Abstract
Purpose:
To improve resiliency and reduce burnout in nurses through implementation of the Healing Pathways program (University of Maryland School of Medicine, Baltimore). Aims of this study include assessment of feasibility and acceptability and to explore changes in stress, coping, burnout, and mindfulness.
Design:
A single-group, pre-, posttest design of an 8-week program in which participants attended weekly sessions that included Reiki, yoga, and meditation. Sample included 8 nurses with 1 advanced practice nurse, all female, ages ranging from 22 to 49 years, experience levels ranging from <1 year to 26 years.
Methods:
Participants completed the Perceived Stress Scale, Coping Self-Efficacy Scale, Maslach Burnout Inventory, and Mindful Attention Awareness Scale before intervention, at last session, and 1 month after last session. Data were analyzed using one-way analysis of variance and qualitative narrative inquiry.
Findings:
Improvements were noted in perceived stress, coping, burnout exhaustion subscale, and mindfulness.
Conclusion:
Healing Pathways was effective at reducing stress and improving coping and mindfulness in nurses.
Implications:
Nurses who invest time in self-care techniques including Reiki, yoga, and meditation improve their overall wellbeing and may provide higher-quality patient care. Implementation of an 8-week program in integrative self-care is feasible and important for the health of nurses.
Key Words: Integrative, nursing, coping, resiliency, burnout, mindfulness, Healing Pathways, Reiki, yoga, meditation
摘要
目的:为了提高灵活性,并通过 实施康复之路 (Healing Pathways)课程(巴尔的摩马里 兰大学医学院)以减轻护士的倦 怠。这项研究的目的包括:探讨 压力、应对、倦怠与专注力的变 化的可行性和可接受性的评估。
设计:单组,设计为 8 个星期的 课程前测试和课程后测试,参与 者参加每周一次的课程,包括灵 气、瑜伽和冥想。样例包括 8 名 护士与 1 名高级执业护士,均为 女性,年龄从 22 至 49 岁,经 验水平从少于 1 年到 26 年。
方法:在干预前,最后一次课程 以及最后一次课程一个月后,参 与者分别完成感知压力量表、应 对自我效能感量表、工作倦怠量 表和铭记的关注意识量表。数据 分析采用单向方差分析和定性的 叙事研究。
研究结果:在感觉到的压力、应 对、倦怠疲惫程度和专注力上有 所改善。
结论:护士在减轻压力、提高应 对和专注力方面,康复之路课程 是有效的。
意义: 护士在自我护理技术(包括灵气、瑜伽和冥想) 方面投入时间, 可以改善他们整体 的福祉且可能提供更高质量的 患者护理。 实施一体化自我护理 8 周课程对护士的健康是可行和重要的。
SINOPSIS
Propósito: Mejorar la resiliencia y reducir el desgaste en el personal de enfermería a través de la implementación del programa Healing Pathways (Caminos de cura), (University of Maryland School of Medicine, Baltimore). Los fines de este estudio incluyen la valoración de la viabilidad y aceptabilidad y la exploración de cambios en el estrés, el afrontamiento, el desgaste y la concienciación.
Diseño: Diseño de un programa de prueba anterior y posterior de 8 semanas para un único grupo en el cual los participantes asistían a sesiones semanales que incluían Reiki, yoga y meditación. La muestra incluía 8 enfermeras con una enfermera de practica avanzada, todas mujeres, con edades comprendidas entre los 22 y los 49 años, con niveles de experiencia entre <1 año y 26 años.
Métodos: Las participantes completaron la Escala de estrés percibido, la Escala de manejo de autoeficacia, el Inventario de desgaste de Maslach y la Escala de concienciación de atención consciente antes de la intervención, en la última sesión y un mes después de la última sesión. Se analizaron los datos usando un análisis de la varianza unidireccional y encuestas narrativas cualitativas.
Hallazgos: Se notaron mejoras en el estrés percibido, el afrontamiento, la subescala de agotamiento por desgaste y la concienciación.
Conclusión: Healing Pathways fue efectivo a la hora de reducir el estrés y mejorando el afrontamiento y la concienciación en las enfermeras.
Consecuencias: Las enfermeras que invirtieron tiempo en técnicas de autocuidado incluyendo Reiki, yoga y meditación mejoraron su bienestar general y pudieron proporcionar una mejor calidad en la atención al paciente. Es viable la implementación de un programa de 8 semanas de autocuidado integrador y es importante para la salud de las enfermeras.
BACKGROUND AND SIGNIFICANCE
Nurses face a variety of stressful situations in their daily work and require effective coping skills to manage stress over their careers. Stress and burnout are reported by one-quarter to one-third of nurses and have been linked to a large number of nurses leaving the bedside.1,2 Job dissatisfaction and burnout have been linked to poorer patient outcomes, lower patient satisfaction levels, higher turnover rates, on-the-job injuries, and decision to leave the bedside.2,3
Burnout is defined as a psychological syndrome with three key dimensions: overwhelming exhaustion, feelings of cynicism or detachment from the job, and a sense of ineffectiveness.4 Another form of burnout is job dissatisfaction, which is described as apathy, wanting to quit, lack of satisfaction from one's own work, and frustration, despair, or anger surrounding one's work. With burnout and job dissatisfaction being linked to nurses leaving the bedside, they may also be linked to nursing turnover. This becomes a quality and cost concern for employers.5 The financial cost of nursing turnover has been estimated at 0.3 to 3 times nurses' salaries, and rates are estimated at 14% nationally.6,7
Stress-reduction techniques including Reiki, yoga, and meditation have been shown to decrease exhaustion, improve levels of self-care and care of others, and decrease stress, fatigue, and burnout.8 Studies show that an 8-week program offering training in complementary techniques to the healthcare provider is effective for reducing stress.8,9 The purpose of this project was to improve resiliency and reduce burnout in nurses through implementation of the Healing Pathways program (University of Maryland School of Medicine, Baltimore).
Reiki
Reiki is defined as a Japanese technique for stress reduction, relaxation, and healing promotion.10 The term Reiki comes from two Japanese words: rei, meaning universal, and ki, which is the same as chi in Chinese, prana in Sanskrit, and ti or ki in Hawaiian, meaning life energy.10 The technique of Reiki involves “laying on of hands” and is learned through an apprenticeship with a Reiki master.10 The practice of Reiki is relatively new to the United States, having been brought by Hawayo Takata in 1937.10
The use of Reiki in treating nurses with stress-related problems has been documented in several studies.11-14 Diaz-Rodrigues et al found that a single Reiki session can improve immune function and blood pressure regulation.13 In a phenomenological study of 8 nurse/Reiki masters, seven themes were developed showing the benefits received by the practitioner during a Reiki client therapy session, including feeling more peaceful, calm, and relaxed; handling stress and anxiety better; helping the client's healing process; and an increased satisfaction with being a nurse/Reiki practitioner as compared with previous or present nursing work.14 Reiki level-1 training improves nurses' beliefs around their caring behaviors at the bedside.11 Additionally, Reiki level 1 is associated with reductions in work-related stress levels as measured by the Perceived Stress Scale in a pilot study.12 In several studies, reduced pain and anxiety, improved wellbeing, increased ability to focus on patients, and improved problem solving were found in association with Reiki practice.15-17
Yoga
Yoga means union, specifically of the individual soul with the universal spirit; it is also described as a means of uniting the physical, mental, and spiritual self.18 Hartfel et al describe yoga as a form of physical activity being introduced to improve health and well-being.19 Recent studies have shown yoga to be successful at reducing perceived stress, anxiety, and back pain and improving psychological wellbeing.19,20 In the CALM-BP (Comprehensive Approach to Lower Blood Pressure) study, use of yoga in combination with medication was more effective at improving blood pressure control and cardiovascular risk factors than the use of the DASH (Dietary Approaches to Stop Hypertension) diet in combination with medication.21 Additionally, onsite yoga programs at work have reduced anxiety and stress, improved fitness levels, reduced cardiovascular risk, reduced metabolic diseases, and improved heart rate variability in adults.22-24
MEDITATION
Meditation is a term used to describe various methods involving quieting of the mind and/or drawing one's focus into a particular moment, task, or object. Meditation can be practiced in different physical positions, from sitting very still in a cross-legged pose to walking or even while performing tasks such as washing dishes. The usefulness of meditation extends from increasing mindfulness (connection with the present) to stress reduction and physical wellbeing.25-29 A recent meta-analysis confirms that meditation is effective for reducing anxiety, depression, and pain, and therefore clinicians should be prepared to discuss meditation with their clients.30
STUDY DESIGN
The design of the study was a single group, pre-, posttest design of an 8-week program in which participants attended weekly sessions that included Reiki, yoga, meditation, and a reflection.
METHODS
Participants
Eight registered nurses, including 1 nurse practitioner, were recruited for the study. Participants were recruited by emailed flyers sent to the unit directors of 3 units. The unit directors sent the flyer to all the nurses on their units and posted the flyer in their unit's lounge. Approximately 175 nurses received an email for recruitment. Ten additional nurses responded but were unable to attend the program on the dates specified and were therefore excluded from the enrollment. All participants were female adults aged 22 to 49 years. The participants' nursing experience levels ranged from <1 year to 26 years. All of the study participants agreed to complete surveys before starting the program, at the end of the program, and 1 month after completion of the program. Additionally, all of the nurses recruited were working at the bedside, so it was assumed that they were fit enough to participate in yoga.
Setting
Participants were recruited at a 520-bed urban teaching hospital from three units. The units selected for this program were the emergency department, a medical intensive care unit, and an oncology unit. Sessions were held at the University of Pittsburgh Medical Center (UPMC) Center for Integrative Medicine.
Measures
The project's specific aims were measured using valid and reliable tools. Measures used in this project included the Perceived Stress Scale, the Coping Self-efficacy Scale, the Maslach Burnout Inventory, the Mindful Attention Awareness Scale (MAAS), program attendance, and a post-program qualitative survey.
The Perceived Stress Scale (PSS) is a 10-item Likert scale on which participants rated the degree to which they felt that life was manageable and their ability to cope with stressors. The scale's effectiveness and external validity has been verified.31
The Coping Self-Efficacy Scale is a 26-item scale that measures the level of confidence that respondents have in managing and responding to adverse events. This scale has been validated and shown to be reliable.32
The Maslach Burnout Inventory is a 22-question instrument that measures three dimensions: emotional exhaustion, depersonalization, and personal accomplishment. This inventory was originally validated by its authors, has been said to be the most commonly used instrument to measure burnout, and has been validated recently.33
Mindfulness is considered to be the level to which someone is attentive, aware, and conscious within the current moment. Mindfulness has been linked to positive psychological wellbeing outcomes and can be measured using the MAAS, which measures the frequency of mindful states over time.34 The MAAS is a 5-item scale that has been validated in a study by MacKillop and Anderson.35
In addition to the formal surveys, participant attendance was also measured to quantify program acceptability. It was presumed that if participants attended the program or makeup sessions, they found the program to be an acceptable form of learning and valued the techniques being taught. Participants were also given the opportunity to provide qualitative feedback in the form of an open-ended survey given at the end of the last session. The open-ended survey invited the participants to write about how the program affected them, whether it changed their outlook on nursing, and if they would recommend the program to other nurses/healthcare providers.
PROCEDURE
Prior to the start of the program, the instructor trained with the director of Healing Pathways to ensure consistency in teaching. The program was taught primarily by a registered nurse who is a registered yoga teacher (RYT 200), Reiki master, and graduate of the Healing Pathways program. Prior to initiation of the program, approval was gained from the Internal Review Board of the University of Pittsburgh, University of Pittsburgh School of Nursing, and the UPMC Quality Review Committee.
The program consisted of six 3-hour sessions and two 5-hour sessions held weekly over the course of 8 weeks. The program was conducted at the hospital campus. Each of the weekly sessions involved a 60- to 90-minute yoga practice and a 1-hour didactic component. For reinforcement, an exercise, reflection, or meditation was included. The yoga practice used various yogic asanas, or physical positions, from styles including Embodi yoga, Hatha yoga, and Raja yoga. The didactic component consisted of lectures on the 7 energetic centers of the body known as chakras. Information on the names, sounds, emotions/feelings, and reflections associated with each chakra was provided. The exercises, reflections, and meditations also reflected mental and emotional tasks to reinforce the didactic components. The two 5-hour sessions covered the content on the history and teachings of Usui Reiki Practice as is traditionally taught by a Reiki master during attunements. The first Reiki session, which was held during the third week of the program, covered Reiki level I. The second Reiki session, which was held during the sixth week of the program, covered Reiki level II.
Data Collection
Participants were given surveys to complete prior to the first session, at the end of the last session, and 1 month after the last session. All surveys were completed anonymously and tracked via a nonassociated study participant number for pre-, posttest analysis.
DATA ANALYSIS AND FINDINGS
Data were analyzed using one-way analysis of variance (ANOVA) and for qualitative narrative. Significance level was set at α=0.05. In addition, narrative feedback was gathered at the end of the intervention.
Findings
In the post-program narrative, survey participants reported themes including improved focus, increased positive feelings about nursing, feeling more peaceful/relaxed, improved wellbeing, and feeling less reactive, less anxious, and “generally happier.” In addition to this qualitative information, a quantitative analysis was performed using one-way ANOVA.
Stress scores decreased considerably from the start of the program to the 1-month post-intervention mark (P=.002; Figure 1). Coping scores improved at the end of the intervention and were maintained at the 1-month post-intervention mark (P=.000; Figure 2).
Figure 1.

Perceived Stress Scale.
Figure 2.

Coping Self-efficacy Scores.
The Maslach Burnout Inventory subscale of professional efficacy did not show a statistically significant change (P=.371; Figure 3). The subscale for exhaustion, however, showed drastic improvement at both the post-intervention and 1-month follow-up points (P=.017). The final subscale on the Maslach Burnout Inventory calculated was the cynicism scale, which showed improvement that was not statistically significant (P=.065). Mindfulness improved significantly at both the post-intervention and follow-up points (P=.026; Figure 4).
Figure 3.
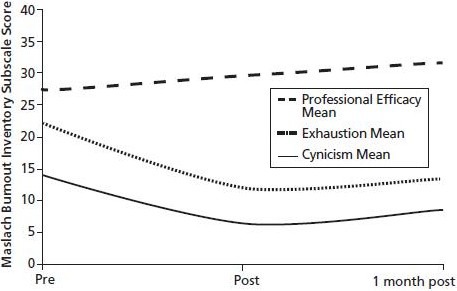
Maslach Burnout Inventory.
Figure 4.
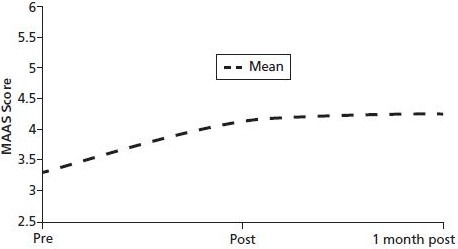
Mindful Attention Awareness Scale (MAAS).
Attendance of the program was used to address acceptability of the program. Three of the participants missed 1 session, and all but 1 of the missed sessions were made up on alternate dates. All but 1 of the participants completed the equivalent of 28 session hours, meaning the participants found this program format acceptable. In addition to an overall effect of acceptability, some general statements can be made about the data that were collected.
It was noted that 2 participants were unable to complete the 1-month post-intervention survey. A second ANOVA was run on each scale using the participants' post-intervention scores for their 1-month post-intervention score as well. This showed a change in the Maslach Burnout Inventory subscale for cynicism from insignificant to significant (P=.041). No other significant changes were noted in the data set using this method.
DISCUSSION
Participants were able to use the techniques learned to decrease their perceived stress levels and improve their coping efficacy. Improved coping scores illustrate that the nurses were able to apply the techniques learned to improve their ability to cope with daily personal and work-related stressors in a healthier manner. By reducing their perceived stress levels while improving coping, nurses may experience a higher level of wellbeing and ability to handle the difficult aspects of their nursing positions.
Improved MAAS scores indicate that the participants became more mindful during the program. Becoming more mindful indicates that participants were more aware or conscious of their state in the present moment. Increased mindfulness may be helpful in improved mental clarity, attaining calm acceptance of feelings, and increased ability to deal with unexpected situations that arise.
While most of the scores were statistically significantly improved, the professional efficacy and cynicism subscales of the Maslach Burnout Inventory were not significantly changed. It is possible that the participants were satisfied in their positions upon start of the program and therefore had limited room to improve as the mean score was relatively high. Feeling cynical indicates a general distrust of human integrity and/or sincerity. This lack of change indicates that participants' feelings about the reliability they seek in others was unchanged by participation in the program. The cynicism subscale scores were greatly reduced at the post-intervention mark but had returned toward the baseline at the 1-month post-intervention mark. This indicates that the program had some effect but the results weren't significantly changed over time. It is possible that professional events such as job changes may have skewed final results as the sample size was small. The findings of this study are of limited generalizability because of the small sample size. However, both the qualitative and the quantitative findings point toward positive implications for future use of this and similar programs.
IMPLICATIONS
In the face of a growing nursing shortage, creating resiliency in the current nursing workforce is essential. The US Centers for Disease Control and Prevention recently reported occupational stress as a job hazard, stating, “healthcare workers have higher rates of substance abuse and suicide than other professions and elevated rates of depression and anxiety linked to job stress.”36 Nurses must take action to care for themselves by reducing stress and increasing coping abilities. Reiki is a practice that can be learned and accomplished over time in varying lengths by nurses from any background. Yoga practice can also be attained through the use of regular session attendance to learn initially and then implemented as home practice. Meditation practice is a skill that, once learned, is perfected through self-practice over time. Nurses should seek out resources to help them cope with the pressures faced in day-to-day work to prevent burnout and unhealthy coping. These modalities are effective at improving resiliency through a short program that can be taught in or out of the hospital.
The cost-effectiveness of this program lies in the possibility of preventing nursing turnover and early departure from nursing careers. An original study by Aiken et al found that “burnout and dissatisfaction predict nurses' intentions to leave their current jobs within a year.”37 Additionally, reducing stress may reduce nursing turnover expenses because stress and harsh work environments are a leading cause of nurses leaving the bedside.1 Stress-related issues are a leading cause of nurses' motivation to leave and are therefore a key place to start when looking to improve staff resiliency as a cost-saving measure.
The findings from this program are limited by the small sample size. More research is needed with larger sample sizes to confirm these findings and improve generalizability. These modalities are safe and affordable to implement, may greatly improve the lives of nurses, and should therefore be considered for use by nurses seeking to improve their self-care regimen along with nursing units looking to improve nurses' coping and resiliency.
Acknowledgments
The authors would like to thank Tanya Bayne, Cortney Seltman, Monica Gaydos, and Lisa Clark for their work as teachers and for their never-ending encouragement. In addition, thank you to Dr Sandy Rader, Sharon Hanchett, Denise Abernethy, Patricia Macara, Lenore Costello, and Karen Henerey for their support in implementation of the project. A special acknowledgement to Jeanette Adams, Dr Ronald Glick, and the UPMC Center for Integrative Medicine for lending us their classroom and expertise.
Disclosures The authors completed the ICMJE Form for Disclosure of Potential Conflicts of Interest and had no conflicts to disclose.
Contributor Information
Stephanie Deible, University of Pittsburgh School of Nursing, Pennsylvania (Ms Deible), United States.
Marie Fioravanti, University of Pittsburgh School of Nursing, Pennsylvania (Ms Fioravanti), United States.
Bonnie Tarantino, University of Maryland Center for Complementary Medicine, Baltimore (Ms Tarantino), United States.
Susan Cohen, University of Pittsburgh School of Nursing, Pennsylvania (Dr Cohen), United States.
REFERENCES
- 1.US Department of Health and Human Services Health Resources and Services Administration. Findings from the 2008 National Sample Survey of Registered Nurses, 2010. http://bhpr.hrsa.gov/healthworkforce/rnsurveys/rnsurveyfinal.pdf AccessedNovember19, 2014.
- 2.McHugh MD, Kutney-Lee A, Cimiotti JP, Sloane DM, Aiken LH. Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff (Millwood). 2011;30(2):202–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vecchio N, Scuffham PA, Hilton MF, Whiteford HA. Work-related injury in the nursing profession: an investigation of modifiable factors. J Adv Nurs. 2011;67(5):1067–78. [DOI] [PubMed] [Google Scholar]
- 4.Maslach C, Shaufeli W, Leiter M. Job burnout. Ann Rev Psychol. 2001;52: 397–422. [DOI] [PubMed] [Google Scholar]
- 5.Jones CB. The costs of nurse turnover: part 1: an economic perspective. J Nurs Adm. 2004;34(12):562–70. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Jones CB. A literature review of nursing turnover costs. J Nurs Manag. 2013;21(3):405–18. [DOI] [PubMed] [Google Scholar]
- 7.Jones CB. The costs of nurse turnover, part 2: application of the Nursing Turnover Cost Calculation Methodology. J Nurs Adm. 2005;35(1):41–9. [DOI] [PubMed] [Google Scholar]
- 8.Tarantino B, Earley M, Audia D, D'Adamo C, Berman B. Qualitative and quantitative evaluation of a pilot integrative coping and resiliency program for healthcare professionals. Explore (NY). 2013;9(1):44–7. [DOI] [PubMed] [Google Scholar]
- 9.Goodman MJ, Schorling JB. A mindfulness course decreases burnout and improves well-being among healthcare providers. Int J Psychiatry Med. 2012;43(2):119–28. [DOI] [PubMed] [Google Scholar]
- 10.Rand W. Reiki: the healing touch first and second degree manual. Southfield, MI: Vision Publications; 1991. [Google Scholar]
- 11.Brathovde A. A pilot study: Reiki for self-care of nurses and health care providers. Holist Nurs Pract. 2006;20(2):95–101. [DOI] [PubMed] [Google Scholar]
- 12.Cuneo CL, Curtis Cooper MR, Drew CS, et al. The effect of Reiki on work-related stress of the registered nurse. J Holist Nurs. 2011;29(1):33–43. [DOI] [PubMed] [Google Scholar]
- 13.Díaz-Rodríguez L, Arroyo-Morales M, Cantarero-Villanueva I, Férnandez-Lao C, Polley M, Fernández-de-las-Peñas C. The application of Reiki in nurses diagnosed with Burnout Syndrome has beneficial effects on concentration of salivary IgA and blood pressure. Rev Lat Am Enfermagem. 2011;19(5):1132–8. [DOI] [PubMed] [Google Scholar]
- 14.Whelan KM, Wishnia GS. Reiki therapy: the benefits to a nurse/Reiki practitioner. Holist Nurs Pract. 2003;17(4):209–17. [DOI] [PubMed] [Google Scholar]
- 15.Bowden D, Goddard L, Gruzelier J. A randomised controlled single-blind trial of the efficacy of Reiki at benefitting mood and well-being. Evid Based Complement Alternat Med. 2011;2011: 381862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raingruber B, Robinson C. The effectiveness of Tai Chi, Yoga, meditation, and Reiki healing sessions in promoting health and enhancing problem solving abilities of registered nurses. Issues Ment Health Nurs. 2007;28(10):1141–55. [DOI] [PubMed] [Google Scholar]
- 17.Thrane S, Cohen SM. Effect of Reiki therapy on pain and anxiety in adults: an in-depth literature review of randomized trials with effect size calculations. Pain Manag Nurs. 2014February27 pii: S1524–9042(13) 00080–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iyengar B. The tree of yoga. Boston, MA: Shambhala Publications Incorporated; 1998:3–5. [Google Scholar]
- 19.Hartfiel N, Burton C, Rycroft-Malone J, et al. Yoga for reducing perceived stress and back pain at work. Occup Med (Lond). 2012;62(8):606–12. [DOI] [PubMed] [Google Scholar]
- 20.Köhn M, Persson Lundholm U, Bryngelsson IL, Anderzén-Carlsson A, Westerdahl E. Medical yoga for patients with stress-related symptoms and diagnoses in primary health care: a randomized controlled trial. Evid Based Complement Alternat Med. 2013;2013: 215348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ziv A, Vogel O, Keret D, et al. Comprehensive Approach to Lower Blood Pressure (CALM-BP): a randomized controlled trial of a multifactorial lifestyle intervention. J Hum Hypertens. 2013;27(10):594–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cheema BS, Houridis A, Busch L, et al. Effect of an office worksite-based yoga program on heart rate variability: outcomes of a randomized controlled trial. BMC Complement Altern Med. 2013;13: 82 doi:10.1186/1472-6882-13-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheema BS, Marshall PW, Chang D, Colagiuri B, Machliss B. Effect of an office worksite-based yoga program on heart rate variability: a randomized controlled trial. BMC Public Health. 2011July20; 11: 578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papp ME, Lindfors P, Storck N, Wändell PE. Increased heart rate variability but no effect on blood pressure from 8 weeks of hatha yoga—a pilot study. BMC Res Notes. 2013February11; 6: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bhasin MK, Dusek JA, Chang B, et al. Relaxation response induces temporal transcriptome changes in energy metabolism, insulin secretion and inflammatory pathways. PLOS One. 2013;8(5):e62817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edenfield TM, Saeed SA. An update on mindfulness meditation as a self-help treatment for anxiety and depression. Psychol Res Behav Manag. 2012;5: 131–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoge EA, Bui E, Marques L, et al. Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. J Clin Psychiatry. 2013;74(8):786–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martín-Asuero A, García-Banda G. The Mindfulness-based Stress Reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span J Psychol. 2010;13(2):897–905. [DOI] [PubMed] [Google Scholar]
- 29.Praissman S. Mindfulness-based stress reduction: a literature review and clinician's guide. J Am Acad Nurse Pract. 2008;20(4):212–6. [DOI] [PubMed] [Google Scholar]
- 30.Goyal M, Singh S, Sibinga EM, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. [PubMed] [Google Scholar]
- 32.Chesney MA, Neilands TB, Chambers DB, Taylor JM, Folkman S. A validity and reliability study of the coping self-efficacy scale. Br J Health Psychol. 2006;11(Pt 3):421–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach burn-out inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int J Nurs Stud. 2009;46(7):894–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84(4):822–48. [DOI] [PubMed] [Google Scholar]
- 35.MacKillop J, Anderson E. Further psychometric validation of the Mindful Attention Awareness Scale (MAAS). J Psychopathol Behav Assess. 2007;29: 289–93. [Google Scholar]
- 36.US Centers for Disease Control and Prevention. Exposure to stress: occupational hazards in hospitals. http://www.cdc.gov/niosh/docs/2008-136/ AccessedNovember20, 2014.
- 37.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288(16):1987–93. [DOI] [PubMed] [Google Scholar]


