Abstract
Hypoglycemia is a common presenting feature of diabetes in the emergency department. Cardiovascular and neuroglycopenia features are well documented in the literature. We here report a case of 55-year-old female who came to our emergency with clinical features suggestive of cerebellar stroke. Laboratory investigations revealed severe hypoglycemia. The cerebellar signs and symptoms improved completely with intravenous dextrose infusion. Her MR imaging and Doppler of carotid and vertebrobasilar arteries were noncontributory. Hypoglycemia causes behavioral changes, confusion, loss of consciousness, and seizures. It is also well known to cause hemiplegia and aphasia. Hypoglycemia presenting as cerebellar stroke is rarely reported in the literature. This case highlights an uncommon manifestation of a common clinical condition. Physician must rule out hypoglycemia in every stroke patients.
Keywords: Cerebellar, hypoglycemia, hemiplegia, myelinolysis, stroke
Introduction
Hypoglycemia is defined as blood glucose level less than 70 mg/dl.[1] Its a common occurrence in diabetic patients receiving pharmacologic treatment. Transient hypoglycemia is well known to produce a stroke-like picture with hemiplegia and aphasia.[2,3,4] Hypoglycemia-induced hemiplegia usually resolves immediately with the administration of intravenous glucose. Rarely, neuroglycopenia can present as ataxia after a hypoglycemic episode, and prolonged and potentially irreversible deficits may occur.[5,6,7] We report a case of a 55-year-old female with diabetes who experienced sudden onset unilateral cerebellar symptoms during a hypoglycemic episode. Hypoglycemia presenting clinically as cerebellar stroke has not been reported in the literature. This case highlights hypoglycemia as a potential mimic for cerebellar stroke.
Case Report
A previously asymptomatic, 55-year-old diabetic female, came to our emergency with sudden onset of inability to maintain posture and impaired co-ordination in body movements for 8 h. She had difficulty in sitting upright from lying down posture and was unable to walk without support. Patient also faced difficulty in reaching objects around her. These complaints were worst at the time of onset and had slightly improved upon presentation. Patient was a known diabetic for 10 years on glibenclamide therapy at a dose of 5 mg once daily. Her glycemic status was unknown at presentation. She was not previously diagnosed or treated for hypertension, coronary artery disease, and valvular heart disease. She had no history of smoking, alcohol, or any substance abuse. On examination, the patient was conscious, alert, and afebrile with pulse rate of 108/min without any irregularity or asymmetry. There was no carotid bruit. Her blood pressure was 110/70 mmHg without any postural drop. Respiratory rate was 16/min. Patients cardiac, respiratory, and abdominal examinations were within normal limits. Her Glasgow coma scale score was 15/15. Her higher mental functions were normal with no meningeal signs. Her pupils were equal and reactive without any nystagmus. Cranial nerve, motor, and sensory examinations were normal. Patient demonstrated dysmetria on the left side in the form of past pointing on finger-nose testing and abnormal heel knee-shin test. Her gait was slow, broad based and she was able to take few steps only without support. Patient had abnormal rapid alternating movements when performed by using left hand. A provisional diagnosis of cerebellar stroke was made and a MRI of brain was requested. At this stage, bedside blood glucose was measured and it was 41 mg/dl. She was given 50 ml of 50% dextrose followed by an infusion of 10% dextrose before being shifted for imaging. On re-examination after 20 min of dextrose administration, there was complete resolution of cerebellar signs previously noted at presentation. Her repeat blood glucose was 186 mg/dl. Considering the risk of recurrent hypoglycemia due to long acting sulfonylurea, glibenclamide, the patient was observed clinically in emergency for 24 h with frequent blood glucose testing. Neurologic examination of the patient remained normal during her hospital stay and the blood glucose did not fall below 120 mg/dl. A diagnosis of hypoglycemia-induced cerebellar dysfunction was made but a possibility of a transient ischemic attack was also kept. MRI showed subtle but diffuse cerebral and cerebellar atrophic changes with no areas of infarction, hemorrhage, or demyelination [Figures 1 and 2]. Doppler study revealed no atherosclerotic plaques or luminal narrowing in vertebrobasilar or carotid arteries refuting transient ischemic attack for her cerebellar symptoms. The patient was discharged after 24 h and followed up at day 30 with no recurrence of cerebellar complaints subsequently.
Figure 1.
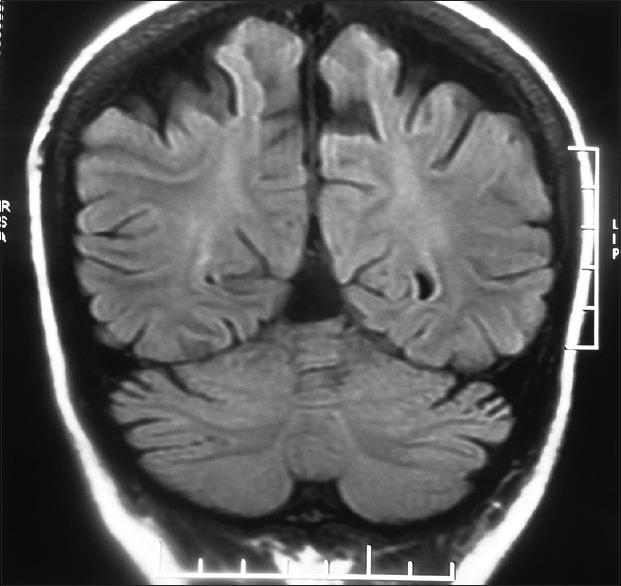
MRI brain FLAIR coronal image showing mild cerebral and cerebellar atrophy. No hematoma or infarction can be seen
Figure 2.
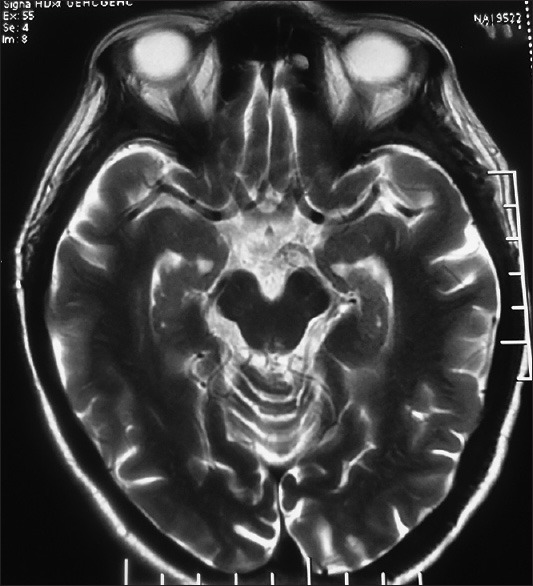
MRI brain T2 axial image showing mild atrophy bilateral cerebral hemisphere and midbrain. No infarction or hematoma can be seen
Discussion
Hypoglycemia causes behavioral changes, confusion, loss of consciousness, and seizures. It is well known to cause hemiplegia and aphasia.[2,3,4] Non-ischemic causes account for around 13% of cases with stroke-like deficits.[8] Hypoglycemia needs to be excluded in patients with clinical suspicion of suspected stroke.[9] Hypoglycemia presenting as cerebellar stroke has not been reported. Cerebellar dysfunction is a rare complication of severe hypoglycemia. The search of literature revealed cases presenting with severe hypoglycemia with significant cognitive impairment with demonstrated residual features of cerebellar dysfunction after resuscitation.[7,8] Imaging studies in these cases revealed features of pontine and extrapontine myelinolysis. Only two case reports are available in which the patients had complete resolution of cerebellar dysfunction, without any evidence of myelinolysis.[5,10] One of these patients presented with unconsciousness and subsequently developed bilateral cerebellar ataxia which persisted for few months.[5] The other patient presented with sweating, palpitations, and features of bilateral cerebellar dysfunction which resolved after 12 h.[10]
Conclusion
Hypoglycemia leading to cerebellar dysfunction is uncommon. Moreover, most of such patients had some myelination abnormalities on MR imaging. None of the reported cases suggest unilateral cerebellar dysfunction without any systemic features suggestive of hypoglycemia. Thus, this case highlights a rare manifestation of hypoglycemia and brings to the notice of the physicians that blood glucose measurement must be considered in all patients who present with features suggestive of cerebellar stroke. Prompt correction of blood glucose in hypoglycemic patients may completely resolve the symptoms and prevent further neuronal damage.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. 2003;26:1902–12. doi: 10.2337/diacare.26.6.1902. [DOI] [PubMed] [Google Scholar]
- 2.Andrade R, Mathew V, Morgenstern MJ, Roberge R, Rubin K, Senekjian D, et al. Hypoglycemic hemiplegic syndrome. Ann Emerg Med. 1984;13:529–31. doi: 10.1016/s0196-0644(84)80521-1. [DOI] [PubMed] [Google Scholar]
- 3.Ay H, Buonanno FS, Rordorf G, Schaefer PW, Schwamm LH, Wu O, et al. Normal diffusion-weighted MRI during stroke-like deficits. Neurology. 1999;52:1784–92. doi: 10.1212/wnl.52.9.1784. [DOI] [PubMed] [Google Scholar]
- 4.Wallis WE, Donaldson I, Scott RS, Wilson J. Hypoglycemia masquerading as cerebrovascular disease (hypoglycemic hemiplegia) Ann Neurol. 1985;18:510–2. doi: 10.1002/ana.410180415. [DOI] [PubMed] [Google Scholar]
- 5.Berz JP1, Orlander JD. Prolonged cerebellar ataxia: An unusual complication of hypoglycemia. J Gen Intern Med. 2008;23:103–5. doi: 10.1007/s11606-007-0407-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rajbhandari SM, Powell T, Davies-Jones GA, Ward JD. Central pontine myelinolysis and ataxia: An unusual manifestation of hypoglycaemia. Diabet Med. 1998;15:259–61. doi: 10.1002/(SICI)1096-9136(199803)15:3<259::AID-DIA548>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 7.Schwaninger M, Haehnel S, Hess K, Fohr B, Nawroth P, Hacke W. Cerebellar ataxia after repeated hypoglycemia. Eur J Neurol. 2002;9:544–5. doi: 10.1046/j.1468-1331.2002.04454.x. [DOI] [PubMed] [Google Scholar]
- 8.Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM VISION Study Group. When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke. 2008;39:1898–900. doi: 10.1161/STROKEAHA.107.497453. [DOI] [PubMed] [Google Scholar]
- 9.Furie KL, Kasner SE, Adams RJ, Albers GW, Bush RL, Fagan SC, et al. American Heart Association Stroke Council, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Interdisciplinary Council on Quality of Care and Outcomes Research. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:227–76. doi: 10.1161/STR.0b013e3181f7d043. [DOI] [PubMed] [Google Scholar]
- 10.Kim DE, Park SH, Kim SK, Nam HW, Lee YS, Chung JK, et al. Hypoglycemia-induced cerebellar dysfunction and quantitative positron emission tomography study. Neurology. 2000;55:418–22. doi: 10.1212/wnl.55.3.418. [DOI] [PubMed] [Google Scholar]


