Abstract
Context
Patients with high blood pressure (BP) visit a physician 4 times or more per year on average in the U.S., yet BP is controlled in only about half. Practical, robust and sustainable models are needed to improve BP control in patients with uncontrolled hypertension.
Objectives
To determine whether an intervention combining home BP telemonitoring with pharmacist case management improves BP control compared with usual care and to determine whether BP control is maintained after the intervention stops.
Design
A clinic-randomized trial with 12 months of intervention and 6 months of post-intervention follow-up.
Patients and Setting
450 adults with uncontrolled BP recruited from 14,692 patients with electronic medical records across sixteen primary care clinics in an integrated health system in Minneapolis-St. Paul, MN.
Interventions
Eight clinics were randomized to provide usual care to their patients (n = 222) and 8 were randomized to provide the telemonitoring intervention (n = 228). Intervention patients received home BP telemonitors and transmitted BP data to pharmacists who adjusted antihypertensive therapy accordingly.
Main Outcome Measures
BP control to <140/90 mm Hg (<130/80 mm Hg in patients with diabetes or kidney disease) at 6 and 12 months. Secondary outcomes were change in BP, patient satisfaction, and BP control at 18 months.
Results
At baseline, enrollees were 45% female, 82% non-Hispanic white, mean age was 61 (sd 12.0) years and mean BP was 148/85 mm Hg. BP was controlled at both 6 and 12 months in 57.2% (95% CI, 44.8% - 68.7%) of Telemonitoring Intervention patients and 30.0% (95% CI, 23.2% - 37.8%) of Usual Care patients, P=0.001. At 6 months, BP was controlled in 71.8 % (95% CI, 65.6% - 77.3%) of Telemonitoring Intervention patients and 45.2% (95% CI, 39.2% - 51.3%) of Usual Care patients, P<0.0001; at 12 months BP was controlled in 71.2% (95% CI, 62.0% - 78.9%) of Telemonitoring Intervention patients and 52.8% (95% CI, 45.4% - 60.2%) of Usual Care patients, P=0.005; and at 18 months BP was controlled in 71.8% (95% CI, 65.0% - 77.8%) of Telemonitoring Intervention patients and 57.1% (95% CI, 51.5% - 62.6%) of Usual Care patients, P=0.003. Systolic BP decreased from baseline more among Telemonitoring Intervention than Usual Care patients by 10.7 mm Hg (95% CI, 7.3-14.3) at 6 months, 9.7 mm Hg (95% CI, 6.0-13.4) at 12 months, and 6.6 mm Hg (95% CI, 2.5-10.7) at 18 months, all P<0.001. Diastolic BP decreased from baseline more among Telemonitoring Intervention than Usual Care patients by 6.0 mm Hg (95% CI, 3.4-8.6) at 6 months, 5.1 mm Hg (95% CI, 2.8-7.4) at 12 months, and 3.0 mm Hg (95% CI, -0.3-6.3) at 18 months, all P<0.001, except at 18 months.
Conclusions
Home BP telemonitoring and pharmacist case management achieved better BP control compared to usual care during 12 months of intervention, and benefits persisted for 6 months post-intervention.
Trial Registration
ClinicalTrials.gov, NCT00781365. URL: http://clinicaltrials.gov/ct2/show/NCT00781365?term=hyperlink&rank=1
Introduction
High blood pressure (BP) is the most common chronic condition for which patients see primary care physicians, affecting about 30% of U.S. adults, with estimated annual costs exceeding $50 billion.1, 2 Decades of research have shown that treatment of hypertension prevents cardiovascular (CV) events, and many well-tolerated, effective, and inexpensive drugs are readily available.3 Although BP control has improved over the past 2 decades, BP is controlled to recommended levels in only about half of American adults with hypertension.4
Many types of interventions have been tested to improve BP control. While most studies showed modest improvements in BP, recent systematic reviews summarizing more than 3 decades of inquiry concluded that the most potent methods to improve BP involve a reorganization of clinical practice and empowerment of non-physician practitioners to make changes to antihypertensive therapy.5-7 Nurses and pharmacists are both effective in team-based care for hypertension.7, 8
Home BP monitoring has also been identified as a useful adjunct to team-based care for hypertension.9 Home BP measurement predicts cardiovascular risk better than office BP measurement10 and telemonitoring eliminates underreporting of high home BP readings.11 Several recent studies suggest that a combined intervention of telemedicine with nurse- or pharmacist-led care may be effective for improving hypertension management,12-16 but none included post-intervention follow-up. Also, previous studies excluded patients with co-morbidities and more severe hypertension. The objective of HyperLink was to determine the effect and durability of home BP telemonitoring with pharmacist case management in patients representative of the range of co-morbidity and hypertension severity in typical primary care practices.
Methods
Design, Setting and Patients
The HyperLink study is a two-group clinic-randomized controlled trial conducted at HealthPartners Medical Group, a multispecialty practice in the Minneapolis-St. Paul metropolitan area that is part of an integrated health system. The trial's rationale and design have been described in detail.17 The study protocol was approved by the HealthPartners Institutional Review Board.
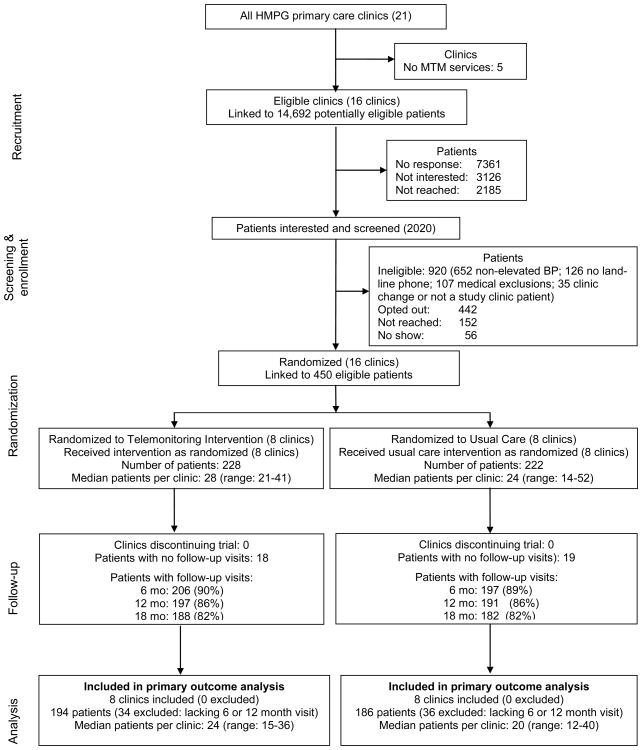
We used electronic medical records to identify adult patients who had an elevated BP (systolic BP ≥140 or diastolic BP ≥90 mm Hg, hereafter abbreviated ≥140/90 mm Hg) at the two most recent primary care encounters in the previous year (Figure 1). Patients meeting these criteria received up to two mailings followed by telephone calls to non-responders. Patients who responded were screened for eligibility by telephone and in the research clinic. During the research clinic screening patients had to have uncontrolled BP (≥140/90 mm Hg or ≥130/80 mm Hg if diabetes or kidney disease was present)3 based on the average of three automated measurements taken using a standardized protocol.17 All patients provided verbal consent to the phone screening and signed a full informed consent form at the beginning of the research clinic visit. All recruitment occurred between March 2009-April 2011.
Figure. 1.
Medical exclusion criteria included stage 4 or 5 kidney disease or albumin-creatinine ratio ≥700 mg/g creatinine; acute coronary syndrome, coronary revascularization, or stroke within past 3 months; known secondary causes of hypertension; pregnancy; class III or IV New York Heart Association heart failure, or known left ventricular ejection fraction <30%. We also required a land-line phone initially, but near the end of recruitment patients with only a cell phone were permitted to enroll.
Of 21 HealthPartners primary care clinics in 2009, 16 had a Medication Therapy Management (MTM) pharmacist on-site at least once weekly.18 At these clinics there was a clinical practice agreement between pharmacists and primary care physicians that allowed pharmacists to prescribe and change antihypertensive therapy within specified parameters. The 16 study clinics were matched by size and clinic-level BP control at baseline and then randomly assigned to either the Telemonitoring Intervention (n = 8) or Usual Care (n = 8) group. Four doctoral pharmacists worked in intervention clinics. They received 8 hours of formal training on the study protocol and each pharmacist was observed conducting a telephone visit on two occasions to verify fidelity to the intervention. Patients were linked to their clinic by self-report and assigned a treatment accordingly. All consenting patients and pharmacists were blinded before randomization, but were informed of their treatment assignment post-randomization.
Interventions
Intervention patients received home monitors (A&D Medical 767PC® automated oscillometric BP monitor, San Jose, CA) that store and transmit BP data to a secure website via modem (AMC Health, New York, NY). Pharmacists met with patients for a one-hour in-person visit, during which they reviewed the patient's relevant history, covered general teaching points about hypertension, instructed them on using the home BP telemonitor system and the individualized home BP goal (i.e., <135/85 mmHg or <125/75 mmHg for patients with diabetes or kidney disease).19, 20 Patients were instructed to transmit at least 6 BP measurements weekly (three in the morning and three in the evening). During the first 6 months of intervention, patients and pharmacists met every two weeks via phone until BP control was sustained for 6 weeks, then frequency was reduced to monthly. During intervention months 7-12, phone visits were every two months. After 12 months, patients returned the telemonitors, returned to their primary physicians' care, and received no pharmacist support. A previous analysis found that patients sent at least 6 BP measurements in 73% of the weeks during the first 6 months of the intervention and that 88% of expected phone visits were conducted.21
During phone visits, pharmacists emphasized lifestyle changes and medication adherence. They assessed and adjusted antihypertensive drug therapy based on an algorithm (Supplemental Tables 1 and 2) using the percentage of home BP readings meeting goal.17 If at least 75% of readings since the last visit met BP goal, no medication changes were generally suggested. If fewer than 75% of readings met goal, the algorithm recommended treatment intensification. Regardless of BP control, if patients experienced adverse effects the drug dosage could be lowered or the drug changed. Pharmacists communicated with patients' primary care teams through the electronic medical record following each visit.
During the study period, Usual Care patients worked with their primary care physicians as usual. This could include referral to an MTM pharmacist for consultation (1-2 visits without telephone follow-up or prolonged monitoring) and conventional home BP measurement.
Outcomes
The primary outcome was the proportion of patients with controlled BP at both the 6 and 12 month research clinic visits. Other outcomes included change in systolic BP (SBP) and diastolic (DBP) at each time point, patient satisfaction with care, and BP control at 18 months. BP-related outcomes were based only on BP measurements taken at research clinic visits.
All patients visited a research clinic for study screening and enrollment, and at 6, 12, and 18 months of follow-up. Research staff were not blinded to study group, but were trained to treat patients in both arms identically. Demographic data were collected at baseline, including sex, self-identified race and ethnicity (White, Black, Asian, other; Hispanic, Non-Hispanic), education, income and marital status. BP was measured at each research visit using standardized technique with an automated monitor identical to the home device. Three measurements were averaged. The number and type of BP medications were inventoried and self-reported adherence was recorded using Morisky's 4-item scale (modified for BP medications).22
Survey data collected at research visits included quality of life and general health measured by the Medical Outcomes Study Short Form 12 questionnaire (version 2), and self-efficacy for managing BP measured by a 13-item subset of questions assessing perceived self-efficacy.13, 23 Six items were selected from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) adult survey v4.0 regarding satisfaction with care.24
We assessed safety by collecting reports at each research visit of all hospitalizations, emergency room, urgent care, and same-day medical visits for problems related to elevated BP, hypotension, fainting, loss of consciousness, or allergic reaction. Medical records of events were reviewed by a physician unrelated to the study with experience assessing adverse events for trials. The severity of the event and probability of its relationship to the study treatment were assessed on 5-point scales.
Direct Program Cost Estimate
All patient encounters with study pharmacists were logged in a database. The pharmacist recorded time spent during encounters with patients, pre-visit time reviewing BP telemonitoring data and preparing for the phone call, and post-visit time documenting the encounter. Monthly time logs were used to reimburse the pharmacy department for the participation of their staff in the study. The price for home BP telemonitoring was negotiated ahead of the trial, with a fixed per-patient enrollment fee and a monthly telemonitoring rate based on the 12-month intervention period. Program cost estimates here exclude patient time, pharmacy, laboratory tests, and non-study encounters.
Sample Size and Statistical Analysis
This study was powered at 80% (alpha=0.05, two-sided test) to detect a difference in the proportion of patients with controlled BP at both 6 and 12 months of 40% in Usual Care and 60% in Telemonitoring Intervention. The sample size was based on recruitment of 450 patients from 16 clinics, of whom 405 (90%) would complete the 6 month clinic visit and 360 (80%) would complete both 6 and 12 month clinic visits.
We used generalized linear mixed models with a logit link and a random intercept for clinic to test the effect of the intervention on the binary outcomes of BP control at 6, 12 and 18 months. For continuous and binary measures obtained over time we used general and generalized linear mixed models with a time period (categories of baseline, 6 months, 12 months, 18 months) by study group interaction term and an additional random term to model the repeated measures from baseline to 6, 12 and 18 months, assuming data were missing at random. To account for missing data on continuous outcomes we used maximum likelihood based ignorable methods that yield valid inference when the outcome data are missing at random. We conducted sensitivity analyses adjusting for race and hypertension treatment, which showed some imbalance by study group. All analyses were 2-sided and P values <.05 were considered statistically significant. Multiple comparisons of BP control and changes in BP were controlled using Holm's step-down procedure. Corrections for multiple comparisons were not conducted for other outcomes.
Results
In total, 14,692 potentially eligible patients were identified using EMR data (Figure 1). Of those, 2,020 expressed interest in participating and agreed to be phone screened; 650 patients did not complete screening. Of the 1,370 who completed screening, 920 were excluded, mostly for non-elevated BP. In total, 450 patients were enrolled and linked to their primary care clinic by self-report. Of these, 228 patients were assigned to Telemonitoring Intervention and 222 patients were assigned to Usual Care. Mean research clinic follow-up time from baseline visit to 6 months was 187.7 days (s.d. 16.9), baseline to 12 months 368.7 days (s.d. 17.3), and baseline to 18 months 547.7 days (s.d. 15.0). Missing a research clinic visit at 6, 12, or 18 months was not associated with study group, baseline SBP or DBP, or baseline BP medication adherence (data not reported).
At baseline, the 450 participants had a mean age of 61.1 years (s.d. 12.0), 45% were women, and 82% were white (Table 1). Nearly half (48%) had a college degree. Many patients had comorbid conditions, including obesity (54%), diabetes (19%), kidney disease (19%), or a history of cardiovascular disease (10%). At baseline, mean BP was 148/85 mm Hg and patients reported taking an average of 1.5 (s.d. 1.2) antihypertensive drug classes. There were significantly more Hispanic patients in Usual Care (P=0.009), and Telemonitoring Intervention patients were somewhat more likely to report receiving hypertension care at baseline (P=0.07).
Table 1. Patient Baseline Characteristics.
| Mean (sd) or No. (%) | Mean (sd) or No. (%) | ||
|---|---|---|---|
| All (N=450) | Telemonitoring Intervention (n=228) | Usual Care (n=222) | |
| Age, mean (sd) | 61.1 (12.0) | 62.0 (11.7) | 60.2 (12.2) |
| Women | 201 (44.7) | 103 (45.2) | 98 (44.1) |
| Race/Ethnicity | |||
| White | 368 (81.8) | 191 (83.8) | 177 (79.7) |
| Black | 53 (11.8) | 24 (10.5) | 29 (13.1) |
| Asian | 7 (1.6) | 4 (1.8) | 3 (1.4) |
| Other (American Indian, Mixed, Other) | 22 (4.9) | 9 (4.0) | 13 (5.9) |
| Hispanic ethnicity | 10 (2.2) | 1 (0.4) | 9 (4.1) |
| Education a | |||
| <= High school or GED | 76 (17.4) | 36 (16.3) | 40 (18.6) |
| Some college or technical school | 151 (34.6) | 72 (32.6) | 79 (36.7) |
| 4 year college degree | 82 (18.8) | 46 (20.8) | 36 (16.7) |
| > 4 year college degree | 127 (29.1) | 67 (30.3) | 60 (27.9) |
| Paid work status a | |||
| Full time | 176 (40.5) | 86 (38.9) | 90 (42.1) |
| Part time | 53 (12.2) | 28 (12.7) | 25 (11.7) |
| Not working | 43 (9.9) | 20 (9.1) | 23 (10.8) |
| Retired | 163 (37.5) | 87 (39.4) | 76 (35.5) |
| Relationship status a | |||
| Married, living together | 301 (69.2) | 160 (72.4) | 141 (65.9) |
| Household income a | |||
| <$30,000 | 65 (17.0) | 34 (18.2) | 31 (15.9) |
| $30-49,999 | 63 (16.5) | 27 (14.4) | 36 (18.5) |
| $50-99,999 | 150 (39.3) | 69 (36.9) | 81 (41.5) |
| >=$100,000 | 104 (27.2) | 57 (30.5) | 47 (24.1) |
| Body mass index a | |||
| Normal (18.5-24.9) | 66 (14.9) | 36 (16.1) | 30 (13.6) |
| Overweight (25–29.9) | 137 (30.9) | 71 (31.7) | 66 (30.0) |
| Obese (>=30) | 241 (54.3) | 117 (52.2) | 124 (56.4) |
| Smoked in last 30 days a | 49 (11.0) | 24 (10.7) | 25 (11.4) |
| Comorbidities affecting BP goal | |||
| Diabetes | 86 (19.1) | 46 (20.2) | 40 (18.0) |
| Chronic kidney disease | 84 (18.6) | 47 (20.6) | 37 (16.7) |
| Diabetes or chronic kidney disease | 146 (32.4) | 81 (35.5) | 65 (29.3) |
| Previous history of cardiovascular disease † | 43 (9.6) | 23 (10.1) | 20 (9.0) |
| eGFR (CKD Epi equation) <60 ml/min/1.73m2 a | 71 (15.9) | 39 (17.1) | 32 (14.6) |
| Urine albumin creatinine ratio >=30 mg/g creatinine a | 88 (19.6) | 46 (20.2) | 42 (19.1) |
| Received medical care for hypertension in past 12 months a | 279 (63.3) | 151 (67.4) | 128 (59.0) |
| Antihypertensive medication classes | |||
| 0 | 118 (26.2) | 54 (23.7) | 64 (28.8) |
| 1 | 116 (25.8) | 56 (24.6) | 60 (27.0) |
| 2 | 115 (25.6) | 63 (27.6) | 52 (23.4) |
| 3 | 78 (17.3) | 42 (18.4) | 36 (16.2) |
| 4+ | 23 (5.1) | 13 (5.7) | 10 (4.5) |
| Antihypertensive medication classes, mean (sd) | 1.5 (1.2) | 1.6 (1.2) | 1.4 (1.2) |
| Systolic BP, mm Hg, mean (sd) | 147.9 (13.0) | 148.2 (12.9) | 147.7 (13.2) |
| Diastolic BP, mm Hg, mean (sd) | 84.7 (11.6) | 84.5 (11.7) | 84.9 (11.5) |
Abbreviations: sd, standard deviation; BP, blood pressure; eGFR, estimated glomerular filtration rate
ever had a heart attack, stroke, heart bypass surgery, or cardiac stent/balloon angioplasty
Missing data for 2-18 patients
The proportions of patients attending follow-up visits were 90% Telemonitoring Intervention and 89% Usual Care at 6 months, 86% in both groups at 12 months, and 82% in both groups at 18 months (Figure 1). By study design all patients had uncontrolled BP at baseline. Among the 380 patients attending both 6 and 12 month visits, the proportions of patients with controlled BP at both visits were 57.2% (95% CI, 44.8%-68.7%) in Telemonitoring Intervention and 30.0% (95% CI, 23.2%-37.8%) in Usual Care (Table 2, P=.001). Under the assumption that all 70 patients with neither a 6 nor 12 month visit had uncontrolled BP at both time points, BP was controlled at both 6 and 12 months in 48.5% (95% CI, 37.0%-60.1%) of Telemonitoring Intervention patients and 25.1% (95% CI, 20.0%-31.0%) of Usual Care patients (P=.001). At 6 months, BP was controlled in 71.8% (95% CI, 65.6%-77.3%) of Telemonitoring Intervention patients and 45.2% (95% CI, 39.2%-51.3%) of Usual Care patients (P<0.0001). At 12 months, BP was controlled in 71.2% (95% CI, 62.0%-78.9%) of Telemonitoring Intervention patients and 52.8% (95% CI, 45.4%-60.2%) of Usual Care patients (P=.005). At 18 months, BP was controlled in 71.8% (95% CI, 65.0%-77.8%) of Telemonitoring Intervention patients and 57.1% (95% CI, 51.5%-62.6%) of Usual Care patients (P=0.003). Among the 362 patients attending all visits at 6, 12 and 18 months, the proportions of patients with controlled BP at all visits were 50.9% (95% CI, 36.9%-64.8%) in Telemonitoring Intervention and 21.3% (95% CI, 14.4%-30.4%) in Usual Care (P=.002). Under the assumption that all 88 patients with one or more missing visits had uncontrolled BP at those time points, BP was controlled at all visits in 40.9% (95% CI 29.7%-53.1%) of Telemonitoring Intervention patients and 17.2% (95% CI, 11.9%-24.3%) of Usual Care patients (P=0.002). The mean difference in SBP change between Telemonitoring Intervention and Usual Care was -10.7 mmHg (95% CI, -14.3 - -7.3 mmHg) at 6 months (P<.0001); -9.7 mmHg (95% CI, -13.4 - -6.0) at 12 months (P<.0001); and -6.6 mmHg (95% CI, -10.7 - -2.5) at 18 months (P=.004). The mean difference in DBP change between Telemonitoring Intervention and Usual Care was -6.0 mm Hg (95% CI, -8.6 - -3.4) at 6 months (P<.0001); 5.1 mmHg (95% CI, -7.4 - -2.8) at 12 months (P=.0003); and -3.0 mmHg (95% CI, -6.3 - 0.3) at 18 months (P=.07). Inclusion of Hispanic ethnicity and having hypertension care in the past 12 months at baseline as covariates in models predicting BP control and change in BP values showed trivial differences in model coefficients and p-values (data not reported).
Table 2. Study Outcomes – Blood Pressure.
| Telemonitoring Intervention | Usual Care | |||||||
|---|---|---|---|---|---|---|---|---|
| No. | % (95% CI) | No. | % (95% CI) | Differential change from baseline | P value | |||
| Composite blood pressure control | ||||||||
| Baseline | 0 | 0% | 0 | 0% | ||||
| 6 and 12 months | 113 | 57.2% (44.8, 68.7) | 58 | 30.0% (23.2, 37.8) | +27.2% (13.4, 40.0) | .001a | ||
| 6, 12, and 18 months | 96 | 50.9% (36.9, 64.8) | 42 | 21.3% (14.4, 30.4) | +29.6% (13.1, 46.0) | .002b | ||
| Blood pressure control | ||||||||
| Baseline | 0 | 0% | 0 | 0% | ||||
| 6 months | 148 | 71.8% (65.6, 77.3) | 89 | 45.2% (39.2, 51.3) | +26.6% (19.1, 33.1) | <.0001c | ||
| 12 months | 141 | 71.2% (62.0, 78.9) | 102 | 52.8% (45.4, 60.2) | +18.4% (7.9, 27.0) | .005c | ||
| 18 months | 135 | 71.8% (65.0, 77.8) | 104 | 57.1% (51.5, 62.6) | +14.7% (7.0, 21.4) | .003c | ||
| Telemonitoring Intervention | Usual Care | |||||||
| Mean (95% CI) | Reduction from baseline, mean (95% CI) | Mean (95% CI) | Reduction from baseline, mean (95% CI) | Differential change from baseline, mean (95% CI) | P value | |||
| Systolic blood pressure | ||||||||
| Baseline | 148.2 (146.3, 150.0) | 147.7 (145.8, 149.5) | ||||||
| 6 months | 126.7 (124.4, 129.0) | -21.5 (-23.9, -19.1) | 136.9 (134.6, 139.2) | -10.8 (-13.3, -8.3) | -10.7 (-14.3, -7.3) | <.0001d | ||
| 12 months | 125.7 (123.4, 128.0) | -22.5 (-25.1, -19.9) | 134.8 (132.5, 137.2) | -12.9 (-15.5, -10.2) | -9.7 (-13.4, -6.0) | <.0001d | ||
| 18 months | 126.9 (124.3, 129.4) | -21.3 (-24.2, -18.4) | 133.0 (130.4, 135.5) | -14.7 (-17.6, -11.8) | -6.6 (-10.7, -2.5) | .004 d | ||
| Diastolic blood pressure | ||||||||
| Baseline | 84.4 (82.3, 86.6) | 85.1 (82.9, 87.3) | ||||||
| 6 months | 75.0 (72.9, 77.2) | -9.4 (-11.1, -7.6) | 81.7 (79.5, 84.0) | -3.4 (-5.2, -1.5) | -6.0 (-8.6, -3.4) | <.0001d | ||
| 12 months | 75.1 (72.8, 77.4) | -9.3 (-11.0, -7.7) | 80.8 (78.5, 83.2) | -4.3 (-5.9, -2.7) | -5.1 (-7.4, -2.8) | .0003d | ||
| 18 months | 75.1 (73.0, 77.2) | -9.3 (-11.7, -7.0) | 78.7 (76.6, 80.9) | -6.4 (-8.7, -3.9) | -3.0 (-6.3, +0.3) | .07 d | ||
Abbreviations: TI,Telemonitoring Intervention; UC, Usual Care
Note: Model-based results from general linear mixed models for BP values (baseline to 6 months, baseline to 12 months, baseline to 18 months), and generalized linear mixed models for BP control (6 months, 12 months, 18 months, 6/12 month composite, 6/12/18 month composite)
Blood pressure data available from research clinic visit from n=228 TI, n=222 UC at baseline; n=206 TI, n=197 UC at 6 months; n=197 TI, n=191 UC at 12 months; n=188 TI, n=182 UC at 18 months
All p-values except diastolic blood pressure reduction at 18 months are significant using Holm step down procedure (alpha=.05) across 11 tests conducted
Study group difference for composite blood pressure control at both 6 and 12 months (n=380, n=194 TI, n=186 UC)
Study group difference for composite blood pressure control at 6 and 12 months and 18 months (n=362, n=184 TI, n=178 UC)
Study group difference at 6 months or 12 months or 18 months
Time by study group term indicating differential reduction from baseline by study group
The mean number of antihypertensive medication classes increased from 1.6 (95% CI, 1.4-1.8) at baseline to 2.2 (95% CI 2.0-2.4) at 6 months in the Telemonitoring Intervention group, and from 1.4 (95% CI, 1.2-1.6) at baseline to 1.6 (95% CI, 1.4-1.8) at 6 months in the Usual Care group (Table 3, P<0.001), with similar differences persisting through 18 months. Between baseline and 6 months, self-reported adherence to hypertension medications increased among Telemonitoring Intervention patients and decreased among Usual Care patients (P<0.05), but did not differ significantly between groups at 12 and 18 months. About half of all patients used a home BP monitor in the past 12 months at baseline, and there was little change in Usual Care patients. During the 12-month intervention home BP monitor use was nearly universal in the Telemonitoring Intervention group, but dropped to 71% (95% CI, 63.0%-78.6%) at 18 months.
Table 3. Other Study Outcomes.
| Telemonitoring Intervention | Usual Care | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline N=228 | 6 mos N=206 | 12 mos N=197 | 18 mos N=188 | Baseline N=222 | 6 mos N=197 | 12 mos N=191 | 18 mos N=182 | |
| No. hypertension medication classes, mean (95% CI) | 1.6 (1.4, 1.8) | 2.2 (2.0, 2.4) | 2.2 (2.0, 2.4) | 2.2 (2.0, 2.4) | 1.4 (1.2, 1.6) | 1.6 (1.4, 1.8) | 1.6 (1.4, 1.8) | 1.7 (1.5, 1.9) |
| Change from baseline, mean (95% CI) | +0.66***† (0.53, 0.78) | +0.63*** (0.49, 0.77) | +0.62** (0.46, 0.77) | +0.16 (0.04, 0.29) | +0.22 (0.07, 0.36) | +0.26 (0.10, 0.42) | ||
|
| ||||||||
| Prescribed any hypertension medications, % (95% CI) | 76.8 (66.1, 84.9) | 94.5 (88.9, 97.4) | 94.6 (89.2, 97.4) | 94.9 (89.4, 97.6) | 73.0 (61.2, 82.1) | 79.3 (68.6, 87.0) | 80.3 (70.6, 87.3) | 81.1 (71.2, 88.1) |
| Change, % (95%) | +17.7** (13.0, 20.3) | +17.8** (13.3, 20.7) | +18.1* (13.5, 20.8) | +6.3 (-2.1, 12.7) | +7.3 (-0.8, 13.8) | +8.1 (-0.3, 14.2) | ||
|
| ||||||||
| Self-reported adherence to hypertension medication, Morisky score=0, % (95% CI) a | 66.7 (58.5, 74.0) | 77.4 (70.2, 83.3) | 68.6 (60.6, 75.6) | 71.6 (63.3, 78.6) | 66.9 (58.1, 74.6) | 61.0 (51.9, 69.4) | 63.7 (54.8, 71.7) | 62.6 (53.1, 71.3) |
| Change, % (95%) | +10.7* (1.5, 17.9) | +1.9 (-8.5, 10.8) | +4.9 (-5.4, 13.3) | -5.9 (-17.8, 4.8) | -3.2 (-14.9, 7.0) | -4.3 (-16.2, 6.2) | ||
|
| ||||||||
| Used home BP monitor past 12 months baseline, past 6 months otherwise, % (95% CI) | 50.6 (42.4, 58.8) | 94.1 (89.1, 96.9) | 95.4 (90.7, 97.7) | 71.4 (63.0, 78.6) | 42.8 (34.7, 51.3) | 43.7 (35.2, 52.6) | 42.8 (34.9, 51.2) | 50.7 (41.7, 59.7) |
| Change, % (95%) | +43.5*** (38.7, 46.2) | +44.8*** (40.0, 47.0) | +20.8 (11.8, 28.5) | +0.9 (-8.4, 10.6) | +0.0 (-10.3, 10.2) | +7.0 (-2.6, 17.0) | ||
|
| ||||||||
| Satisfaction with care b | ||||||||
|
| ||||||||
| Overall rating of health care, mean (95% CI) c | 4.3 (4.2, 4.4) | 4.6 (4.4, 4.7) | 4.5 (4.4,4.6) | 4.5 (4.4, 4.7) | 4.3 (4.1, 4.4) | 4.4 (4.2, 4.5) | 4.4 (4.3, 4.6) | 4.4 (4.3, 4.5) |
| Change, mean (95% CI) | +0.27 (0.16, 0.39) | +0.22 (0.08, 0.35) | +0.26 (0.13, 0.38) | +0.11 (-0.01, 0.23) | +0.18 (0.14, 0.32) | +0.15 (0.03, 0.28) | ||
| Providers listened carefully, mean (95% CI) d | 3.5 (3.4, 3.6) | 3.7 (3.6, 3.8) | 3.6 (3.5, 3.8) | 3.6 (3.5, 3.8) | 3.5 (3.4, 3.7) | 3.5 (3.4, 3.7) | 3.6 (3.5, 3.7) | 3.7 (3.5, 3.8) |
| Change, mean (95% CI) | +0.20 ** (0.11, 0.31) | +0.13 (0.03, 0.23) | +0.13 (0.01, 0.24) | +0.01 (-0.10, 0.11) | +0.05 (-0.05, 0.15) | +0.12 (0.01, 0.22) | ||
|
| ||||||||
| Providers explained things clearly, mean (95% CI) d | 3.7 (3.6, 3.7) | 3.8 (3.7, 3.9) | 3.8 (3.7, 3.8) | 3.7 (3.6, 3.7) | 3.6 (3.5, 3.7) | 3.6 (3.5, 37) | 3.7 (3.6, 3.8) | 3.7 (3.6, 3.8) |
| Change, mean (95% CI) | +0.12* (0.02, 0.22) | +0.09 (-0.01, 0.19) | +0.09 (-0.01, 0.19) | -0.03 (-0.13, 0.07) | +0.10 (0.01, 0.20) | +0.13 (0.02, 0.23) | ||
|
| ||||||||
| Providers respected what I said, mean (95% CI) d | 3.6 (3.5, 3.7) | 3.8 (3.7, 3.9) | 3.8 (3.6, 3.9) | 3.7 (3.6, 3.9) | 3.7 (3.6, 3.8) | 3.7 (3.6, 3.9) | 3.7 (3.6, 3.8) | 3.7 (3.6, 3.9) |
| Change, mean (95% CI) | +.19* (0.10, 0.28) | +0.14 (0.05, 0.23) | +0.11 (-0.02, 0.24) | +0.02 (-0.07, 0.12) | +0.01 (-0.08, 0.11) | +0.07 (-0.06, 0.20) | ||
|
| ||||||||
| Providers spent enough time with me, mean (95% CI) d | 3.4 (3.3, 3.6) | 3.6 (3.5, 3.8) | 3.6 (3.4, 3.7) | 3.6 (3.5, 3.7) | 3.5 (3.4, 3.7) | 3.6 (3.4, 3.7) | 3.6 (3.5, 3.8) | 3.7 (3.5, 3.8) |
| Change, mean (95% CI) | +0.20 (0.07, 0.31) | +0.11 (-0.03, 0.25) | +0.17 (0.06, 0.28) | +0.04 (-0.08, 0.17) | +0.13 (-0.01, 0.27) | +0.15 (0.03, 0.26) | ||
|
| ||||||||
| Had problems getting care needed, mean (95% CI) d | 1.7 (1.5, 1.9) | 1.9 (1.6, 2.1) | 1.9 (1.6, 2.1) | 1.8 (1.5, 2.1) | 1.9 (1.6, 2.1) | 2.0 (1.8, 2.3) | 1.9 (1.7, 2.2) | 1.9 (1.7, 2.2) |
| Change, mean (95% CI) | +0.15 (-0.09, 0.39) | +0.15 (-0.15, 0.45) | +0.07 (-0.22, 0.35) | +0.18 (-0.07, 0.43) | +0.04 (-0.26, 0.35) | +0.05 (-0.24, 0.34) | ||
|
| ||||||||
| Physical and mental function, mean (sd) | ||||||||
|
| ||||||||
| SF 12 physical, mean (95% CI) e | 48.0 (45.8, 50.2) | 47.5 (45.2, 49.8) | 47.2 (44.8, 49.5) | 47.4 (45.1, 49.7) | 47.3 (45.1, 49.6) | 46.2 (43.9, 48.5) | 46.6 (44.3, 49.0) | 46.6 (44.2, 48.9) |
| Change, mean (95% CI) | -0.50 (-1.56, 0.56) | -0.84 (-2.00, 0.32) | -0.54 (-1.77, 0.69) | -1.17 (-2.26, 0.07) | -0.72 (-1.90, 0.45) | -0.82 (-2.09, 0.45) | ||
|
| ||||||||
| SF 12 mental, mean (95% CI) e | 52.2 (50.7, 53.8) | 52.5 (51.0, 54.0) | 52.1 (50.4, 53.8) | 53.7 (52.3, 55.1) | 51.2 (49.6, 52.8) | 51.3 (49.8, 52.9) | 50.5 (48.8, 52.3) | 51.8 (50.3, 53.2) |
| Change, mean (95% CI) | +0.25 (-0.88, 1.38) | -0.05 (-1.83, 0.78) | +1.51 (-0.18, 2.40) | +0.09 (-1.08, 1.26) | -0.78 (-2.11, 0.55) | +0.50 (-0.83, 1.84) | ||
|
| ||||||||
| Self efficacy | ||||||||
|
| ||||||||
| Can communicate with nurse/pharmacist, mean (95% CI) f | 4.4 (4.3, 4.5) | 4.5 (4.4, 4.6) | 4.4 (4.3, 4.5) | 4.5 (4.4, 4.7) | 4.4 (4.3, 4.5) | 4.4 (4.2, 4.5) | 4.4 (4.2, 4.5) | 4.5 (4.3, 4.6) |
| Change, mean (95% CI) | +0.09 (-0.01, 0.18) | -0.02 (-0.14, 0.11) | +0.12 (0.02, 0.21) | -0.03 (-0.12, 0.07) | -0.02 (-0.15, 0.11) | +0.05 (-0.05, 0.15) | ||
|
| ||||||||
| Can communicate with health care team, mean (95% CI) f | 4.4 (4.2, 4.5) | 4.5 (4.3, 4.6) | 4.4 (4.2, 4.5) | 4.5 (4.4, 4.6) | 4.4 (4.2, 4.5) | 4.3 (4.2, 4.4) | 4.4 (4.3, 46) | 4.5 (4.3, 4.6) |
| Change, mean (95% CI) | +0.08* (-0.02, 0.18) | -0.02 (-0.13, 0.10) | +0.11 (-0.01, 0.21) | -0.06 (-0.16, 0.04) | +0.07 (-0.04, 0.18) | +0.09 (-0.01, 0.20) | ||
|
| ||||||||
| Can include home BP monitoring in weekly routine, mean (95% CI) f | 4.6 (4.4, 4.7) | 4.7 (4.5, 4.9) | 4.2 (4.0, 4.4) | 4.0 (3.8, 4.2) | 4.5 (4.3, 4.6) | 3.8 (3.6, 4.0) | 3.7 (3.5, 3.9) | 4.0 (3.8, 4.2) |
| Change, mean (95% CI) | +0.16*** (-0.04, 0.37) | -0.34** (-0.54, 0.14) | -0.51 (-0.72, 0.30) | -0.69 (-0.90, 0.48) | -0.77 (-0.97, 0.57) | -0.50 (-0.71, 0.28) | ||
|
| ||||||||
| Can follow medication regime, mean (95% CI) f | 4.7 (4.6, 4.9) | 4.8 (4.7, 4.9) | 4.7 (4.6, 4.8) | 4.8 (4.7, 4.9) | 4.7 (4.6, 4.8) | 4.5 (4.4, 4.6) | 4.6 (4.5, 4.7) | 4.6 (4.5, 4.7) |
| Change, mean (95% CI) | +0.05* (-0.05, 0.15) | -0.08 (-0.20, 0.05) | +0.05 (-0.06, 0.16) | -0.15 (-0.26, 0.04) | -0.09 (-0.21, 0.04) | -0.07 (-0.19, 0.04) | ||
|
| ||||||||
| Can keep BP under control, mean (95% CI) f | 3.8 (3.7, 4.0) | 4.2 (4.1, 4.4) | 4.2 (4.0, 4.3) | 4.3 (4.2, 4.4) | 3.9 (3.7, 4.0) | 3.9 (3.7, 4.0) | 3.9 (3.7, 4.0) | 4.0 (3.9, 4.1) |
| Change, mean (95% CI) | +0.40** (0.24, 0.55) | +0.34** (0.19, 0.50) | +0.47* (0.30, 0.63) | 0.01 (-0.15, 0.16) | +0.01 (-0.14, 0.17) | +0.15 (-0.02, 0.32) | ||
|
| ||||||||
| Lifestyle change | ||||||||
|
| ||||||||
| Smoked in last 30 days, % (95% CI), | 7.0 (2.2, 19.9) | 5.5 (1.7, 16.5) | 6.1 (2.0, 16.8) | 4.4 (1.3, 14.0) | 10.3 (3.5, 26.7) | 10.7 (3.6, 27.9) | 9.0 (3.2, 23.1) | 9.7 (3.2, 25.6) |
| Change, %, (95% CI) | -1.5 (-4.1, 3.2) | -1.0 (-4.7, 3.5) | -2.6 (-5.1, 1.6) | +0.4 (-4.3, 8.4) | -1.3 (-5.9, 5.6) | -0.6 (-4.9, 7.2) | ||
|
| ||||||||
| Add salt after served at table, daily or more, % (95% CI) | 21.1 (15.3, 28.3) | 10.3 (6.4, 16.3) | 10.4 (6.1, 17.1) | 12.3 (7.8, 18.9) | 19.4 (13.8, 26.6) | 18.9 (13.1, 26.4) | 20.9 (3.7, 15.1) | 19.3 (13.3, 27.2) |
| Change, %, (95% CI) | -10.8* (-14.9, -4.4) | -10.7* (-14.8, -4.1) | -8.8 (-13.5, -1.6) | -0.5 (-8.2, 6.9) | +1.4 (-5.8, 10.2) | -0.2 (-7.0, 8.7) | ||
|
| ||||||||
| Add salt when preparing food, daily or more, % (95% CI) | 27.3 (20.6, 35.2) | 15.3 (10.2, 22.1) | 13.4 (8.7, 20.1) | 13.8 (9.3, 20.2) | 23.3 (17.0, 31.0) | 25.4 (18.5, 33.7) | 24.6 (17.9, 32.8) | 23.3 (17.2, 30.8) |
| Change, %, (95% CI) | -12.0* (-17.3, -4.7) | -13.9* (-18.6, -6.7) | -13.5* (-18.4, -6.2) | +2.1 (-5.5, 11.5) | +1.3 (-6.3, 10.5) | +0.0 (-8.3, 9.4) | ||
|
| ||||||||
| 7+ alcohol drinks/wk, % (95% CI) | 20.4 (13.6, 29.5) | 16.7 (10.6, 25.3) | 18.2 (11.5, 27.7) | 15.8 (9.8, 24.4) | 18.4 (11.9, 27.3) | 15.0 (9.2, 23.4) | 13.1 (7.7, 21.3) | 13.0 (7.7, 21.1) |
| Change, %, (95% CI) | -3.7 (-9.5, 4.3) | -2.2 (-8.5, 6.1) | -4.6 (-10.5, 3.1) | -3.4 (-8.9, 4.3) | -5.3 (-10.1, 2.1) | -5.5 (-11.0, 1.6) | ||
|
| ||||||||
| BMI, mean (95% CI) | 31.3 (30.2, 32.5) | 31.4 (30.2, 32.5) | 31.6 (30.4, 32.7) | 31.6 (30.5, 32.8) | 31.7 (30.5, 32.8) | 31.7 (30.5, 32.9) | 31.7 (30.5, 32.9) | 31.5 (30.4, 32.7) |
| Change, mean (95% CI) | +0.05 (-0.20, 0.31) | +0.27 (-0.01, 0.55) | +0.36* (0.03, 0.68) | +0.04 (-0.22, 0.30) | +0.05 (-0.23, 0.33) | -0.15 (-0.48, 0.18) | ||
|
| ||||||||
| Physical activity meets CDC guidelines, % (95% CI) g | 34.3 (25.4, 44.5) | 39.6 (29.9, 50.3) | 43.1 (34.1, 52.6) | 36.5 (28.2, 45.7) | 32.3 (23.5, 42.6) | 30.7 (21.9, 41.3) | 39.9 (31.0, 49.4) | 37.7 (29.1, 47.3) |
| Change, %, (95% CI) | +5.3 (-3.6, 15.0) | +8.8 (-0.5, 18.7) | +2.2 (-6.6, 12.0) | -1.6 (-9.7, 7.9) | +7.5 (-1.6, 17.4) | +5.3 (-4.4, 14.8) | ||
Note: Model-based results from general and generalized linear mixed models predicting outcome from study arm, time, arm by time interaction.
P< .05,
P< .01,
P< .001
P-values (as shown with asterisks) from the time by study group interaction term indicate differential change by study group from baseline to 6 months, baseline to 12 months, or baseline to 18 months.
Limited to patients who self-report taking hypertension medications (n=330 baseline, 336 at 6 months, 332 at 12 months, 317 at 18 months). Scored 0-4 based on 4 questions about non-adherence. Each positive response is 1 point; on scale of 0-4, 0 is perfect self-reported adherence.22
Limited to patients saying they received health care in last 12 months at baseline (n=425), last 6 months at 6 month clinic visit (n=334), last 6 months at 12 month clinic visit (n=303), last 6 months at 18 months (n=272). Includes selected items from the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey.24
From CAHPS survey. Item answered on scale of 0-5, with 0=“worst” and 5=“best.”
From CAHPS survey. Items answered on scale of 1=“never”, 2=“sometimes”, 3=“usually”, 4=“always”.
From SF-12 survey, scored on scale of 0-100 with 100 indicating highest levels of health.23
Items answered on scale of 1-5, with 1=“Not confident”, 5=“Very confident”.13
Based on U.S. Centers for Disease Control and Prevention guidelines for moderate-intensity physical activity in adults. Available for reference at http://www.cdc.gov/physicalactivity/everyone/guidelines/adults.html
Among patients receiving any medical care in the previous period, overall satisfaction with care was similar in both groups. Satisfaction items concerning health care providers listening carefully, explaining things clearly, and respecting what the patient said showed larger improvements among Telemonitoring Intervention than Usual Care at 6 months (all P<0.05), but not at 12 or 18 months. Functional status did not differ by study group. Self-efficacy questions indicated Telemonitoring Intervention patients were substantially more confident than Usual Care patients that they could communicate with their health care team, include home BP monitoring in their weekly routine, follow their medication regime, and keep their BP under control. Telemonitoring Intervention patients self-reported adding less salt to food than Usual Care patients at all time points, but other lifestyle factors did not differ.
There were 109 possible adverse events reported, 60 in Usual Care and 49 in Telemonitoring Intervention. Most events were non-cardiovascular hospitalizations. There were two allergic reactions attributed to blood pressure medicine in Usual Care patients. There were seven events related to hypotension, dizziness, or loss of consciousness (six Telemonitoring Intervention, one Usual Care), and five events related to hypertension (four Usual Care, one Telemonitoring Intervention). All the hypotension-related events in Telemonitoring Intervention patients occurred among patients with the lower BP goal of <130/80 mmHg due to having either diabetes or kidney disease. Other cardiovascular events included: 7 strokes (5 Usual Care, 2 Telemonitoring Intervention), 3 transient ischemic attacks (all Usual Care), 2 episodes of atrial fibrillation (1 Usual Care, 1 Telemonitoring Intervention), 1 myocardial infarction (Usual Care), 1 episode of angina (Telemonitoring Intervention) and two cardiac bypass surgeries (both Usual Care).
Direct program costs per patient in the intervention group were $1045 over the 12-month intervention period. About half (48%) of program costs were for care management services and the remainder were for telemonitoring services; however, the study received discounted pricing for research from the telemonitoring vendor. In the Telemonitoring Intervention group, all 228 patients used pharmacist services, averaging 11.4 (s.d. 3.9) visits each and 34.2 minutes per encounter; and 217 used telemonitoring services, averaging 9.8 (s.d. 2.5) months of actual use. Under prevailing market rates and this level of telemonitoring utilization, we estimate that direct program costs would total about $1350 per patient.
Discussion
Our results show that, compared to usual primary care, home BP telemonitoring with pharmacist management resulted in large improvements in BP control and substantial decreases in BP over 12 months. Compared to Usual Care patients, Telemonitoring Intervention patients had greater antihypertensive medication intensification and better self-reported adherence to antihypertensive medication and sodium restriction. The intervention also improved some aspects of patient satisfaction and appeared to have acceptable safety.
Unique features of our study were the primary outcome of composite BP control at 6 and 12 months, the maintenance intervention from 6-12 months and the extended post-intervention follow-up at 18 months. We selected a composite primary outcome because early and persistent BP control is likely to be more effective for prevention of CV events than intermittent control. Although BP control in both groups was lower for the composite measure than at single time points, the Telemonitoring Intervention group had 25%-30% higher absolute control rates compared to the Usual Care group. The pattern of BP control that we observed was maintenance of the level of BP control achieved at 6 months in the Telemonitoring Intervention group though 18 months. In contrast, BP control gradually improved in the Usual Care group, but still remained substantially lower than the Telemonitoring Intervention group by an absolute 15% by 18 months. Improvement in the usual care group over time has been observed in other studies.16 Although we did not find significant changes in antihypertensive treatment, lifestyle or self-reported medication adherence in the Usual Care group, the measures reported here may not have captured subtle changes that resulted in improved BP over time. Data on the long-term effectiveness of team-based care and home BP monitoring interventions beyond 12 months are limited and conflicting, and no study has measured post-intervention outcomes with rigorous research-quality BP measures.7-9, 14, 16, 25-28 Our study shows that high levels of BP control are maintained with less intensive intervention and persist for at least 6 months after the intervention is stopped.
HyperLink included several of the six domains designated by the Chronic Care Model, a framework for organizational changes to improve chronic illness care: delivery system redesign, clinical information systems, and self-management support.29 HyperLink's design was also based on three decades of quality improvement trials for hypertension care showing that organizational interventions, including non-physician hypertension care, achieved the largest BP reductions.5-8, 25, 30-36 In most cases, these interventions included a nurse or pharmacist and were called “team change,” “team-based care,” “case management,” “disease management,” or “nurse- or pharmacist-led care.” In a 2006 meta-analysis of these studies, average BP dropped by 10/4 mmHg, and the absolute proportion of patients achieving BP control improved by 20%.5 The most successful interventions did not depend upon the physician responding to recommendations. A recently updated meta-analysis including 31 additional studies confirmed these findings, and although BP reductions were smaller (6/2 mm Hg), the benefits extended to improving other CV risk factors (lipids and glycemic control).7
Other strategies in previous research associated with large BP improvements include patient self-management and self-monitoring with resources or devices that enhance patients' abilities to manage their condition.5, 30, 32, 37-39 Home BP monitoring with or without additional support was the subject of several recent comprehensive evidence reviews concluding that home monitoring alone results in small BP reductions at 6 months compared with usual care (reductions of 3/2 mm Hg), but evidence regarding longer-term efficacy is lacking.6, 9, 40-42 In contrast, improved BP outcomes were more robust in high-quality studies combining home BP monitoring with some additional support intervention for up to 12 months (SBP reductions of 3 to 9 mm Hg and DBP 2 to 4 mm Hg).9
The combination of home BP monitoring and team-based hypertension care has been the subject of several high quality studies. A recent study by Green and colleagues using secure email to convey home BP data to pharmacists found BP and BP control improvements compared to usual care over 12 months that were quite similar to those observed in HyperLink, but the study excluded patients with diabetes, renal disease or cardiovascular disease.13 In another recently published study conducted in a managed care setting, patients randomly assigned to home BP telemonitoring combined with pharmacist-led care had 13 mm Hg greater reductions in SBP than usual care over a 6-month period.43
Artinian and colleagues12 studied 387 urban African Americans with uncontrolled BP randomly assigned to community nurse-managed telemonitoring or usual care. At 12 months, intervention patients had a 5 mm Hg greater reduction in SBP, but DBP and BP control did not differ. A British study randomized patients with uncontrolled BP on up to two antihypertensive drugs to usual care or an intervention combining home BP telemonitoring and self-titration of medications.15 SBP decreased 6 mm Hg more in the intervention group after 12 months and most patients in the intervention made at least one medication change. Another recent study among U.S. veterans compared a telemonitoring intervention with various types of nurse management to usual care.16 The largest effect was observed for a combined behavioral and medication management intervention in the post-hoc subgroup with inadequate BP control at baseline (SBP was15 mm Hg lower at 12 months and 8 mm Hg lower at 18 months, both significantly different than control).
It is important to consider intervention costs in addition to effectiveness. We project that direct program costs would total $1350 per patient under current market rates when patients are given up to 12 months of access to telemonitoring. This is quite similar to the cost estimate for 18 months of combined behavioral and medication management for hypertension in the telemonitoring trial conducted among veterans.16 It may be possible to reduce total program costs through better targeting of patients, negotiating volume discounts, and by individual tailoring of the intervention, for example by replacing telemonitoring with a standard home BP monitor after a patient demonstrates that they have reached and sustained home BP goals. We plan future analyses that will take into account indirect costs over 18 months and long-term cost saving from averting hypertension-related adverse events.
Some limitations of HyperLink should be considered in interpreting its results. Although the study aimed to enroll a broad population, only about 1 in 7 patients solicited by mail for participation responded, and of those screened only about 1 in 4 was eligible. Participants were generally well-educated with high incomes, and perhaps reflecting the study population's interest in hypertension, about half had used a home BP monitor in the previous year. The study was conducted in one integrated health care system, but our findings are in agreement with studies conducted in Washington, Colorado, Michigan and North Carolina in a variety of health care settings. As in any multi-component intervention, it is difficult to separate how much of the intervention effect is attributable to the telemonitoring and pharmacist case management. The study was not blinded, which could have had an effect on the reporting of subjective outcomes and adverse events. However, BP was measured using automated devices with a standard protocol and is unlikely to have been biased. Finally, although BP improvement was substantial and a full cost analysis is underway, no study has yet conducted a thorough cost-effectiveness analysis of this type of intervention. Lack of information on long-term effects, reimbursement mechanisms and return on investment have been identified as barriers to implementation.7, 9 We hope to address these issues when a planned long-term follow-up study is completed.
We conclude that BP telemonitoring and pharmacist case management was safe and effective for improving BP control compared to usual care over 12 months and the improved BP in the intervention group was maintained for 6 months following the intervention. HyperLink included patients with a much wider range of hypertension severity and comorbidity than have been enrolled in previous trials. If these results are found to be cost-effective and durable over an even longer period, it should spur wider testing and dissemination of similar alternative models of care for managing hypertension and other chronic conditions.
Supplementary Material
Acknowledgments
This study is supported by a grant from the National Heart, Lung, and Blood Institute (R01HL090965). The sponsor had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript. Co-author Stephen E. Asche had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Authors Karen L. Margolis, MD, MPH, Stephen E. Asche, MA, Anna R. Bergdall, MPH, Steven P. Dehmer, PhD, Tessa J. Kerby, MPH, Michael V. Maciosek, PhD, Patrick J. O'Connor, MD, MPH, Rachel A. Pritchard, BA, Jaime L. Sekenski, BS, JoAnn M. Sperl-Hillen, MD, MPH, Nicole K. Trower, BA receive grant support administered through their institution, HealthPartners Institute for Education and Research (HPIER), for work on Hyperlink. Dr. Sperl-Hillen is listed as an inventor on a U.S. patent (#8,388,342 B2) issued in 2013 titled “Disease Treatment Simulation.” She is eligible to receive revenue in the future per HPIER intellectual property policy. To date, she has received no payment for this role. HealthPartners Institute for Education and Research has recently entered into a royalty-bearing license agreement with a third party to commercialize the simulated learning technology for the purpose of broader dissemination. Dr. Sperl-Hillen will serve as a non-paid director on the board of directors for that licensee. She has no other relevant financial or nonfinancial relationships to report. Supplemental material includes: Margolis KL, Kerby TJ, Asche SE, Bergdall AR, Maciosek MV, O'Connor PJ, et al. Design and rationale for Home Blood Pressure Telemonitoring and Case Management to Control Hypertension (HyperLink): A cluster randomized trial. Contemp Clin Trials. Jul 2012;33(4):794-803, and two tables.
References
- 1.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics--2012 update: a report from the American Heart Association. Circulation. 2012 Jan 3;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsiao C, Cherry D, Beatty P, Rechtsteiner E. National Ambulatory Medical Care Survey: 2007 summary. 27. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 3.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 4.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010 May 26;303(20):2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 5.Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, Lewis R, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006 Jul;44(7):646–657. doi: 10.1097/01.mlr.0000220260.30768.32. [DOI] [PubMed] [Google Scholar]
- 6.Glynn LG, Murphy AW, Smith SM, Schroeder K, Fahey T. Interventions used to improve control of blood pressure in patients with hypertension. Cochrane Database Syst Rev. 2010;(3):CD005182. doi: 10.1002/14651858.CD005182.pub4. [DOI] [PubMed] [Google Scholar]
- 7.Guide to Community Preventive Services. Cardiovascular disease prevention and control: team-based care to improve blood pressure control. 2012 Apr; doi: 10.1016/j.amepre.2014.03.003. www.thecommunityguide.org/cvd/teambasedcare.html. [DOI] [PubMed]
- 8.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009 Oct 26;169(19):1748–1755. doi: 10.1001/archinternmed.2009.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uhlig K, Balk EM, Patel K, Ip S, Kitsios GD, Obadan NO, et al. Self-Measured Blood Pressure Monitoring: Comparative Effectiveness. Rockville, MD: Agency for Healthcare Research and Quality (US); Jan, 2012. [PubMed] [Google Scholar]
- 10.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-Term Risk of Mortality Associated With Selective and Combined Elevation in Office, Home, and Ambulatory Blood Pressure. Hypertension. 2006 May 1;47(5):846–853. doi: 10.1161/01.HYP.0000215363.69793.bb. [DOI] [PubMed] [Google Scholar]
- 11.Mengden T, Hernandez Medina RM, Beltran B, Alvarez E, Kraft K, Vetter H. Reliability of reporting self-measured blood pressure values by hypertensive patients. Am J Hypertens. 1998;11:1413–1417. doi: 10.1016/s0895-7061(98)00241-6. [DOI] [PubMed] [Google Scholar]
- 12.Artinian NT, Flack JM, Nordstrom CK, Hockman EM, Washington OGM, Jen KC, et al. Effects of nurse-managed telemonitoring on blood pressure at 12-month follow-up among urban African Americans. Nurs Res. 2007;56(5):312–316. doi: 10.1097/01.NNR.0000289501.45284.6e. [DOI] [PubMed] [Google Scholar]
- 13.Green BB, Cook AJ, Ralston JD, Fishman PA, Catz SL, Carlson J, et al. Effectiveness of home blood pressure monitoring, Web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299(24):2857–2867. doi: 10.1001/jama.299.24.2857. Jun 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bosworth HB, Olsen MK, Grubber JM, Neary AM, Orr MM, Powers BJ, et al. Two self-management interventions to improve hypertension control: a randomized trial. Ann Intern Med. 2009 Nov 17;151(10):687–695. doi: 10.1059/0003-4819-151-10-200911170-00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McManus RJ, Mant J, Bray EP, Holder R, Jones MI, Greenfield S, et al. Telemonitoring and self-management in the control of hypertension (TASMINH2): A randomised controlled trial. The Lancet. 2010 Jul 17;376(9736):163–172. doi: 10.1016/S0140-6736(10)60964-6. [DOI] [PubMed] [Google Scholar]
- 16.Bosworth HB, Powers BJ, Olsen MK, McCant F, Grubber J, Smith V, et al. Home blood pressure management and improved blood pressure control: Results from a randomized controlled trial. Arch Intern Med. 2011 Jul 11;171(13):1173–1180. doi: 10.1001/archinternmed.2011.276. [DOI] [PubMed] [Google Scholar]
- 17.Margolis KL, Kerby TJ, Asche SE, Bergdall AR, Maciosek MV, O'Connor PJ, et al. Design and rationale for Home Blood Pressure Telemonitoring and Case Management to Control Hypertension (HyperLink): A cluster randomized trial. Contemp Clin Trials. 2012 Jul;33(4):794–803. doi: 10.1016/j.cct.2012.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare and Medicaid Services (CMS), U.S. Department of Health & Human Services. Medicare Part D Medication Therapy Management (MTM) Programs:2010 Fact Sheet. 2010 http://www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/downloads/MTMFactSheet_2010_06-2010_final.pdf.
- 19.Pickering T. Recommendations for the use of home (self) and ambulatory blood pressure monitoring. Am J Hypertens. 1996;9:1–11. doi: 10.1016/0895-7061(95)00341-x. [DOI] [PubMed] [Google Scholar]
- 20.Staessen JA, Den Hond E, Celis H, Fagard R, Keary L, Vandenhoven G, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial.[see comment] JAMA. 2004;291(8):955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 21.Kerby TJ, Asche SE, Maciosek MV, O'Connor PJ, Sperl-Hillen JM, Margolis KL. Adherence to blood pressure telemonitoring in a cluster-randomized clinical trial. J Clin Hypertens (Greenwich) 2012 Oct;14(10):668–674. doi: 10.1111/j.1751-7176.2012.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morisky D, Green L, Levine D. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Ware JE, Kosinski M, Turner-Bower D, Gandek B. How to score version 2 of the SF-12 health survey (with a supplement documenting version 1) Lincoln, RI: QualityMetric Incorporated; 2002. [Google Scholar]
- 24.Agency for Healthcare Research and Quality, editor. From the CAHPS Health Plan Survey and Reporting Kit. Rockville, MD: 2007. Preparing a Questionnaire Using the CAHPS Health Plan Survey 4.0. Updated July 2007. [Google Scholar]
- 25.Carter BL, Ardery G, Dawson JD, James PA, Bergus GR, Doucette WR, et al. Physician and pharmacist collaboration to improve blood pressure control. Arch Intern Med. 2009 Nov 23;169(21):1996–2002. doi: 10.1001/archinternmed.2009.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carter BL, Bosworth HB, Green BB. The Hypertension Team: The role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens. 2012 Jan;14(1):51–65. doi: 10.1111/j.1751-7176.2011.00542.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wentzlaff DM, Carter BL, Ardery G, Franciscus CL, Doucette WR, Chrischilles EA, et al. Sustained blood pressure control following discontinuation of a pharmacist intervention. J Clin Hypertens. 2011 Jun;13(6):431–437. doi: 10.1111/j.1751-7176.2011.00435.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Welch LK, Olson KL, Snow KE, Pointer L, Lambert-Kerzner A, Havranek EP, et al. Systolic blood pressure control after participation in a hypertension intervention study. Am J Manag Care. 2011;17(7):473–478. [PubMed] [Google Scholar]
- 29.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 30.Fahey T, Schroeder K, Ebrahim S. Educational and organizational interventions used to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract. 2005;55:875–882. [PMC free article] [PubMed] [Google Scholar]
- 31.Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med. 2004 Apr 12;164(7):722–732. doi: 10.1001/archinte.164.7.722. [DOI] [PubMed] [Google Scholar]
- 32.Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, et al. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143:427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- 33.Tsai AC, Morton SC, Mangione CM, Keeler EB. A meta-analysis of interventions to improve care for chronic conditions. Am J Manag Care. 2005;11:478–488. [PMC free article] [PubMed] [Google Scholar]
- 34.Weingarten SR, Henning JM, Badamgarav E, Knight K, Hasselblad V, Gano A, et al. Interventions used in disease management programmmes for patients with chronic illness - which ones work? Meta-analysis of published reports. BMJ. 2002;325:925–932. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004 Jul 17;329(7458):145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Clark CE, Smith LF, Taylor RS, Campbell JL. Nurse led interventions to improve control of blood pressure in people with hypertension: systematic review and meta-analysis. BMJ. 2010;341:c3995. doi: 10.1136/bmj.c3995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Friedman RH, Kazis LE, Jette A, Smith MB, Stollerman J, Torgerson J, et al. A Telecommunications System for Monitoring and Counseling Patients With Hypertension: Impact on Medication Adherence and Blood Pressure Control. Am J Hypertens. 1996;9(4):285. doi: 10.1016/0895-7061(95)00353-3. [DOI] [PubMed] [Google Scholar]
- 38.Artinian N, Washington O, Templin T. Effects of home telemonitoring and community-based monitoring on blood pressure control in urban African Americans: A pilot study. Heart Lung. 2001;30:191–199. doi: 10.1067/mhl.2001.112684. [DOI] [PubMed] [Google Scholar]
- 39.Rogers MA, Small D, Buchan DA, Butch CA, Stewart CM, Krenzer BE, et al. Home monitoring service improves mean arterial pressure in patients with essential hypertension. A randomized, controlled trial. Ann Intern Med. 2001 Jun 5;134(11):1024–1032. doi: 10.7326/0003-4819-134-11-200106050-00008. [DOI] [PubMed] [Google Scholar]
- 40.Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004 Jul 17;329(7458):145. doi: 10.1136/bmj.38121.684410.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bray EP, Holder R, Mant J, McManus RJ. Does self-monitoring reduce blood pressure? Meta-analysis with meta-regression of randomized controlled trials. Ann Med. 2010 Jul;42(5):371–386. doi: 10.3109/07853890.2010.489567. [DOI] [PubMed] [Google Scholar]
- 42.Agarwal R, Bills JE, Hecht TJ, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control: a systematic review and meta-analysis. Hypertension. 2011 Jan;57(1):29–38. doi: 10.1161/HYPERTENSIONAHA.110.160911. [DOI] [PubMed] [Google Scholar]
- 43.Magid DJ, Olson KL, Billups SJ, Wagner NM, Lyons EE, Kroner BA. A pharmacist-led, american heart association heart360 web-enabled home blood pressure monitoring program. Circ Cardiovasc Qual Outcomes. 2013 Mar 1;6(2):157–163. doi: 10.1161/CIRCOUTCOMES.112.968172. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.