and the classification for selection of treatment. This system sets the importance of medial portion of articular column of distal aspect of radius for determining prognosis and treatment options [Table 2].[12]
Table 2.
Melone's classification of intra-articular distal radius fractures
The AO classification system, which comprises 27 categories, is the most inclusive. The various categories are organized in an order of increasing severity of osseous and articular lesions making it useful for broad anatomical categorization of large numbers of fractures for trauma registries even though it lacks sufficient focus for use in clinical decision-making.[13]
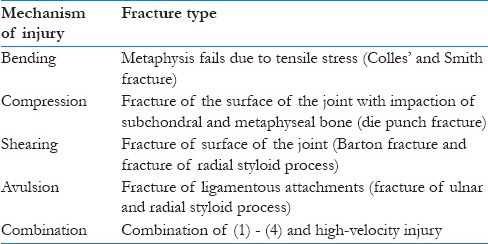
In 1993, Fernandez published a specified classification that separates the fractures of the distal end of the radius according to the mechanism of injury [Table 3].[14]
Table 3.
Fernandez classification of distal end of radius
Radiographic Evaluation
Plain radiographs
Radiographic imaging is important in diagnosis, classification, treatment and follow-up assessment of these fractures. The routine minimal evaluation for distal radius fractures must include two views-a postero-anterior (PA) view and lateral view.[15] The PA view should be obtained with the humerus abducted 90 degrees from the chest wall, so that the elbow is at the same level as the shoulder and flexed 90 degrees.[16] The palm is maintained flat against the cassette. For lateral view, the humerus is adducted against the chest wall and elbow is flexed to 90 degrees. The wrist and hand are maintained in neutral rotation and held perpendicular to film cassette.
It has become apparent through the work of several authors that restoration of articular congruency is potentially of greater importance than other criteria [Figure 1]. It has been reported that the development of post-traumatic osteoarthrosis in 100% of wrists with articular incongruities of 2.0 mm or more.[17] However, other investigators[18,19] found that displacement of even 1.0 mm resulted in pain and stiffness of wrist. In an effort to improve outcome of these injuries, surgical reduction is advocated for articular incongruities greater than 1 to 2 mm after closed reduction. After initial reduction of an intra-articular distal radius fracture in plaster cast, it is important to evaluate the post-reduction X-ray films for assessment of articular incongruity. The assessment of articular incongruity and comminution can be difficult at times, particularly with a plaster cast in place. This occurs in part because of normal volar tilt and radial angulation, which by definition prevent seeing the distal radial articular surface as a plane perpendicular to the film and in part because of the curved shape of distal radio-ulnar joint. The congruity of the distal radius can be assessed and graded according to the congruity of its subchondral line.[17]
Figure 1.
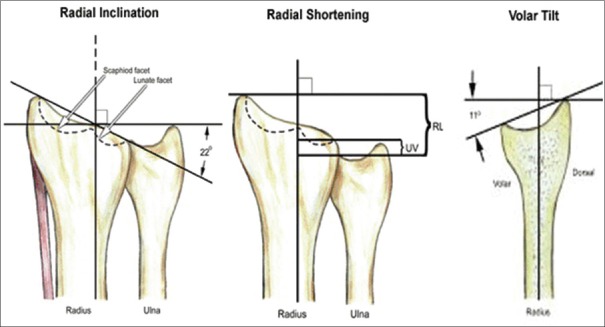
Various tilts and angles at distal radius and ulnar articular surface
Computed Tomography
CT may be useful and can give significant information in comparison with that obtained with conventional radiography in evaluation of complex or occult fractures, distal radial articular surface, distal radio-ulnar joint, ventro-medial fracture fragment (as described by Melone),[12] assessments of fracture healing as well as post-surgical evaluation.[7] CT may be indicated for the confirmation of occult fractures suspected on the basis of physical examination, when plain films are normal. CT may be indicated for preoperative evaluation of complex comminuted distal radius fractures and for exact evaluation of distal articular surface. As suggested in recent studies evaluating CT examination, imaging in axial and sagittal or axial and coronal planes with 2 mm contiguous sections is usually sufficient.[6,7,20] Cole concluded that CT scanning data, using the arc method of measurement, are more reliable for quantifying articular surface incongruities of distal radius than plain radiographic measurements.[21]
Magnetic Resonance Imaging
Although this modality is not the first choice in evaluating acute distal radius fractures, it is a powerful diagnostic tool to assess bony, ligamentous and soft tissue abnormalities associated with these fractures. MRI has proved to be a very important diagnostic tool for delineating perforation of triangular fibrocartilage complex (TFCC),[22] perforation of interosseous ligaments of proximal carpal row, evaluating occult fractures, post-traumatic or avascular necrosis of carpal bones. In regard to related injuries to flexor or extensor tendons as well as injury to the median nerve, MRI can be a very useful modality.[15] An evaluation of carpal tunnel disease after malunion of distal radial fractures can be performed successfully with MRI.[23]
Treatment Options
The basic principle of fracture treatment is to obtain accurate fracture reduction and then to use a method of immobilization that will maintain and hold that reduction. While the goal of treatment in fracture distal end of radius is restoration of normal function, the precise methods to achieve that desired outcome are controversial. Intra-articular fractures of distal end of the radius can be difficult to treat, at times, with traditional conservative method. A number of options for treatment are available to prevent the loss of reduction in an unstable fracture of the distal end of the radius.
Closed reduction and casting
All fractures characterized by minor comminution, without or with minimal displacements can be considered for closed reduction and cast immobilization. Mainly type I and type IIA Melone's fracture can be managed conservatively. The fracture should be kept under closed observation to look for any re-displacement. Despite the widespread acceptance of immobilization in a plaster cast, questions remain regarding the optimum position, the duration of immobilization and the need to extend the cast proximal to elbow. No clear consensus exists as to the best position for immobilizing the wrist in plaster. Sarmiento et al.[24] advocated immobilization in a position of supination to decrease the deforming force of the brachioradialis, which may cause loss of reduction. In contrast, Wahlstrom recommended immobilization in pronation because he claimed that the pronator quadratus causes the deforming force most responsible for the loss of reduction.[25] Most surgeons immobilize distal radius fractures in some amount of palmar flexion on the principle that dorsal periosteal hinge provides stability. However, the optimal position of hand function is with the wrist in dorsiflexion. Immobilization of the wrist in palmar flexion has a detrimental effect on hand function because dorsiflexion at the wrist is needed for proper rehabilitation of fingers.[26,27]
Pins and plaster technique
Placement of pins in the metacarpals and forearm was initially advocated by Bohler in 1923, but it gained popularity after the report by Green, who showed good or excellent results in 86% of his patients.[28] However, he noted a high incidence of minor or major complications, one-third of which were related to pin site only. Other researchers also noted that one-third of the complications were related to pins and 16% of the patients needed reoperation for complications.[29] Although this technique offers a method of maintaining reduction of many unstable fractures at a limited expense, the complications have led to a need for re-evaluation of this technique.
Percutaneous pinning
Extra-articular fractures of the distal end of the radius with extensive comminution or the fractures that have no more than two articular fragments, in which anatomical reduction is obtainable, are amenable to percutaneous pinning of the fracture fragments and application of a plaster cast. A single pin placed through the radial styloid as a means of stabilizing the displaced fracture fragment was first suggested by Lambotte in 1908.[30,31] Later, Depalma introduced the concept of large pin ulnar-radial pin fixation for the fractures of distal end of the radius with articular surface involvement.[32] Various modifications have been used by different authors showing good results. This is not effective for high energy complex fractures or fractures associated with soft tissue problems that preclude the use of plaster cast. However, this technique can be combined with metal fixation in these situations. Kapandji double intra-focal pinning and triple intra-focal pinning are the only methods that place 2 mm pins directly into fracture surface and then into the proximal radius.[33,34] In effect distal fragments are never directly engaged but rather are buttressed in place. This is a safe, simple and effective method for treatment of unstable fractures of the distal radius. Another method of ulnar-radial pinning with fixation of distal radio-ulnar joint was proposed in 1989.[35] He passed 4−9 (average 6) pins into the ulna, first horizontally across the distal radio-ulnar joint and then at increasing angles in a proximal direction along the ulna. Biomechanically this technique is very stiff but there is still not enough data to support this method of percutaneous pinning.
External fixation
External fixation is generally accepted as superior to plaster immobilization in the young patients with an intra-articular comminuted fracture of the distal radius. Other indications for external fixation include some unstable extra-articular fractures with significant comminution and failure to maintain reduction after an initial attempt at closed management in a cast, certain situations of multiple trauma, presence of dysfunctional contralateral limb, severe open fractures with significant soft tissue injury and neurovascular compromise, and bilateral injuries.[36] External fixation relies upon the principle of ligamentotaxis to apply traction and restore displacements. The use of an external fixation device is the only practical means of overcoming the force of the muscles of the forearm that pull comminuted distal radial fractures into a collapsed position. The use of an external fixator in the treatment of unstable intra-articular fractures of the distal radius has recently received support.[37]
A large variety of devices are available for this purpose. All involve distraction across the wrist joint with placement of pins in the radius and the metacarpals. Lipton and Wollstein suggested the placement of two pins into the second metacarpal, both in a plane that is at 45 degrees from the true vertical and from the true lateral.[38] The distal most pin angles slightly in a proximal direction and the proximal most pin angles in a slightly distal direction. The radial shaft is approached by placing the threaded pins between the brachioradialis and extensor carpi radialis longus. The fixator clamps and connecting bars are then placed in position, and while maintaining the distraction-reduction maneuver, the clamps are tightened and secured. Opponents of external fixation consider that it has got high incidence of complications, most of which are related to the pin problems.[39] This method is also unable to reduce the medial die-punch fragments.
Limited open reduction
In intra-articular fractures that have more than 2 mm of displacement, the radio-carpal joint may be incongruent despite adequate attempts at reduction. The incongruency usually involves the lunate part of the distal end of the radius. The radial styloid process and scaphoid facet are more amenable to reduction through ligamentotaxis or by manipulation and reduction. A new technique of combining external fixation with open reduction of the displaced lunate fossa through a small, longitudinal incision and elevation of the impacted fragment without direct visualization of the surface of the joint has been described.[40]
Open reduction and internal fixation
One of the recent advances in treatment of distal radius fractures is the more frequent application of open reduction and internal fixation, especially for intra-articular fractures. There are two groups of fractures for which open reduction and internal fixation is advisable. The first group includes the two-part shear fracture (Barton fracture), which actually is a radio-carpal fracture dislocation. Although anatomical reduction is possible by closed means in some cases, these fractures are very unstable and difficult to control in plaster. The second group includes complex intra-articular fractures in which the articular fragments are displaced, rotated or impacted and are not amenable to reduction through a limited operative exposure. Melone[5] reported on a series of 15 patients who underwent operative reconstruction of the distal radial articular surface; 14 of the 15 had good or excellent results.[41] A retrospective study reported that all patients with step off of 2 mm or more in the distal radial articular surface developed post-traumatic osteoarthrosis, whereas patients who healed with less than a 2 mm step off had only a 25% incidence of arthrosis.[42] Achievement of articular congruency in 88% of 17 patients treated with open reduction and internal fixation of comminuted intra-articular fractures of the distal end of the radius has been reported.[43]
Although enthusiasm for the operative approach for complex articular fractures of the distal end of the radius is growing, serious complications like loss of fixation, neuritis of the median nerve, reflex sympathetic dystrophy, infection of the wound and late post-traumatic arthritis can occur even when the surgeon is experienced.[44]
Most distal radial fractures result in an apex-volar angulation with dorsal cortical comminution. First-generation dorsal plate designs were a logical solution but were fraught with complications secondary to tendon dysfunction and rupture, which prompted a move to fixed-angle volar plating techniques after the development of angle-stable screws.[45] There is still a role for dorsal plating, and newer lower-profile designs may decrease complications. In certain situations, such as arthroscopy-assisted management of wrist fractures, dorsal die-punch fractures or fractures with displaced dorsal lunate facet fragments, a dorsal approach with a low-profile fragment-specific plate appears to work well.[46]
Several clinical studies have reported better functional results with volar plating than with dorsal plating, external fixation and percutaneous pinning; however, a complication rate of approximately 15% also has been reported with volar plating, primarily problems with tendon ruptures and tenosynovitis from prominent screws. Precise volar plate placement on the metaphyseal area of the distal radius may lessen the problems of flexor tendon irritation and eventual rupture.
Arthroscopic-Assisted Fracture Reduction
Intra-articular fractures of the radius can be arthroscopically assessed, and reduction of the articular components and assessment and repair of ligamentous injury can then be undertaken.[47,48,49,50,51,52] The ideal timing for arthroscopically assisted distal radius surgery is 3 to 7 days after injury. If performed later, it becomes difficult to manipulate the bone fragments. Due to soft tissue swelling and distortion of osseous landmarks, fluoroscopy is often used to identify portal sites. Distraction of the wrist with an external fixator can obviate the need for the wrist tower and allow manipulation and pinning of the fragments with the arm horizontal on the hand table. For simple fractures, such as those of the radial styloid, standard traction techniques are used. The procedure is contraindicated for patients with extensive soft tissue injuries, median nerve symptoms, compartment syndrome, or an open joint. Care must be taken to ensure that excessive fluid extravasation into the forearm compartments does not occur.
Many workers have independently reported excellent results with this technique in their series of patients.[50,51] A recent study has also provided some encouraging outcome data. Patients who underwent an arthroscopically assisted procedure had greater reduction of volar tilt, ulnar variance and articular gap displacement, and increased range of motion and grip strength at a mean of 31 months after the procedure, compared with patients who underwent open reduction and internal fixation.[53] However, in the above study, intra-operative fluoroscopy was not used; hence, the usefulness of arthroscopy over fluoroscopy could not be demonstrated in precise reduction.
In 2008, Lutsky et al. did arthroscopic assessment in all patients undergoing open reduction and internal fixation and observed that a volar approach, indirect reduction and locked plate fixation is a useful technique in restoring articular congruity after distal radius fracture.[54] They also stated that the magnitude of step and gap deformity may be underestimated by fluoroscopy.
Recent work assessing the follow-up functional results in patients undergoing arthroscopy and fluoroscopy-assisted external fixation with pinning versus only fluoroscopy assisted external fixation with percutaneous pinning has found better wrist range of motion in flexion, extension and supination.[55,56] DASH scores were comparable in either group in both studies.
These abovementioned studies focused only on single technique of fixation followed by arthroscopic assessment. No recent work demonstrates the role of arthroscopy in different types of reduction and fixation techniques and its comparative results in either. The differential role of arthroscopy in various fixation techniques has not been probed yet.
Complications
The type and frequency of complications varies among different series. McKay et al. found overall complication rates ranging from 6% to 80% and rates of post-traumatic arthritis that ranged from 7% to 65%. The most frequent complication is malunion with an intra-articular or extra-articular deformity as the most frequent complication. Other complications include non-union, hardware complications tendon attrition/rupture and neurological injuries.
Prevention and Prophylaxis
Prevention of any ailment is the best treatment of itself. For the fracture concerned here, the first step in prophylaxis or prevention is of around identification of risk factors and its evaluation. It starts from very beginning as physical examination and complete history taking. It includes multifactorial etiology, which is correlated with each other. Primordial prevention includes identification of these factors and implementing of methods and options either at personal level or at community level. The most common factor is low mineral density also known as osteopenia and osteoporosis. It is affected by various factors as age, sex, race, demographic factors, medical and surgical co-morbidities, hormonal imbalance, medicines that hinder calcium and vitamin metabolism, psycho-social factors, accident factors, etc., thus prevalence of fractures depends on complicated mesh of multifactorial causes.
Second step includes awareness of these factors and implementation. It can be improved by multiple ways in different strata. Education regarding these and primary health care completely cover this phase. Medical practitioner as family doctor or physician can fulfill this. He/she is a qualified teacher who knows about every aspect of fracture and its pathophysiology at primary level. Education and counseling regarding factors as lifestyle modifications, regular check-up of medical and surgical co-morbidities, and health consciousness helps in a very cost-effective way. Lifestyle modifications include healthy habits regarding avoidance of alcohol, tobacco and other addiction, and acceptance of adequate complete dietary advice. It also includes regular exercise, mostly isometric exercises, meditation activities, yoga exercises and recreation activities. A physician resides in the local community so it is very easy for him to explain and counsel to people about the whole texture of prevention in their own language and curriculum. He is also well experienced with primary treatment of fractures at primary level as splinting, bracing, general medications and maintenance doses. By some medical education camp in local community, he also explains and demonstrates about the usefulness of dietary supplements and their cost-effectiveness according to particular community. It includes proper balanced diet in regular basis according to seasons and social infrastructure. Addition of food supplement in deficient area, proper hygiene habits, water purification and way of consuming goods in an efficient way are some useful practices that can be done by a physician. Pain management after injury, immobilization with braces, and various positions and life-saving procedures concerned with fractures as management of shock, hypotension, fat embolism and sympathetic imbalance can be identified early by the physician and he can treat a patient either by himself or can refer to some specialist. He can also advise prophylaxis against future injury either at same organ or in different by teaching about use of braces, medications, gait training and minimal intervention procedures as RICE therapy, wax therapy, physiotherapy and rehabilitation practices. Thus a medical practitioner can play an efficient mediator for prevention of fractures by different manners.
Third and higher steps include different health programs, policies and their acts, health culture acculturation, and implementations of legal practices at community, national and international level. It stands at the apex of a pyramid and related with tertiary care centers, apex care centers and government statuary bodies.
Prevention of fracture is also concerned with different accidents. There are multiple factors that are either directly related with them or indirectly associated. It includes personal factors, community and other miscellaneous factors. Personal factors include medical and surgical problems associated with a person. Fracture incidence increases with poor vision, mental illness, lack of activities, chronic diseases as CRF, chronic liver diseases, chronic heart diseases, drug abuse, chronic drug therapy, immunity-deficient disorder, congenital and dysplastic disorder, weaning from chronic drugs and chronic steroid therapy. With these factors, even a trivial trauma can progress in a fracture of high severity. Community factors include broken family, nuclear family, poor care at old age, orphanage, population explosion, poor rehabilitation and stress in life. These are related with higher exposure to accidents and suicidal tendencies. Other miscellaneous are lack of awareness, avoidance of traffic rules, natural disasters, etc. Thus, most of the factors are modifiable and by modifying these we can prevent fracture incidence and its social burden in the form of morbidity and mortality.
Conclusion
Distal radius fracture is one of the most common fractures. It may be sustained due to low-energy trauma or high-energy trauma. Low energy extra-articular fractures are best managed conservatively while ORIF offers the best chances of an optimum outcome in intra-articular fracture. Wrist arthroscopy holds a promising future for this fracture and will certainly help in providing the best functional outcome for the patient. Family physicians have an important role in the prevention and prophylaxis of this fracture.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Pogue DJ, Vegas SF, Patterson RM, Peterson PD, Jenkins DK, Sweo TD, et al. Effects of distal radius malunion on wrist joint mechanics. J Hand Surg Am. 1990;15:721–7. doi: 10.1016/0363-5023(90)90143-f. [DOI] [PubMed] [Google Scholar]
- 2.Solomon L, Warwick D, Nayagam S. 9th ed. Florida: CRC press; 2001. Apley's System of Orthopaedics and Fractures; pp. 615–8. [Google Scholar]
- 3.Havemann D, Busse FW. Accident mechanisms and classifications in distal radius fractures. Langenbecks Arch Chir Suppl II Verh Dtsch Ges Chir. 1990:639–42. [PubMed] [Google Scholar]
- 4.Koval KJ, Zuckerman JD, Kenneth E. 2nd ed. Philadelphia, USA: Lippincott williams and Wilkins; Handbook of Fractures; pp. 133–8. [Google Scholar]
- 5.Trumble TE, Culp R, Hanel HP, Geissler WB, Berger RA. Instructional Course Lectures, The American Academy of Orthopaedic Surgeons - Intra-Articular Fractures of the Distal Aspect of the Radius. J Bone Joint Surg Am. 1998;80:582–600. [PubMed] [Google Scholar]
- 6.Stewart NR, Gilula LA. CT of the wrist: A tailored approach. Radiology. 1992;183:13–20. doi: 10.1148/radiology.183.1.1549659. [DOI] [PubMed] [Google Scholar]
- 7.Quinn SF, Murray W, Watkins T, Kloss J. CT for determining the results of treatment of fractures of the wrist. AJR Am J Roentgenol. 1987;149:109–11. doi: 10.2214/ajr.149.1.109. [DOI] [PubMed] [Google Scholar]
- 8.Nissen-lie HS. Fracture radii “typical”. Nord Med. 1939;1:293–303. [Google Scholar]
- 9.Gartland JJ, Jr, Werley CW. Evaluation of healed Colles’ fractures. J Bone Joint Surg Am. 1951;33:895–907. [PubMed] [Google Scholar]
- 10.Lidstrom A. Fractures of the distal end of the radius. A clinical and statistical study of end results. Acta Orthop Scand Suppl. 1959;41:1–118. [PubMed] [Google Scholar]
- 11.Frykman G. Fractures of the distal radius, including sequelae - shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function: A clinical and experimental study. Acta Orthop Scand. 1967;108:3+. doi: 10.3109/ort.1967.38.suppl-108.01. [DOI] [PubMed] [Google Scholar]
- 12.Melone CP., Jr Articular fractures of the distal radius. Orthop Clin North Am. 1984;15:217–36. [PubMed] [Google Scholar]
- 13.Mueller ME, Nazarian S, Koch P. Berlin: Springer-Verlag; 1987. AO classification of fractures. [Google Scholar]
- 14.Fernandez DL. Fractures of the distal radius: Operative treatment. Instr Course Lect. 1993;42:73–88. [PubMed] [Google Scholar]
- 15.Metz VM, Gilula LA. Imaging techniques for distal radius fractures and related injuries. Orthop Clin North Am. 1993;24:217–28. [PubMed] [Google Scholar]
- 16.Hardy DC, Totty WG, Reinus WR, Gilula LA. Postero-anterior wrist radiography: Importance of arm positioning. J Hand Surg Am. 1987;12:504–8. doi: 10.1016/s0363-5023(87)80196-x. [DOI] [PubMed] [Google Scholar]
- 17.Knirk J, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg. 1986;68:647–59. [PubMed] [Google Scholar]
- 18.Trumble TE, Culp RW, Hanel DP, Geissler WB, Berger RA. Intra-articular fractures of the distal aspect of the radius. Instr Course Lect. 1999;48:465–80. [PubMed] [Google Scholar]
- 19.Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg Am. 1991;16:375–84. doi: 10.1016/0363-5023(91)90001-r. [DOI] [PubMed] [Google Scholar]
- 20.Biondetti PR, Vannier MW, Gilula LA, Knapp R. Wrist: Coronal and transaxial CT scanning. Radiology. 1987;163:149–51. doi: 10.1148/radiology.163.1.3823428. [DOI] [PubMed] [Google Scholar]
- 21.Cole RJ, Bindra RR, Evanoff BA, Gilula LA, Yamaguchi K, Gelberman RH. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: Reliability of plain radiography versus computed tomography. J Hand Surg. 1997;22:792–800. doi: 10.1016/s0363-5023(97)80071-8. [DOI] [PubMed] [Google Scholar]
- 22.Golimbu CN, Firooznia H, Melone CP, Jr, Rafii M, Weinreb J, Leber C. Tears of the triangular fibrocartilage of the wrist: MR imaging. Radiology. 1989;173:731–3. doi: 10.1148/radiology.173.3.2813778. [DOI] [PubMed] [Google Scholar]
- 23.Kellerhouse LE, Reicher MA. MRI of the wrist and hand. New York: Raven Press; 1990. Osteonecrosis and fractures of the wrist; p. 107. [Google Scholar]
- 24.Sarmiento A, Pratt GW, Berry NC, Sinclir WF. Colles’ fractures. Functional bracing in supination. J Bone Joint Surg Am. 1975;57:311–7. [PubMed] [Google Scholar]
- 25.Wahlstrom O. Treatment of Colles’ fractures. Acta Orthop Scand. 1991;62:284–7. doi: 10.3109/17453678208992206. [DOI] [PubMed] [Google Scholar]
- 26.Gupta A. The treatment of Colles’ fractures. Immobilisation with the wrist dorsiflexed. J Bone Joint Surg Br. 1991;73:312–5. doi: 10.1302/0301-620X.73B2.2005163. [DOI] [PubMed] [Google Scholar]
- 27.Agee JM. External fixation. Technical advances based upon multiplanar ligamentotaxis. Orthop Clin North Am. 1993;24:265–74. [PubMed] [Google Scholar]
- 28.Green DP. Pins and plaster treatment of comminuted fractures of the distal end of the radius. J Bone Joint Surg Am. 1975;57:304–10. [PubMed] [Google Scholar]
- 29.Chapman DR, Bennet JB, Bryan WJ, Tullos HS. Complications of distal radial fractures: Pins and plaster treatment. J Hand Surg Am. 1982;7:509–12. doi: 10.1016/s0363-5023(82)80049-x. [DOI] [PubMed] [Google Scholar]
- 30.Rayhack JM. The history and evolution of percutaneous pinning of displaced distal radial fractures. Orthop Clin North Am. 1993;24:287–300. [PubMed] [Google Scholar]
- 31.Mah ET, Atkinson RN. Percutaneous Kirschner wire stabilisation following closed reduction of Colles’ fractures. J Hand Surg Br. 1992;17:55–62. doi: 10.1016/0266-7681(92)90012-q. [DOI] [PubMed] [Google Scholar]
- 32.DePalma AF. Comminuted fractures of the distal end of the radius treated by ulnar pinning. J Bone Joint Surg Am. 1952;34:651–62. [PubMed] [Google Scholar]
- 33.Kapandji A. Bone fixation by double percutaneous pinning. Functional treatment of non-articular fractures of the distal radius. Ann Chir Main. 1976;6:903–8. [PubMed] [Google Scholar]
- 34.Kapandji A. Internal fixation by double intrafocal pinning. Functional treatment of non-articular fractures of the lower end of the radius. Ann Chir. 1976;30:903–8. [PubMed] [Google Scholar]
- 35.Rayhack JM, Langworthy JN, Belsole RJ. Transulnar percutaneous pinning of displaced distal radial fractures: A preliminary report. J Orthop Trauma. 1989;3:107–14. doi: 10.1097/00005131-198906000-00004. [DOI] [PubMed] [Google Scholar]
- 36.Seitz WH., Jr External fixation of distal radius fractures. Indications and technical principles. Orthop Clin North Am. 1993;24:255–64. [PubMed] [Google Scholar]
- 37.Cooney WP. External fixation of distal radial fractures. Clin Orthop Relat Res. 1983:44–9. [PubMed] [Google Scholar]
- 38.Lipton HA, Wollstein R. Operative treatment of intra-articular distal radial fractures. Clin Orthop Relat Res. 1996:110–24. doi: 10.1097/00003086-199606000-00016. [DOI] [PubMed] [Google Scholar]
- 39.Szabo RM, Weber SC. Comminuted intra-articular fractures of the distal radius. Clin Orthop Relat Res. 1988:39–48. [PubMed] [Google Scholar]
- 40.Axelrod T, Paley D, Green J, McMurtry RY. Limited open reduction of the lunate facet in comminuted intra-articular fractures of distal radius. J Hand Surg Am. 1988;13:372–7. doi: 10.1016/s0363-5023(88)80012-1. [DOI] [PubMed] [Google Scholar]
- 41.Melone CP., Jr Open treatment for displaced articular fractures of the distal radius. Clin Orthop Relat Res. 1986:103–11. [PubMed] [Google Scholar]
- 42.Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1989;71:839–47. [PubMed] [Google Scholar]
- 43.Axelrod TS, McMurtry RY. Open reduction and internal fixation of comminuted intra-articular fractures of the distal radius. J Hand Surg Am. 1990;15:1–11. doi: 10.1016/s0363-5023(09)91097-8. [DOI] [PubMed] [Google Scholar]
- 44.Porter M, Stockley I. Fractures of the distal radius. Intermediate and end results in relation to radiological parameters. Clin Orthop Relat Res. 1987:241–52. [PubMed] [Google Scholar]
- 45.Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D. Fracture of the distal radius: Risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011;36:3–9. doi: 10.1016/j.jhsa.2010.09.033. [DOI] [PubMed] [Google Scholar]
- 46.Ross M, Heiss-Dunlop W. Volar angle stable plating for distal radius fractures. In: Slutsky DJ, editor. Principles and Practice of Wrist Surgery. 2nd ed. Philadelphia: Elsevier; 2010. pp. 126–39. [Google Scholar]
- 47.Whipple TL. The role of arthroscopy in the treatment of intra-articular wrist fractures. Hand Clin. 1995;11:13–8. [PubMed] [Google Scholar]
- 48.Geissler WB, Freeland AE. Arthroscopically assisted reduction of intraarticular distal radial fractures. Clin Orthop Relat Res. 1996:125–34. doi: 10.1097/00003086-199606000-00017. [DOI] [PubMed] [Google Scholar]
- 49.Osterman AL. Wrist arthroscopy: Operative procedures. In: Green DP, Hotchkiss RN, Pederson WC, editors. Green's Operative Hand Surgery. 4th ed. Vol. 1. New York: Churchill Livingstone; 1999. pp. 207–22. [Google Scholar]
- 50.Wolfe SW, Easterling KJ, Yoo HH. Arthroscopic-assisted reduction of distal radius fractures. Arthroscopy. 1995;11:706–14. doi: 10.1016/0749-8063(95)90114-0. [DOI] [PubMed] [Google Scholar]
- 51.Culp RW, Osterman AL. Arthroscopic reduction and internal fixation of distal radius fractures. Orthop Clin North Am. 1995;26:739–48. [PubMed] [Google Scholar]
- 52.Richards RS, Bennett JD, Roth JH, Milne K., Jr Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22:772–6. doi: 10.1016/S0363-5023(97)80068-8. [DOI] [PubMed] [Google Scholar]
- 53.Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: Arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999;81:1093–110. doi: 10.2106/00004623-199908000-00005. [DOI] [PubMed] [Google Scholar]
- 54.Lutsky K, Boyer MI, Steffen JA, Goldfarb CA. Arthroscopic assessment of intra-articular distal radius fractures after open reduction and internal fixation from a volar approach. J Hand Surg Am. 2008;33:476–84. doi: 10.1016/j.jhsa.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 55.Ruch DS, Vallee J, Poehling GG, Smith BP, Kuzma GR. Arthroscopic reduction versus fluoroscopic reduction in the management of intra-articular distal radius fractures. Arthroscopy. 2004;20:225–30. doi: 10.1016/j.arthro.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 56.Varitimidis SE, Basdekis GK, Dailiana ZH, Hantes ME, Bargiotas K, Malizos K. Treatment of intra-articular fractures of the distal radius: Fluoroscopic or arthroscopic reduction? J Bone Joint Surg Br. 2008;90:778–85. doi: 10.1302/0301-620X.90B6.19809. [DOI] [PubMed] [Google Scholar]


