Abstract
A 74-year-old male patient with type 2 diabetes mellitus admitted to the emergency department with the complaints of progressive breathlessness, dry cough, and swollen lower extremities. Our patient had type 2 diabetes mellitus and hypertension for 3 years. His HbA1c was not within the target range so sitagliptin was added to on-going therapy. After 1 week of starting sitagliptin therapy, even though the patient had not heart failure he applied to the emergency department with a complaint of dyspnea. The cardiovascular safety and efficacy of many anti-hyperglycemic agents such as sitagliptin, saxagliptin are unclear. Our case has shown that dipeptidyl peptidase 4 inhibitors may cause pulmonary edema. Hence, it should be used with cautious, especially in patients with heart failure.
Keywords: Dipeptidyl peptidase 4 inhibitor, heart failure, pulmonary edema, sitagliptin
Introduction
We don’t know that what the new anti-diabetic agents’ long-term or unknown rare side-effects are on patients. By the time, we will be experienced their rare or long-term side-effects together. In this case, we aim to make health care providers alert to focus on a possible side effect of sitagliptin that may lead to noncardiac pulmonary edema. O2 saturation detected by pulse oximetry before starting the treatment was about 80%. The rest of the physical examination was normal. In the emergency department, the administration of oxygen therapy, inhalation of beta agonist and intravenous furosemide infusion was started quickly. During follow-up of the patient, his symptoms improved by the treatment. After few hours, his complaints remarkably decreased.
Case Report
A 74-year-old male patient with type 2 diabetes mellitus admitted to the emergency department with the complaints of progressive breathlessness, dry cough and swollen lower extremities. Our patient had type 2 diabetes mellitus and hypertension for 3 years. He was taking acarbose 50 mg 3 times a day and telmisartan hydrochlorothiazide 80/12.5 mg once a day. The patient had metformin intolerance so he was given acarbose. His HbA1c was not within the target range so sitagliptin was added to ongoing therapy. After 1 week of starting sitagliptin therapy even though the patient had not heart failure he applied to the emergency department with a complaint of dyspnea. In the admission he had severe dyspnea and lower extremity edema. Physical examination revealed bibasilar lung crackles, ++/++ pretibial edema, arterial blood pressure of 120/80 mmHg, heart rate of 120 pulse/min and respiratory rate of 30/min. O2 saturation detected by pulse oximetry before starting the treatment was about 80%. The rest of the physical examination was normal. In the emergency department the administration of oxygen therapy, inhalation of beta agonist and intravenous furosemide infusion was started quickly. Chest X-ray revealed bibasilar pulmonary edema [Figure 1].
Figure 1.
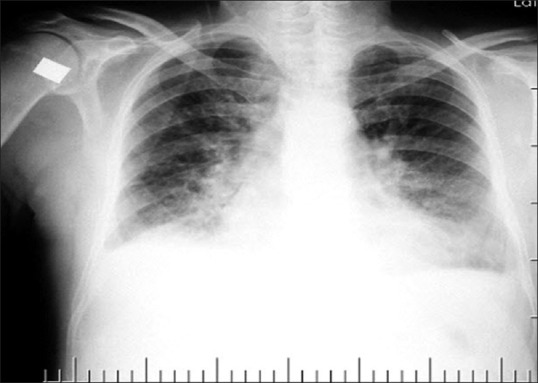
Chest X-ray
During follow-up of the patient, his symptoms improved by the treatment. After few hours his complaints remarkably decreased. The re-evaluation after the treatment revealed mild bibasilar crackles and pretibial edema. In addition, O2 saturation detected by pulse oximetry was about 99%. The patient refused hospitalization so we decided to discharge him. The patient applied to us after 3 days. He stopped taking sitagliptin for 3 days. He had not any complaint. His physical examination was normal. Fasting plasma glucose was 231 mg/dl and the remaining laboratory parameters were normal.
Discussion
Cardiogenic or noncardiogenic pulmonary edema is a condition that is associated with high morbidity and mortality. Acute respiratory distress syndrome, high altitude pulmonary edema, disseminated intravascular coagulopathy, smoke inhalation, head trauma, overwhelming sepsis, hypovolemia shock, near-drowning and many drugs (ranging from illegal drugs such as heroin and cocaine to aspirin and chemotherapy drugs) are known to cause noncardiac pulmonary edema.[1,2,3] We ruled out them for our patient. There was not any known cause of pulmonary edema except sitagliptin. Naranjo probability scale of our patient was seven and we thought that it was probably an adverse drug reaction. So we told the patient to stop taking sitagliptin and recalled him for re-evaluation after few days.
The cardiovascular safety and efficacy of many anti-hyperglycemic agents are unclear. Previous study reported that another dipeptidyl peptidase 4 (DPP-4) inhibitors saxagliptin increased the rate of hospitalization for diabetic patients with heart failure.[4] Furthermore, there is an eHealthMe document which shows us that the sitagliptin is also one of the causes of noncardiac pulmonary edema. 17,872 people reported to have side effects when taking sitagliptin. Among them, 7 people (0.04%) have noncardiogenic pulmonary edema.[5] Our case and a previous study have shown that DPP-4 inhibitors may cause pulmonary edema. Hence, it should be used with cautious especially in patients with heart failure.
Conclusion
Pulmonary edema is one of the sitagliptin rare and serious side effect. If a patient admit an emergency unit with severe dyspnea, the physician should ask if it is related with the sitagliptin or not.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Sporer KA, Dorn E. Heroin-related noncardiogenic pulmonary edema: A case series. Chest. 2001;120:1628–32. doi: 10.1378/chest.120.5.1628. [DOI] [PubMed] [Google Scholar]
- 2.Heffner JE, Sahn SA. Salicylate-induced pulmonary edema. Clinical features and prognosis. Ann Intern Med. 1981;95:405–9. doi: 10.7326/0003-4819-95-4-405. [DOI] [PubMed] [Google Scholar]
- 3.Murray JF. Pulmonary edema: Pathophysiology and diagnosis. Int J Tuberc Lung Dis. 2011;15:155–60,. [PubMed] [Google Scholar]
- 4.Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–26. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 5. [Last accessed on 2014 Mar 28]. Available from: http://www.ehealthme.com/ds/januvia/increased-permeability+pulmonary+edema .


