Abstract
Background:
Depressive symptoms are often not detected properly in elderly. The aim of this study was to explore the prevalence of depressive symptoms and possible co relational factors among elderly population.
Materials and Methods:
In a cross-sectional study, 100 elderly persons were screened. Geriatric depression scale (GDS) was used to assess depressive symptoms. A self-rating questionnaire was used to detect some sociodemographics and clinical variables.
Results:
100 respondents interviewed, 40 were 70 years and above and 41% were male. Sixty individuals (25 males and 35 females) were found to be mildly depressed. Seventeen (4 males and 13 females) were suffering from severe depression.
Conclusion:
This study is in line with previous studies showing the high prevalence of depression in elderly. Results suggest a proper screening for depression among elderly.
Keywords: Depression, geriatric, mental health, prevalence
Introduction
Population ageing is a global phenomenon. The elderly over 60 years of age constituted 7% of India's population in 2009, likely to increase to 20–30% by 2050 as projected.[1] Due to improved health-care delivery and decreased mortality, population of elderly is growing. This has lead to the increased risk of multiple chronic medical disorders and geriatric syndromes and many socioeconomic challenges. It has been documented that elderly are more prone to psychological problems and depression is the most common geriatric psychiatric disorder. In India, elderly face multitude of psychological, social, and physical health problems. With the advancement of age there is increased morbidity and functional loss. Various life events greatly impact one's psychological status. Depression in elderly is manifested as major or minor depression characterized by collection of depressive symptoms.[2]
According to WHO, factors increasing depression risk in older adults include genetic susceptibility, chronic disease and disability, pain, frustration with limitations in activities of daily living (ADL), personality traits (dependent, anxious or avoidant), adverse life events (separation, divorce, bereavement, poverty, and social isolation) and lack of adequate social support.[3] Many studies have demonstrated a relationship between depression and various socioeconomic variables such as advanced age, low education, poverty, and manual occupation.[4,5,6]
The goal of this study is to explore the magnitude and risk factors of problems of depression in elderly people residing in Faridkot and surrounding areas both in urban and rural setting.
Material and Methods
A cross-sectional study is conducted among elderly persons belonging to different socioeconomic and varying demographic groups of Faridkot and adjoining areas. A total of 100 persons were interviewed.
Inclusion criteria
Comprised of all consenting subjects equal to or more than 60 years of age.
Exclusion criteria
Persons not consenting were excluded and with whom communication was difficult due to any reason (hearing loss and language problems) were also excluded.
Data collection
The questionnaire was divided into two parts. The first part comprised of sociodemographic information covering a diverse set of parameters as age, sex, marital status, education, area of residence, and occupation. Any chronic illness if present is also recorded. The second part comprised of a scale known as geriatric depression scale (GDS).
The GDS is a 30-item self-report assessment used to identify depression in the elderly. The scale was first developed in 1982 by JA Yesavage and others.[7]
Data analysis
The data were analyzed using SPSS-16 and the results were recorded as frequencies, means ± standard deviations (SD) and P values. Tables and figures were used for comprehensive viewing of the results. The Chi-square test was used for categorical variables. A P value of < 0.05 was taken as the criteria of significance for all purposes.
The GDS questions are answered ‘yes’ or ‘no’, instead of a five-category response set. This simplicity enables the scale to be used with ill or moderately cognitively impaired individuals. The scale is commonly used as a routine part of a comprehensive geriatric assessment. One point is assigned to each answer and the cumulative score is rated on a scoring grid. The grid sets a range of 0–9 as ‘normal’, 10–19 as ‘mildly depressed’, and 20–30 as ‘severely depressed’.
Observations
A total of 100 subjects were interviewed and using GDS, 23 subjects were found to be having score 0–9 that means normal, 60 were mildly depressed with GDS score 10–19 and 17 were severely depressed having a score >20. So prevalence of severe depression was found to be 17% [Table 1]. Community-based mental health studies in India have revealed that the point prevalence of depressive disorders in the elderly Indian population varies between 13% and 25%.[8,9] Nandi et al. in their pioneering epidemiological survey found that 21.4% of subjects aged 60 and above in the community suffered from depression.[8]
Table 1.
Distribution of GDS-30 scores (n=100)
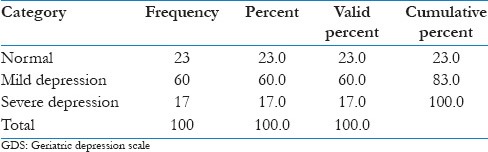
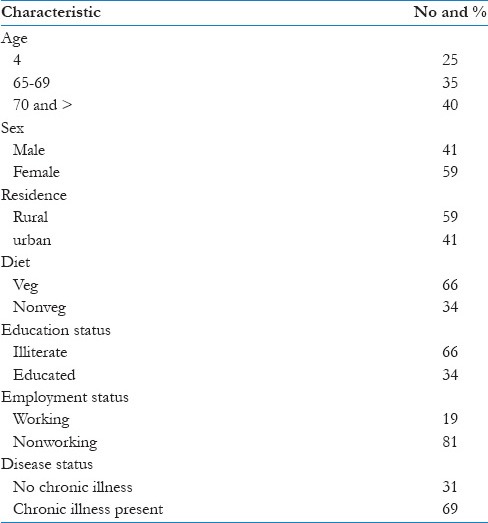
Table 2 reveals various socioeconomic and demographic profiles of subjects. Among 100 subjects 25% were between 60–64 years of age, 35% between 65–69 years and 40% were 70 years and above. Forty-one percent were males and 59% were females. Fifty-nine percent of subjects belonged to rural areas and 41% resided in urban set up. Sixty-six percent of subjects were illiterate and 34% were educated. Among 100 subjects 81% were not doing any job so they were dependent on other family members for monetary needs. Sixty-nine percent were suffering from various diseases like diabetes, hypertension, chronic renal failure etc., and 31% were otherwise normal.
Table 2.
Sociodemographic characteristics of study subjects (n=100)
Discussion
In this study, severe depressive symptoms in were found to be 17% elderly while 60% were mildly depressed. Depression is often not detected properly in elderly population. Prevalence of depressive symptoms varied from 13.5% to 36.8% in community dwelling older adults.[10,11,12] Some other studies have revealed that the prevalence rates for depression in community samples of elderly in India vary from 6% to 50%.[13,14] The prevalence of depression in Caucasian elderly populations in the West vary from 1% to 42%.[15]
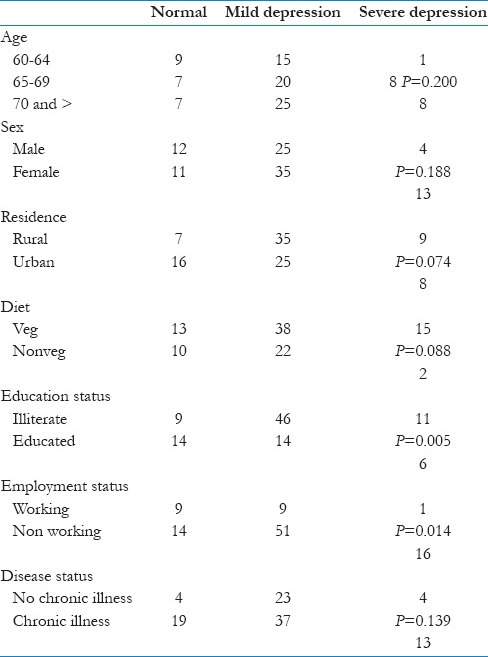
Depressive symptoms were positively correlated to Education status (P = 0.005) and employment status (P = 0.014). There was a higher rate of depression in literates. But there was no significant association between sex (P = 0.188), diet (P = 0.088), living area (P = 0.074), and disease status (P = 0.139) and depressive symptoms among sample. There was no change in the ratio of depressive symptoms in the various age group [Table 3].
Table 3.
Sociodemographic characteristics and depression (n=100)
The absence of a caregiver was deduced to be a possible risk factor for depression. However, we did not find any significant association with depression in our study. One possible reason for this finding could be that we did not ask the number of caregivers or who the caregiver was.
The high prevalence of depression observed among older adults emphasize on the need of increased community support and availability of health care services for better care of the elderly. There is also an urgent need for greater awareness of depression among family members and community at large. At the same time, it is important to increase community support and create networks for better geriatric care, in accordance with WHO findings. This type of study is important to persuade community-based medical personnel like family physician of the importance of diagnosing and treating depression. When dealing with older adults, health personnel must always keep in mind the possibility of depression; it frequently manifests with somatic symptoms (headache, tension, heaviness, etc.), for which patients visit nonpsychiatric outpatient departments seeking relief for their symptoms.
The cross-sectional nature of this study is a limitation, in that causal relationships cannot be inferred. Also, the small sample size limits generalizability, so large-scale studies are needed for a better picture of mental health in rural older adults in India.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.United Nations Dept. of International Economic and Social Affairs, population Division (2010) World Population Ageing 2009, United Nations NY. 2010 [Google Scholar]
- 2.Satcher D. Mental health – A report of the surgeon general. 2000;31:15–23. [Google Scholar]
- 3.World Health Organization. Geneva: World Health Organization; 2001. [Last cited on 2012 Nov 21]. The World Health Report 2001. Mental Health: New Understanding, New Hope [Internet] p. 169. Available from: http://www.who.int/whr/2001/en/whr01_en.pdf . [Google Scholar]
- 4.Murata C, Kondo K, Hirai H, Ichida Y, Ojima T. Association between depression and socio-economic status among community-dwelling elderly in Japan: The Aichi Gerontological Evaluation Study (AGES) Health Place. 2008;14:406–14. doi: 10.1016/j.healthplace.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 5.Kim JM, Shin IS, Yoon JS, Stewart R. Prevalence and correlates of late-life depression compared between urban and rural populations in Korea. Int J Geriatr Psychiatry. 2002;17:409–15. doi: 10.1002/gps.622. [DOI] [PubMed] [Google Scholar]
- 6.Barua A, Ghosh MK, Kar N, Basilio MA. Socio-demographic factors of geriatric depression. Indian J Psychol Med. 2010;32:87–92. doi: 10.4103/0253-7176.78503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: A preliminary report. J Psychiatr Res. 1982-83;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 8.Nandi DN, Rajkumar S, Padmavathy R, Thara R. The incidence of mental disorders in one year in a rural community in West Bengal. Indian J Psychiatry. 1976;18:79–87. [Google Scholar]
- 9.Ramchandran V, Menon SM, Arunagiri S. Socio-cultural factors in late onset depression. Indian J Psychiatry. 1982;24:268–73. [PMC free article] [PubMed] [Google Scholar]
- 10.Beekman AT, Copeland JR, Prince MJ. Review of community prevalence of depression in later life. Br J Psychiatry. 1999;174:307–11. doi: 10.1192/bjp.174.4.307. [DOI] [PubMed] [Google Scholar]
- 11.Blazer D, Williams CD. The epidemiology of dysphoria and depression in an elderly population. Am J Psychiatry. 1980;137:439–44. doi: 10.1176/ajp.137.4.439. [DOI] [PubMed] [Google Scholar]
- 12.Urbina Torija JR, Flores Mayor JM, Garcia Salazar MP, Torres Buisán L, Torrubias Fernández RM. Depressive symptoms in the elderly. Prevalence and associated factors. Gac Sanit. 2007;21:37–42. doi: 10.1157/13099119. [DOI] [PubMed] [Google Scholar]
- 13.Venkoba Rao A. Psychiatry of old age in India. Int Rev Psychiatry. 1993;5:165–70. [Google Scholar]
- 14.Nandi PS, Banerjee G, Mukherjee SP, Nandi S, Nandi DN. A study of psychiatric morbidity in an elderly population in a rural community in West Bengal. Indian J Psychiatry. 1997;39:122–9. [PMC free article] [PubMed] [Google Scholar]
- 15.Djernes JK. Prevalence and predictors of depression in populations of elderly: A review. Acta Psychiatr Scand. 2006;113:372–87. doi: 10.1111/j.1600-0447.2006.00770.x. [DOI] [PubMed] [Google Scholar]


