Abstract
Patient: Male, 27
Final Diagnosis: Tracheobronchopathia osteochondroplastica
Symptoms: Shortness of breath • stridor
Medication: —
Clinical Procedure: Neck computer tomography • pulmonary function test • neck surgical exploration • tracheostomy placement
Specialty: Critical Care Medicine
Objective:
Unusual clinical course
Background:
Tracheobronchopathia osteochondroplastica is a rare benign and often indolent disease. We report the first case of tracheobronchopathia osteochondroplastica (TBO) presenting as acute hypercarbic respiratory failure due to superimposed subglottic submucosal abscess.
Case Report:
A 27-year-old man presented to the emergency department in respiratory distress that required mechanical ventilation for acute hypercarbic respiratory failure. Upon extubation the next day, stridor was elicited with ambulation. Spirometry revealed fixed upper airway obstruction. Neck imaging showed a 2.8×2.0×4.0 cm partially calcified subglottic mass with cystic and solid component obstructing 75% of the airway. Surgical exploration revealed purulent drainage upon elevation of the thyroid isthmus and an anterolateral cricoid wall defect in communication with a subglottic submucosal cavity. Microbiology was negative for bacteria or fungi. Pathology showed chondro-osseous metaplasia compatible with tracheobronchopathia osteochondroplastica (TBO). The patient received a course of antibiotics and prophylactic tracheostomy. Since tracheostomy removal 3 days later, the patient remains asymptomatic.
Conclusions:
Tracheobronchopathia osteochondroplastica is a rare disease with usually benign clinical course and incidental diagnosis. It may present as acute hypercarbic respiratory failure when subglottic infection is superimposed.
MeSH Keywords: Abscess, Airway Obstruction, Asthma
Background
Tracheobronchopathia osteochondroplastica (TBO) is a benign cartilaginous proliferation of the central airway of unknown etiology. Its clinical course is usually indolent, and the larynx is usually spared. Symptoms are relatively rare – and upper airway obstruction even more so – and most cases of TBO are found incidentally during bronchoscopy performed for other indications or at autopsy. We report the first case in the literature of TBO presenting as acute respiratory failure due to superimposed subglottic submucosal abscess.
Case Report
A 27-year-old Egyptian man presented to the emergency department (ED) with dyspnea. He had noted dyspnea with exertion for 3 weeks, prompting 2 prior ED visits, 1 resulting in endotracheal intubation and treatment for suspected acute asthma exacerbation. He reported some improvement with these treatments but dyspnea with exertion persisted.
He was mildly tachypneic and tachycardic with oxygen saturation of 100% while breathing room air at rest. He received IV prednisolone and nebulized albuterol and ipratropium. Due to worsening respiratory distress associated with oxygen saturation of 85% and minimal air entry on auscultation, he underwent endotracheal intubation and mechanical ventilation. Direct laryngoscopy was unremarkable. Post-intubation arterial blood gas on FiO2 of 100% revealed a pH of 7.1; pCO2 76 mmHg; pO2 413 mmHg. No wheezing was noted. He was extubated within 24 hours.
Further interview revealed no history of atopy or symptoms of episodic dyspnea, wheezing, or cough prior to onset of dyspnea 3 weeks ago. There was no history of surgery or trauma. There was no family history of asthma. The patient denied fever, night sweats, weight loss, or hemoptysis. He had a 30-pack year smoking history. On exam, lungs were clear. Stridor was elicited with ambulation.
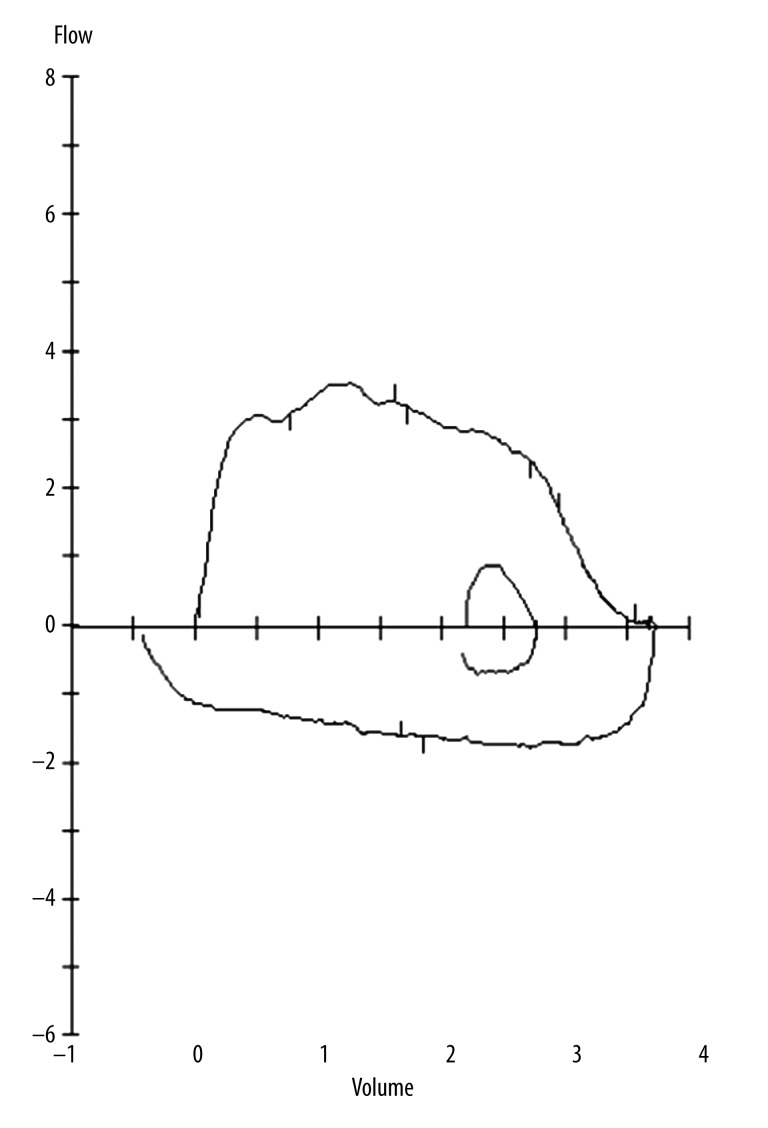
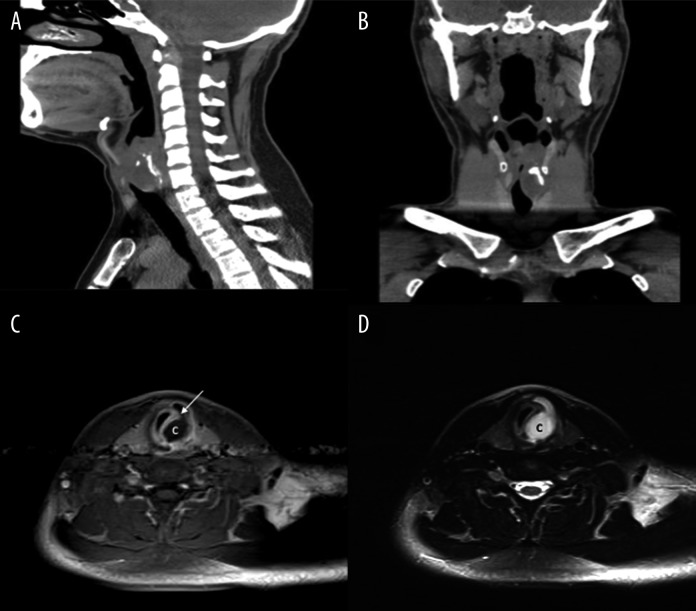
Flexible direct laryngoscopy revealed left vocal cord immobility with a normal epiglottis, clear vallecula and patent upper airway to the level of the cords. Spirometry (Figure 1) showed variable extra-thoracic upper airway obstruction. Computerized tomography (CT) of the neck (Figure 2A, 2B) revealed a 2.8×2.0×4.2 cm low-attenuation, partially calcified mass in the subglottic larynx protruding into the lumen with tracheal narrowing estimated at 75% and destruction of the arytenoid and cricoid cartilages. Neck magnetic resonance imaging (MRI) revealed that the mass had cystic and solid components, with enhancement of the solid component following contrast administration (Figure 2C, 2D), suggesting a tracheal chondrosarcoma.
Figure 1.
Flow Volume Loop. Flattening of inspiratory limb revealing variable extra-thoracic airway obstruction.
Figure 2.
Neck CT. Sagittal (A) and coronal (B) images showing a low-attenuation subglottic laryngeal mass containing calcifications and protruding into the lumen of the larynx with 75% luminal obstruction and destruction of the arytenoid and cricoid cartilage, Neck MRI. T1W post-contrast (C) and T2W (D) images showing a mixed solid and cystic submucosal mass in the subglottic larynx. The cystic component (c) shows low T1 and high T2 signal intensity, whereas the solid component (arrow) shows contrast enhancement.
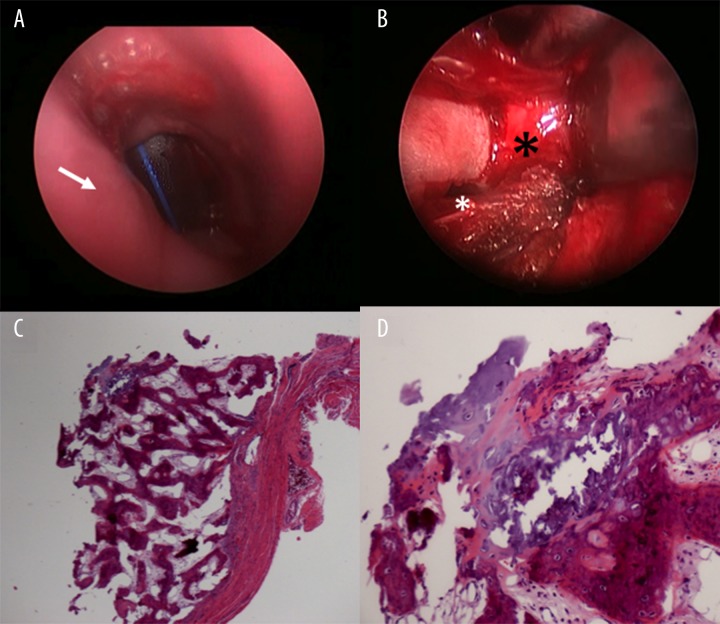
The patient underwent prophylactic tracheostomy and neck exploration. Laryngoscopy revealed left vocal cord fixation and immobility with submucosal fullness without mucosal abnormalities (Figure 3A). During elevation of the thyroid isthmus, sudden drainage of abundant purulent material was noted. Exploration revealed a defect along the left anterolateral cricoid wall in communication with a subglottic submucosal cavity (Figure 3B).
Figure 3.
Direct Laryngoscopy (A). Smooth subglottic mucosa, slight medial displacement of left subglottic wall, immediately lateral to the drained abscess pocket (arrow). In the distance, the tracheotomy tube is seen. Neck Exploration (B). Exposed left anterolateral aspect of cricoid lamina (black asterisk) showing an obvious defect within the wall (white asterisk), in communication with abscess pocket. Subglottic mass lining biopsy (C). Fibroconnective tissue with an attached nodular portion of bone and chondroid tissue (10×). (D) Transition of benign chondroid/cartilaginous and osseous/bony tissue favoring a benign chondro-osseous metaplastic process (40×).
The patient underwent successful tracheostomy removal 3 days postoperatively. Cultures were negative for bacteria, mycobacteria, and fungi. Pathology specimens (Figures 3C, 3D) were reviewed in our pathology consensus conference and revealed benign chondro-osseous metaplasia without fungal organisms or amyloid deposition compatible with TBO. Two weeks postoperatively, the patient was asymptomatic with unlimited exercise tolerance, although the left vocal cord remained fixed.
Discussion
Tracheobronchopathia osteochondroplastica (TBO) is a rare benign submucosal proliferation of cartilage and bone of the anterolateral wall of the central airway, and less frequently, the posterior wall [1]. The etiology of TBO is unknown. Chronic infections, irritants, metabolic disorders, and genetic predisposition have been proposed as causal factors. Most commonly asymptomatic or with minimal symptoms, it is usually diagnosed incidentally during bronchoscopy or autopsy [1,2]. When symptomatic, its presentation is related to the degree and location of airway obstruction.
The larynx is usually spared. Progressive deterioration of ventilatory function is not typical for TBO [3]. Upper airway obstruction due to subglottic laryngeal involvement of TBO is infrequent despite its narrow anatomy [4]. Differential diagnosis of subglottic stenosis includes congenital and acquired etiologies. In this case, the subacute onset and rapidly progressive symptoms make congenital causes less likely. Trauma accounts for the vast majority of cases of acquired subglottic stenosis.
In this case, the patient’s first intubation had occurred very recently after the onset of new respiratory symptoms and was very brief. Imaging did not show tracheal narrowing due to scar tissue but rather a subglottic mass causing upper airway narrowing. Other acquired etiologies include infections, neoplasms, and chronic inflammatory conditions such as granulomatous polyangiitis, relapsing polychondritis, and sarcoidosis. The lack of radiologic involvement of the tracheobronchial tree and presence of a single subglottic mass pointed towards a neoplastic process or superimposed infection. The latter was confirmed during surgical exploration. The pathologic findings confirmed TBO as the underlying chronic process.
Acute respiratory failure from upper airway obstruction may mimic acute asthma, laryngospasm, or angioedema. The lack of wheezing or history of atopy and the rapid resolution of hypercarbia with endotracheal intubation were suggestive of upper airway disease. The normal supraglottic anatomy by direct laryngoscopy during endotracheal intubation ruled out laryngospasm and angioedema as possible etiologies of respiratory failure. The benign clinical course of TBO has been well documented [1,3]. Acute presentation of TBO as a result of an ongoing infection [4–7] or progressive tracheal narrowing [1,3,8,9] is exceedingly rare. Acute [8] and imminent [10] respiratory failure due to upper airway obstruction caused by TBO has been reported. These cases were caused by rapidly progressive TBO causing severe tracheal stenosis over the course of a few weeks [8] or by near total occlusion of the upper airway due to a single tracheal mass caused by TBO [10].
The mechanism for respiratory failure in our patient differs significantly from the previously reported cases. Our patient exhibited pathologic findings compatible with TBO although the etiology of upper airway obstruction was caused by a superimposed subglottic infection.
Conclusions
This is the first report in the literature of a case of TBO presenting as acute respiratory failure due to superimposed subglottic submucosal abscess. Although a rare disease with a well-described benign course, TBO lesions have the potential to become superinfected and provoke severe upper airway obstruction and acute respiratory failure. This case report should serve as a reminder to clinicians to always question the etiology of acute respiratory failure in a patient with suspected asthma. The possibility of an underlying rare disease should never be discounted without thorough investigation.
Footnotes
Conflict of interest statement
All authors report no conflicts of interest. The views expressed in this manuscript do not communicate an official position of any scientific society, government agency, or funding source.
References:
- 1.Leske V, Lazor R, Coetmeur D, et al. Tracheobronchopathia osteochondroplastica: a study of 41 patients. Medicine (Baltimore) 2001;80:378–90. doi: 10.1097/00005792-200111000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bartwal MS, Chatterji RS, Mehta A. Tracheobronchopathia osteochondroplastica. Indian J Chest Dis Allied Sci. 2004;46:43–63. [PubMed] [Google Scholar]
- 3.Tukianen H, Torkko M, Terho EO. Lung function in patients with tracheobronchopathia osteochodroplastica. Eur Respi J. 1988;1:632–35. [PubMed] [Google Scholar]
- 4.Vilkman S, Keinstinen T. Tracheobronchopathia osteochondroplastica: a report of a young man with severe disease and retrospective review of 18 cases. Respiration. 1995;62:151–54. doi: 10.1159/000196411. [DOI] [PubMed] [Google Scholar]
- 5.Hantous-Zannad S, Sebai L, Zidi A, et al. Tracheobronchopathia osteochrondroplastica presenting as a respiratory insufficiency: disgnosis by bronchoscopy and MRI. Eur J Radiol. 2003;45:113–16. doi: 10.1016/s0720-048x(02)00028-1. [DOI] [PubMed] [Google Scholar]
- 6.de Wall N, Roggenbuck C, Endres P, et al. Tracheobronchopathia osteochondroplastica and coexisting mucoepidermoif carcinoma of the lung: Case report. Pneumologie. 1992;46(2):74–77. [PubMed] [Google Scholar]
- 7.Lobo R, Mulloy EM. An unusual cause of recurrent chest infection. BMJ Case Rep. 2012 Oct;2012:pii. doi: 10.1136/bcr-2012-006910. bcr2012006910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Molloy AR, McMahon JN. Rapid progression of tracheal stenosis associated with trachobronchopathia osteochondroplastica. Intensive Care Med. 1988;14:60–62. doi: 10.1007/BF00255642. [DOI] [PubMed] [Google Scholar]
- 9.Raess PW, Cowan SW, Haas AR, et al. Tracheobronchopathia osteochondroplastica presenting as a single dominant tracheal mass. Ann Diagn Pathol, 201. 15:431–35. doi: 10.1016/j.anndiagpath.2011.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Raess PW, Cowan SW, Haas AR, et al. Trachobronchopathia osteochondroplastica presenting as a single dominant tracheal mass. Ann Diagn Pathol. 2011;15:431–35. doi: 10.1016/j.anndiagpath.2011.04.009. [DOI] [PubMed] [Google Scholar]