Abstract
We examined the hypothesis that self-compassion is associated with lower levels of stress-induced inflammation. On two consecutive days, plasma concentrations of interleukin-6 (IL-6) were assessed at baseline and at 30 and 120 minutes following exposure to a standardized laboratory stressor in a sample of 41 healthy young adults. Participants who were higher in self-compassion exhibited significantly lower day 1 IL-6 responses, even when controlling for self-esteem, depressive symptoms, demographic factors, and distress. Self-compassion was not related to day 2 IL-6 response but was inversely related to day 2 baseline IL-6 levels, and to increase in baseline IL-6 from day 1 to day 2. These findings suggest that self-compassion may serve as a protective factor against stress-induced inflammation and inflammation-related disease.
Keywords: Acute psychosocial stress, inflammation, interleukin-6, self-compassion, self-esteem
Although modern humans are spared many of the physical stressors faced by our early ancestors, such as confrontations with predators, psychosocial forms of stress are pervasive in everyday life, from social exclusion to workplace tensions and marital conflict. When chronic, these forms of stress can be damaging to physical health. As one potential pathway, psychosocial stress has been shown to elicit an inflammatory cascade similar to that elicited by illness or injury (Segerstrom & Miller, 2004; Steptoe, Hamer, & Chida, 2007). This biological response is theorized to have evolved to promote healing and prevent infection in wounds resulting from physical conflict (Dhabhar, 1998) and, some have suggested, to promote behavioral disengagement in dangerous situations (Kemeny, Gruenewald, & Dickerson, 2004). Although properly regulated inflammation is required and adaptive in certain contexts, elevated levels of inflammation can increase the risk of a range of diseases, including cardiovascular disease, cancer, and Alzheimer’s disease (e.g., Danesh et al., 2008, Ershler & Keller, 2000).
According to social self preservation theory (Dickerson, Gruenewald, & Kemeny, 2004), psychosocial stress is especially likely to elicit increased peripheral inflammation, as well as other potentially maladaptive biological responses, when it involves threats to the self encountered in social evaluative contexts. A handful of studies provide support for the link between self-threat and inflammation. In one study, participants who performed a speech and math task in front of an evaluative audience showed increases in the production of tumor necrosis factor alpha (TNF-α) following the stressor, whereas those who performed the task alone did not show this response (Dickerson, Gable, Irwin, Aziz, & Kemeny, 2009), suggesting that the presence of a socially evaluative audience was instrumental in eliciting an inflammatory response. A related study found that writing about a traumatic experience of self-blame, but not a neutral experience, led to increases in TNF-α receptor activity, especially among those participants reporting high levels of shame in response to the manipulation (Dickerson, Kemeny, Aziz, Kim, & Fahey, 2004). Trait shame has also been linked cross-sectionally to higher baseline levels of the pro-inflammatory cytokine interleukin-6 (IL-6) as well as to lower glucocorticoid inhibition of IL-6 in vitro (Rohleder, Chen, Wolf, & Miller, 2008).
The present research examined the hypothesis that self-compassion, a self-attitude that involves treating oneself with kindness and nonjudgmental understanding (Neff, 2003a), may be associated with lower stress-induced increases in inflammation. Self-compassion may reduce the extent to which a stressor is experienced as self-threatening, thereby attenuating the magnitude and duration of the corresponding inflammatory response. In support of this idea, prior research found that a self-compassion intervention reduced feelings of shame and self-criticism (Gilbert & Procter, 2006) and that self-compassionate individuals were less emotionally reactive in stressful situations than those low in self-compassion (Leary, Tate, Adams, Allen, & Hancock, 2007). No prior research, however, has examined the relationship between self-compassion and inflammatory responses to stress.
Previous research has shown that inflammation is influenced by psychological states that are related to but distinct from self-compassion. For example, a number of studies have linked positive mood to reduced inflammation (e.g., Brouwers et al., 2012; Sepah & Bower, 2009) and to healthy immune functioning more generally (for a review, see Marsland, Pressman, & Cohen, 2007). In addition, mindfulness meditation, which involves non-evaluative attention to mental processes, has been shown to reduce stress-induced inflammation in both healthy and patient populations (e.g., Creswell, et al., 2012; Rosenkranz, Davidson, MacCoon, Sheridan, Kalin, & Lutz, 2013). Meditation that focuses on increasing compassion for others has also been shown to reduce stress-inducted inflammation (Pace et al., 2009). Finally, recent research found that self-esteem was a protective factor against increases in interleukin-1 receptor antagonist (IL-1Ra) and TNF-α following acute psychosocial stress, but self-esteem was unrelated to IL-6 (O’Donnell, Brydon, Wright, & Steptoe, 2008).
Self-compassion is distinct from these related constructs in important ways. Although self-compassion may involve feelings of positive affect (i.e., compassion), these positive feelings are directed toward the self and toward the specific types of self-conscious emotions likely to arise in self-threatening situations, such as shame and humiliation (Dickerson et al., 2004). Self-compassion is also distinct from mindfulness. Whereas mindfulness involves non-judgmental observation of mental processes, self-compassion goes beyond non-judgment by involving the active expression of warmth and caring toward the self (Neff, 2003a). Some research suggests that the development of self-compassion may in fact be a key mechanism explaining the effectiveness of mindfulness-based interventions (Baer, 2010).
Finally, although self-compassion and self-esteem are both directed toward the self, they are conceptually and empirically distinct. Unlike self-esteem, self-compassion is non-evaluative: people can have compassion for themselves even if they aren’t feeling good about themselves. Self-compassion has been shown to predict more balanced emotional reactions to laboratory-based stressors compared to self-esteem, including lower levels of negative affect and more realistic self-appraisals, potentially because self-compassion is less likely than self-esteem to promote defensive self-enhancement as a means of coping with self-threat (Leary et al., 2007). Research has also shown that self-compassion is associated with greater self-worth stability (Neff & Vonk, 2009), lower narcissism (Neff, 2003b), and greater self-improvement motivation (Breines & Chen, 2012) compared to self-esteem, making it a potentially more adaptive strategy for coping with threats to the self.
Recent research suggests that self-compassion may impact physical health through a number of pathways. For example, self-compassionate people may be more motivated to take care of their health by engaging in healthy lifestyle behaviors and adhering to medical regimens (Terry & Leary, 2011). Self-compassion may also affect health more directly by affecting the degree to which acute psychosocial stressors encountered in everyday life produce elevated levels of systemic inflammation that persist over time. In other words, self-compassion may operate through biological as well as health behavioral pathways.
The goal of the current research was to examine the relationship between self-compassion and inflammatory responses to a repeated laboratory-based psychosocial stressor. The use of a repeated stressor was intended to provide a window into the types of physiological responses participants might be likely to experience in daily life when psychosocial stressors were encountered. A standardized laboratory-based stressor, the Trier Social Stress Test (TSST; Kirschbaum et al., 1993), was used to hold constant the type and degree of stress and to allow for repeated blood sampling and assessment of interleukin-6 (IL-6), a pro-inflammatory cytokine that has been shown to be sensitive to stress and also to predict long-term health outcomes (Brydon & Steptoe, 2005; Steptoe et al., 2007). It was hypothesized that participants who were higher in trait self-compassion would show lower IL-6 responses to both an initial stressor and a similar stressor repeated on the following day.
Furthermore, it was hypothesized that the relationship between self-compassion and IL-6 response would be independent of self-esteem and depressive symptoms, which have been linked to both self-compassion and inflammation in prior research (Hiles, Baker, de Malmanche & Attia, 2012; O’Donnell et al., 2008), and independent of demographic factors (i.e., age, gender, ethnicity) and body mass index (BMI). We also hypothesized that the relationship between self-compassion and inflammation would not be explained by differences in the extent to which the TSST was experienced as emotionally distressing.
Method
Participants
Data for this article were collected as part of a larger research project conducted over 2 years in which young adults (age 18–35) and older adults (age 50–65) were recruited. Participants were recruited from the Greater Boston area and the Brandeis University campus via newspaper, magazine, and facebook advertisements and received monetary compensation. In the current report we focused on the young adult participant group only (N = 45; Mean age = 21.17; SD = 3.91).
All participants underwent a brief medical and psychological screening by telephone before testing and were invited to participate only if they met a specific selection criteria: a) body mass index (BMI) within the reference range between 18 and 30 kg/m2; b) luteal phase of menstrual cycle at time of participation, for females; c) absence of psychiatric, endocrine, or cardiovascular diseases, or other specific chronic diseases; d) no intake of psychoactive drugs, beta-blockers, gonadal steroids (hormonal contraceptives), GCs; e) non-smoker, and e) no previous experience with the stress protocol.
Four participants were excluded from analyses because their baseline IL-6 scores fell at least 3 standard deviations above the mean on the first study day (n = 1) or the second study day (n = 3). Two participants did not return on day 2 due to difficult blood draws, but they are still included in analyses conducted using data from the first study day.
Participants in the final sample (N = 41) were 44% female. Fifty one percent of participants identified as White or Caucasian American, 34% as Asian or Asian American, 5% as Black or African American, and 10% as Other. BMI ranged from 19 to 30 kg/m2 (M = 24.26, SD = 3.30).
Procedure
Eligible participants were scheduled for laboratory sessions on two consecutive days. All laboratory sessions were scheduled in the afternoon (1:30pm–6:30pm) to control for circadian variation of stress hormones. Participants were instructed to refrain from eating or drinking anything but water for 1 hour before the laboratory sessions. Written informed consent was obtained prior to participation and ethical approval was granted by the Brandeis University Institutional Review Board.
Each laboratory session lasted approximately three hours and included a resting period followed by exposure to the Trier Social Stress Test (TSST), and blood draws at baseline, 30, and 120 minutes following the TSST. At the beginning of day 1, self-compassion, self-esteem, depressive symptoms, and demographic factors were assessed using self-report paper-and-pencil questionnaires. Details about these procedures are described below. Other measures not germane to the present investigation were also assessed.
Measures
Self-Compassion
At the beginning of the first study day, participants completed the 26-item Self-Compassion Scale (SCS; Neff, 2003b). The SCS includes five items related to self-kindness (e.g., “I try to be understanding and patient toward aspects of my personality I don’t like”), five reverse-scored items related to self-judgment (e.g., “I’m disapproving and judgmental about my own flaws and inadequacies”), four items related to perceptions of common humanity (e.g., “I try to see my failings as part of the human condition”), four reverse-scored items related to perceived isolation (e.g., “When I think about my inadequacies it tends to make me feel more separate and cut off from the rest of the world”), four items related to mindfulness (e.g., “When something painful happens I try to take a balanced view of the situation”), and four reverse-scored items related to over-identification with emotions (e.g., “When I’m feeling down I tend to obsess and fixate on everything that’s wrong”). Responses to the SCS were given on a 5-point scale (1 = Almost never; 5 = Almost always). The SCS has demonstrated concurrent, convergent, and discriminant validity, as well as test–retest reliability (Neff, 2003; Neff, Kirkpatrick, & Rude, 2007). In the present study, the SCS was internally consistent (α = 0.92). On average, participants reported moderate levels of self-compassion (M = 3.11; SD = 0.69).
Self-esteem
Self-esteem was assessed using the 10-item Rosenberg Self-Esteem Scale (RSE; Rosenberg, 1965). Participants rated their agreement or disagreement with ten statements (e.g., “I take a positive attitude toward myself”) on a 4-point response scale (0 = Strongly disagree; 3 = Strongly agree). Final scores are computed by averaging scores on all items after reverse scoring five items. The RSE has demonstrated reliability and validity (Blascovich & Tomaka, 1991). In the present study, the RSE was internally consistent (α = 0.83), and participants reported moderate levels of self-esteem on average (M = 2.32; SD = 0.55).
Depressive symptoms
Depressive symptoms were assessed using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). The CES-D is designed to assess depressive symptoms in the general population, making it appropriate for detecting variation in non-clinical samples. Respondents are asked to indicate how often they have felt or behaved in the stated manner over the past week, including statements such as “I felt depressed.” Ratings are made on a 4-point scale (0 = Rarely or none of the time; 3 = Most or all of the time) and final scores are computed by summing scores on all items after reverse scoring four items. The CES-D has demonstrated reliability and validity (Radloff, 1977). In the present study, the CES-D was internally consistent (α = 0.93) and average scores fell below the clinical cut-off (M = 12.82; SD = 0.55).
Body mass index (BMI)
Height and weight measurements were taken using a tape measurer and a Seca column scale. BMI was computed using the following formula: weight in kg/(height in m × height in m).
Stress induction paradigm
Acute psychosocial stress was induced using the Trier Social Stress Test (TSST; Kirschbaum et al., 1993), a widely used standardized laboratory stress paradigm. The TSST used in the present study consisted of a three minute preparation period, a five minute public speech, and a five minute mental arithmetic task in front of an audience of two judges wearing lab coats and maintaining a neutral evaluative facial expression. The public speech involved describing how one’s personality makes one qualified for a dream job and the mental arithmetic ask involved counting backwards from 2043 by increments of 17 on the first study day and from 2011 by 13 on the second study day. Participants were informed that these judges were trained in analyzing verbal and non-verbal behavior and that their performance would be videotaped. The TSST has demonstrated reliability and validity and has been shown to produce strong biological responses to stress (Dickerson & Kemeny, 2004).
Immediately following each TSST, participants rated the extent to which they felt “distressed” by the task on a 5-point scale (1 = Very slightly or not at all; 5 = Extremely). On average, participants reported feeling moderate psychological distress (day 1 M = 3.02, SD = 1.51; day 2 M = 2.59, SD = 1.19).
Blood collection and measurement of interleukin-6 (IL-6) in plasma
At baseline (pre-TSST) and 30 and 120 minutes post-TSST, whole blood was drawn using a peripheral venous catheter (BD Nexiva IV catheter, Becton-Dickinson, Franklin Lakes, NJ) and collected in Vacutainers (Becton-Dickinson, Franklin Lakes, NJ) containing EDTA as an anticoagulant. Initial placement of the catheter was followed by a resting period of 30 minutes to ensure recovery from potential stress response to catheter placement or traveling to the laboratory. Blood samples were centrifuged immediately and plasma was then aliquoted and stored at −80C.
IL-6 concentrations were determined using a commercial high-sensitivity ELISA (R&D Systems, Oxford, UK). The limit of detection for IL-6 was 0.09 pg/ml with inter- and intra-assay CVs of 9.2% and 5.3%, respectively. Specific procedures are described in detail in Rohleder et. al. (2009). IL-6 responses on both days were computed as delta scores (i.e., IL-6 levels at 120 minutes post-TSST minus IL-6 levels at pre-stress baseline). The 120 minute time point was chosen because prior research suggests that inflammation peaks approximately 2 hours following stress (von Kanel, Kudielka, Preckel, Hanebuth, & Fischer 2006). Peak levels in the present sample were consistent with this pattern.
Because IL-6 response scores on both days showed significant violations of the assumption of normality, log-10 transformations were conducted to correct negative skews. Analyses reported below using the IL-6 response variable were performed using the log-10 transformed variables. Parallel analyses performed on the untransformed variables did not differ in direction or significance level from those reported below.
Results
IL-6 response
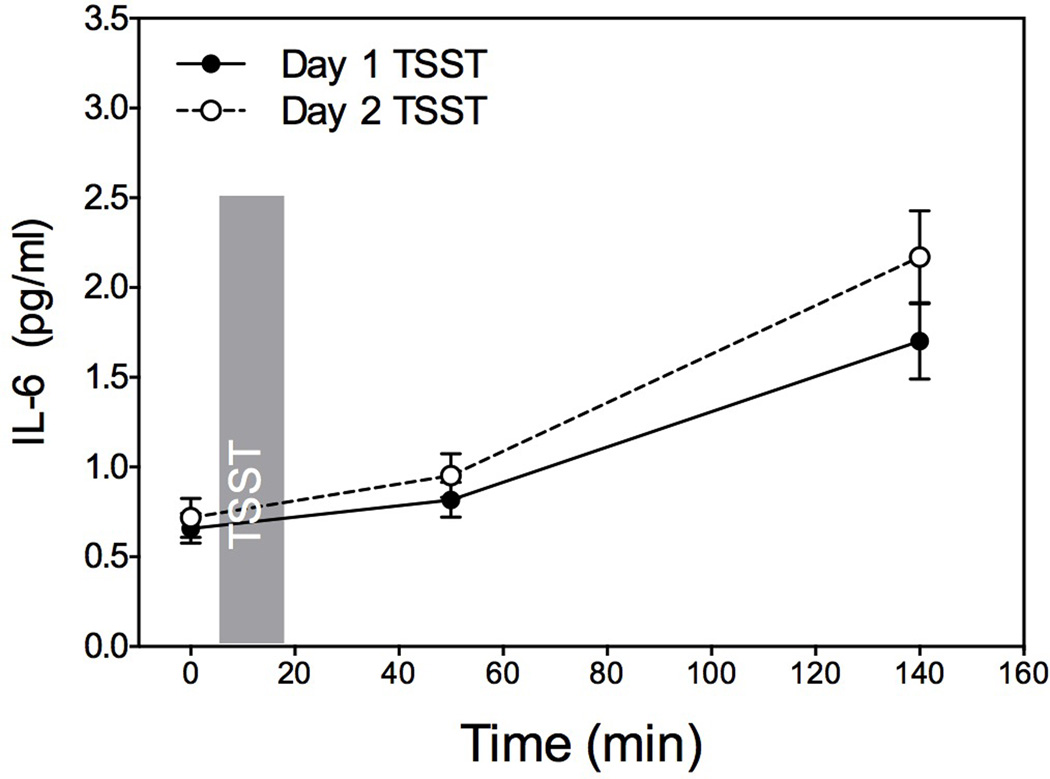
We first examined whether exposure to the TSST induced increases in circulating IL-6. Repeated measures ANOVA indicated that there was a significant effect of time for IL-6 on both day 1 and day 2, indicating that IL-6 levels increased significantly from baseline to 120 minutes following the TSST on both days: day 1 F (1, 39) = 43.64, p < 0.001; day 2 F (1, 34) = 49.01, p < 0.001. IL-6 increase did not differ significantly across days, F (1, 34) = 2.70, p = 0.11, indicating that while stress induced increases in plasma IL-6 concentrations, there was no habituation or sensitization upon repeated stress exposure, consistent with prior research (von Kanel et al., 2006). Mean IL-6 levels across the 3 time points on both days are shown in Figure 1.
Figure 1.
Mean IL-6 levels at baseline and 30 and 120 minutes post-TSST on days 1 and 2.
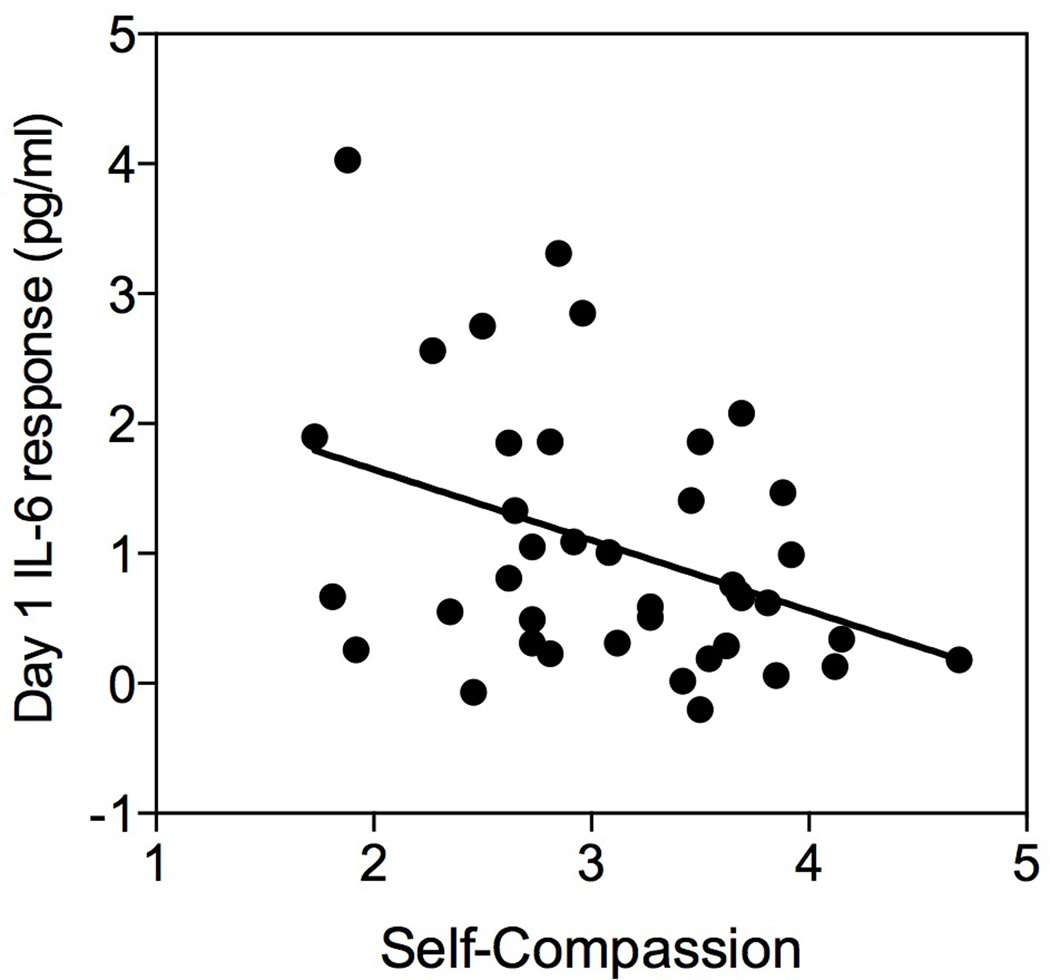
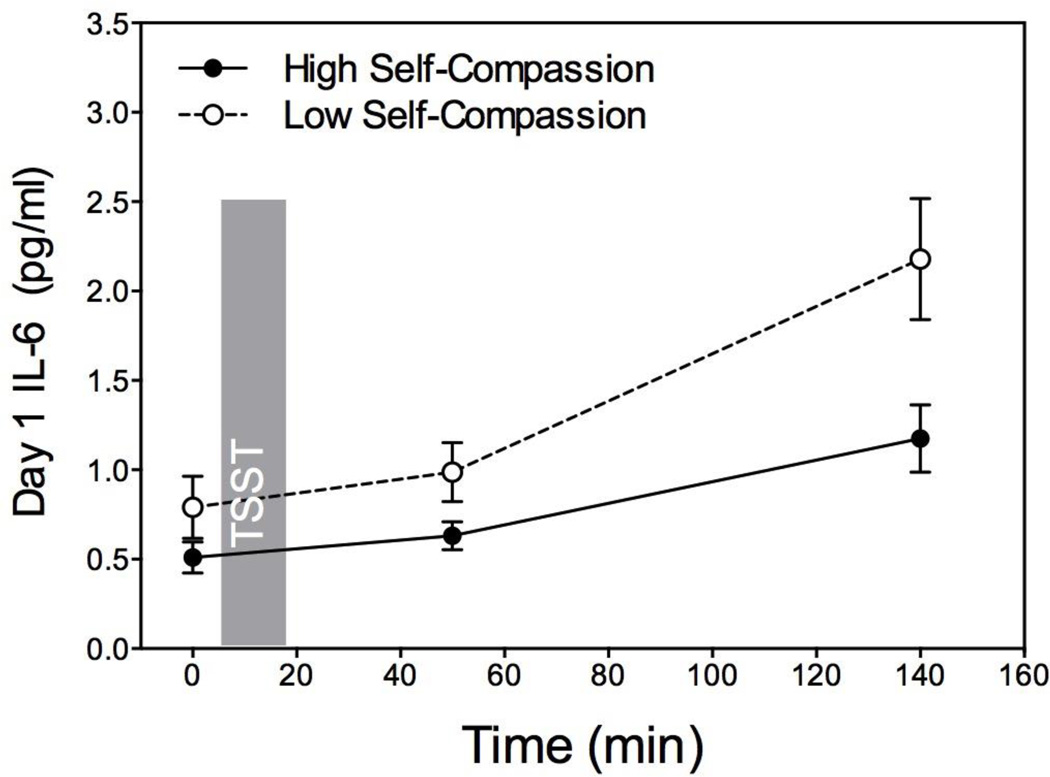
Self-compassion and day 1 IL-6 response
We next performed a series of linear regression analyses to examine whether self-compassion predicted IL-6 response on day 1. Consistent with hypotheses, self-compassion was a significant negative predictor of day 1 IL-6 response, β = −0.40, t(1, 36) = −2.61, p = 0.013, accounting for approximately 16% of the variance in IL-6 response, R2 = 0.16, F(1, 36) = 6.80, p = 0.013 (see Figures 2 and 3).
Figure 2.
Self-compassion predicting IL-6 response.
Figure 3.
Mean day 1 IL-6 levels at baseline and 30 and 120 minutes post-TSST for participants above and below the mean on self-compassion.
Covariate analyses
We next examined the alternative hypothesis that the relationship between self-compassion and day 1 IL-6 response could be due to related psychological factors (i.e., self-esteem, depressive symptoms, post-TSST distress), demographic factors (i.e., age, gender, ethnicity), temporal factors (i.e., TSST timing), or physical factors (i.e., BMI).
We first created a linear regression model where each covariate was entered simultaneously as a predictor of day 1 IL-6 response along with self-compassion. When all covariates were entered simultaneously, self-compassion remained a significant negative predictor of day 1 IL-6 response, β = −0.94, t(9, 28) = −3.31, p = 0.003. None of the covariates were significant predictors of day 1 IL-6 response (ps > 0.1), with the exception of BMI, which predicted marginally significant higher IL-6 response, β = 0.27, t(9, 28) = 1.72, p = 0.097.
To ensure that the contribution of each covariate was not masked by the presence of other covariates in the model, we also conducted a series of linear regression models for which each covariate was entered independently, along with self-compassion. In each model, self-compassion remained a significant predictor of day 1 IL-6 response (ps < 0.05), and all other predictors were non-significant (ps > 0.1).
Self-compassion and day 2 IL-6 response
We next examined whether self-compassion predicted IL-6 response on day 2. Unexpectedly, self-compassion was not a significant predictor of day 2 IL-6 response, β = 0.02, t(1, 32) = −0.08, p = 0.13, R2 = 0.001, F(1, 32) = 0.02, p = 0.88. The inclusion of covariates did not change this result.
Follow-up analyses
Self-compassion was found to predict marginally significantly lower baseline IL-6 levels on day 2, β = −0.31, t(1, 33) = −1.95, p = 0.06, and this relationship was significant when controlling for baseline IL-6 levels on day 1, β = −0.25, t(1, 32) = −2.43, p = 0.02. Self-compassion did not predict baseline IL-6 levels on day 1, β = −0.15, t(1, 38) = −0.92, p = 0.36. Analyzed another way, self-compassion was a significant negative predictor of increase in IL-6 baseline levels from day 1 to day 2, β = −0.40, t(1, 33) = −2.49, p = 0.02, suggesting that participants lower in self-compassion were more likely to show greater IL-6 baseline levels on day 2 compared to day 1. This relationship remained significant (ps < 0.05) when covariates were included, including day 2 TSST timing and day 2 post-TSST distress.
In addition, participants lower in self-compassion showed significantly greater total day 2 IL-6 output (computed as area under the curve relative to ground; Pruessner, Kirschbaum, Meinlschmid, & Hellhammer, 2003), β = −0.32, t(1, 36) = −2.03, p = 0.049, whereas self-compassion was not related to total output on day 1, β = −0.17, t(1, 39) = −1.09, p = 0.28.
Discussion
In this research we examined the role of trait self-compassion as a predictor of inflammatory responses to a repeated laboratory-based psychosocial stressor. Consistent with hypotheses, trait self-compassion was negatively related to the strength of the IL-6 response to a novel psychosocial stressor (i.e., day 1 TSST). The relationship between self-compassion and stress-induced IL-6 remained significant when controlling for self-esteem, depressive symptoms, age, gender, ethnicity, body mass index (BMI), and post-TSST distress. The inclusion of these covariates allowed us to address the alternative hypothesis that self-compassion may relate to inflammation only indirectly, through its relationship with other known correlates of stress-induced inflammation. We did not find evidence to support this alternative hypothesis.
On the second study day, however, when the TSST was repeated, self-compassion did not significantly predict IL-6 response. Follow-up analyses revealed that participants lower in self-compassion were more likely to show an increase in IL-6 baseline levels from day 1 to day 2, suggesting that a negative feedback inhibition loop may have limited the extent to which participants with high day 2 baselines could mount a strong IL-6 response on day 2. This unexpected finding also raises the possibility that the higher day 2 baselines among low self-compassion participants might reflect a carry-over of the IL-6 response from the first study day. That is, participants who were lower in self-compassion may have had IL-6 responses on day 1 that persisted until day 2 or were maintained by psychological processes such as rumination or anticipatory stress. This interpretation is purely speculative, however, and further research would be needed to examine the extended time course and recovery of stress-induced inflammation by assessing IL-6 and other inflammatory markers at regular intervals across a longer time period. Although IL-6 was assessed at two hours following stress in the present study, it may not have yet reached peak levels for many participants.
The inverse relationship between self-compassion and inflammatory responses to the novel stressor (i.e., day 1 TSST) is consistent with social self preservation theory (Dickerson et al., 2004), which highlights the critical role of threats to the self in increasing vulnerability to maladaptive biological responses to stress. While individuals experiencing high levels of shame and other negative self-directed emotions have shown greater inflammatory responses to psychosocial stress (e.g., Dickerson et al., 2004), self-compassionate individuals appear to be more protected, perhaps because they experience less of a sense of threat in these situations.
Self-compassion may be especially relevant for moderating stress-induced inflammation because of its functional similarity to perceived available social support, which has been linked to healthier immune functioning (Cohen & Wills, 1985). Researchers have posited that self-compassion, which can be seen as a form of self-directed support, may produce physiological changes that also occur in the context of social support, such as the release of the hormone oxytocin (Gilbert & Procter, 2006). Oxytocin, in turn, has been shown to play a role in reducing social threat and downregulating the stress response (Heinrichs, Baumgartner, Kirschbaum, & Ehlert, 2003).
The findings of the present research suggest that self-compassion may represent not only a protective factor against acute inflammation, but, due to the relationship between inflammation and disease (e.g., Danesh, Kaptoge, & Mann, 2008, Ershler & Keller, 2000), it may also have the potential to positively influence longer-term health outcomes. In combination with prior research, these findings help to advance our understanding of the role of psychological factors, specifically self-relevant factors, in shaping the human biological stress response, and may help to inform interventions aimed at preventing and controlling stress-related illness.
The present study has a number of limitations. First, participants were a sample of healthy young adults. It remains to be seen whether the relationship between self-compassion and stress-induced inflammation is also present in other age groups and among individuals with health problems. Second, the current study used a standardized laboratory-based stress paradigm that may not accurately reflect the types of psychosocial stressors that people are likely to encounter in their daily lives. In particular, participants were aware that they were participating in a psychology experiment and that their performance on the task would have no real consequences for them socially or professionally. Similar stressors encountered in real life, such as job interviews, may in fact elicit stronger psychological and biological responses because of their greater stakes. The development of reliable methods for assessing stress-induced inflammation in naturalistic settings outside of the laboratory would help to shed light on this issue. Third, it is important to emphasize that the presence of stress-induced inflammation at a single time point does not in itself represent health risk. Rather, it represents a snapshot of an individual’s typical response to unfamiliar psychosocial stress. The extent to which a given stress response pattern is likely to adversely impact long-term health depends in part on the frequency with which individuals a) encounter psychosocial stressors, and b) respond in maladaptive ways to such stressors, for example with shame and self-criticism rather than self-compassion, as well as other factors. Fourth, the correlational design of the present study did not permit the examination of causal hypotheses regarding the potential for self-compassion to reduce stress-induced inflammation. Experimental research is needed to examine such hypotheses.
Taken together, these findings suggest that individuals who are higher in self-compassion may be buffered from increased inflammation following unfamiliar psychosocial stress, whereas individuals who are lower in self-compassion may be especially vulnerable to the adverse effects of this form of stress. Efforts to help people cope more effectively with acute stress and reduce disease risk should seek not only to relieve negative emotions and appraisals but also to foster positive emotional states such as self-compassion.
Acknowledgements
We would like to thank the numerous research assistants in the Health Psychology Laboratory at Brandeis University who assisted with data collection.
Funding
This work was supported by a research grant from the American Federation of Aging Research.
References
- Baer RA. Self-compassion as a mechanism of change in mindfulness- and acceptance-based treatments. In: Baer RA, Baer RA, editors. Assessing mindfulness and acceptance processes in clients: Illuminating the theory and practice of change. Oakland, CA: New Harbinger Publications; 2010. pp. 135–153. [Google Scholar]
- Blascovich J, Tomaka J. Measures of self-esteem. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes, Volume I. San Diego, CA: Academic Press; 1991. [Google Scholar]
- Breines JG, Chen S. Self-compassion increases self-improvement motivation. Personality and Social Psychology Bulletin. 2012 doi: 10.1177/0146167212445599. [DOI] [PubMed] [Google Scholar]
- Brouwers CJ, Mommersteeg PMC, Nyklicek I, Pelle AJM, Westerhuis BLWJJM, Szabó BM, Denollet J. Positive affect dimensions and their association with inflammatory biomarkers in patients with chronic heart failure. Biological Psychology. 2012;92(2):220–226. doi: 10.1016/j.biopsycho.2012.10.002. [DOI] [PubMed] [Google Scholar]
- Brydon L, Steptoe A. Stress-induced increases in interleukin-6 and fibrinogen predict ambulatory blood pressure at 3-year follow up. Journal of Hypertension. 2005;23(5):1001–1007. doi: 10.1097/01.hjh.0000166841.57474.d0. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychological Bulletin. 98:310–357. [PubMed] [Google Scholar]
- Creswell JD, Irwin MR, Burklund LJ, Lieberman MD, Arevalo J, Ma J, Breen E, Cole S. Mindfulness-Based Stress Reduction training reduces loneliness and pro inflammatory gene expression in older adults: a small randomized controlled trial. Brain, Behavior, & Immunity. 2012;26:1095–1101. doi: 10.1016/j.bbi.2012.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Danesh J, Kaptoge S, Mann AG, Sarwar N, Wood A, Gudnason V. Long term interleukin 6 levels and subsequent risk of coronary heart disease: two new prospective studies and a systematic review. PLoS Medicine. 2008;5(4) doi: 10.1371/journal.pmed.0050078. 0600-0610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhabar FS. Stress-induced enhancement of cell-mediated immunity. Annals of the New York Academy of Science. 1998;840:359–372. doi: 10.1111/j.1749-6632.1998.tb09575.x. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Gable SL, Irwin MR, Aziz N, Kemeny ME. Social evaluative threat and proinflammatory cytokine regulation: An experimental laboratory investigation. Psychological Science. 2009;20:1237–1244. doi: 10.1111/j.1467-9280.2009.02437.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson SS, Gruenewald TL, Kemeny ME. When the social self is threatened: Shame, physiology, and health. Journal of Personality. 2004;72(6):1192–1216. doi: 10.1111/j.1467-6494.2004.00295.x. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME, Aziz N, Kim KH, Fahey JL. Immunological effects of induced shame and guilt. Psychosomatic Medicine. 2004;66(1):124–131. doi: 10.1097/01.psy.0000097338.75454.29. [DOI] [PubMed] [Google Scholar]
- Ershler WB, Keller ET. Age-Associated Increased Interleukin-6 Gene Expression, Late-Life Diseases, and Frailty. Annual Review of Medicine. 2000;51:245–270. doi: 10.1146/annurev.med.51.1.245. [DOI] [PubMed] [Google Scholar]
- Gilbert P, Procter S. Compassionate mind training for people with high shame and self-criticism: Overview and pilot study of a group therapy approach. Clinical Psychology & Psychotherapy. 2006;13:353–379. [Google Scholar]
- Heinrichs M, Baumgartner T, Kirschbaum C, Ehlert U. Social support and oxytocin interact to suppress cortisol and subjective responses to psychosocial stress. Biological Psychiatry. 2003;54:1389–1398. doi: 10.1016/s0006-3223(03)00465-7. [DOI] [PubMed] [Google Scholar]
- Hiles SA, Baker AL, de Malmanche T, et al. A meta-analysis of differences in IL-6 and IL-10 between people with and without depression: Exploring the causes of heterogeneity. Brain, Behavior, and Immunity. 2012;26:1180–1188. doi: 10.1016/j.bbi.2012.06.001. [DOI] [PubMed] [Google Scholar]
- Kemeny ME, Gruenewald TL, Dickerson SS. Shame as the emotional response to threat to the social self: Implications for behaviour, physiology, and health. Psychological Inquiry. 2004;15:153–160. [Google Scholar]
- Kirschbaum C, Pirke K-M, Hellhammer DH. The “Trier Social Stress Test” – a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Leary MR, Tate EB, Adams CE, Allen AB, Hancock J. Self-compassion and reactions to unpleasant self-relevant events: The implications of treating oneself kindly. Journal of Personality and Social Psychology. 2007;92(5):887–904. doi: 10.1037/0022-3514.92.5.887. [DOI] [PubMed] [Google Scholar]
- Marsland AL, Pressman S, Cohen S. Positive affect and immune function. In: Ader R, editor. Psychoneuroimmunology. 4th ed. Vol. 2. San Diego, CA: Elsevier; 2007. pp. 761–779. [Google Scholar]
- Neff KD. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003a;2(2):85–102. [Google Scholar]
- Neff KD. Development and validation of a scale to measure self-compassion. Self and Identity. 2003b;2:223–250. [Google Scholar]
- Neff KD, Kirkpatrick K, Rude SS. Self-compassion and its link to adaptive psychological functioning. Journal of Research in Personality. 2007;41:139–154. [Google Scholar]
- Neff KD, Vonk R. Self-compassion versus global self-esteem: Two different ways of relating to oneself. Journal of Personality. 2009;77(1):23–50. doi: 10.1111/j.1467-6494.2008.00537.x. [DOI] [PubMed] [Google Scholar]
- O'Donnell K, Brydon L, Wright CE, Steptoe A. Self-esteem levels and cardiovascular and inflammatory responses to acute stress. Brain, Behavior, and Immunity. 2008;22:1241–1247. doi: 10.1016/j.bbi.2008.06.012. [DOI] [PubMed] [Google Scholar]
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Issa MJ, Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009;34:87–98. doi: 10.1016/j.psyneuen.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for the computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28(7):916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Rohleder N, Chen E, Wolf JM, Miller GE. The psychobiology of trait shame in young women: extending the social self preservation theory. Health Psychology. 2008;27(5):523–532. doi: 10.1037/0278-6133.27.5.523. [DOI] [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. NJ: Princeton: University Press; 1965. [Google Scholar]
- Rosenkranz M, Davidson R, MacCoon D, Sheridan J, Kalin N, Lutz A. A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain, Behavior, and Immunity. 2013;27:174–184. doi: 10.1016/j.bbi.2012.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segerstrom SC, Miller GE. Psychological stress and the human immune system: A meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepah SC, Bower JE. Positive affect and inflammation during radiation treatment for breast and prostate cancer. Brain, Behavior and Immunity. 2009;23(8):1068–1072. doi: 10.1016/j.bbi.2009.06.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Hamer M, Chida Y. The effects of acute psychological stress on circulating inflammatory factors in humans: A review and meta-analysis. Brain, Behavior, and Immunity. 2007;21:901–912. doi: 10.1016/j.bbi.2007.03.011. [DOI] [PubMed] [Google Scholar]
- Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self and Identity. 2011;10:352–362. [Google Scholar]
- von Kanel R, Kudielka BM, Preckel D, Hanebuth D, Fischer JE. Delayed response and lack of habituation in plasma interleukin-6 to acute mental stress in men. Brain, Behavior, and Immunity. 2006;20:40–48. doi: 10.1016/j.bbi.2005.03.013. [DOI] [PubMed] [Google Scholar]