Abstract
Background and objectives:
Obesity and overweight is a growing pandemic affecting millions of adolescents in developed as well as developing countries. Obesity is associated with the onset of major chronic diseases leading to complications and also psychosocial problems in adolescents. The greater concern is that the risks of obesity during childhood will persist into adolescence and adulthood. The objectives of the study were to assess the prevalence of being overweight and obesity and to study the associated risk factors.
Materials and Methods:
1900 adolescents in the age group of 10–19 years were included in the study. A predesigned and pretested questionnaire which included the variables such as going to school by bus or cycle, eating habits, playing video/computer games or outdoor games and sibling count were recorded. Body weight and height were recorded in subjects for calculating body mass index (BMI). International Obesity Task Force (IOTF) classification was used for the estimation of being overweight and obese.
Results:
The mean age of the study subjects was 14.84 years (SD = 2.81). Mean weight increased from 34.7 to 55.09 kg from the age group 10–13 to 17–19 years. Mean height also increased from 1.34 to 1.57 m from the age group 10–13 to 17–19 years. Similarly, the mean body mass index was 19.23 at 10–13 years, followed by 21.11 at 14–16 years and 22.46 at 17–19 years. On binary logistic regression analysis, female gender, bus as a mode of transport, not playing games, and single sibling were found to have independent association with prevalence of being overweight.
Keywords: Adolescents, anthropometry, body mass index, obesity, overweight
Introduction
The World Health Organization (WHO) describes overweight and obesity as one of the today's most important public health problem, which is being escalated as a global epidemic.[1] It is also increasingly recognized as a significant problem in developing countries and countries undergoing economic transition.[2] The problem of being overweight and obesity is confined not only to adults but also being reported among the children and adolescents in the developed countries during the past two decades[3] as well as similar trends are being observed even in the developing world, though less rapidly.[4,5,6]
Global trends of childhood obesity show huge shifts in recent times. Surveys from 144 countries suggest that 43 million preschool children (35 million in developing countries) are overweight and obese and 92 million are at risk of being overweight. The worldwide prevalence of childhood overweight and obesity increased from 4.2% in 1990 to 6.7% in 2010. This trend is likely to continue and the prevalence is expected to reach 9.1%, or 60 million, in 2020.[7]
A study conducted among 24,000 school children in south India showed that the proportion of overweight children increased from 4.94% of the total students in 2003 to 6.57% in 2005 demonstrating the time trend of this rapidly growing epidemic.[8]
At least 30% of obesity begins in childhood. Conversely 50% to 80% of obese children become obese adults.[7] In the Harvard study, morbidity from cardiovascular diseases, diabetes, obesity-related cancers and arthritis were 50–100% higher in obese individuals who were also obese as children and generally the cardiovascular mortality in such individuals was doubled.[9]
India is facing a “twin epidemic” in the form of under- and over-nutrition in children and adolescents. Over-nutrition predisposes them to insulin resistance, metabolic syndrome, and type 2 diabetes mellitus (T2DM). Increasing prevalence of obesity and insulin resistance has been reported in Asian Indian adolescents.[10] It is the need of the hour to access and check the rising menace of this upcoming epidemic. Hence, close monitoring of overweight prevalence in children and adolescents and taking timely preventive measures will be an effective approach in dealing with the problem of obesity. In view of these contexts, this study was undertaken to estimate the prevalence of overweight and obesity in urban adolescent students of Rohtak (Haryana), India and to study the possible risk factors in adolescents aged 10–19 years.
Materials and Methods
Study area
This study was conducted in government and private schools and colleges of the Rohtak city that is an urban city in north India located 70 km northwest of New Delhi and 250 km south of the state capital Chandigarh.
Study design
Cross-sectional and observational study.
Study period
The study was conducted from the period August 2011 to July 2012.
Inclusion criteria
Age between 10 to 19 years.
Exclusion criteria
Subjects with bony deformities
Chronic or diarrhoeal diseases
Subjects on long term medicines
Subjects absent on the day of visit
Subjects who did not volunteer to participate in the study.
Study participants
All students aged 10–19 years from class V to junior college present at the time of visit constituted the study population.
Sample size calculation
The sample size was calculated as 1900, assuming the prevalence of obesity in urban areas as 5%[11] and allowable error of 20% at 95% of level of significance.
Ethical consideration
The study protocol was reviewed and approved by the institutional review board and written informed consent was obtained from head of institutions and each study subject before enrolment.
Study protocol
A list of schools and junior colleges was obtained from DEO (District Education Office) and by simple random sampling (using lottery method); a total of 10 schools (five Govt and five Private) and two Junior colleges were selected. Equal representation from govt. and private institutions as well as of male and female subjects was ensured. The subjects were divided into three categories of 10–13 years, 14–16 years, and 17–19 years with equal number of subjects in each of the three age groups, respectively. Randomization of study subjects was ensured for each class division employing simple random sampling without replacement taking class attendance register as reference on the day of the visit.
A predesigned and pretested questionnaire which included the characteristics of respondents such as type of family, literacy status, and occupation of father and mother and variables such as going to school by bus or cycle, eating habits, playing video/computer games or outdoor games and sibling count were filled by the investigator himself by interviewing the study subjects individually. The date of birth of each student was taken from the school records to verify the age. After filling the questionnaire, study subjects were called to a separate room to take their anthropometric measurements. For female study subjects, privacy was maintained and a female paramedical health worker was present while taking measurements.
Anthropometry
Anthropometric measurements including body weight (to the nearest 0.1 kg) and height (to the nearest. 001 m) were recorded in subjects without shoes and socks. The weighing scale was regularly checked with known standard weights and a portable anthropometric rod was used for measuring height. Using the weight and height, Body mass index (BMI) was calculated in Kg/m2, for each subject.
Criteria for overweight and obesity
IOTF classification was utilized for the estimation of overweight and obese subjects. Overweight is defined as children with BMI value between 85th to 95th percentile for a specific age and sex. Similarly obesity is defined as children with a BMI value above 95th percentile for a specific age and sex.[12]
Statistical analysis
Analysis was carried out using SPSS for version 17.0. Pearson's Chi-square test was used to evaluate differences between groups for categorized variables. Normally distributed data were presented as means and standard deviation, or 95% confidence intervals. All tests were performed at a 5% level significance. Logistic regression analysis was used to determine the odds ratio (95% CI) of the presence of at least one risk factor in subjects categorized as overweight or obese.
Results
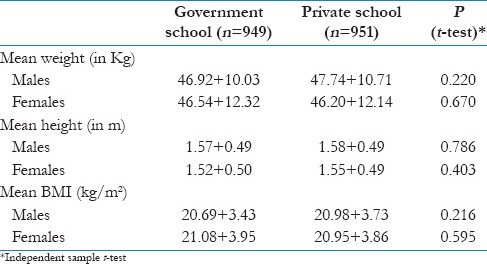
Mean age of the study subjects was 14.84 ± 2.81 years. Mean weight increased from 34.7 to 55.09 kg from age group 10–13 years to 17–19 years. The mean height also increased from 1.34 to 1.57 m from age group 10–13 to 17–19 years. Similarly, mean body mass index was 19.23 at 10–13 year, followed by 21.11 at 14–16 year and 22.46 at 17–19 year. Mean weight, height, and BMI among male subjects were higher in private schools whereas in female subjects, mean weight, and BMI were higher in government schools [Table 1]. These values were not found to be statistically significant.
Table 1.
Comparison between government and private institutes for different anthropometric parameters
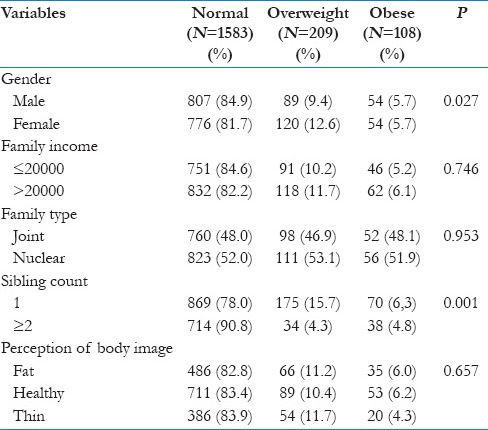
The prevalence of overweight and obesity was found to be 11% and 5.7%, respectively, using IOTF age and sex specific 85th and 95th percentile criteria. Both male and female subjects had equal prevalence of obesity (5.7%) while overweight prevalence was found to be higher in females (12.6%) than in male subjects (9.4%) and this finding was statistically significant (P: 0.027) [Figures 1 and 2]. The prevalence of obesity and overweight was found to be higher (6.1% and 11.7%) in higher income group (>20000 Rs) when compared to lower income group (≤20000 Rs). Higher prevalence of overweight (53.1%) and obesity (51.9%) was found among subjects of nuclear family when it was compared with subjects of joint family (46.9%) and (48.1%), respectively, but this finding was not statistically significant (P: 0.953). The prevalence of overweight and obesity was higher in subjects who were having one sibling as compared to subjects who were having sibling count ≥ 2 and this finding was statistically significant (P < 0.001). Among obese and overweight subjects, 11.7% and 13.6% were not involved in playing games. The prevalence of overweight and obesity among subjects using bus as mode of transport was found as 20.4% and 8.7% compared to subjects using cycle as a mode of transport in which it was 7.2% and 4.4%, respectively. This finding was statistically significant (P < 0.001). 11.2% of overweight and 6.0% of obese subjects had a perception of being fat whereas 11.7% and 4.3% of being overweight and obese subjects thought themselves to be thin. This finding was not significant. Other variables like education and occupation of parents, diet pattern and having breakfast before going to school were not significantly related to the prevalence of overweight and obesity [Table 2].
Figure 1.
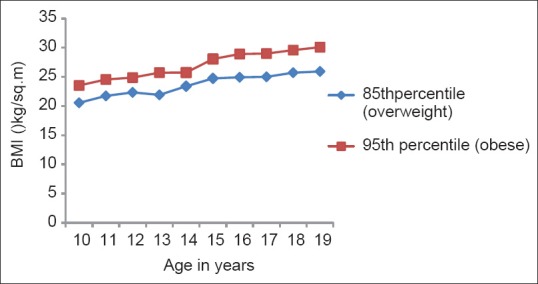
Line diagram for 85th and 95th percentile of BMI for male study subjects
Figure 2.
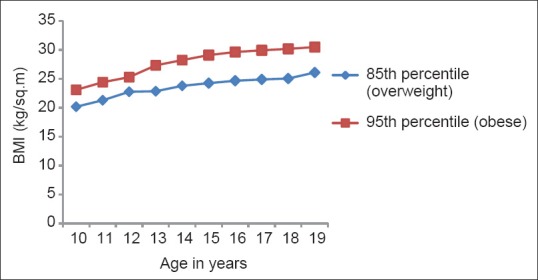
Line diagram for 85th and 95th percentile of BMI for female study subjects
Table 2.
Baseline characteristics of the study subjects
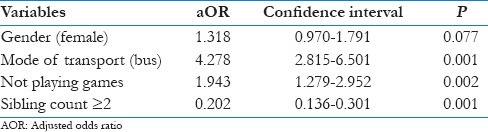
Binary logistic regression was applied to predict the prevalence of overweight using gender, family income, family type, sibling count, diet pattern, physical activity, mode of transport, having breakfast, and perception of body image as predictors. In our study population female gender, bus as a mode of transport, not playing games and one sibling count were found to have independent association with prevalence of overweight [Table 3]. Adolescents are four times more likely to be overweight if they use bus as a mode of transport (aOR: 4.278; 95% CI: 2.815–6.501, P < 0.01). Female gender and not playing games also had a positive relation with overweight (Female gender; aOR: 1.318,95% CI: 0.970–1.791, P: 0.077, not playing games; aOR: 1.943, 95% CI: 1.279–2.952, P: 0.002). Sibling count more than two was also a positive predictor of overweight (aOR: 0.202: 95% CI: 0.136–0.301, P < 0.001).
Table 3.
Independent association of variables with overweight and obesity (logistic regression analysis)
Discussion
Indians, as an ethnic group are particularly at high risk for insulin resistance (syndrome X) and central obesity, both forerunners of diabetes, CHD and other “life style" disorders. It is now emerging convincingly that these disorders begin in childhood and manifest due to interactions and accumulation of various risk factors, throughout the life course. Mehta et al. in a cross-sectional study done in four public schools of Delhi reported the prevalence of obesity and overweight as 5.3% and 15.2%, respectively[13] while in an another study Sharma et al. reported the prevalence of obesity as 6.4% in school children of Delhi.[14] In our study the prevalence of overweight and obesity was found to be 11.0% and 5.7%, respectively. This is because Rohtak city enjoys all modern amenities such as readily available fast/junk food corners, availability of modern gadgets and transport facilities for school are leading factors for the increased prevalence of overweight and obesity in adolescents.
Maximum prevalence of obesity (6.6%) was observed in adolescents at 16 years of age whereas 14.2% of overweight subjects were at age 15 years. Similar findings of 10.8% overweight at the age of 15 years were reported by Laxmaiah et al. in Hyderabad.[15] This increase of prevalence in the aforementioned age group may be associated with the increase in adipose tissue and overall weight gain during the pubertal growth spurt. Playing outdoor games are also compromised in this age group because of increased study hours. Significantly higher prevalence (57.4%) of overweight was seen in female adolescents than the males while the prevalence of obesity was equal. On logistic analysis, female gender was found to be a predictor of overweight (aOR-1.318). Kumari and Krishna in Guntur, Andhra Pradesh reported significantly higher prevalence of overweight among girls than boys.[16] Similarly, Singh et al. conducted a study in Manipur which revealed a higher prevalence of overweight in girls (5.10%) as compared to boys (2.34%)(17).[21] This may be due to the physiological fact that adolescence is a period of increase in fatness of females and transient decrease in fatness of males due to increase in muscle and bone mass in the body. Secondly, due to social reasons, girls play less outdoor games as compared to boys, as parents do not allow them to go far from houses and little space is available in homes to play outdoor games effectively.
Bivariate analysis revealed that odds of getting overweight were reduced (aOR-0.202) when sibling count was ≥2. This finding was statistically significant. Padez et al. revealed that the prevalence of overweight and obesity significantly decreased as the number of siblings’ increased.[18] Another study by Guedes et al. among Brazilian school children depicted similar findings that the prevalence of being overweight significantly decreased as the number of siblings increased (P: 0.037).[19] The aforementioned finding may be explained by the fact that having more siblings is associated with lower rates of obesity. Social scientists have observed that additional children in the family may dilute available parental time and resources. However, siblings may also serve as a stimulus for child-to-child interactions, cooperative play or activities that increase the time each child devotes to physical activity along with division of parental pampering.
11.7% obese and 13.6% overweight subjects were not involved in playing activities and this finding was statistically significant. Bivariate analysis found playing outdoor games to be a significant predictor of overweight (aOR-1.943; 95% CI: 1.279–2.952; P-0.002). Goyal et al. reported that outdoor games on weekly basis had an odds ratio of 1.75 for obesity and overweight in comparison to no outdoor games having odds ratio 2.23.[20] The prevalence of overweight and obesity among subjects using bus as mode of transport was found as 20.4% and 8.7% compared to subjects using cycle as a mode of transport in which it was 7.2% and 4.4%, respectively. Logistic regression analysis revealed that bus as a mode of transport is a strong predictor of overweight and obesity (OR-4.27, 95% CI = 2.815–6.501, P < 0.01). Goyal et al. observed that going to school by bus/auto was associated with 2.14 times risk of developing obesity[20] while Joshi et al. reported that the mode of conveyance to school differed significantly among normal, overweight, and obese subjects.[21] Guedes et al. on multivariate analysis found 1.5 times risk of developing obesity with car being used as a mode of transport.[19] 6.2% of obese subjects were having a self-body perception of being healthy in comparison to 10.4% overweight subjects. Similarly 6.0% obese and 11.2% overweight subjects perceived themselves fat and 11.7% overweight and 4.3% obese subjects thought that they were underweight. These findings were found to be nonsignificant. Ramesh depicted in their study that among overweight subjects 14.1% perceived themselves as normal weight whereas 31.7% normal weight subjects had a perception of being obese.[22]
The strength of this study is usage of age and sex specific BMI criteria for overweight and obesity which is arguably better than criteria used by WHO for adults. The limitation of this study was that measurements of the subjects could only be performed once and it has not provided direct indication of the chronology of overweight and obesity. Another limitation is that although BMI is an inexpensive tool to categorize obesity, it cannot be compared with waist/height ratio or waist/hip ratios that are superior in ability to predict cardiovascular disease as compared to BMI or body fat percentage. The data available on overweight/obesity is patchy and it is sometimes difficult to compare food habits and lifestyle that vary across the country. However, there has been no clear cut guideline for classification of adolescent obesity and there should be a consensus among policy makers, health administrators, and clinicians. New longitudinal studies are required for estimation of adolescent overweight and obesity.
Conclusion
To conclude the prevalence of overweight and obesity is a problem of adolescent school going children in this study area which shows comparable trends with other parts of the country. Using bus as the mode of transport, not playing outdoor games, and sibling count more than two are independent predictors for being overweight and obesity. School-based programs for lifestyle and behavioral modification, motivation of school teachers, active participation in sports irrespective of the gender, regular anthropometric examinations of students in schools and sensitization of parents are some of the remedial measures to curb this rising menace.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.World Health Organization Controlling the global obesity pandemic (document on the internet) [Last accessed on 2014, Jul 17]. Available from: http://www.who.int/nutrition/topics/obesity/en/
- 2.Popkin BM. The nutrition transition and obesity in the developing world. J Nutr. 2001;131:871–3. doi: 10.1093/jn/131.3.871S. [DOI] [PubMed] [Google Scholar]
- 3.Lobstein T, Baur L, Uauy R. Report to the WHO. London: IASO International Obesity Task Force; 2004. Obesity in children and young people: A crisis in public health. [DOI] [PubMed] [Google Scholar]
- 4.Martorell R, KettelKhan L, Hughes ML, Grummer-Strawn LM. Overweight and obesity in preschool children from developing countries. Int J Obes Relat Metab Disord. 2000;24:959–67. doi: 10.1038/sj.ijo.0801264. [DOI] [PubMed] [Google Scholar]
- 5.Pouliot MC, Després JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: Best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73:460–8. doi: 10.1016/0002-9149(94)90676-9. [DOI] [PubMed] [Google Scholar]
- 6.Kissebah AH, Vydelingum N, Murray R, Evans DJ, Hartz AJ, Kalkhoff RK, et al. Relation of body fat distribution to metabolic complications of obesity. J Clin EndocrinolMetab. 1982;54:254–60. doi: 10.1210/jcem-54-2-254. [DOI] [PubMed] [Google Scholar]
- 7.de Onis M, Blössner M. Prevalence and trends of overweight among preschool children in developing countries. Am J Clin Nutr. 2000;72:1032–9. doi: 10.1093/ajcn/72.4.1032. [DOI] [PubMed] [Google Scholar]
- 8.Raj M, Sundaram KR, Paul M, Deepa AS, Kumar RK. Obesity in Indian children: Time trends and relationship with hypertension. Natl Med J India. 2007;20:288–93. [PubMed] [Google Scholar]
- 9.Styne DM. Childhood and adolescent obesity. Prevalence and significance. Pediatr Clin North Am. 2001;48:823–854. doi: 10.1016/s0031-3955(05)70344-8. vii. [DOI] [PubMed] [Google Scholar]
- 10.Guo SS, Huang C, Maynard LM, Demerath E, Towne B, Chumlea WC, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: The Fels longitudinal study. Int J Obes Relat Metab Disord. 2000;24:1628–35. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 11.Kaur S, Kapil U, Singh P. Pattern of chronic diseases amongst adolescent obese children in developing countries. Curr Sci. 2005;88:1052–6. [Google Scholar]
- 12.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ. 2000;320:1240–3. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta M, Bhasin SK, Agrawal K, Dwivedi S. Obesity amongst affluent adolescent girls. Indian JPediatr. 2007;74:619–22. doi: 10.1007/s12098-007-0109-8. [DOI] [PubMed] [Google Scholar]
- 14.Sharma A, Sharma K, Mathur KP. Growth pattern and prevalence of obesity in affluent schoolchildren of Delhi. Public Health Nutr. 2007;10:485–91. doi: 10.1017/S1368980007223894. [DOI] [PubMed] [Google Scholar]
- 15.Laxmaiah A, Nagalla B, Vijayaraghavan K, Nair M. Factors affecting prevalence of overweight among 12- to17-years-old urban adolescents in Hyderabad, India. Obesity (Silver Spring) 2007;15:1384–90. doi: 10.1038/oby.2007.165. [DOI] [PubMed] [Google Scholar]
- 16.Kumari DJ, Krishna BS. Prevalence and risk factors for adolescents (13-17 years):Overweight and obesity. CurrSci. 2011;100:373–7. [Google Scholar]
- 17.Singh MS, Devi RK. Nutritional status among the urban Meitei children and adolescents of Manipur, Northeast India. J Anthropol. 2013;1:1–5. [Google Scholar]
- 18.Padez C, Mourão I, Moreira P, Rosado V. Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr. 2005;94:1550–7. doi: 10.1080/08035250510042924. [DOI] [PubMed] [Google Scholar]
- 19.Guedes DP, Rocha GD, Silva AJ, Carvalhal IM, Coelho EM. Effects of social and environmental determinants on overweight and obesity among Brazilian schoolchildren from a developing region. Rev Panam Salud Publica. 2011;30:295–302. [PubMed] [Google Scholar]
- 20.Goyal JP, Kumar N, Parmar I, Shah VB, Patel B. Determinants of overweight and obesity in affluent adolescent in Surat City, South Gujarat region, India. Indian J Community Med. 2011;36:296–300. doi: 10.4103/0970-0218.91418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joshi M, Gumashta R, Kasturwar NB, Deshpande A. Avoid junk food and start cycling to school: An easy way to manage adolescent obesity. Int J Pharm Biol Sci. 2012;4:21–7. [Google Scholar]
- 22.Ramesh K. Body weight/image perceptions and prevalence of obesity among adolescents-Kerala, India. Int J Health Allied Sci. 2012;1:92–7. [Google Scholar]


