Abstract
Background
While most motor vehicle crash (MVC)-related injuries have been decreasing, one study showed increases in MVC-related spinal fractures from 1994 to 2002 in Wisconsin. To our knowledge, no studies evaluating nationwide trends of MVC-related thoracolumbar spine injuries have been published. Such fractures can cause pain, loss of functionality or even death. If the incidence of such injuries is increasing, it may provide a motive for reassessment of current vehicle safety design.
Questions/purposes
We questioned whether the incidence of thoracolumbar spine injuries increased in the United States population with time (between 1998 and 2011), and if there was an increased incidence of thoracolumbar injuries, whether there were identifiable compensatory “trade-off injury” patterns, such as reductions in sacropelvic injuries.
Patients and Methods
Institutional review board approval was obtained for retrospective review of three national databases: the National Trauma Databank® (NTDB®), 2002–2006, National Automotive Sampling System (NASS), 2000–2011, and National Inpatient Sample (NIS), 1998–2007. In each database, the total number of MVC-related injuries and the number of MVC-related thoracolumbar injuries per year were identified using appropriate Abbreviated Injury Scale (AIS) or ICD-9 codes. Sacropelvic injuries also were identified to evaluate their potential as trade-off injuries. Poisson regression models adjusting for age were used to analyze trends in the data with time.
Results
All databases showed increases in MVC-related thoracolumbar spine injuries when adjusting for age with time. These age-adjusted relative annual percent increases ranged from 8.22% (95% CI, 5.77%–10.72%; p < 0.001) using AIS of 2 or more (AIS2 +) injury codes in the NTDB®, 8.59% (95% CI, 5.88%-11.37%; p < 0.001) using ICD-9 codes in the NTDB®, 8.12% (95% CI, 7.20%–9.06%; p < 0.001) using ICD-9 codes in the NIS, and 8.10 % (95% CI 5.00%–11.28%; p < 0.001) using AIS2+ injury codes in the NASS. As these thoracolumbar injuries have increased, there has been no consistent trend toward a compensatory reduction in terms of sacropelvic injuries.
Conclusions
While other studies have shown that rates of many MVC-related injuries are declining with time, our data show increases in the incidence of thoracolumbar injury. Although more sensitive screening tools likely have resulted in earlier and increased recognition of these injuries, it cannot be stated for certain that this is the only driver of the increased incidence observed in this study. As seatbelt use has continued to increase, this trend may be the result of thoracolumbar injuries as trade-offs for other injuries, although in our study we did not see a compensatory decrease in sacropelvic injuries. Investigation evaluating the root of this pattern is warranted.
Introduction
Since the mid-1990s, the United States has had declining rates of motor vehicle crash (MVC)-related injuries. The National Highway Traffic Safety Administration (NHTSA) reported a 23% decline in nonfatal injuries among occupants of MVCs from 1996 to 2005 [19]. Many of these improvements can be attributed to advances in motor vehicle design and the promotion of safer driving behaviors. Seatbelts have been credited with reducing the risk of fatal injury to front-seat passengers by 45% and the risk of moderate-to-critical injury by 50% [15]. This effect is augmented with appropriate deployment of front air bags [15]. Additionally, seatbelt compliance rates have increased to 82% and alcohol-related driving fatalities have decreased in recent years [15].
In contrast to these data, trauma physicians at our Level I trauma center have anecdotally noted an increase in thoracolumbar spine injuries during the same period. Likewise, one study indicated that the occurrence of spinal fractures associated with MVCs had increased in Wisconsin from 1994 to 2002 [20]. As more people survive MVCs, a wider variety of nonfatal injuries have been seen and evaluated [1, 7, 11]. When lap belts were introduced, their use was responsible for saving countless lives. However, it soon was discovered that such lap belts were associated with a constellation of abdominal and spinal injuries, termed “seatbelt syndrome.” Such injuries may serve as trade-off injuries for more severe or fatal injuries that may have occurred had the occupant not been restrained [1, 11]. Lap belts mostly have been replaced with lap-shoulder belts, which have improved efficacy compared with lap belts, especially in combination with airbag use [1]. It is possible that a new breed of trade-off injuries has developed in response to these new technologies. For example, as more individuals survive MVCs, lower extremity injuries have become more significant [7]. Conversely, more sensitive imaging, especially for the thoracic and lumbar spine, may account for increasing recognition of thoracolumbar injuries in MVC survivors [4, 8].
Given that thoracolumbar fractures cause pain, loss of functionality, or even death, it is important for the medical world to recognize if such injuries are increasing in incidence. If such a trend is discovered, it may indicate that newer vehicle safety designs such as lap-shoulder belts and airbags, while preventing other injuries, do not adequately protect against injuries of the thoracolumbar spine and may provide motive for reassessment of current vehicle safety design.
Study Questions
Has the incidence of thoracolumbar spine injuries from MVCs increased in the US population with time between 1998 and 2011? If there is an increased thoracolumbar injury incidence, are there identifiable compensatory trade-off injury patterns, such as reductions in sacropelvic injuries?
Patients and Methods
Study Design and Setting
Institutional review board approval was obtained for the retrospective analysis of deidentified patient data in three national databases: the National Trauma Databank® (NTDB®), the National Automotive Sampling System-Crashworthiness Data System (NASS-CDS), and the National Inpatient Sample (NIS).
The NTDB® is the largest aggregation of trauma registry data [5]. Data are collected from participating trauma centers on an annual basis and are rigorously examined by NTDB® administrators. We evaluated National Trauma Data Bank® Research Data System (NTDB®-RDS) version 7.1 data from admission years 2002 to 2006.
NASS-CDS contains detailed data on a representative, random sample of thousands of minor, serious, and fatal tow-away crashes in the United States. Trained crash investigators obtain data from crash sites, interview crash victims, and review medical records. Weighting factors are applied to injury data collected to create population-based estimates of the incidence of particular injuries in the United States [16]. Our study used NASS data years 2000 to 2011. NHTSA requirements for NASS-CDS crash investigations changed in 2009 and many variables, including injury data, were not collected for vehicles older than 10 years after 2009. Thus, NASS-CDS 2009 to 2011 data with such vehicles were excluded from our analysis. This resulted in exclusion of approximately 11,814 distinct occupants between 2009 and 2011.
NIS contains hospital discharge data from approximately 8 million hospital stays each year. NIS is supported by the Healthcare Cost and Utilization Project (HCUP), a project that collects data to inform decision making at the national, state, and community levels. Like NTDB®, NIS assigns weighting factors to the diagnoses to create a representative sample of disease prevalence in the United States [10]. NIS data from 1998 to 2007 were analyzed for our study.
Participants/Study Subjects
Identification of Patients with Thoracolumbar Spine Injuries
All three databases code for injuries using either the Abbreviated Injury Scale (AIS) 1990 update 98 lexicon [2] or the ICD-9 lexicon [14]. AIS codes consist of two numerical components. The first component is a six-digit injury descriptor code (“pre-dot”), that classifies the injury by anatomic region, type of anatomic structure, specific structure, and level. The second component is a severity score (“post-dot”), graded on a scale of 1 through 6, with 6 identifying the most severe injuries. Using this classification schema, occupants sustaining thoracolumbar injuries were identified as those with an AIS pre-dot first digit of 6 (indicating spine injury), and AIS pre-dot fifth and sixth digits of 04 or 06 (indicating thoracic and lumbar spine injuries, respectively). Only occupants with injuries of a post-dot severity of 2 or greater (AIS2 +) were included for analysis, as AIS1 injuries are mostly inconsequential, superficial injuries. Further evaluation of pre-dot digits allowed for separate evaluation of bony fractures. For example, AIS code 640602.3 represents a lumbar spinal cord contusion with transient neurologic signs but no fracture while AIS code 650604.3 represents a lumbar spinal cord contusion with transient neurologic signs and associated lumbar fracture.
ICD-9 codes provide nominal diagnoses for medical conditions and typically are comprised of three pre-dot and one to two post-dot digits. Pre-dot codes 805 and 806 specify fractures of the vertebral column, with post-dot digits 20 to 39 and 40 to 59 referring to thoracic and lumbar fractures, respectively. Such codes thus were used to identify thoracolumbar fractures. For example 805.2 refers to a closed fracture of a thoracic vertebra without spinal cord injury while 805.4 refers to a closed fracture of a lumbar vertebra without spinal cord injury. Pre-dot digits 847 refer to vertebral column sprains, and pre-dot digits 951 and 952 refer to cord or nerve root injury. For all pre-dot digits 847, 951, and 952, post-dot digits 1 and 2 indicate thoracic and lumbar injury, respectively. Such codes were used to identify nonbony injury of the thoracolumbar spine. The ICD-9 lexicon offers no severity coding, so all severity injuries were included.
Identification of Patients With Potential Trade-off Sacrum and Pelvis Injuries
Given the potential of energy transfer from the spine to the pelvis, injuries to the sacrum and pelvis were evaluated as potential trade-off injuries. Although these are not the only potential trade-off injuries possible, the proximity of the sacrum and pelvis to the thoracolumbar spine makes these injuries a logical choice for initial evaluation. AIS codes with pre-dot digits 8526 (indicating bony pelvic ring or sacral injury) were identified as sacropelvic injuries. As with thoracolumbar AIS codes, codes with post-dot digits of 1 were excluded. ICD-9 codes with pre-dot digits 805 and 806 paired with any post-dot digits 60 through 79 identified fracture of the sacrum or coccyx. Pre-dot digits 808 with any post-dot digit represented fracture of the pelvis.
Identification of MVC Occupants
ICD-9 external cause of injury codes (E-codes) 810–819 with a post-dot of 0 or 1 designate MVCs including drivers and passengers. Only cases with appropriate E-codes were analyzed in this study.
Description of Experiment, Treatment, or Surgery
NTDB® collects AIS and ICD-9 codes. Thus, two analyses were run. First, the total number of MVC-induced injuries that were reported in the database during each specified time as noted by ICD-9 codes was recorded. In this group, all occupants with documented thoracolumbar injuries by ICD-9 codes were identified. Next, all reported MVC-induced AIS2+ injuries in the database were recorded and in this group, all occupants with AIS2+ coded thoracolumbar injuries were identified. Year of injury and age were abstracted for all occupants.
NASS-CDS records only AIS codes, while NIS reports only ICD-9 codes. In these databases, patients were identified by AIS2+ or ICD-9 codes as appropriate. Data were collected regarding the total number of MVC-induced injuries, by year and occupant age. From these cases, all occupants with documented thoracolumbar injuries were identified.
The same methods were used to evaluate the prevalence of sacropelvic injuries in each database.
Variables, Outcome Measures, Data Sources, and Bias
The annual incidence rate of thoracolumbar injuries was calculated as the number of MVC-related AIS2+ or ICD-9 thoracolumbar injuries divided by the total number of all MVC-related AIS2+ or ICD-9 injuries in a given year. Occupant age was stratified into five groups: 0–19 years, 20–39 years, 40–59 years, 60–79 years, and 80+ years. The evaluation of annual trends in the incidence rate of MVC-related thoracolumbar injuries was examined, while controlling for age. Use of ICD-9 and AIS codes to identify bony fractures also allowed for subanalysis of these same trends with respect to thoracolumbar fractures.
The same process was performed to study the incidence rate of MVC-induced sacropelvic injuries across time.
Statistical Analysis, Study Size
Trends in incidence rate of MVC-related thoracolumbar and sacropelvic injuries were tested in each database using Poisson regression with a log-linear model that included age group as a covariate. Using estimates from the age-adjusted Poisson model, the relative annual percent change in incidence rate of thoracolumbar and sacropelvic injuries per year was calculated for each database. Subanalysis of trends in thoracolumbar fracture incidence rate was performed. Probability values less than 0.05 were considered significant. All statistical analyses were performed using SAS 9.3 (SAS Institute; Cary, NC, USA) and JMP Pro 10.0.0 (SAS institute).
Results
Has the Incidence Rate of Thoracolumbar Spine Injuries Increased in the United States With Time?
Evaluation of all three of the databases considered (NTDB®, NASS-CDS, and NIS) provided evidence that with the time of interest, the incidence rate of thoracolumbar injuries and thoracolumbar fractures increased.
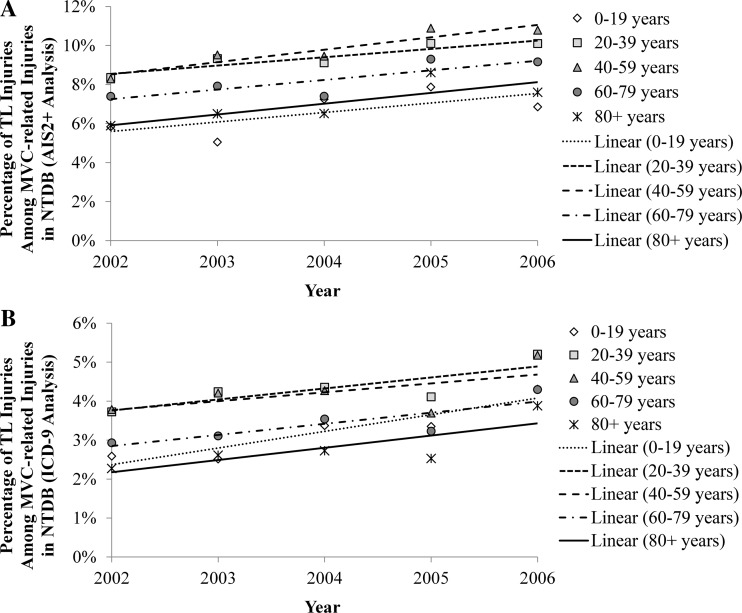
Query of the NTDB® 2002 to 2006 revealed an overall increase in the number and relative percentage of thoracolumbar injuries using AIS and ICD-9 codes (Table 1). The number of thoracolumbar AIS2+ injuries increased from 7058 in 2002 to 11,391 in 2006 (6.5% to 8.7% of all AIS2+ injuries). This trend was apparent in all age groups (Fig. 1). After controlling for age, there was an estimated 8.22% relative annual increase in incidence rate of AIS2+ thoracolumbar injuries (p < 0. 001; 95% CI, 5.77%–10.72%). Similarly, after controlling for age and excluding nonfractures, there was an estimated 8.49% relative annual increase in thoracolumbar fractures (p < 0.001; 95% CI, 6.01%–11.02%). When evaluating ICD-9-diagnosed injuries, results showed increased documentation of thoracolumbar injuries, from 10,533 such injuries in 2002 to 15,958 in 2006 (3.3% to 4.9% of all ICD-9 injuries), which held true for all age stratifications (Fig. 1). Adjusting for age, the estimated relative annual increase was 8.59% (p < 0.001; 95% CI, 5.88%–11.37%). After exclusion of nonfractures, the age-adjusted relative annual increase in incidence in such injuries was estimated to be 9.89% (p < 0.001; 95% CI 7.29%–12.56%) per year.
Table 1.
Comparison of Registries’ Crash Demographics
| Crash demographic | NTDB® AIS2+ | NTDB® ICD9 | NASS (AIS2+) | NIS (ICD9) |
|---|---|---|---|---|
| Number occupants injured | 348,399 | 498,064 | 24,541 | 401,221 |
| Number of injuries (AIS2+ or ICD9) among occupants | 748,406 | 1,494,076 | 7,059,057 | 13,232,777 |
| Occupant age, mean +/− SD | 35.1 +/− 20.2 years | 34.6 +/− 20.3 years | 36.5 +/− 19.2 years | 39.7 +/− 22.1 years |
| Number of occupants with thoracolumbar injuries, (%) | 42,536 (12.2%) | 38,062 (7.6%) | 2,626 (10.7%) | 39,916 (9.9%) |
| Number of thoracolumbar injuries, (%) | 65,042 (8.7%) | 60,180 (4.0%) | 465,451 (6.6%) | 238,434 (1.8%) |
| Occupant age with thoracolumbar injuries, mean +/− SD | 37.4 +/− 18.2 years | 37.07 +/− 18.52 years | 36.7 +/− 17.98 years | 39.1 +/− 19.9 years |
NTDB® = National Trauma Database®; AIS2+ = Abbreviated Injury Scale score of 2 or more; NASS = National Automotive Sampling System; NIS = National Inpatient Sample.
Fig. 1A–B.
These illustrations show the relative percent MVC-related injuries comprised of thoracolumbar injuries by year, stratified by age group in the NTDB®, by (A) AIS 2+ codes and (B) ICD-9 codes. MVC = motor vehicle crash; NTDB® = National Trauma Databank®; AIS = Abbreviated Injury Scale; TL = thoracolumbar.
Query of NASS-CDS 2000 to 2011, likewise, showed an increased incidence rate of thoracolumbar injuries with time (Table 1). From 2000 to 2011, the weighted number of AIS2+ thoracolumbar injuries recorded decreased from 774,922 to 254,856 (corresponding to exclusion of data reported in the Methods section). However, the relative percentage of thoracolumbar injuries among all AIS2+ injuries increased from 4.5% to 10.2%. This trend persisted across all age groups (Fig. 2). After adjusting for age, there was an estimated 8.10% relative increase in thoracolumbar injuries per year (p < 0.001; 95% CI, 5.00%–11.28%). After exclusion of nonfractures, NASS-CDS revealed an estimated age-adjusted 8.05% relative annual increase in thoracolumbar fractures (p < 0.001; 95% CI, 4.93%–11.26%).
Fig. 2.
The relative percent of all AIS 2+ MVC-related injuries comprised of thoracolumbar injuries by year in the NASS-CDS, stratified by age group, is shown. Weighted data are reported. TL = thoracolumbar; MVC = motor vehicle crash; NIS = National Inpatient Sample.
Finally, query of the NIS 1998 to 2007 showed similarly increasing trends in thoracolumbar injuries with time (Table 1).
From 1998 to 2007, there was an increase in thoracolumbar injuries from 19,836 to 29,428 (1.3% to 2.4% of all MVC-related injuries). This change persisted across all age stratifications (Fig. 3), with an estimated 8.12% relative annual increase in thoracolumbar injury incidence rate after controlling for age (95% CI, 7.20%–9.06%; p < 0.0001). Similarly, after exclusion of nonfractures, there was an estimated age-adjusted 9.7% relative annual increase in thoracolumbar fractures (p < 0.001; 95% CI, 8.63%–10.8%).
Fig. 3.
The relative percent of all ICD-9 MVC-related injuries comprised of thoracolumbar injuries by year in the NIS, stratified by age group, is shown. Discharge-weighted data are reported. TL = thoracolumbar; MVC = motor vehicle crash; NASS-CDS = National Automotive Sampling System-Crashworthiness Data System; AIS2+ = Abbreviated Injury Scale of 2 or more.
If There is an Increased Thoracolumbar Injury Incidence, and Are There Identifiable Compensatory Trade-off Injury Patterns?
Evaluation of the incidence rate of sacropelvic fractures revealed mixed results across the various databases. The NASS revealed a slight decrease in the incidence rate of AIS2+ sacropelvic injuries from 2000 to 2011 with an estimated age-adjusted 3.18% relative annual decrease in incidence (p = 0.0079; 95% CI, −5.46% to −0.84%). The NTDB®, however, using the same AIS2+ criteria, showed an estimated age-adjusted 2.48% relative annual increase in such injuries from 2002 to 2006 (p = 0.033; 95% CI, 0.20%–4.81%). Use of ICD-9 codes in the NTDB® revealed no change in pelvic fracture incidence rate with time (p = 0.3572 for age-adjusted trend) but did show an estimated 7.59% age-adjusted relative annual increase in sacral fractures from 2002 to 2006 (p < 0.001; 95% CI, 4.95%–10.31%). Evaluation of the NIS showed an age-adjusted relative annual increase in pelvic fracture incidence rate of 2.69% (p < 0.001; 95% CI, 1.63%–3.74%) and an estimated age-adjusted relative annual increase in sacral fractures of 9.81% (p < 0.001; 95% CI, 8.27%–11.37%).
Discussion
With declining rates of MVC-related injuries, anecdotal observations and a state-wide analysis in Wisconsin suggest that the incidence of MVC-induced injuries comprised of thoracolumbar spine injuries is increasing [20]. Such injuries are of clinical importance as they are associated with pain, decreased function, and sometimes death. We therefore sought to evaluate national trends in thoracolumbar injury incidence rates. Using three large national databases, we identified consistent age-adjusted relative annual increases in thoracolumbar injury incidence rates, and when evaluating for compensatory reductions in sacropelvic injuries, we saw no consistent trends.
This study had several limitations imparted by the databases. First, owing to missing injury data, the NASS-CDS 2009 to 2011 cases with model year vehicles older than 10 years old were excluded from our analysis, eliminating approximately of cases during this period. This exclusion, however, affected all injuries, and, presumably the numerator and denominator of our incidence rates, thus allowing for accurate interpretation of trends. Second, the NTDB® is biased toward high acuity cases, as only designated trauma centers contribute information. However, this would not discredit our findings regarding thoracolumbar injury incidence rate in this more severely injured cohort. Third, the NTDB® and NIS do not contain crash severity data and so these factors were not controlled for. By using large representative databases, however, the probability of selection bias of only particular crash types is low. Additionally, the goal of our study was to evaluate national trends, not factors causing thoracolumbar injuries. Finally, all three databases collect information from a wide array of medical centers, likely with varying degrees of quality control. It is possible that process improvements were made in certain centers during the study to improve the detection or documentation of injuries. Such improvements could have contributed to the increased numbers of injuries reported in our databases and we have no way of knowing the extent to which process improvements could have affected our data. However, it is likely that process improvements would have improved the detection of all types of injuries and thus our investigation of the relative percentage of MVC-induced injuries comprised of thoracolumbar injuries may help to eliminate some of this bias.
This study also was restricted by the limitations of medical coding. First, particular ICD-9 and AIS2+ codes were selected to identify thoracolumbar and sacropelvic injuries. However, ICD-9 codes and AIS2+ codes are not identical. Thus, our evaluation of thoracolumbar injuries and sacropelvic injuries as identified by ICD-9 and by AIS2+ codes may represent evaluation of two heterogeneous groups of patients. Second, ICD-9 coding offers no modifier for severity of injury. Thus, the trends observed in this study may reflect injuries of relatively low clinical consequence. In databases with AIS coding, elimination of low-severity AIS1 injuries may help to eliminate some of these injuries of little consequence from our calculation and improve the likelihood that trends observed reflect clinically relevant injuries. To this point, it is reassuring that similar trends were seen with ICD-9 codes and AIS2+ codes. An additional limitation is the availability of more sensitive screening methods now commonplace in large hospitals. Several studies have shown the superiority of CT scans over plain radiographs for diagnosis of thoracolumbar fractures regarding sensitivity, cost-, and time-effectiveness [3, 9, 18]. Brown et al. [4] reported that a spiral CT scan was suitable to completely replace plain radiographs for thoracolumbar screening. Griffey et al. [8] subsequently reported that CT scan thoracolumbar reformats had completely replaced plain films for screening at their Level 1 Trauma Center. They also noted that thoracolumbar fracture screening had increased by 52% since the introduction of such reformatting techniques, without an increase in patient volume or acuity [8]. However, before the use of CT reformats, it is presumable that patients with significant thoracolumbar injuries would have had persistent symptoms prompting diagnostic tests of increased sensitivity. Thus, although early detection may have missed an injury, diagnosis likely ultimately was achieved. Therefore, although CT scans are unlikely to account for an increasing incidence of clinically significant injuries, it is almost certain that they have allowed for improved recognition of clinically insignificant thoracolumbar injuries and have contributed at least in part to the findings observed in our study. One point that is reassuring, however, is that CT scans have been commonplace at most large hospitals for thoracolumbar injury screening since the early 2000s. Our study spans multiple times beyond this, decreasing the probability that CT screening alone has produced the trends we report.
Finally, our study may be limited by our choice of compensatory injury. We chose to evaluate trends in sacropelvic injuries although many other injuries may be candidates as potential trade-off injuries. As previously stated, the relationship of the sacrum and pelvis with the thoracic and lumbar spine make injuries of these regions a logical point for initial evaluation. Other possible trade-off injuries will be evaluated in the future.
Our results showed increasing incidence of thoracolumbar injuries across three large national databases. An important impetus for this study was an article that reported increasing rates of MVC-related spinal fractures in Wisconsin [20], which is in contrast to national reports declaring consistent declines in MVC-related injuries. In this Wisconsin study, Wang et al. [20] found that after adjusting for age, seat belt use, air bag use, vehicle type, and location of crash, the odds of spinal fracture increased by 4% per year. To account for other injuries decreasing during the evaluated time, a sensitivity analysis was performed to ensure that the decreasing denominators were not driving the increasing incidence rates. Results showed that such decreases in denominators could only partially explain the increase in observed incidence rates. For instance, had the total number of thoracolumbar injuries present in the NIS remained constant (ie, no increase in the numerator) with time, the overall increase in the incidence rate during the period would have given us a relative percent change less than 18.7% based on the decrease in the denominator values. However, we observed an increase much larger than this (relative percent change of 76.1%) during this period, suggesting that the majority of the increase in incidence is attributable to an increase in the number of thoracolumbar injuries. This apparent increase in incidence is important because thoracolumbar injuries cause pain, loss of function, and sometimes death. Post et al. [17] evaluated 10-year outcomes after nonoperative, Type A spinal fractures using a VAS spine score and the Roland-Morris disability questionnaire. Both revealed diminished functional outcomes 10 years after injury and 6% of patients reported poor long-term outcomes [17]. Complementing that study, McLain [13] found that in his cohort of patients with spinal fractures treated operatively, only 54% returned to their previous level of employment without restrictions. Likewise, Defino and Canto [6] found that only 50% of patients with operatively treated thoracolumbar burst fractures were able to return to full work duty. Such studies point to the clinical significance of such injuries.
We also sought to determine whether a closely related anatomic region, the sacropelvic girdle, exhibited compensatory decreases in injury frequency as the incidence of thoracolumbar injuries increased. Increases in nonfatal injuries in exchange for decreases in more serious and fatal injuries have been seen in other settings [1, 7, 11]. In our study, however, no consistent compensatory decreasing trends were observed in sacropelvic injuries as a whole. However, when incidence of sacral and pelvis injuries could be evaluated individually (with ICD-9 coding), sacral spine injuries showed increasing trends similar to those of thoracolumbar injuries. Although we do not have sufficient data to speak to the mechanisms contributing to this trend, we can speculate that the increasing parallel trends observed with thoracolumbar and sacral fractures implicate similar mechanistic etiologies of these injuries. Likewise, the failure of sacral and pelvic ring injuries to show parallel trends may imply that different mechanisms are at play with respect to these injuries.
Although pelvic ring injuries were not definitively shown to serve as trade-off injuries, other trade-off injuries are still possible. Seatbelt use has continued to increase and new injury patterns in the postseatbelt era may not be fully appreciated. The Wisconsin-based study that showed increasing thoracolumbar injuries with time revealed that patients with such thoracolumbar injuries commonly were wearing seatbelts without airbag deployment while patients without such injuries were more likely to have been wearing seatbelts with proper airbag deployment [20]. Increasing thoracolumbar injuries then potentially could reflect anterior loads from lap-shoulder belts that result when air bags do not deploy. Just as lap belts eventually were implicated in seatbelt syndrome, lap-shoulder belts may prove to lead to new injury patterns. Likewise, continued advancements in seatbelt effectiveness, including the advent of pretensioners and load limiters, which attempt to improve belt fit and limit force on the chest, may continue to alter injury patterns [12]. Complicating this matter is the growing obesity trend in the United States, which also may lead to changing injury patterns with poorly fitting seat belts in this population.
In an era of decreasing MVC-related injuries, our study showed an apparent increasing incidence rate of thoracolumbar injuries in the United States population across three national databases. Although the improved availability, cost-effectiveness, and speed of CT scans likely has contributed to this finding, we cannot be certain that this is the only driver of the increased incidence observed in our study. In other settings, trade-offs in MVC-related injuries were observed as new safety techniques allowed for increased survival [1, 7, 11] but no such trade-offs were observed in our study. As seatbelt and airbag technologies continue to improve, thoracolumbar injuries may be trade-offs for injuries to other anatomic regions not evaluated in our study. Given that thoracolumbar spinal injuries can cause pain, loss of function, and sometimes death, further investigations should seek to discern if other types of injuries are decreasing as thoracolumbar injuries are increasing, and the mechanisms contributing to these patterns. If the mechanisms driving increases in thoracolumbar injury incidence can be uncovered, steps could be taken to improve vehicle design to mitigate these increases.
Acknowledgments
NTDB® data were provided by the Committee on Trauma, American College of Surgeons, NTDB® Version 7.1 Chicago, IL, 2007. The content reproduced from the NTDB® remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables, or figures.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was not required.
References
- 1.Abbas AK, Hefny AF, Abu-Zidan FM. Seatbelts and road traffic collision injuries. World J Emerg Surg. 2011;6:18. doi: 10.1186/1749-7922-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Association for the Advancement of Automotive Medicine. The Abbreviated Injury Scale. Available at: http://www.aaam.org/about-ais.html. Accessed January 7, 2014.
- 3.Brandt MM, Wahl WL, Yeom K, Kazerooni E, Wang SC. Computed tomographic scanning reduces cost and time of complete spine evaluation. J Trauma. 2004;56:1022–1026. doi: 10.1097/01.TA.0000124304.68584.2C. [DOI] [PubMed] [Google Scholar]
- 4.Brown CV, Antevil JL, Sise MJ, Sack DI. Spiral computed tomography for the diagnosis of cervical, thoracic, and lumbar spine fractures: its time has come. J Trauma. 2005;58:890–895; discussion 895–896. [DOI] [PubMed]
- 5.Committee on Trauma; American College of Surgeons. National Trauma Data Bank. Available at: http://www.facs.org/trauma/ntdb/index.html. Accessed July 30, 2014.
- 6.Defino HL, Canto FR. Low thoracic and lumbar burst fractures: radiographic and functional outcomes. Eur Spine J. 2007;16:1934–1943. doi: 10.1007/s00586-007-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dischinger PC, Read KM, Kufera JA, Kerns TJ, Burch CA, Jawed N, Ho SM, Burgess AR. Consequences and costs of lower-extremity injuries. Annu Proc Assoc Adv Automot Med. 2004; 48:339–353. Available at: http://www.ntis.gov. Accessed July 10, 2014. [PMC free article] [PubMed]
- 8.Griffey RT, Ledbetter S, Khorasani R. Changes in thoracolumbar computed tomography and radiography utilization among trauma patients after deployment of multidetector computed tomography in the emergency department. J Trauma. 2007;62:1153–1156. doi: 10.1097/01.ta.0000200818.58534.5a. [DOI] [PubMed] [Google Scholar]
- 9.Hauser CJ, Visvikis G, Hinrichs C, Eber CD, Cho K, Lavery RF, Livingston DH. Prospective validation of computed tomographic screening of the thoracolumbar spine in trauma. J Trauma. 2003;55:228–234; discussion 234–235. [DOI] [PubMed]
- 10.HCUP Databases. Healthcare Cost and Utilization Project (HCUP). June 2014. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://www.hcup-us.ahrq.gov/databases.jsp. Accessed July 30, 2014.
- 11.Hodson-Walker NJ. The value of safety belts: a review. Can Med Assoc J. 1970;102:391–393. [PMC free article] [PubMed] [Google Scholar]
- 12.Kahane C. Effectiveness of pretensioners and load limiters for enhancing fatality reduction by seat belts. (Report No. DOT HS 811 835). Washington DC: National Highway Traffic Safety Administration. Available at: http://www-nrd.nhtsa.dot.gov/Pubs/811835.pdf. Accessed June 27, 2014.
- 13.McLain RF. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine (Phila Pa 1976) 2004;29:470–477. doi: 10.1097/01.BRS.0000092373.57039.FC. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics (NCHS) and the Centers for Medicare and Medicaid Services. Centers for Disease Control and Prevention. The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed June 27, 2014.
- 15.National Highway Traffic Safety Administration. Traffic Safety Facts. Available at: http://www-nrd.nhtsa.dot.gov/Pubs/811172.pdf . Accessed July 30, 2014.
- 16.National Highway Traffic Safety Administration, National Automotive Sampling System (NASS). Available at: http://www.nhtsa.gov/NASS. Accessed January 7, 2014.
- 17.Post RB, van der Sluis CK, Leferink VJ, Dijkstra PU, ten Duis HJ. Nonoperatively treated type A spinal fractures: mid-term versus long-term functional outcome. Int Orthop. 2009;33:1055–1060. doi: 10.1007/s00264-008-0593-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sheridan R, Peralta R, Rhea J, Ptak T, Novelline R. Reformatted visceral protocol helical computed tomographic scanning allows conventional radiographs of the thoracic and lumbar spine to be eliminated in the evaluation of blunt trauma patients. J Trauma. 2003;55:665–669. doi: 10.1097/01.TA.0000048094.38625.B5. [DOI] [PubMed] [Google Scholar]
- 19.Starnes M. Trends in non-fatal traffic injuries: 1996–2005. National Highway Traffic Safety Administration. Available at: http://www-nrd.nhtsa.dot.gov/pubs/810944.pdf. Accessed December 18, 2013.
- 20.Wang MC, Pintar F, Yoganandan N, Maiman DJ. The continued burden of spine fractures after motor vehicle crashes. J Neurosurg Spine. 2009;10:86–92. doi: 10.3171/SPI.2008.10.08279. [DOI] [PubMed] [Google Scholar]