Abstract
Background
Randomized, controlled trials have shown that nurse-led disease management for patients with heart failure can reduce hospitalizations. Less is known about the cost-effectiveness of these interventions.
Objective
To estimate the cost-effectiveness of a nurse-led disease management intervention over 12 months, implemented in a randomized, controlled effectiveness trial.
Design
Cost-effectiveness analysis conducted alongside a randomized trial.
Data Sources
Medical costs from administrative records, and self-reported quality of life and nonmedical costs from patient surveys.
Participants
Patients with systolic dysfunction recruited from ambulatory clinics in Harlem, New York.
Time Horizon
12 months.
Perspective
Societal and payer.
Intervention
12-month program that involved 1 face-to-face encounter with a nurse and regular telephone follow-up.
Outcome Measures
Quality of life as measured by the Health Utilities Index Mark 3 and EuroQol-5D and cost-effectiveness as measured by the incremental cost-effectiveness ratio (ICER).
Results of Base-Case Analysis
Costs and quality of life were higher in the nurse-managed group than the usual care group. The ICERs over 12 months were $17 543 per EuroQol-5D–based quality-adjusted life-year (QALY) and $15 169 per Health Utilities Index Mark 3–based QALY (in 2001 U.S. dollars).
Results of Sensitivity Analysis
From a payer perspective, the ICER ranged from $3673 to $4495 per QALY. Applying national prices in place of New York City prices yielded a societal ICER of $13 460 to $15 556 per QALY. Cost-effectiveness acceptability curves suggest that the intervention was most likely cost-effective for patients with less severe (New York Heart Association classes I to II) heart failure.
Limitation
The trial was conducted in an ethnically diverse, inner-city neighborhood; thus, results may not be generalizable to other communities.
Conclusion
Over 12 months, the nurse-led disease management program was a reasonably cost-effective way to reduce the burden of heart failure in this community.
Health care administrators and policymakers are increasingly turning to nurse-led disease management to lessen the economic and health burden of chronic diseases, such as heart failure. Meta-analyses of randomized, controlled trials (RCTs) suggest that nurse management can be effective at reducing rehospitalization and sometimes at improving functioning (1). To our knowledge, however, no previous RCT has included a cost-effectiveness analysis sufficient to inform policymakers as to whether nurse management improves quality of life for patients with heart failure at a reasonable cost to society. Studies have not followed recommended cost-effectiveness guidelines or thoroughly calculated intervention costs (2). Establishing the cost-effectiveness of nurse management for heart failure may be especially important in minority communities, which have disproportionate rates of hospitalization for heart failure (3) and shortfalls in the use of proven effective therapies (4) and in patients’ understanding of heart failure (5).
We aimed to estimate the cost-effectiveness of a nurse-led disease management intervention that was conducted alongside a randomized, controlled effectiveness trial. The trial, conducted in Harlem, New York, from 1999 to 2003, found that patients in the nurse-managed group maintained better physical functioning, as measured by the Short Form-12 (SF-12) physical component score, and had statistically significantly fewer hospitalizations than did patients in the control group (6).
Methods
For the RCT, we recruited patients from outpatient clinics at the 4 hospitals serving East and Central Harlem in New York City. We randomly assigned 406 patients to usual care (203 patients) or a nurse-led program (203 patients) in which patients had 1 in-person visit with a trained nurse and periodic follow-up telephone calls over 12 months (6). The nurses stressed adherence to a low-salt diet and to medications and worked with the patient’s physician to optimize heart failure medications according to published guidelines. Primary outcomes were total hospitalizations and physical functioning as measured by the SF-12 physical component score. Trained surveyors who were blinded to treatment assignment called patients in both groups every 3 months for 18 months to administer the SF-12 and collect information on health care utilization, amount of informal care received, and patients’ estimates of their time engaged in receiving health care over the past 3 months.
We measured cost-effectiveness by using the incremental cost-effectiveness ratio (ICER), which is the difference in average costs between the nurse-managed and usual care groups (CostN – CostUC) divided by the difference in mean quality-adjusted life-years (QALYs) (QALYN – QALYUC):
ICER = (CostN – CostUC)/(QALYN – QALYUC)
QALYs
We estimated QALYs for the 12-month intervention by translating the SF-12 physical and mental component scores into Health Utility Index Mark 3 (HUI3) and Euro-Qol-5D (EQ-5D) quality-of-life scores by using methods described by Franks and colleagues (7). We chose these translations over other published methods (8–10) because they were validated in African-American patients, and most of the patients in our trial were African American or Hispanic. Patients who died were assigned a quality-of-life score of 0 in subsequent periods. We calculated QALYs by connecting the 5 quality-of-life scores for each patient (baseline and quarterly through 12 months) by using straight lines and calculating the area of the resulting 4 trapezoids. We estimated adjusted differences in QALYs by the coefficient on treatment from a linear regression of each patient’s QALY on his or her quality-of-life score at baseline and treatment assignment (11).
Societal Costs
We followed guidelines for cost-effectiveness analysis (2) to estimate costs from a societal perspective and included intervention, medical, and nonmedical costs (Appendix Table, available at www.annals.org). Intervention costs included all intervention materials (for example, scales), telephone service for 2 patients who did not have it, patients’ transportation costs to the initial nurse meeting, nurses’ salaries and fringe benefits, physician time overseeing the nurse activities, and costs for office space and equipment used by the nurses.
Appendix Table.
Data Sources and Imputations for Cost Items
| Cost Component | Data Source for Units | Data Sources and Imputations for Price per Unit |
|---|---|---|
| Direct medical utilization | ||
| Hospital | ||
| Participating hospitals | Administrative data | Charges multiplied by cost-to-charge ratio from CMS cost reports; for physician charges, assume 1 initial physician visit at $157 (CPT 99223) plus 1 follow-up visit at $57 (CPT 99232) per day for length of stay* |
| Nonparticipating sites | PS: “In the past 3 months, how many times were you admitted to that (other) hospital?” | Number of admissions times the average cost per admission from participating hospitals ($7475), plus 1 initial physician visit at $157 (CPT 99223) and 1 follow-up visit at $57 (CPT 99232) per day for 5 additional days |
| Outpatient physician visits | ||
| Participating sites | CPT evaluation and management codes from administrative data | Medicare Physician Fee schedule* and Hospital Outpatient facility charge for APC 601 ($50)† |
| Nonparticipating sites | PS: “In the past 3 months, how many times, if any, did you see medical doctors outside of [recruiting site]?” | Average charge per outpatient visit from billing data ($52) applied to number of encounters from the survey |
| Emergency department | ||
| Participating emergency departments | Administrative data | Charged amount |
| Nonparticipating emergency departments | PS: “In the past 3 months, how many times in total did you go to the other ERs?” | Average charge from billing data ($202) applied to number of encounters from survey, plus a physician charge of $95 (CPT 99284) |
| Medications | ||
| Prescription medications | Units from drugs prescribed, abstracted from patients’ charts | Prices for each prescription from average payment, including dispensing fee, by state Medicaid programs for each medication |
| Over-the-counter medications | PS: “In the past 3 months, how much did you spend in total on these over-the-counter medications?” | Reported amount |
| Other direct medical utilization | ||
| Physician home visits | PS: “In the past 3 months, how many times has this type of provider come to your home to help you? … A doctor for a home visit?” | $140 per visit based on Medicare fee schedule for CPT 99343 in New York City in 2001 |
| Nurse home visits | PS: “… A visiting nurse?” | $70 per visit; estimate based on cost of physician home visit and relative wages for GPs and internists versus nurses in New York City‡ |
| Home health aid visits | PS: “… A home health aide or attendant?” | $47 per visit; estimate based on cost of physician home visit and relative wages for GPs and internists versus home health aides in New York City‡ |
| Medical equipment | PS: “In the past 3 months, did you buy or rent any medical equipment, such as a wheelchair, etc. [specify]?” | The specified equipment times the prices of equipment from BETOS codes D1A–D1F§ |
| Nursing home | PS: “In the past 3 months, how many days, if any, were you a patient in a nursing home or any other similar place that provides long-term care?” | Number of days times $176/dǁ |
| Physician telephone calls | PS: “In the past 3 months, how many times have you talked on the telephone with a medical doctor?” | Assumed a 10-min conversation and an hourly wage of $49, which is wage for GPs and internists in New York City‡ |
| Telephone calls with other health providers | PS: “In the past 3 months, how many times have you talked on the telephone with providers who are not medical doctors?” | Assumed a 10-min call and an average hourly wage of $28, which is employment-weighted average wage for various “other health professionals” in New York City‡ |
| Other outpatient procedures or laboratory tests | CPT codes from administrative data | Medicare fee schedule* |
| Direct nonmedical | ||
| Housekeeper | PS: “In the past 3 months, how many times has this type of provider come to your home to help you? … A housekeeper?” | $24 per visit (2-h visit times $12/h)‡ |
| Other | PS: “… Any other person not mentioned above?” | $24 per visit (2-h visit times $12/h)‡ |
| Transportation | PS: “In the past 3 months, which of the following did you usually use to get to doctors’ appointments: walking, bus, subway, driving, ambulette, ambulance?” (Number of medical encounters calculated from PS and administrative data) |
Bus or subway ($3); ambulance ($283); ambulette ($100); taxi ($2 plus $1.50/mile) |
| Patient time | ||
| Time traveling to medical encounters | PS: “In the past 3 months, which of the following did you usually use to get to doctors’ appointments: walking (30 min/mile); bus or subway (5 min/mile); driving, ambulette, or ambulance (2 min/mile)?” |
Sex- and age-specific wage rates¶ |
| Time spent in medical care | Emergency department visits (180 min/visit) plus outpatient visits (60 min/visit) plus telephone consultations (10 min/call) | Sex- and age-specific wage rates¶ |
| Intervention costs | ||
| Patient cost for initial visit | Transportation and patient time (2 h) | Car service to appointment ($15); Metro card to return home ($1.50); sex- and age-specific wage rates for patient time¶ |
| Nurse salary | Nurses’ logs for percentage of time per month on intervention | Nurses’ annual salaries and fringe benefit rate multiplied by percentage of full-time equivalent on intervention |
| Physicians, principal investigator, project manager | Timesheets of investigators for time associated with developing the intervention and overseeing the nurse activities | Individual’s annual salary and fringe benefit rate multiplied by percentage of full-time equivalent on intervention |
| Patient supplies | Scales, booklets; telephone and service for 3 patients, toll-free 800 service | Billed amount for supplies; $10 paid per telephone; $22 per patient-month for telephone service; telephone company prices |
| Nurse equipment | Computers, binders, pagers | Billed amount |
| Overhead | Square feet of office space for 3.72 full-time equivalent nurses | Mount Sinai–estimated cost of per full-time equivalent staff person, $12 000 |
APC = Ambulatory Payment Classification; BETOS = Berenson-Eggers Type of Service; CMS = Centers for Medicare & Medicaid Services; CPT = Current Procedure Terminology; ER = emergency room; GP = general practitioner; PS = patient survey.
Data from reference 14.
Data from reference 35.
Data from reference 36.
Data from reference 37.
Data from reference 38, updated to 2001 U.S. dollars.
Data from reference 39.
We derived medical costs for inpatient, outpatient, and emergency department use from administrative records from the 4 hospitals that participated in the trial. For inpatient costs, we converted billed charges to costs by using the cost-to-charge ratio for each hospital (2, 12) and converted the costs to 2001 U.S. dollars by using the Producer Price Index for general and surgical hospitals (13). For outpatient and emergency department claims, we applied the 2001 Medicare fee schedule for the New York City region (14) to billed procedure codes. For medication costs, we obtained medications prescribed from patients’ charts and prices for those medications from the average prices paid by Medicaid (15).
We used quarterly patient surveys to collect information on inpatient and outpatient utilization at nonparticipating institutions (to supplement administrative records from participating hospitals) and information on nonmedical costs, which included nursing home stays; patient transportation and time costs associated with medical encounters; and costs of informal care or assistance with household chores provided by friends, family members, or paid housekeepers. Costs are reported in 2001 U.S. dollars.
Because of skewed cost data and a high percentage of patients with zero costs for many cost categories, we evaluated the statistical significance of the difference in costs between nurse-managed and usual care groups by using 2-part gamma models (16). In the first part, we estimated the probability of costs being greater than 0 by logistic regression, with treatment assignment; age; sex; race (non-Hispanic black, non-Hispanic white, or other non-Hispanic); Hispanic ethnicity; recruitment site; education; preference for Spanish interview; New York Heart Association (NYHA) heart failure class; and indicators for diabetes, chronic pulmonary disease, and ischemic heart disease as explanatory variables. In the second part, for patients with costs greater than zero, we modeled costs as a function of the same explanatory variables by using generalized linear models with a gamma distribution and a logarithmic link function. For nursing home costs, which had a very small probability of being greater than 0, we calculated unadjusted differences in mean costs and bootstrapped SEs by using 500 replicates stratified by treatment.
We replaced missing observations for SF-12 scores and self-reported utilization with 10 imputed values found by using imputation by chained equations (17) as implemented by the ICE command in Stata, version 10.0 (StataCorp, College Station, TX) (18). The previously listed explanatory variables at baseline and administrative data for hospitalizations and outpatient visits at baseline and quarterly follow-up were regressors in these equations. We estimated the 2-part models described previously on each imputed data set and combined the results by using Rubin’s rules (19).
Uncertainty in the ICER
We created 500 bootstrapped replicates (50 from each of the 10 imputations) and plotted the corresponding cost-effectiveness acceptability curves (20). We calculated approximate empirical CIs for the ICER by using the bootstrap percentile method (21). To explore whether nurse management is more likely to be cost-effective for patients with varying heart failure severity, we computed separate acceptability curves according to baseline NYHA class.
Sensitivity Analysis
We estimated costs on the basis of national prices for all cost items. We used the national 2001 Medicare fee schedule to calculate costs for outpatient and emergency department use (14), deflated costs for hospitalizations and self-reported medical use by the ratio of the United States to New York metropolitan area Consumer Price Index for medical care, and deflated nonmedical costs by the ratio of the United States to New York metropolitan area Consumer Price Index for urban dwellers (22).
To characterize the cost implications from the payer’s perspective, we also calculated costs to the Medicare program on the basis of categories and proportions of societal costs that Medicare typically covers. These included intervention costs but excluded costs for nursing home stays, patient time, telephone consultations, nonphysician office visits, and informal care. We decreased payer costs by the deductible and copayment rates for Medicare beneficiaries in 2001. We included drug costs because Medicare and most insurers now cover medications. We assumed the deductible and copayment rate of the 2006 Medicare prescription drug plan, but no coverage gap.
We investigated the influence of imputing missing survey data on the results by reporting the ICER for the observed data only (available data analysis) for patients who responded to every quarterly telephone survey until death or 12 months (complete case analysis) and for a data set in which a patient’s missing observations were replaced with the mean value of that patient’s observed responses (patient-specific imputation).
We conducted all analyses in Stata, version 10 (18). The study was approved by institutional review boards at each participating institution.
Results
The sample of 203 usual care and 203 nurse-managed patients consisted mostly of black and Hispanic patients of lower socioeconomic status (Table 1). Most (59%) had NYHA class III or IV heart failure, the most severe classes of heart failure. Functional status at baseline as measured by the SF-12 physical and mental component scores and costs in the 3 months before randomization did not differ statistically significantly between groups.
Table 1.
Selected Patient Characteristics at Baseline
| Characteristic | All Patients | Usual Care Group | Nurse Management Group |
|---|---|---|---|
| Patients, n | 406 | 203 | 203 |
| Mean age (SD), y | 59.4 (13.7) | 59.3 (13.7) | 59.6 (13.8) |
| Race, n (%) | |||
| Non-Hispanic white | 62 (15) | 31 (15) | 31 (15) |
| Non-Hispanic black | 186 (46) | 90 (44) | 96 (47) |
| Hispanic | 132 (33) | 72 (35) | 60 (30) |
| Other | 26 (6) | 10 (5) | 16 (8) |
| Women, n (%) | 188 (46) | 97 (48) | 91 (45) |
| Interviewed in Spanish, n (%) | 92 (23) | 51 (25) | 41 (20) |
| Education, n (%) | |||
| Less than high school | 187 (46) | 101 (50) | 86 (42) |
| High school graduate | 105 (26) | 47 (24) | 58 (15) |
| Greater than high school | 108 (27) | 52 (26) | 56 (28) |
| New York Heart Association class, n (%) | |||
| I | 75 (18) | 39 (19) | 36 (18) |
| II | 91 (22) | 41 (20) | 50 (25) |
| III | 57 (14) | 24 (12) | 33 (16) |
| IV | 183 (45) | 99 (49) | 84 (41) |
| Selected comorbid conditions, n (%) | |||
| Charlson Comorbidity Index score | 1.9 (3.1) | 3.2 (1.9) | 3.0 (1.9) |
| Diabetes | 155 (38) | 81 (40) | 74 (36) |
| Chronic pulmonary disease | 126 (31) | 58 (29) | 68 (33) |
| Ischemic disease | 182 (45) | 97 (48) | 85 (42) |
| Mean functional status at baseline (SD) | |||
| SF-12 physical component score | 39.2 (9.1) | 38.8 (9.0) | 39.5 (9.2) |
| SF-12 mental component score | 48.7 (10.9) | 48.4 (10.9) | 49.0 (10.9) |
| Mean costs in 3 months before randomization (SD), $* | |||
| Medical | 3285 (7585.9) | 3400 (7585.5) | 3171 (6222.9) |
| Nonmedical | 240 (560.7) | 254 (587.7) | 226 (533.7) |
| Patient time | 112 (283.2) | 115 (329.4) | 110 (228.8) |
| Total | 3638 (7145.1) | 3768 (7775.8) | 3509 (6470.0) |
SF-12 = Short Form-12.
Costs in 2001 U.S. dollars.
QALYs during the Intervention
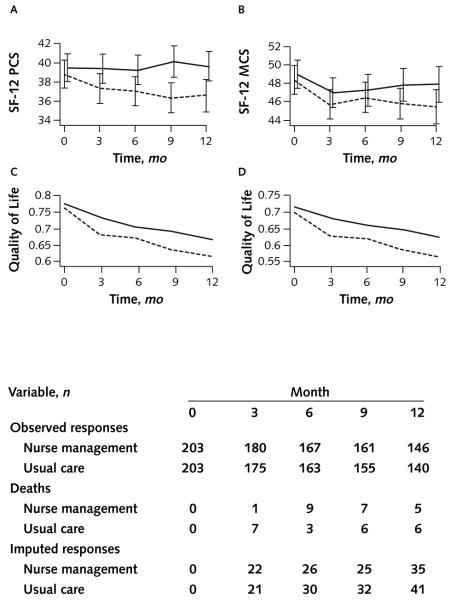
Patients in the nurse-managed group maintained better physical functioning throughout the 12-month intervention than did patients who received usual care (Figure 1). Mental health did not differ statistically significantly by group. Each group had 22 deaths. Loss to follow-up was considerable in both groups, resulting in the need by month 12 to impute 35 and 41 SF-12 scores for nurse-managed and usual care patients, respectively. Translating the SF-12 scores into quality-of-life scores yielded higher quality of life in every period in the nurse-managed group. The difference in the area under these curves represents the increment in QALYs, and that difference was 0.0497 QALY per person for the HUI3 and 0.0430 QALY per person for the EQ-5D. Other translations of the SF-12 into QALYs (8–10) yielded similar results, which are available from the authors.
Figure 1.
Functioning and quality-of-life scores for patients in the nurse management (solid lines) and usual care (dashed lines) groups.
A and B. Mean Short Form-12 (SF-12) physical component score (PCS) and mental component score (MCS), by month and treatment group. Vertical bars represent SEs. C and D. Mean quality-of-life scores as measured by translation of SF-12 scores into EuroQol-5D and Health Utility Index Mark 3, by month and treatment group. We assigned deceased patients quality-of-life scores of 0.
Incremental Costs
Intervention costs totaled $2177 per patient. Nurse time ($1506 per patient) and physician and other investigator time ($232 per patient) were the largest cost components.
No cost categories statistically significantly differed between groups during the intervention, except for outpatient procedures, which were more costly in the nurse-managed group (Table 2). Lower costs per person for hospitalizations in the nurse-managed group were partially offset by higher costs for outpatient procedures and laboratory services and home care costs. Higher nursing home costs among nurse-managed patients were attributable largely to 2 patients who entered a nursing home within the first 3 months of the study. Higher physician home visit costs were due mainly to 1 nurse-managed patient who used home care extensively.
Table 2.
Utilization and Costs during the 12-Month Intervention, by Treatment Group*
| Intervention | Usual Care Group |
Nurse Management Group |
Difference: Nurse Management Minus Usual Care |
||||
|---|---|---|---|---|---|---|---|
| Value, n | Cost per Patient, $ |
Value, n | Cost per Patient, $ |
Value, n | Cost per Patient, $ |
P
Value† |
|
| Direct medical utilization | |||||||
| Hospitalizations at participating hospitals | 180 | 12 014 | 143 | 10 204 | −37 | −1809 | 0.84 |
| Hospitalizations at other hospitals | 55 | 2137 | 40 | 1568 | −15 | −569 | 0.44 |
| Physician visits at participating clinics | 1459 | 642 | 1530 | 651 | 71 | 9 | 0.123 |
| Physician visits at other clinics | 807 | 206 | 623 | 159 | −185 | −47 | 0.136 |
| Emergency department use at participating sites | 157 | 69 | 147 | 69 | −10 | −1 | 0.79 |
| Emergency department use at other sites | 98 | 144 | 80 | 117 | −18 | −27 | 0.82 |
| Prescription and over-the-counter drugs | − | 1342 | − | 1364 | − | 22 | 0.94 |
| Other direct medical utilization | |||||||
| Physician home visits | 39 | 27 | 125 | 86 | 85 | 59 | 0.27 |
| Nurse home visits | 1612 | 556 | 1848 | 637 | 236 | 81 | 0.77 |
| Home health aide visits | 8286 | 1918 | 8625 | 1997 | 339 | 79 | 0.29 |
| Medical equipment | − | 13 | − | 17 | − | 5 | 0.99 |
| Nursing home stays | 61 | 53 | 711 | 617 | 651 | 564 | 0.092 |
| Physician telephone calls | 746 | 30 | 840 | 34 | 94 | 4 | 0.45 |
| Nonphysician office visits | 1057 | 48 | 1211 | 55 | 153 | 7 | 0.94 |
| Other procedures or laboratories, claims | 807 | 329 | 820 | 555 | 13 | 226 | 0.012 |
| Direct nonmedical utilization | |||||||
| Patient trips to or from clinic, emergency department, or hospital | 7153 | 946 | 7180 | 937 | 27 | −9 | 0.56 |
| Relative, friend, or neighbor visits for help | 7327 | 866 | 7940 | 939 | 614 | 73 | 0.48 |
| Housekeeper visits | 2656 | 314 | 1776 | 210 | −880 | −104 | 0.99 |
| Patient time involved in medical care, h | 7387 | 479 | 7542 | 494 | 155 | 16 | 0.62 |
| Cost of the intervention | − | 0 | − | 2177 | 0 | 2177 | − |
| Total societal costs | − | 22 134 | − | 22 888 | − | 754 | 0.73 |
| Cost to payer | − | 17 680 | − | 17 838 | − | 158 | 0.79 |
Costs are 2001 U.S. dollars.
P value is for the analysis of differences in costs from 2-part models.
ICER
The 12-month incremental cost per QALY gained—the ICER—was $17 543 for the estimate of quality of life based on translation of the SF-12 to the EQ-5D and $15 169 for translation to HUI-3 (Table 3). Adjustment for the small, statistically insignificant differences in quality of life between groups at baseline increased these estimates to $21 470 and $19 691, respectively. From the perspective of a payer like Medicare, the incremental net cost over 12 months of implementing this program was $158 per patient enrolled and $3673 and $3176 per QALY for EQ-5D–derived and HUI-3-derived quality of life, respectively (Table 3).
Table 3.
Incremental Costs, Quality-Adjusted Life-Years, and Incremental Cost-Effectiveness Ratios for Nurse Management versus Usual Care during the 12-Month Intervention*
| Variable | Usual Care Group |
Nurse Management Group |
Difference: Nurse Management Minus Usual Care (95% CI) |
Adjusted Difference: Nurse Management Minus Usual Care (95% CI)† |
|---|---|---|---|---|
| Deaths, n | 22 | 22 | 0 | – |
| Mean life-years | 0.9463 | 0.9528 | 0.0065 | – |
| Mean QALYs | ||||
| EuroQol-5D | 0.6651 | 0.7080 | 0.0430 (0.0012 to 0.0848) | 0.0351 (0.0004 to 0.0698) |
| Health Utilities Index Mark 3 | 0.6122 | 0.6619 | 0.0497 (0.0054 to 0.0940) | 0.0383 (0.0035 to 0.0731) |
| Mean societal costs, $ | 22 134 | 22 888 | 754 (−6963 to 8472) | – |
| ICER: societal perspective, $/QALY | ||||
| EuroQol-5D | – | – | 17 543 (−139 295 to 458 900) | 21 470 (−96 156 to 350 058) |
| Health Utility Index Mark 3 | – | – | 15 169 (−114 748 to 282 657) | 19 691 (−159 887 to 379 482) |
| ICER: payer perspective | ||||
| Mean payer costs, $ | 17 680 | 17 838 | 158 (−7230 to 7546) | |
| EuroQol-5D, $/QALY | – | – | 3673 (−156 085 to 379 855) | 4495 (−184 228 to 375 295) |
| Health Utilities Index Mark 3, $/QALY |
– | – | 3176 (−135 581 to 238 659) | 4123 (−216 488 to 1585 43) |
ICER = incremental cost-effectiveness ratio; QALY = quality-adjusted life-year.
Costs are 2001 U.S. dollars.
Adjusted difference is the coefficient on treatment assignment from a linear regression of QALYs over 12 months on baseline quality-of-life score and treatment assignment. 95% CIs for ICERs and costs were bootstrapped.
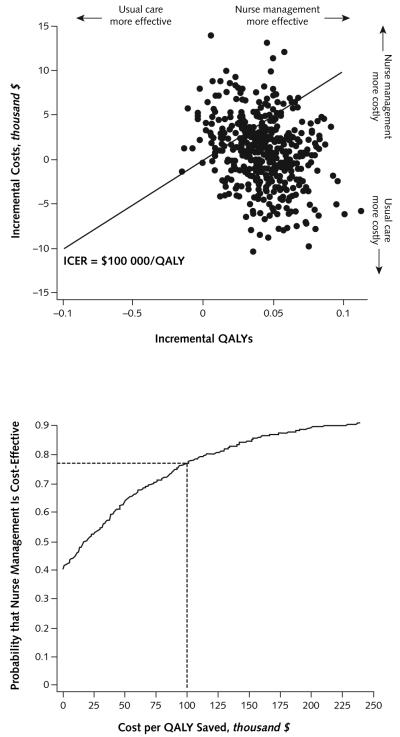
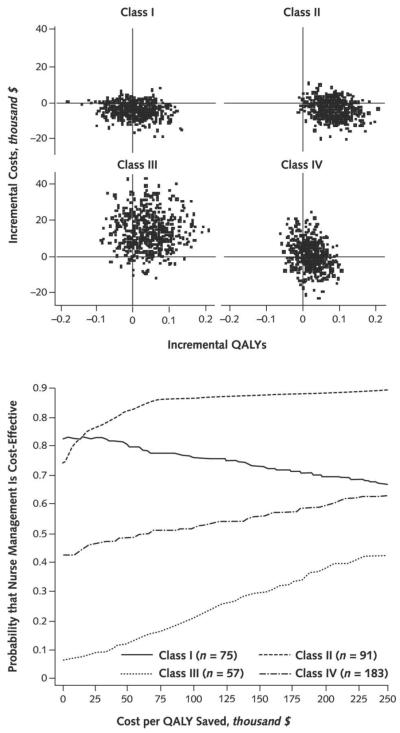
Figure 2 (top) shows 500 bootstrapped replicates of incremental costs and incremental QALYs with a diagonal line representing all points with an ICER of $100 000 per QALY. The corresponding cost-effectiveness acceptability curve (bottom) suggests 64% and 77% probabilities that nurse-led management is cost-effective, at $50 000 per QALY and $100 000 per QALY, respectively. Figure 3 shows similar plots by NYHA class, with probabilities of cost-effectiveness at $100 000 per QALY of 76%, 97%, 21%, and 52% for patients with baseline NYHA classes I through IV, respectively.
Figure 2.
Five hundred bootstrapped replicates of incremental costs and incremental quality-adjusted life-years (QALYs) for nurse management versus usual care (top) and the resulting cost-effectiveness acceptability curve (bottom).
ICER = incremental cost-effectiveness ratio.
Figure 3.
Five hundred bootstrapped replicates of incremental costs and incremental quality-adjusted life-years (QALYs) for nurse management versus usual care (top) and the resulting cost-effectiveness acceptability curve (bottom), by New York Heart Association class at baseline.
Sensitivity Analyses
Limiting the sample only to patients who completed all survey rounds before they died or during 12 months suggested that the intervention improved quality of life and saved costs (Table 4). Limiting the sample to only observed responses resulted in an ICER of $18 599 per QALY (Table 4), and replacing missing observations with patient-specific mean resulted in an ICER of $27 992 per QALY.
Table 4.
Sensitivity Analysis of the Effects of Alternative Treatment of Unit Prices and Missing Observations on the ICER
| Effect | Difference in QALYs: Nurse Management Minus Usual Care (95% CI)* |
Difference in Societal Costs: Nurse Management Minus Usual Care (95% CI), $† |
ICER (95% CI), $/QALY† |
|---|---|---|---|
| Alternative treatments for missing data | |||
| Multiple imputation by chained equations (base case) |
0.0430 (0.0012 to 0.0848) | 754 (−6963 to 8472) | 17 543 (−139 295 to 458 900) |
| Patient-specific mean imputation of missing data |
0.0354 (−0.0054 to 0.0766) | 990 (−7045 to 8922) | 27 992 (−228 614 to 13 000 000) |
| Complete cases only | 0.0614 (0.0147 to 0.1019) | −612 (−5809 to 3694) | Cost-saving |
| Available data only | 0.0462 (0.0017 to 0.0860) | 859 (−6870 to 8597) | 18 599 (−120 716 to 342 654) |
| U.S. prices versus New York City prices | |||
| QALYs based on EQ-5D (base case) | 0.0430 (0.0012 to 0.0848) | 669 (−6640 to 7978) | 15 556 (−133 617 to 433 891) |
| QALYs based on HUI3 | 0.0497 (0.0054 to 0.0940) | 669 (−6640 to 7978) | 13 460 (−109 610 to 265 911) |
EQ-5D = EuroQol-5D; HUI3 = Health Utilities Index Mark 3; ICER = incremental cost-effectiveness ratio; QALY = quality-adjusted life-year.
QALYs measured by translation of Short Form-12 scores into EQ-5D scores unless otherwise noted.
Costs are 2001 U.S. dollars.
Using national prices to calculate costs yielded ICER estimates of $15 556 and $13 460 per QALY gained, where the QALYs were measured by the EQ-5D and HUI3 methods, respectively (Table 4).
Discussion
A nurse-led disease management program for patients with heart failure improved quality of life at an expected cost to society of less than $25 000 per QALY gained. The intervention costs of $2177 per patient were more than offset by reduced hospital costs ($2378 per patient), but higher costs for outpatient procedures, medications, and home health care prevented the intervention from being cost-saving over the 12-month study.
At less than $25 000 per QALY, nurse-led disease management for heart failure lies within the range usually considered a reasonable cost to gain 1 year of healthy life. Among studies from 1976 to 1996 that met an expert panel’s criteria for creditable cost-effectiveness analysis, the median cost per QALY gained, translated to 2001 U.S. dollars, was $21 967 for health education and counseling interventions and $15 771 for interventions related to the circulatory system (23). The lowest estimate of society’s willingness to pay for 1 QALY from an analysis of the value-of-life literature was $28 811 (translated to 2001 U.S. dollars) (24).
To our knowledge, this is the first cost-effectiveness analysis for nurse management of heart failure to include all recommended categories of cost. An English-language MEDLINE search (25 May 2008) found 6 U.S. RCTs of nurse management for heart failure that presented costs. One that reported all costs except patient time found that statistically significantly lower hospital costs in the nurse group were offset by higher intervention and caregiver costs, resulting in statistically insignificant total cost differences (25). Two studies that limited their cost analyses to inpatient care reported lower inpatient charges through 12 months or lower diagnosis-related group payments through 24 months among intervention patients (26, 27). Two studies that excluded the cost of the intervention or other cost categories found no cost difference among treatment groups (28, 29).
A recent study conducted in San Antonio that took a health care system perspective reported no difference in direct medical costs and an ICER of $95 721 per QALY (2003 U.S. dollars) for patients with systolic dysfunction and $67 784 per QALY for patients with NYHA class III or IV symptoms (30). These latter results contrast starkly with our study, which found better evidence of cost-effectiveness for patients with NYHA class I and II heart failure. As Figure 3 shows, for patients with NYHA class I heart failure there was little evidence that the intervention improved QALYs; bootstrapped replicates of incremental costs and QALYs were scattered on either side of the vertical line for zero difference in QALYs. However, most points were below the zero-cost line, which suggests that the intervention reduced costs for patients with NYHA class I heart failure. This is reflected in the high but downward-sloping acceptability curve for patients with NYHA class I heart failure (Figure 3, bottom). The height of the curve at $0 per QALY shows that if society were unwilling to incur any additional costs to improve quality of life—that is, were we interested only in reducing costs—then nurse management for patients with NYHA class I heart failure is more likely to be acceptable, because 80% of the replicates suggest cost savings. The curve slopes downward because as society values interventions that improve QALYs more, the apparent ineffectiveness of the intervention for patients with NYHA class I heart failure reduces the likelihood that it is cost-effective. In contrast, patients with class II heart failure at baseline generally showed both higher QALYs and lower costs from the intervention and a high probability of cost-effectiveness for any maximum acceptable value of costs per QALY. Patients with class III or IV heart failure showed improved QALY but also had higher costs. The cost-effectiveness acceptability curves suggest relatively low probability that the intervention was cost-effective for these patients.
Our findings contrast with those of the San Antonio study because patient functioning in that study decreased in both treatment groups (31), whereas physical functioning in our study was maintained in the nurse-managed group over the 12-month intervention. As Figure 1 shows, the intervention yielded higher quality of life by forestalling the decline in physical functioning. This was especially true for patients with NYHA class II heart failure, resulting in a higher likelihood of cost-effectiveness for these patients. The intervention in the San Antonio study affected primarily survival among patients with systolic dysfunction and class III or IV heart failure. Dissimilar interventions and study populations may have contributed to these disparate results. The San Antonio study sample was 72% white, and 30% had diastolic dysfunction compared with our sample, which was 15% white and had only systolic heart failure. The nurse-led intervention in the former study was purely telephonic, whereas that in our study required an initial face-to-face patient meeting.
Our study has several limitations. We did not project costs and quality of life past the end of the 12-month intervention. Data from the main trial suggested that patients’ SF-12 scores deteriorated after 12 months—when the nurses stopped working with the patients (6). If the intervention has no durable effects on quality of life or costs, then the figures we present are reasonable estimates of the long-run cost effectiveness of a 12-month intervention, although we do not know the implications of continuing the intervention.
We conducted the trial in an ethnically diverse, inner-city neighborhood, and these results may not be generalizeable to other settings. Nevertheless, because heart failure is a major cause of death and disability in these communities (3, 32, 33), our findings are valuable and relevant to a large group of vulnerable patients with heart failure. Finally, the sizeable number of survey nonresponses required that we impute a large number of cost items and quality of life, although the sensitivity analyses suggest that the approach we took yielded reasonable results.
Given their established relationships with patients, hospital-based providers may be the most effective entity to administer a nurse management program. Financial considerations for providers, however, may inhibit the adoption of such a program, even one that is likely to improve health-related outcomes and is cost-effective from a societal perspective. Under mainstream U.S. payment arrangements that do not pay for disease management, a hospital-based program would add the costs of the nurse managers to hospital expenses and would also reduce hospital revenues through avoided heart failure–related hospitalizations. Whether this is a net gain or loss to a hospital depends on several factors that are difficult to quantify, including the margin that a hospital earns on the avoided hospitalizations, but clearly payer reimbursement would encourage greater use of nurse management by hospital-based providers.
Although cost-effective at less than $5000 per QALY gained, our nurse management intervention is unlikely to be cost-saving for the Medicare program if it covered all patients with heart failure. To our knowledge, no experimental evidence of nurse management for heart failure justifies an expectation of cost saving from a societal or any other perspective. The 12-month intervention would have cost Medicare $158 per patient, an estimate with reasonably good generalizability to similar communities given our trial’s broad inclusion criteria and recruitment of patients from ambulatory settings. These findings match the results of Medicare’s ongoing demonstration project, which randomly assigned patients with heart failure, diabetes, or coronary artery disease to disease management and found no evidence that the nurse management interventions were cost-saving or cost-neutral (34). The appropriate question for policymakers, however, is not about costs in isolation, but whether the likely health benefits to be gained are worth the costs to be invested. Further research is clearly needed to understand which types of nurse management interventions and which types of patients with heart failure result in programs that provide good value for the money.
At less than $25 000 per QALY saved, this nurse-led disease management program was reasonably cost-effective over 12 months, especially for patients with earlier stages of heart failure. Wider adoption of such programs may be a sensible approach to reducing the burden of heart failure in ethnically diverse, urban communities.
Context
Although evidence indicates that nurse-led care management improves clinical outcomes for patients with heart failure, evidence on the economic benefits of these programs is lacking.
Contribution
Using data on costs from a randomized trial of 12 months of care management versus usual care for socioeconomically disadvantaged patients with heart failure, the investigators estimated that the cost-effectiveness of case management is less than $20 000/QALY.
Caution
The results might not apply to patients in less socioeconomically disadvantaged settings.
—The Editors
Acknowledgments
Role of the Funding Source
Funding was provided by the Agency for Healthcare Research and Quality. The funding source had no role in the design, conduct, or analysis of the study or in the decision to submit the manuscript for publication.
Grant Support: Dr. Sisk was supported by a grant from the Agency for Healthcare Research and Quality (R01 HS10402-01).
Potential Financial Conflicts of Interest: Grants received: C. Horowitz (National Institutes of Health).
Footnotes
Requests for Single Reprints: Paul L. Hebert, PhD, Health Services Research and Development, Veterans Affairs Puget Sound Health Care System, 1100 Olive Way, Suite 1400, Seattle, WA 98101.
Current author addresses and author contributions are available at www.annals.org.
References
- 1.McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. Am J Med. 2001;110:378–84. doi: 10.1016/s0002-9343(00)00743-9. [PMID: 11286953] [DOI] [PubMed] [Google Scholar]
- 2.Gold M, Siegel J, Russell L, Weinstein M. Cost-Effectiveness in Health and Medicine. Oxford Univ Pr; New York: 1996. [Google Scholar]
- 3.Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [PMID: 17194875] [DOI] [PubMed] [Google Scholar]
- 4.Ghali JK, Kadakia S, Cooper R, Ferlinz J. Precipitating factors leading to decompensation of heart failure. Traits among urban blacks. Arch Intern Med. 1988;148:2013–6. [PMID: 3046541] [PubMed] [Google Scholar]
- 5.Horowitz CR, Rein SB, Leventhal H. A story of maladies, misconceptions and mishaps: effective management of heart failure. Soc Sci Med. 2004;58:631–43. doi: 10.1016/s0277-9536(03)00232-6. [PMID: 14652059] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sisk JE, Hebert PL, Horowitz CR, McLaughlin MA, Wang JJ, Chassin MR. Effects of nurse management on the quality of heart failure care in minority communities: a randomized trial. Ann Intern Med. 2006;145:273–83. doi: 10.7326/0003-4819-145-4-200608150-00007. [PMID: 16908918] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Franks P, Lubetkin EI, Gold MR, Tancredi DJ. Mapping the SF-12 to preference-based instruments: convergent validity in a low-income, minority population. Med Care. 2003;41:1277–83. doi: 10.1097/01.MLR.0000093480.58308.D8. [PMID: 14583690] [DOI] [PubMed] [Google Scholar]
- 8.Brazier JE, Roberts J. The estimation of a preference-based measure of health from the SF-12. Med Care. 2004;42:851–9. doi: 10.1097/01.mlr.0000135827.18610.0d. [PMID: 15319610] [DOI] [PubMed] [Google Scholar]
- 9.Lawrence WF, Fleishman JA. Predicting EuroQoL EQ-5D preference scores from the SF-12 Health Survey in a nationally representative sample. Med Decis Making. 2004;24:160–9. doi: 10.1177/0272989X04264015. [PMID: 15090102] [DOI] [PubMed] [Google Scholar]
- 10.Sengupta N, Nichol MB, Wu J, Globe D. Mapping the SF-12 to the HUI3 and VAS in a managed care population. Med Care. 2004;42:927–37. doi: 10.1097/01.mlr.0000135812.52570.42. [PMID: 15319619] [DOI] [PubMed] [Google Scholar]
- 11.Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14:487–96. doi: 10.1002/hec.944. [PMID: 15497198] [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services Payment Impact File. 2007 Accessed at www.cms.hhs.gov/AcuteInpatientPPS on 20 August 2008. [Google Scholar]
- 13.U.S. Department of Labor, Bureau of Labor Statistics . Producer Price Index Industry Data: 1 Month Percent Change. U.S. Department of Labor; Washington, DC: 2001. Series ID pcu622110622110. Accessed at http://data.bls.gov/PDQ/servlet/SurveyOutputServlet?data_tool=latest_numbers&series_id=PCU622110622110&output_view=pct_1mth on 2 September 2008. [Google Scholar]
- 14.Centers for Medicare & Medicaid Services Annual Physician Fee Schedule Payment Amount File, Calendar Year 2001. Accessed at www.cms.hhs.gov/PhysicianFeeSched/PFSNPAF/list.asp#TopOfPage on 2 September 2008.
- 15.Centers for Medicare & Medicaid Services Medicaid Federal Upper Limits Data. 2003 Accessed at www.cms.hhs.gov/MedicaidDrugRebateProgram/SDUD/list.asp on 2 September 2008. [Google Scholar]
- 16.Blough DK, Madden CW, Hornbrook MC. Modeling risk using generalized linear models. J Health Econ. 1999;18:153–71. doi: 10.1016/s0167-6296(98)00032-0. [PMID: 10346351] [DOI] [PubMed] [Google Scholar]
- 17.Baker DW, Williams MV, Parker RM, Gazmararian JA, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38:33–42. doi: 10.1016/s0738-3991(98)00116-5. [PMID: 14528569] [DOI] [PubMed] [Google Scholar]
- 18.StataCorp . Stata Statistical Software: Release 10.0 [manual] StataCorp; College Station, TX: 2005. [Google Scholar]
- 19.Rubin DB. Multiple Imputation for Nonresponse in Surveys. J Wiley; New York: 1987. [Google Scholar]
- 20.Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves—facts, fallacies and frequently asked questions. Health Econ. 2004;13:405–15. doi: 10.1002/hec.903. [PMID: 15127421] [DOI] [PubMed] [Google Scholar]
- 21.Glick HA, Doshi JA, Sonnad SS, Polsky D. Economic Evaluations in Clinical Trials. Oxford Univ Pr; New York: 2007. pp. 181–3. [Google Scholar]
- 22.U.S. Department of Labor, Bureau of Labor Statistics . Consumer Price Index Detailed Report Tables, Annual Average Indexes 2001. Vol. 2007. U.S. Department of Labor; Washington, DC: 2001. Consumer Price Index—All Urban Consumers—Medical Care. Series IDs CUURA101SAM, CUUR000SAM. [Google Scholar]
- 23.Chapman RH, Stone PW, Sandberg EA, Bell C, Neumann PJ. A comprehensive league table of cost-utility ratios and a sub-table of “panel-worthy” studies. Med Decis Making. 2000;20:451–67. doi: 10.1177/0272989X0002000409. [PMID: 11059478] [DOI] [PubMed] [Google Scholar]
- 24.Hirth RA, Chernew ME, Miller E, Fendrick AM, Weissert WG. Willingness to pay for a quality-adjusted life year: in search of a standard. Med Decis Making. 2000;20:332–42. doi: 10.1177/0272989X0002000310. [PMID: 10929856] [DOI] [PubMed] [Google Scholar]
- 25.Rich MW, Nease RF. Cost-effectiveness analysis in clinical practice: the case of heart failure. Arch Intern Med. 1999;159:1690–700. doi: 10.1001/archinte.159.15.1690. [PMID: 10448770] [DOI] [PubMed] [Google Scholar]
- 26.Benatar D, Bondmass M, Ghitelman J, Avitall B. Outcomes of chronic heart failure. Arch Intern Med. 2003;163:347–52. doi: 10.1001/archinte.163.3.347. [PMID: 12578516] [DOI] [PubMed] [Google Scholar]
- 27.Naylor MD, Brooten DA, Campbell RL, Maislin G, McCauley KM, Schwartz JS. Transitional care of older adults hospitalized with heart failure: a randomized, controlled trial. J Am Geriatr Soc. 2004;52:675–84. doi: 10.1111/j.1532-5415.2004.52202.x. [PMID: 15086645] [DOI] [PubMed] [Google Scholar]
- 28.Kasper EK, Gerstenblith G, Hefter G, Van Anden E, Brinker JA, Thiemann DR, et al. A randomized trial of the efficacy of multidisciplinary care in heart failure outpatients at high risk of hospital readmission. J Am Coll Cardiol. 2002;39:471–80. doi: 10.1016/s0735-1097(01)01761-2. [PMID: 11823086] [DOI] [PubMed] [Google Scholar]
- 29.Pugh L, Havens D, Xie S, Robinson J, Blaha C. Case management for elderly persons with heart failure: the quality of life and cost outcomes. Medsurg Nurs. 2001;10:71–8. [Google Scholar]
- 30.Smith B, Hughes-Cromwick PF, Forkner E, Galbreath AD. Cost-effectiveness of telephonic disease management in heart failure. Am J Manag Care. 2008;14:106–15. [PMID: 18269306] [PubMed] [Google Scholar]
- 31.Smith B, Forkner E, Zaslow B, Krasuski RA, Stajduhar K, Kwan M, et al. Disease management produces limited quality-of-life improvements in patients with congestive heart failure: evidence from a randomized trial in community-dwelling patients. Am J Manag Care. 2005;11:701–13. [PMID: 16268753] [PubMed] [Google Scholar]
- 32.Davis SK, Liu Y, Gibbons GH. Disparities in trends of hospitalization for potentially preventable chronic conditions among African Americans during the 1990s: implications and benchmarks. Am J Public Health. 2003;93:447–55. doi: 10.2105/ajph.93.3.447. [PMID: 12604494] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kozak LJ, Hall MJ, Owings MF. Trends in avoidable hospitalizations, 1980-1998. Health Aff (Millwood) 2001;20:225–32. doi: 10.1377/hlthaff.20.2.225. [PMID: 11260947] [DOI] [PubMed] [Google Scholar]
- 34.Chen A, Brown R, Esposito D, Schore J, Shapiro R. Report to Congress on the Evaluation of Medicare Disease Management Programs. 2008 Feb 14; Mathematica Policy Research Report No. 8914-762. Princeton: Mathematica Policy Research. [Google Scholar]
- 35.Centers for Medicare & Medicaid Services Update of Calendar Year 2001 Hospital Outpatient Payment Rates and Coinsurance Amounts Effective April 1, 2001. Accessed at https://www.cms.hhs.gov/hospitaloutpatientpps/downloads/apr001a.pdf on 2 September 2008.
- 36.U.S. Department of Labor, Bureau of Labor Statistics 2000 Metropolitan Area Occupational Employment and Wage Estimates. Accessed at www.bls.gov/oes/2000/oes_5600.htm#b29-0000 on 26 August 2008.
- 37.Centers for Medicare & Medicaid Services Health Care Procedure Coding System (HCPCS) procedure codes and the Berenson-Eggers Type of Service (BETOS) code, 2001. Accessed at www.cms.hhs.gov/hcpcsreleasecodesets/20_betos.asp on 2 September 2008.
- 38.Gabrel CS. An overview of nursing home facilities: data from the 1997 National Nursing Home Survey. Adv Data. 2000:1–12. [PMID: 10977763] [PubMed] [Google Scholar]
- 39.U.S. Bureau of Labor Statistics, U.S. Bureau of the Census Current Population Survey, 2001. Accessed at www.bls.census.gov/cps_ftp.html on 26 August 2008.