Abstract
Malaria and dengue fever are endemic in the South-East Asian region including India. Both the illnesses share similar symptomatology, but differ in certain respects such as different- causative organisms and mosquito vector with diverse habitat. Hence, concurrent malaria and dengue fever in the same patient is said to be unusual. There have been cases of concurrent malaria and dengue, but they are scarce from highly endemic region like ours. Here, we describe three unusual cases of Plasmodium vivax and dengue co-infection diagnosed by use of rapid diagnostic tests. Early diagnosis and timely intervention is crucial in managing such patients.
Keywords: Co-infection, dengue, malaria
Introduction
Malaria and dengue fever, the two vector borne diseases, are endemic in tropical countries causing high morbidity and mortality. Co-infection with malaria and dengue infection has been described in the literature;[1,2,3] although the reports are scarce from India.[3,4,5,6] Herein, we describe three unusual cases of malaria and dengue co-infection in paediatric population.
Case 1
A 12-year-old boy presented with high-grade fever for 5 days and 2 episodes of vomiting on admission. Apart from mild periorbital puffiness, other findings were unremarkable. On admission, hemoglobin was 13 g/dl; TLC-51 × 109/L and platelet count-62 × 109/L. Peripheral blood smear (PBS) for malaria parasite was negative. Dengue NS 1 antigen (Bhat Biotech, Banglore, India) was reactive. He was treated with intravenous fluids and antipyretics. Fever continued to persist. Widal test was negative. A repeat PBS for malaria revealed Plasmodium Vivax. Fever responded to chloroquine. The patient was started on primaquine, and discharged on day 5 after normalization of platelet counts.
Case 2
A 10-year-old boy was admitted with high-grade fever, cough, and bodyache for 8 days. He was initially treated with cefpodoxime by a general practioner and referred to us with diagnosis of dengue fever (positive Dengue IgM and IgG ELISA). Other investigations disclosed hemoglobin 13.7 gm/dL, TLC 38 × 109L, platelet count 205 × 109/L and negative PBS for malaria parasite. On examination, vitals were stable; bilateral conjunctival congestion, coated tongue and a splenomegaly of 2 cm was noted.
Investigation: Hemoglobin 12.4 gm/dl; TLC 34 × 109/L, and platelet count 110 × 109/L. PBS for malaria parasite was negative. Child was treated with ceftriaxone. Widal test and blood culture was negative, but the rapid malaria antigen test (SD BIOLINE Pf/Pan test, Biostandard Diagnostic LTD, Gurgaon, India) detected Plasmodium Vivax. Child responded well to intravenous fluid therapy and chloroquine. Thrombocytopenia and leucopenia recovered within a week and he was discharged on oral primaquine.
Case 3
An 8-month-old female infant presented with 4 days of high fever, cough, and 2 days of vomiting. Infant was hemodynamically stable. Air entry was reduced on the right side of the chest. Liver was 2 cm and spleen was just palpable below costal margins. Laboratory results included: TLC 138 × 109/L, Hb 10.9 g/dl, platelet count 55 × 109/L and trophozoites of Plasmodium Vivax on PBS; aspartate transaminase 1764 U/L; alanine transminase 724 U/L; total protein 5.4 g/dl; and albumin 3.4 g/dl. Pleural effusion was noted on chest X-ray [Figure 1]. Because of thrombocytopenia and pleural effusion, possibility of dengue co-infection was considered. Dengue NS 1 antigen was positive. Infant was treated with chloroquine and appropriate fluid management. On fifth day, hemogram showed, Hb: 7.8 g/dl and rise in platelet counts to 130 × 109/L. Repeat chest X-ray showed clear costophrenic angles. Patient was discharged on the sixth day with oral primaquine and haematinics. On follow up visits, she was doing well.
Figure 1.
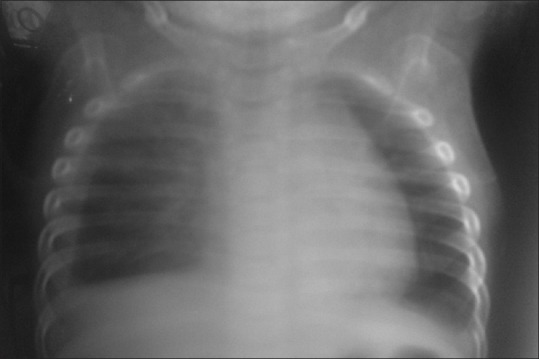
Showing right-sided pleural effusion in Case 3
Discussion
Malaria and dengue fever are prevalent in tropical countries. The probability of malaria and dengue co-infection in the same patient is still rare as both the illness differ in certain respects. Malaria, a protozoa infection, is caused by bite of Anopheles mosquito whereas dengue is a viral infection transmitted to humans by bite of infected Aedes aegypti. Dengue mosquito is considered a day-biting mosquito, while malaria is a night-biting mosquito. Dengue is more prevalent in urban areas with reservoir being stored clean water, while malaria is seen in rural areas breeding in stagnant water sources. Hence, overlapping habitat may not be easily available and concurrent infection has to be by chance.[7]
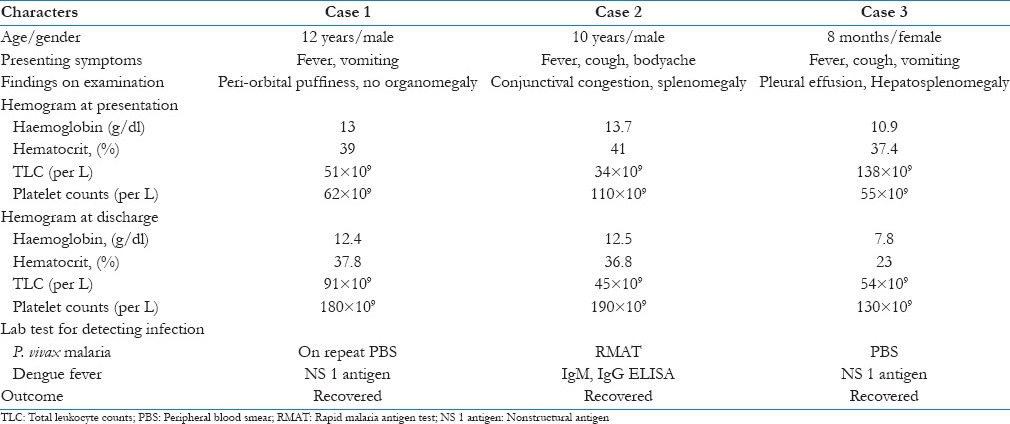
Although dengue and malaria co-infection is not a frequent occurrence, it has been seldom mentioned in the literature.[1,2,3,4,5,6] Co-infection has been reported to be more severe than single infection with severe thrombocytopenia and anaemia.[2,3] In our case series, thrombocytopenia without any bleeding manifestations was observed in all subjects. Anemia was seen in one case (Case 3). All three cases had Plasmodium Vivax malaria, but diagnosed with different microbiological laboratory tools. In Case 1, P. Vivax trophozoites were detected on repeat PBS whereas in Case 2, the same was diagnosed with the help of malaria antigen test. Table 1 outlines the summary of each case discussed.
Table 1.
Characteristics of three patients co-infected with malaria and dengue fever
Thick smear is considered a gold standard for detecting malaria parasite; however, its interpretation rely on the in hand experience of the microbiologist. Repeated blood smears are very essential to avoid false negative results and subsequent misdiagnosis of malaria. Rapid Malaria antigen test (RMAT) done by immunochromatographic methods is a rapid, qualitative differential test for detecting parasite lactate dehydrogenase (pLDH) pan specific to plasmodium species (P. vivax, Plasmodium ovale, and Plasmodium malariae) and histidine rich protein II (HRP II) specific to P. falciparum in under 20 min. Palmer et al. found that RMAT (using pLDH specific to malaria parasites) had sensitivities of 94% and 88% and specificities of 100% and 99%, respectively, when compared to traditional blood films for the detection of P. vivax and P. falciparum malaria.[8]. Combined rapid test kit for detection of non-structural protein (NS1) antigen and Dengue IgM/IgG is more useful, sensitive, and specific for the diagnosis of acute dengue infection.[9,10]
Crame et al. [1] reported the specific rate of concurrent infection of malaria and dengue from overall febrile patients equal to 0.99% that means there is high chance of malaria–dengue co-infection in South-East Asian region, including India, yet these are unusually reported. The reason may be both the illnesses present with acute febrile illness with overlapping symptoms and when one particular infection is diagnosed; the possibility of concurrent infection may not be suspected.
Clinicians in the tropical area should think of malaria–dengue co-infection whenever a patient presents with acute febrile illness, anemia and or thrombocytopenia, and there is no satisfactory response to initial treatment. Rapid diagnostic kits for detecting dengue or malaria are helpful for early diagnosis and to prevent delay in the treatment which will help in improving management of such patients. A single combined rapid diagnostic kit which will detect both dengue and malaria, with a few drops of blood, is the need of the hour.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Carme B, Matheus S, Donutil G, Raulin O, Nacher M, Morvan J. Concurrent dengue and malaria in Cayenne hospital, French Guiana. Emerg Infect Dis. 2009;15:668–71. doi: 10.3201/eid1504.080891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Epelboin L, Hanf M, Dussart P, Ouar-Epelboin S, Djossou F, Nacher M, et al. Is dengue and malaria co-infection more severe than single infections? A retrospective matched-pair study in French Guiana. Malar J. 2012;11:142. doi: 10.1186/1475-2875-11-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magalhães BM, Alexandre MA, Siqueira AM, Melo GC, Gimaque JB, Bastos MS, et al. Clinical profile of concurrent dengue fever and Plasmodium vivax Malaria in the Brazilian Amazon: Case series of 11 hospitalized patients. Am J Trop Med Hyg. 2012;87:1119–24. doi: 10.4269/ajtmh.2012.12-0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaushik RM, Varma A, Kaushik R, Gaur KJ. Concurrent dengue and malaria due to Plasmodium falciparum and P. vivax. Trans R Soc Trop Med Hyg. 2007;101:1048–50. doi: 10.1016/j.trstmh.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Mushtaq MB, Qadri MI, Rashid A. Concurrent infection with dengue and malaria: An unusual presentation. Case Rep Med 2013. 2013:520181. doi: 10.1155/2013/520181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alam A, Dm M. A case of cerebral malaria and dengue concurrent infection. Asian Pac J Trop Biomed. 2013;3:416–7. doi: 10.1016/S2221-1691(13)60087-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wiwanitkit V. Concurrent malaria and dengue infection: A brief summary and comment. Asian Pac J Trop Biomed. 2011;1:326–7. doi: 10.1016/S2221-1691(11)60053-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Palmer CJ, Lindo JF, Klaskala WI, Quesada JA, Kaminsky R, Baum MK, et al. Evaluation of the OptiMAL test for rapid diagnosis of Plasmodium vivax and Plasmodium falciparum malaria. J Clin Microbiol. 1998;36:203–6. doi: 10.1128/jcm.36.1.203-206.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arya SC, Agarwal N, Parikh SC, Agarwal S. Simultaneous detection of dengue NS1 Antigen, IgM plus IgG and Platelet Enumeration during an outbreak. Sultan Qaboos Univ Med J. 2011;11:470–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Wang SM, Sekaran SD. Early diagnosis of Dengue infection using a commercial Dengue Duo rapid test kit for the detection of NS1, IGM, and IGG. Am J Trop Med Hyg. 2010;83:690–5. doi: 10.4269/ajtmh.2010.10-0117. [DOI] [PMC free article] [PubMed] [Google Scholar]


