Abstract
Objective
This meta-analysis systematically compiles intervention research designed to increase medication adherence among underrepresented adults.
Method
Comprehensive searching located published and unpublished studies with medication adherence behavior outcomes. Studies were included if samples were adults living in North America who had any of the following backgrounds or identities: African American, Native American, Latino, Latino American, Asian, Asian American, Pacific Islander, Native Alaskan, or Native Hawaiian. Random-effects analyses synthesized data to calculate effect sizes as a standardized mean difference and variability measures. Exploratory moderator analyses examined the association between specific efforts to increase the cultural relevance of medication adherence studies and behavior outcomes.
Results
Data were synthesized across 5,559 subjects in 55 eligible samples. Interventions significantly improved medication adherence behavior of treatment subjects compared to control subjects (standardized mean difference = 0.211). Primary studies infrequently reported strategies to enhance cultural relevance. Exploratory moderator analyses found no evidence that associated cultural relevance strategies with better medication adherence outcomes.
Conclusion
The modest magnitude of improvements in medication adherence behavior documents the need for further research with clear testing of cultural relevance features.
Keywords: medication adherence, meta-analysis, minority groups
Introduction
Effective medication adherence (MA) is an important component of individuals’ behavior to prevent disease and management their acute and chronic illnesses (Christensen, 2004; Pigott, 1994; Viswanathan et al., 2012). Even so, around 50% of patients do not consume medications as prescribed (Dunbar-Jacob et al., 2000). High levels of non-adherence occur across diverse diseases and samples (Christensen, 2004; Garg et al., 2008). Multiple studies document lower MA rates among underrepresented groups than the majority population (Jin et al., 2008; Lewis et al., 2012; Saha et al., 2008; Sewell and Velayos, 2013). Health disparities are common among diseases that require MA to achieve health outcomes, such as hypertension and diabetes. Population differences in MA may contribute to health outcomes (Heisler et al., 2007).
The need for culturally relevant health behavior change interventions for underrepresented populations is important for diverse societies (Bernal and Domenech Rodriguez, 2012; Kreuter and McClure, 2004; Resnicow et al., 1999; Sanders Thompson et al., 2008). Lower rates of MA among underrepresented adults may reflect lack of culturally relevant interventions by health care providers. Culturally relevant interventions reflect the target group’s beliefs, norms, values, practices, and patterns (Bernal and Domenech Rodriguez, 2012; Kreuter and McClure, 2004). These interventions use people, locations, and language familiar to participants (Kumanyika and Yancey, 2009; Resnicow et al., 1999). Culturally relevant interventions reflect an understanding of the psychological, familial, social, environmental, cultural, and historical context of health behavior (Resnicow et al., 1999). For example, interventions could attend to cultural values such as spirituality, verbal communication and testimony, communalism, commitment to family, knowing through intuition and experience, and expressiveness (Kreuter and McClure, 2004; Resnicow et al., 1999). Despite the potential importance of cultural relevance, no standards or common terminology exist (Kumanyika and Yancey, 2009; Resnicow et al., 1999). Although many interventions have been tested in underrepresented participants, scant evidence is available about how best to achieve cultural relevance for health behavior interventions (Sanders Thompson et al., 2008).
The importance of MA combined with strong evidence of insufficient MA has prompted multiple trials testing interventions to improve this behavior. Findings have been mixed across intervention studies in underrepresented samples. Some studies report higher MA among treatment groups than control subjects (Mann, 2001; Simoni et al., 2007; Walker, 2000; Werner, 1979), though other studies do not report better MA outcomes among treatment subjects (Bogart et al., 2012; Burrelle, 1986; Harper, 1984; McPherson-Baker et al., 2000). The importance of MA, the proliferation of primary research testing MA interventions among underrepresented populations, and inconsistent results across trials justify efforts to summarize and synthesize findings. Few previous reviews have attempted to summarize findings. Manias and Williams (2010) reviewed seven studies of underrepresented population samples and reported an MA outcome odds ratio effect size of 0.81 for the five studies with dichotomous outcomes, and a standardized mean difference effect size of 0.22 for the two studies with continuous outcomes. Neither effect size was statistically significant, perhaps due to the very small sample size. Bailey, Cates, Kruske, Morris, Brown, and Chang (2009) reviewed four studies with interventions designed to be culturally relevant to underrepresented children and adults with asthma, but they did not report MA outcomes. Other reviews of MA intervention trials in the general population have mentioned the importance of underrepresented populations without addressing the findings of studies testing interventions in such groups (Viswanathan et al., 2012).
This systematic review and meta-analysis was designed to fill gaps in knowledge by quantitatively synthesizing primary research testing MA interventions and by exploring the association between strategies to increase the cultural relevance of interventions and outcomes. Primary study participants included underrepresented adults with prescribed medications. Study interventions were designed to increase MA. This project focused on comparisons between treatment and control group MA behavior outcomes. The research questions were: 1) What are the overall average effects of interventions designed to increase MA among underrepresented adults on MA behavior outcomes? 2) Do effects of interventions vary depending on strategies to increase the cultural relevance of interventions?
Materials and Methods
Widely accepted systematic review (including PRISMA guidelines) and meta-analytic methods were used for the project (Cooper et al., 2009; Liberati et al., 2009). Searching, screening, and coding procedures were conducted as part of a larger meta-analysis. The review protocol may be obtained by contacting the corresponding author.
Eligibility Criteria
Studies interventions designed to increase MA were eligible for inclusion. MA was defined as the extent to which medication-taking behavior is consistent with health care provider recommendations (World Health Organization, 2003). Since meta-analysis converts primary study outcomes to unitless standardized indices, studies with varied MA measures (e.g., pill counts, pharmacy refill, electronic bottle cap devices, self-report) were included. Diverse MA interventions were included. Studies of medications prescribed by health care providers were included. Sexual or reproductive function medications, immunizations, smoking or other substance abuse cessation drugs, and medications administered exclusively by health care providers were excluded. Some prescribed medications, such as immunizations, are typically administered by health care providers and not patients. These medications are often administered during outpatient health care visits. While patients must consent to these medications, the process of administering the medication is different from those administered by patients. The reasons underrepresented adults may not obtain ambulatory health care may differ from reasons they are not adherent with self-administered medications at home. Interventions to address MA in substance abuse patients likely differ from medications for other non-psychiatric medications. Some patient decisions about consuming or ceasing sexual and reproductive medications based on the intended effects are expected. Nutraceuticals, supplements, and vitamins were excluded unless they were prescribed by health care providers.
Intervention research studies were included if they reported adequate data to calculate effect sizes. Corresponding authors of reports without adequate data were contacted to provide effect size information. Both published and unpublished studies were included to avoid bias because the most consistent difference between published and unpublished research is the statistical significance of the findings (Burdett et al., 2003). Pre-experimental and small-sample studies were included, with smaller studies given less weight in analyses than larger studies.
Only studies with predominantly underrepresented participants were included. Studies with less than 70% underrepresented subjects were excluded. For this study, underrepresented refers to individuals living in North America or Hawaii who have any of the following backgrounds or identities: African American, Native American, Latino, Latino American, Asian, Asian American, Pacific Islander, Native Alaskan, or Native Hawaiian (Conn et al., 2012). Studies of children, incarcerated or institutionalized persons, or subjects with psychiatric problems such as schizophrenia or clinical depression were excluded. Studies reported in 1960 or more recently were eligible for inclusion.
Search Strategies and Information Sources
Multiple search strategies were employed to avoid the bias resulting from narrow searches (White, 2009). An expert health sciences librarian conducted searches in PUBMED, PsychINFO, MEDLINE, EBSCSO, Cochrane Central Trials Register, CINAHL, Cochrane Database of Systematic Reviews, EBM Reviews, PDQT, ERIC, IndMed, International Pharmaceutical Abstracts, and Communication and Mass Media. The primary MeSH terms upon which searches were constructed were Patient Compliance and Medication Adherence. Medication Adherence was used to locate studies published after 2008, when the MeSH term was introduced. Patient Compliance was used to locate studies published before 2009. Other MeSH terms used in constructing search strategies were: prescription drugs, pharmaceutical preparations, drugs, dosage forms, or generic. Text words used in searches were: compliant, compliance, adherent, adherence, noncompliant, noncompliance, nonadherent, nonadherence, improve, promote, enhance, encourage, foster, advocate, influence, incentive, ensure, remind, optimize, optimize, increase, impact, prevent, address, decrease, prescription(s), prescribed, drug(s), medication(s), pill(s), tablet(s), regimen(s), chemotherapy, agent(s), antihypertensive(s), antituberculosis, antiretrovirals, and HAART. No search terms were used to identify studies of underrepresented samples because these terms are inconsistently applied and because some authors do not identify their samples as predominantly underrepresented adults in their studies’ titles, abstracts, or keywords (Conn et al., 2012).
Abstracts from 48 conferences were examined for potential studies. Nineteen research registers (e.g., Research Portfolio Online Reporting Tool) were searched. Authors of studies in the research registers were contacted for potential studies. Authors of more than one eligible primary study were contacted for additional studies. Ancestry searches were conducted on all eligible primary studies and review articles. Hand searches were conducted in 57 journals where more than three primary studies in the parent project were published. Searching was completed in 2013.
Study Selection
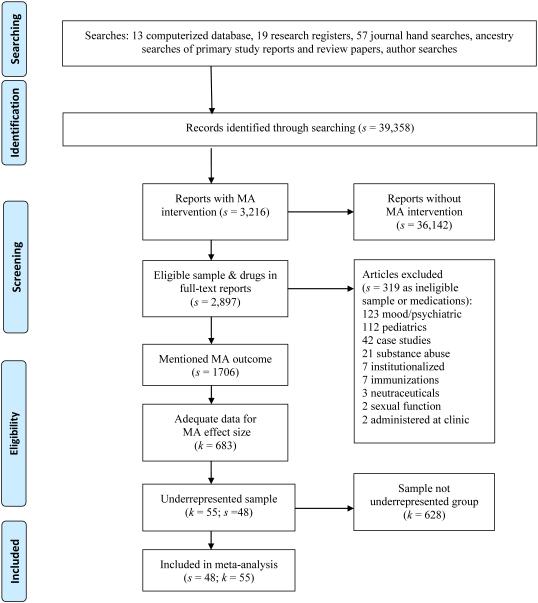
Extensively trained research specialists with graduate education selected the studies. A staged eligibility determination process was used to examine 39,358 potential studies identified through comprehensive searching (see Figure 1 for PRISMA flow diagram). First, titles and abstracts were reviewed for visual heralds. Second, the report was examined for the presence of an intervention to increase MA. Then the sample, including medication types, was evaluated for eligibility (see above). Fourth, the study was examined to determine whether adequate effect size data were available. Corresponding authors were contacted to obtain this information if it was not available in the report. Fifth, studies eligible for the parent study were evaluated to determine if the sample was predominantly underrepresented adults. At each stage of study selection, questionable studies were examined by multiple members of the research team to determine eligibility. Finally, to ensure that only independent samples entered the study, the entire author list for each potential study was compared to author lists of previously-coded studies to locate potential separate reports on the same subjects.
Figure 1. Flow diagram.
Note: s denotes the number of research reports, k indicates the number of comparisons, MA denotes medication adherence
Data Collection Process and Data Items
Extensive examination of review articles, meta-analyses on related topics, and primary studies was used to develop the coding frame. The coding frame includes not only outcomes but also items related to source characteristics, study design and methods, participant characteristics, and intervention attributes. Source characteristics were coded, including publication status, year of distribution, and presence of funding.
Methodological characteristics were coded, including allocation to treatment and control group, allocation concealment, data collector masking, presence of a control group, intention-to-treat analyses, number of intervention sessions, and number of days over which the intervention was delivered. Sample characteristics were coded, including mean age, gender and ethnicity distribution, diseases being treated with prescribed medications, number of prescribed medications, and inclusion of participants with low income, as defined by primary study authors. No information to create a coding scheme for cultural relevance characteristics was located in a literature review of conceptual articles, expert opinion papers, and previous review articles. The coding items for cultural relevance were created differently from other coding items which were developed prior to retrieving studies. The process was based on similar work reported for cultural relevance of interventions to increase physical activity (Conn et al., In press; Conn et al., 2012). Cultural relevance characteristics were coded from studies in two stages to ensure that all relevant information was coded. First, verbatim content related to cultural relevance of study methods or interventions was recorded in a Word file from each eligible research report. Recording verbatim content without previously developing coding schemes ensured that all relevant materials were recorded without imposing investigator constraints. Verbatim comments were grouped into themes to create categories by three members of the research team, including two doctorally prepared underrepresented researchers. Thus the codes for cultural relevance categories were created from the data in the primary studies. Authors of primary studies were not contacted to provide further details because of the age of many studies which would hamper recall and retention of written materials as well because respondent bias toward reporting cultural relevance characteristics might diminish accuracy. The codes for categories were applied to the studies based on the content analysis of verbatim content. These coded items focused on recruitment location at underrepresented specific location, intervention location selected to be familiar to underrepresented samples such as churches, language matched to sample, education materials prepared at a reading level consistent with the sample, compensation for time and costs for subjects, inclusion of cultural content, underrepresented peers as interventionists, well-known people from underrepresented groups appearing in intervention materials, intervention tested in underrepresented focus group or panel of experts, subjects referred to underrepresented adult community resources, and cultural sensitivity training for project staff.
When multiple reports were available for the same sample, all reports were coded to increase available coding information. To enhance validity, data were coded at a micro level for maximum detail (Orwin and Vevea, 2009; Wilson, 2009). Two extensively trained coders independently extracted all data to establish its reliability. The two coders compared all data to achieve 100% agreement. Effect-size data were verified by a third doctorally-prepared coder.
Statistical Analysis: Summary Measure and Method of Analyses
A standardized mean difference effect size was calculated for each primary study comparison (Cooper et al., 2009). Treatment vs. control post-intervention effect size refers to treatment group results compared to control group results after interventions. A positive effect size indicates better results for treatment than for control subjects. Each effect size was weighted by the inverse of variance to give more weight to studies with larger samples (Lipsey and Wilson, 2001). Effect sizes were adjusted for bias (Hedges and Olkin, 1985).
This report’s findings emphasize the treatment vs. control post-intervention effect size. Effect sizes were also calculated for treatment scores pre- vs. post-intervention. A similar analysis was conducted for control group baseline vs. outcome values. The single-group effect sizes are reported as ancillary information.
The random-effects model was used for effect sizes because the model assumes individual effect sizes vary due both to study-level and subject-level variations (Raudenbush, 1994). The random effects model is consistent with this area of science, with its variations in samples, methods, and interventions. Q, a standard heterogeneity statistic, was used to assess homogeneity among effect sizes (Higgins et al., 2003). The I2 index was computed as a measure of heterogeneity beyond within-study sampling error. The expected heterogeneity was handled in four ways (Berlin, 1995; Conn et al., 2007; Lipsey and Wilson, 2001). First, location parameters and measures of heterogeneity were reported. Second, random-effects models were used that assume variations in studies beyond sampling error. Third, exploratory moderator analyses were used to examine potential sources of heterogeneity. Finally, findings were interpreted in light of discovered heterogeneity. U3, an index of the percentage of the treatment groups that exceeded scores of the control groups, was used to help explain the effect size.
Risk of Bias
Methodological quality varies among MA intervention studies. Meta-analysis approaches to address methodological quality include a priori inclusion criteria related to rigor and post hoc procedures for considering quality as an empirical question (Cooper et al., 2009; Valentine, 2009). Combination approaches are common in meta-analyses (Valentine, 2009), and this synthesis used both approaches. To partially address design bias, effect sizes were reported separately for two-group post-intervention comparisons and treatment group pre-post comparisons. To explore potential bias from participating in research, control group pre-post comparisons were reported. The main analyses included only studies with treatment and control groups; single-group comparisons were provided as supplementary information.
Variations in primary study sample size were managed statistically. Small-sample studies may lack statistical power in primary research, but they were included because they contribute to effect size estimates, and meta-analysis does not rely on p values from primary research. Effect size estimates were weighted so more precise estimates (e.g., due to larger sample sizes) would be given proportionally more influence on our findings.
Common indicators of methodological strength (random assignment of subjects to groups, allocation concealment, data collector masking, and intention-to-treat analyses) were examined via moderator analyses as a form of sensitivity analyses to address risk of bias (Liberati et al., 2009). Potential bias from reporting continuous data as dichotomous outcomes was addressed through sensitivity analysis to compare effect sizes between studies reporting dichotomous and continuous MA behavior.
Comprehensive search strategies were employed to avoid the bias of including studies with larger effect sizes which are often easier to locate (White, 2009). Both published and unpublished studies were included because the most consistent difference between published and unpublished studies is the statistical significance of the findings (Rothstein and Hopewell, 2009). Publication bias was assessed using funnel plots (Sutton, 2009). A priori decisions about which MA measures to code were used to avoid potential reporting bias within studies.
Results
From 39,358 potential studies, we identified 55 primary study comparisons from 48 research reports testing interventions to increase MA in underrepresented samples (Anderson et al., 2004; Andrade et al., 2005; Austin, 1986; Babamoto et al., 2009; Bogart et al., 2012; Bogner and de Vries, 2008; Bogner and de Vries, 2010; Burrelle, 1986; Chaisson et al., 2001; Cordasco et al., 2009; DiIorio et al., 2008; DiIorio et al., 2003; Fernandez et al., 2008; Fisher et al., 2011; Freedman, 2007; Gazmararian et al., 2010; Glanz et al., 2012; Harper, 1984; Holzemer et al., 2006; Kalichman et al., 2011; Kellaway and McCrae, 1979; Koenig et al., 2008; Kripalani et al., 2012; Laine et al., 1996; Mann, 2001; Martin et al., 2011; McKenney et al., 1973; McPherson-Baker et al., 2000; Migneault et al., 2012; Moitra et al., 2011; Muir et al., 2012; Mundy, 2009; Murphy et al., 2007; Newsome, 1995; Parsons et al., 2007; Powell, 2002; Purcell et al., 2007; Remien et al., 2005; Simoni et al., 2007; Tagliacozzo et al., 1974; van Servellen et al., 2005; Vivian, 2002; Walker, 2000; Webel, 2010; Weinberger et al., 1991; Werner, 1979; Wohl et al., 2006; Wyatt et al., 2004). The PRISMA flow diagram summarizing study section is found in Figure 1. Nine additional articles reporting on the same studies were located and used as companion papers for additional coding information. The studies included in this project reported on a total of 5,559 subjects. These reports yielded effect size data for 55 comparisons for treatment vs. control at outcome, 51 treatment pre- vs. post-intervention, and 27 control pre- vs. post-intervention.
Study Characteristics
Comparisons were disseminated as journal articles (k = 49) and dissertations (s = number of reports, k = number of comparisons). Although the earliest study was published in 1973, studies of MA in underrepresented adults have increased in recent years, with eight reports disseminated before 1990, and 42 in 2000 or after. Most studies (k = 46) received funding. Table 1 shows descriptive statistics for primary studies. The median of mean sample size was 36 treatment and 35 control subjects. Seven studies were composed predominantly of Latino subjects, and 27 were mainly African-Americans. Women were well represented (median of mean = 54%), and only two studies did not provide gender information. The median value for mean age was 51 years (k = 47). Among the studies which reported income level, 22 studies reported that subjects were low income. Only one study reported including subjects with cognitive impairment. Samples of people with hypertension (s = 13) and human immunodeficiency virus (HIV) (s = 23) were common.
Table 1.
Characteristics of Primary Studies Included in Medication Adherence Meta-Analyses
| Characteristic | k | Min | Q1 | Mdn | Q3 | Max |
|---|---|---|---|---|---|---|
| Total number of treatment Ss at outcome | 55 | 6 | 22 | 36 | 78 | 196 |
| Total number of control Ss at outcome | 48 | 4 | 23.3 | 35 | 74.3 | 212 |
| Percentage female | 53 | 0 | 33 | 53. 5 | 75 | 100 |
| Percent Black | 53 | 0 | 47.9 | 76.0 | 89.4 | 100 |
| Percent Hispanic | 38 | 0 | 0 | 14.8 | 47.8 | 100 |
| Percent Native American | 25 | 0 | 0 | 0 | 0 | 10 |
| Percent Asian American | 28 | 0 | 0 | 0 | 2 | 100 |
| Mean age (years) | 47 | 38 | 42.4 | 50.6 | 60.85 | 73 |
| Number of intervention sessions | 46 | 1 | 3.3 | 5.5 | 8.4 | 120 |
| Number of days over which intervention was delivered |
53 | 1 | 28 | 91.5 | 183 | 549 |
| Mean number of prescribed medications | 5 | 1.9 | 3.1 | 5.1 | 5.3 | 5.9 |
Note. Includes all studies that contributed to primary analyses at least one effect size for any type of comparison. s=number of reports providing data on characteristic; Q1=first quartile, Q3=third quartile.
Overall Effects of Interventions on Medication Adherence Outcomes
Overall MA effect sizes are presented in Table 2. Effect sizes were calculated for 55 treatment-vs.-control-group outcome comparisons of 5,559 subjects. The overall standardized mean difference effect size was 0.211. The positive effect size documents that treatment subjects had significantly better MA outcomes than were reported for control subjects. In terms of U3, 58% of treatment subjects would have better MA values than control subjects. Treatment vs. control comparisons were significantly heterogeneous (based on Q statistics) with I2 of 61.568.
Table 2.
Intervention Effect on Medication Adherence Comparison between Treatment and Control Groups: Random-Effects Estimates and Tests
|
| ||||||||
|---|---|---|---|---|---|---|---|---|
| k | Effect size |
p (ES) | 95% Confidence interval |
Standard error |
I2 | Q | p (Q) | |
|
| ||||||||
| Treatment vs. control all studies | 55 | 0.211 | <.001 | 0.109, 0.242 | 0.052 | 61.568 | 140.508 | <.001 |
|
| ||||||||
| Treatment vs. control continuous data studies | 28 | 0.243 | <.001 | 0.076, 0.410 | 0.085 | 72.307 | 97.497 | <.001 |
|
| ||||||||
| Treatment vs. control dichotomous data studies | 27 | 0.167 | .004 | 0.054, 0.279 | 0.057 | 36.673 | 41.057 | .031 |
|
| ||||||||
| Treatment subjects pre- vs. post-comparisons* | 47 | 0.418 | <.001 | 0.293, 0.542 | 0.064 | 78.296 | 211.943 | <.001 |
|
| ||||||||
| Control subjects pre- vs. post-comparisons** | 24 | −0.022 | .697 | −0.135, 0.090 | 0.058 | 51.139 | 47.072 | .002 |
|
| ||||||||
k denotes number of comparisons, Q is a conventional homogeneity statistic, I2 is the percentage of total variation among studies’ observed ES due to heterogeneity.
Four studies excluded as outliers.
Three studies excluded as outliers.
Effect sizes were calculated for 47 treatment group pre-post comparisons of 2,746 subjects; four studies were excluded as outliers. For treatment pre- vs. post-intervention comparisons, the overall effect size was 0.418. The analyses of 24 control pre- vs. post-intervention comparisons included 1,434 subjects; three studies were excluded as outliers. The control group subjects MA effect size of −.022 documented that control subjects did not improve from participating in studies. Both treatment and control pre-post comparisons displayed significant heterogeneity as evidenced by significant Q values in Table 2. Forest plots of effect sizes are available from the corresponding author.
Cultural Relevance Moderator Analyses
Tables 3 and 4 display results of dichotomous and continuous moderator analyses. Only 15 studies reported any cultural relevance aspect of interventions. The effect sizes of studies with any culturally relevant intervention (0.201) and studies that did not report any strategies to increase cultural relevance (0.220) were nearly identical. The number of culturally relevant study features was unrelated to the MA effect size. Only cultural relevance potential moderators with at least three cases were examined in further analyses. Moderator analyses are exploratory and should be interpreted with caution given the small number of studies in some analyses.
Table 3.
Dichotomous Moderator Results for Medication Adherence: Treatment vs. Control at Outcome
|
| |||||
|---|---|---|---|---|---|
| Moderator | k | Effect size |
Standard error |
Qbetween | p (Qbetween) |
|
| |||||
| CULTURAL RELEVANCE MODERATORS | |||||
|
| |||||
| Intervention location | 1.304 | .354 | |||
|
| |||||
| Location familiar to subjects | 3 | 0.422 | 0.133 | ||
|
| |||||
| Location not selected because it was familiar to subjects |
52 | 0.196 | 0.053 | ||
|
| |||||
| Language | 0.424 | .515 | |||
|
| |||||
| Language specific to subjects | 7 | 0.280 | 0.103 | ||
|
| |||||
| Language of participants not addressed in report |
48 | 0.203 | 0.058 | ||
|
| |||||
| Intervention materials educational level | 0.143 | .705 | |||
|
| |||||
| Intervention designed for low educational level |
3 | 0.145 | 0.181 | ||
|
| |||||
| Educational level of intervention not addressed in report |
52 | 0.217 | 0.055 | ||
|
| |||||
| Cultural content | 0.032 | .857 | |||
|
| |||||
| Cultural content addressed in intervention | 8 | 0.193 | 0.092 | ||
|
| |||||
| Cultural content not addressed | 47 | 0.212 | 0.060 | ||
|
| |||||
| Peers as interventionist | 0.500 | .480 | |||
|
| |||||
| Cultural peers were interventionists | 7 | 0.134 | 0.118 | ||
|
| |||||
| Report did not describe peer interventionists | 48 | 0.227 | 0.058 | ||
|
| |||||
| Cultural sensitivity training of staff | 2.388 | .122 | |||
|
| |||||
| Cultural training provided for staff | 5 | 0.420 | 0.141 | ||
|
| |||||
| No cultural sensitivity training reported for staff |
50 | 0.185 | 0.056 | ||
|
| |||||
| Presence of any cultural relevance component | .033 | .855 | |||
|
| |||||
| At least one cultural relevance component reported |
15 | 0.201 | 0.072 | ||
|
| |||||
| No cultural relevance components | 40 | 0.220 | 0.069 | ||
|
| |||||
| SAMPLE CHARACTERISTIC MODERATORS | |||||
|
| |||||
| Sample socio-economic status | 2.428 | .119 | |||
|
| |||||
| Reported low socio-economic status | 22 | 0.126 | 0.071 | ||
|
| |||||
| Did not report low socio-economic status | 33 | 0.288 | 0.126 | ||
|
| |||||
| Sample predominantly one underrepresented group | 0.599 | .439 | |||
|
| |||||
| Sample predominantly African-American | 27 | 0.191 | 0.065 | ||
|
| |||||
| Sample predominantly Hispanic | 7 | 0.306 | 0.134 | ||
|
| |||||
| Sample selected for poor medication adherence | 3.737 | 0.053 | |||
| Reported sample selected for poor medication adherence |
12 | 0.425 | 0.125 | ||
|
| |||||
| Did not report targeting subjects with poor medication adherence |
43 | 0.159 | 0.125 | ||
|
| |||||
| Sample disease | 2.755 | .097 | |||
|
| |||||
| All subjects had hypertension | 15 | 0.053 | 0.076 | ||
|
| |||||
| All subjects HIV positive | 23 | 0.246 | 0.088 | ||
|
| |||||
| RESEARCH METHODS MODERATORS | |||||
|
| |||||
| Allocation to treatment groups | 0.015 | .904 | |||
|
| |||||
| Randomization of individual subjects | 44 | 0.216 | 0.056 | ||
|
| |||||
| Subjects not individually randomized | 11 | 0.198 | 0.137 | ||
|
| |||||
| Allocation concealment | 0.658 | .417 | |||
|
| |||||
| Allocation concealed | 14 | 0.145 | 0.096 | ||
|
| |||||
| Did not report allocation concealed | 41 | 0.239 | 0.063 | ||
|
| |||||
| Data collector masking | 8.132 | .004 | |||
|
| |||||
| Data collectors masked to group assignment | 14 | 0.050 | 0.069 | ||
|
| |||||
| Did not report data collectors masked to group assignment |
41 | 0.293 | 0.054 | ||
|
| |||||
| Intention-to-treat approach | 0.259 | .611 | |||
|
| |||||
| Reported intention-to-treat approach | 11 | 0.256 | 0.104 | ||
|
| |||||
| Did not report intention-to-treat approach | 44 | 0.195 | 0.059 | ||
|
| |||||
| Outcome data | .554 | .457 | |||
|
| |||||
| Continuous outcome data in primary report | 28 | 0.243 | 0.085 | ||
|
| |||||
| Dichotomous outcome data in primary report | 27 | 0.167 | 0.057 | ||
|
| |||||
k denotes number of comparisons, effect size is standardized mean difference, Q is a conventional homogeneity statistic
Table 4.
Continuous Moderator Results for Medication Adherence: Treatment vs. Control at Outcome
|
| ||||||
|---|---|---|---|---|---|---|
| Moderator | k | Slope | Standard Error | Tau2 | Qmodel | p (slope) |
|
| ||||||
| SAMPLE ATTRIBUTE MODERATORS | ||||||
|
| ||||||
| Age | 47 | −.007 | .003 | .085 | 4.771 | .029 |
|
| ||||||
| Percent African-American subjects | 55 | −.000 | .001 | .081 | 0.124 | .724 |
|
| ||||||
| Percent Hispanic subjects | 38 | .010 | .001 | .064 | 0.685 | .408 |
|
| ||||||
| Percent women | 53 | −.000 | .068 | .081 | 0.547 | .459 |
|
| ||||||
| METHOD AND INTERVENTION MODERATORS | ||||||
|
| ||||||
| Sample size | 55 | −.000 | .000 | .081 | 1.115 | .291 |
|
| ||||||
| Attrition proportion | 53 | −.281 | .159 | .084 | 3.116 | .078 |
|
| ||||||
| Number of cultural relevance component reported |
55 | .014 | .020 | .080 | 0.537 | .464 |
|
| ||||||
k denotes number of comparisons, Q is a conventional homogeneity statistic, Tau2 is the between-study variance
Intervention location associated with underrepresented groups (“relevant”) was coded for three studies that reported interventions were delivered in underrepresented-group clinics, community centers, and churches. The low number of studies with this attribute makes these findings tentative. The difference in effect sizes between studies with relevant locations (0.422) and interventions not delivered in relevant locations (0.196) was not statistically significant.
Seven studies reported that interventions were delivered in the language of the study participants. The effect sizes for studies with language specificity and those in English were similar. The difference in effect sizes between studies that used underrepresented peer interventionists (s = 7, effect size = 0.134) and studies without peer interventionists (0.227) was not statistically significant. Five studies provided cultural sensitivity training to interventionists. The difference between studies with culturally sensitive interventions (0.420) and those without staff trained in cultural sensitivity (0.185) did not achieve statistical significance.
Eight investigators noted that their interventions included culturally-relevant concepts. These were not more effective than other interventions (see Table 3). Some studies altered the educational level of intervention materials developed for underrepresented samples with low education levels. This modification was not associated with significantly different effect sizes. The other items coded for cultural relevance were reported too infrequently for analyses: intervention tested in underrepresented adult focus group or panel of experts, underrepresented media personnel in intervention materials, subjects referred to community resources, compensation for subjects’ time and costs, and recruitment at location specific to underrepresented group.
Sample Moderator Analyses
The difference in effect sizes between studies recruiting low-income subjects (0.126) and studies not recruiting low-income participants (0.288) was not statistically significant. The difference between effect sizes of predominantly Latino subjects (0.306) and predominantly African-American samples (0.191) was not statistically significant. Studies with younger mean age subjects reported slightly higher effect sizes than studies with older subjects (see Table 4 for continuous moderator analysis results). The percentage of women in studies was not a significant moderator for MA effect size. Although studies that recruited samples with poor MA reported an effect size of 0.425, this was not statistically significantly different from studies enrolling subjects regardless of MA (0.159). Studies with HIV positive samples reported a mean MA effect size of 0.246. An effect size of 0.053 was calculated for studies composed entirely of subjects with hypertension.
Risk of Bias
Studies reported similar effect sizes regardless of random or nonrandom assignment of subjects to treatment and control conditions. Nor was the presence or absence of allocation concealment of subject assignment related to effect sizes. Only 14 studies reported that data collectors were masked for subject group assignment. These studies reported significantly smaller effect sizes (0.050) than studies that did not report such masking (0.293). Studies using intention-to-treat analyses reported similar effect sizes as compared to studies without such analyses. Sample size was unrelated to effect sizes. The trend for comparisons with lower attrition to report larger effect sizes was not statistically significant. Effect sizes were calculated separately for four kinds of MA measures. The largest effect sizes were reported for studies that used pill counts (0.539, k = 7) and electronic event monitoring container lids (0.421, k = 12) to measure MA. Lower effect sizes were reported by studies assessing MA using pharmacy refill (0.112, k = 7) and self-report (0.102, k = 28). In subgroup analyses of primary studies, the overall effect size for continuous data (0.243) was not significantly different from the overall effect size for dichotomous data studies (0.167).
Funnel plots of effect size vs. sampling variance revealed some evidence of publication bias among treatment vs. control group comparisons and for treatment pre-post comparisons. The control group pre-post comparison funnel plot did not suggest publication bias. Funnel plots are available from the corresponding author.
Discussion
This is the first comprehensive meta-analysis of interventions to increase MA among predominantly underrepresented participants. Health disparities in many chronic conditions relate directly to the proper use of medication. Thus, discovering the effectiveness of culturally relevant MA interventions is essential to developing the most effective approaches of improving MA among underrepresented adults.
This project’s comprehensive searching, quantitative synthesis with an overall effect size, and exploratory moderator analyses move past previous reviews of MA interventions among underrepresented samples. Earlier reviews used as few as four studies, failed to integrate study findings, and included reports with as few as 26% underrepresented samples (Bailey et al., 2009; Manias and Williams, 2010; Viswanathan et al., 2012). The modest significant effect size of .211 documents that treatment subjects ended studies with better MA than control subjects following interventions. It is difficult to determine if the effect size is clinically significant. Too few studies reported identical measures of MA to allow conversion of the effect size to an original metric. Except for a few diseases such as HIV, scant information is available about the amount of MA required for desired clinical outcomes (Peeters et al., 2011). Clinical outcomes for increases in MA vary among diseases, including infectious diseases such as HIV and non-infectious chronic illnesses such as hypertension, which were common among these primary studies. The expected and observed heterogeneity documents that not all interventions improve MA equally.
Discovering intervention characteristics linked with better MA outcomes is important for developing effective interventions (Viswanathan et al., 2012). This project’s moderator analysis was the first attempt to quantify attempts to make interventions culturally relevant and to explore these characteristics as potential moderators of effect sizes (Bailey et al., 2009). The culturally relevant characteristics were grounded in the studies by the method of recording verbatim descriptions then creating coding categories based on the studies themselves. Neither the presence of any strategy to enhance cultural relevance nor the total number of cultural relevance strategies were related effect sizes for MA. This finding contrasts with common wisdom that health-behavior-change interventions improve as their cultural relevance increases (Kreuter and McClure, 2004; Lau, 2006; Mitrani, 2009; Resnicow et al., 1999).
Inadequate reporting of intervention details is common in intervention reports (Conn and Groves, 2011; Manias and Williams, 2010). Studies conducted by underrepresented researchers or using underrepresented interventionists may have used multiple cultural relevance strategies that they did not describe in reports. Such researchers may consider it normal to enhance cultural relevance and so fail to see that these intervention attributes need to be reported (Kumanyika and Yancey, 2009). It is a persistent problem that no standardized language exists for describing interventions’ cultural relevance. This void hampers scientific progress and implementation of successful interventions in practice.
Given that only a few studies reported each individual moderator, findings should be considered hypothesis-generating and exploratory. The magnitude of potential differences in effect sizes in the exploratory moderator analyses suggests that future research (1) compare interventions located in settings familiar to subjects with interventions in traditional research locations; (2) compare underrepresented peer interventionists to non-underrepresented peer interventionists; and (3) test the use of cultural sensitivity training to improve outcomes. Further research in underrepresented populations should compare intervention effectiveness between African-American and Latino subjects. Future research should focus on other underrepresented groups such as Native Hawaiians. This moderator analysis was limited by the scant information about attempts to make studies culturally relevant. This review’s most interesting finding was perhaps the scarcity of efforts to increase cultural relevance in the studies. The lack of attention to cultural relevance of interventions may contribute to the modest effect size across studies and the resulting lack of power to detect significant differences in effect size due to intervention characteristics designed to improve cultural relevance.
Extant research compares intervention groups to control groups. Identifying causal links between cultural relevance and intervention effectiveness requires direct comparison of culturally-relevant interventions to interventions that are not matched to the underrepresented population (Domenech Rodríguez and Bernal, 2012). Until such comparative-effectiveness studies are conducted, no definitive conclusions are possible regarding the efficacy of culturally relevant intervention approaches.
The impact of heterogeneity in underrepresented groups needs further exploration. Lack of consistent terminology about samples, especially for Latino populations (Manias and Williams, 2010), diminishes generalizability of research findings. Audience-segmentation strategies can increase cultural relevance (Manias and Williams, 2010; Rimal and Adkins, 2003). Based on the common practice of sorting subjects into broad racial/ethnic categories, investigators may make erroneous assumptions about such groups and miss important cultural distinctions among underrepresented samples (Bernal et al., 1995; Kreuter and McClure, 2004; Peeters et al., 2011). This form of stereotyping may reduce potential effectiveness of interventions (Bernal et al., 1995). None of the primary studies in this review used individually- or subgroup-tailored interventions based on individual- or subgroup-matched cultural relevance strategies. Underrepresented group membership may be associated with other characteristics that may influence MA. For example, many studies of MA in underrepresented groups have targeted low-income subjects or included predominantly low-income subjects without specifically recruiting subjects for these characteristics (Lewis et al., 2012). The potential association between MA and other sociodemographic characteristics such as education level, health literacy, or income may confound understanding of underrepresented samples (Ostini and Kairuz, 2014; Peeters et al., 2011).
Conclusion
Inadequate MA is costly at many levels. Non-adherence to medications is estimated to cost between $100 billion and $289 billion dollars in health care expenditures (Viswanathan et al., 2012). More importantly, inadequate MA contributes to significant health disparities, morbidity, and mortality among underrepresented populations. This comprehensive systematic review and meta-analysis documented statistically significant but modest magnitude improvements in MA. The attempts, limited to date, to enhance the cultural relevance of MA interventions targeting underrepresented samples may contribute to limited effectiveness. Future research should test specific strategies to increase cultural relevance.
Supplementary Material
Highlights.
We meta-analyzed medication adherence interventions among underrepresented adults.
Interventions successfully increased medication adherence relative to control.
Moderator analyses examined links between cultural relevance features and outcomes.
Primary studies often lacked detail on culturally relevant strategies.
Future research should fully describe and test cultural relevance of interventions.
Acknowledgements
The project described was supported by Award Number R01NR011990 (Conn-PI) from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding source had no role in designing, collecting, analyzing, or interpreting data. The funding source did not have any role in writing the report or deciding whether the paper should be submitted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement
The authors declare that there are no conflicts of interest.
References
- Anderson KO, Mendoza TR, Payne R, Valero V, Palos GR, Nazario A, Richman SP, Hurley J, Gning I, et al. Pain education for underserved minority cancer patients: A randomized controlled trial. J. Clin. Oncol. 2004;22:4918–25. doi: 10.1200/JCO.2004.06.115. [DOI] [PubMed] [Google Scholar]
- Andrade AS, McGruder HF, Wu AW, Celano SA, Skolasky RL, Jr., Selnes OA, Huang IC, McArthur JC. A programmable prompting device improves adherence to highly active antiretroviral therapy in HIV-infected subjects with memory impairment. Clin. Infect. Dis. 2005;41:875–82. doi: 10.1086/432877. [DOI] [PubMed] [Google Scholar]
- Austin DL. Selected Nursing Interventions for Noncompliant Hypertensive Patients. Texas Woman's University; Denton, TX: 1986. [Google Scholar]
- Babamoto KS, Sey KA, Camilleri AJ, Karlan VJ, Catalasan J, Morisky DE. Improving diabetes care and health measures among Hispanics using community health workers: Results from a randomized controlled trial. Health Educ. Behav. 2009;36:113–26. doi: 10.1177/1090198108325911. [DOI] [PubMed] [Google Scholar]
- Bailey EJ, Cates CJ, Kruske SG, Morris PS, Brown N, Chang AB. Culture-Specific Programs for Children and Adults from Minority Groups Who Have Asthma. Wiley-Blackwell; West Sussex: 2009. [Google Scholar]
- Berlin JA. Invited commentary: benefits of heterogeneity in meta-analysis of data from epidemiologic studies. Am. J. Epidemiol. 1995;142:383–7. doi: 10.1093/oxfordjournals.aje.a117645. [DOI] [PubMed] [Google Scholar]
- Bernal G, Bonilla J, Bellido C. Ecological validity and cultural sensitivity for outcome research: issues for the cultural adaptation and development of psychosocial treatments with Hispanics. J. Abnorm. Child Psychol. 1995;23:67–82. doi: 10.1007/BF01447045. [DOI] [PubMed] [Google Scholar]
- Bernal G, Domenech Rodriguez MM. Cultural adaptation in context: psychotherapy as a historical account of adaptations. In: Bernal G, Domenech Rodriguez MM, editors. Cultrual Adaptations: Tools for Evidence-Based Practice with Diverse Populations. American Psychological Association; Washington, D.C.: 2012. pp. 3–22. [Google Scholar]
- Bogart LM, Wagner GJ, Mutchler MG, Risley B, McDavitt BW, McKay T, Klein DJ. Community HIV treatment advocacy programs may support treatment adherence. AIDS Educ. Prev. 2012;24:1–14. doi: 10.1521/aeap.2012.24.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogner H, de Vries H. Integration of depression and hypertension treatment: A pilot, randomized controlled trial. Ann. Fam. Med. 2008;6:295–301. doi: 10.1370/afm.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogner HR, de Vries HF. Integrating type 2 diabetes mellitus and depression treatment among African Americans: A randomized controlled pilot trial. Diabetes Educ. 2010;36:284–92. doi: 10.1177/0145721709356115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdett S, Stewart LA, Tierney JF. Publication bias and meta-analyses: a practical example. Int. J. Technol. Assess. Health Care. 2003;19:129–34. doi: 10.1017/s0266462303000126. [DOI] [PubMed] [Google Scholar]
- Burrelle TN. Evaluation of an interdisciplinary compliance service for elderly hypertensives. J. Geriatr. Drug Ther. 1986;1:23–51. [Google Scholar]
- Chaisson RE, Barnes GL, Hackman J, Watkinson L, Kimbrough L, Metha S, Cavalcante S, Moore RD. A randomized, controlled trial of interventions to improve adherence to isoniazid therapy to prevent tuberculosis in injection drug users. Am. J. Med. 2001;110:610–5. doi: 10.1016/s0002-9343(01)00695-7. [DOI] [PubMed] [Google Scholar]
- Christensen AJ. Patient Adherence to Medical Treatment Regimens. Yale University Press; New Haven: 2004. [Google Scholar]
- Conn V, Chan K, Banks J, Ruppar T, Scharff J. Cultural relevance of physical activity intervention research with underrepresented populations. The International Quarterly of Community Health Education. doi: 10.2190/IQ.34.4.g. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn VS, Groves PS. Protecting the power of interventions through proper reporting. Nurs. Outlook. 2011;59:318–25. doi: 10.1016/j.outlook.2011.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn VS, Hafdahl AR, Mehr DR, LeMaster JW, Brown SA, Nielsen PJ. Metabolic effects of interventions to increase exercise in adults with type 2 diabetes. Diabetologia. 2007;50:913–21. doi: 10.1007/s00125-007-0625-0. [DOI] [PubMed] [Google Scholar]
- Conn VS, Phillips LJ, Ruppar TM, Chase JA. Physical activity interventions with healthy minority adults: meta-analysis of behavior and health outcomes. J. Health Care Poor Underserved. 2012;23:59–80. doi: 10.1353/hpu.2012.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper H, Hedges LV, Valentine JC. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. p. 615. [Google Scholar]
- Cordasco KM, Asch SM, Bell DS, Guterman JJ, Gross-Schulman S, Ramer L, Elkayam U, Franco I, Leatherwood CL, et al. A low-literacy medication education tool for safety-net hospital patients. Am. J. Prev. Med. 2009;37:S209–16. doi: 10.1016/j.amepre.2009.08.018. [DOI] [PubMed] [Google Scholar]
- DiIorio C, McCarty F, Resnicow K, McDonnell Holstad M, Soet J, Yeager K, Sharma SM, Morisky DE, Lundberg B. Using motivational interviewing to promote adherence to antiretroviral medications: A randomized controlled study. AIDS Care. 2008;20:273–83. doi: 10.1080/09540120701593489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiIorio C, Resnicow K, McDonnell M, Soet J, McCarty F, Yeager K. Using motivational interviewing to promoteadherence to antiretroviral medications: A pilot study. J. Assoc. Nurses AIDS Care. 2003;14:52–62. doi: 10.1177/1055329002250996. [DOI] [PubMed] [Google Scholar]
- Domenech Rodríguez MM, Bernal G. Bridging the gap between research and practice in a multicultural world. In: Bernal G, Domenech Rodríguez MM, editors. Cultural adaptations: Tools for evidence-based practice with diverse populations. American Psychological Association; Washington DC: 2012. pp. 265–87. [Google Scholar]
- Dunbar-Jacob J, Erlen JA, Schlenk EA, Ryan CM, Sereika SM, Doswell WM. Adherence in chronic disease. Annu. Rev. Nurs. Res. 2000;18:48–90. [PubMed] [Google Scholar]
- Fernandez S, Scales KL, Pineiro JM, Schoenthaler AM, Ogedegbe G. A senior center-based pilot trial of the effect of lifestyle intervention on blood pressure in minority elderly people with hypertension. J. Am. Geriatr. Soc. 2008;56:1860–66. doi: 10.1111/j.1532-5415.2008.01863.x. [DOI] [PubMed] [Google Scholar]
- Fisher J, Amico K, Fisher W, Cornman D, Shuper P, Trayling C, Redding C, Barta W, Lemieux A, et al. Computer-based intervention in HIV clinical care setting improves antiretroviral adherence: The LifeWindows Project. AIDS Behav. 2011;15:1635–46. doi: 10.1007/s10461-011-9926-x. [DOI] [PubMed] [Google Scholar]
- Freedman D. The Effects of Group Mental Health Intervention on Adherence to Medication, for People with HIV and AIDS. New York University; New York City: 2007. p. 111. [Google Scholar]
- Garg AX, Hackam D, Tonelli M. Systematic review and meta-analysis: when one study is just not enough. Clin. J. Am. Soc. Nephrol. 2008;3:253–60. doi: 10.2215/CJN.01430307. [DOI] [PubMed] [Google Scholar]
- Gazmararian J, Jacobson KL, Pan Y, Schmotzer B, Kripalani S. Effect of a pharmacy-based health literacy intervention and patient characteristics on medication refill adherence in an urban health system. Ann. Pharmacother. 2010;44:80–7. doi: 10.1345/aph.1M328. [DOI] [PubMed] [Google Scholar]
- Glanz K, Beck AD, Bundy L. Impact of a health communication intervention to improve glaucoma treatment adherence: Results of the interactive study to increase glaucoma adherence to treatment trial. Arch. Ophthalmol. 2012:1–7. doi: 10.1001/archophthalmol.2012.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper DC. Application of Orem's theoretical constructs to self-care medication behaviors in the elderly. ANS Adv. Nurs. Sci. 1984;6:29–46. doi: 10.1097/00012272-198404000-00008. [DOI] [PubMed] [Google Scholar]
- Hedges L, Olkin I. Statistical Methods for Meta-Analysis. Academic Press; Orlando, FL: 1985. [Google Scholar]
- Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch. Intern. Med. 2007;167:1853–60. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holzemer WL, Bakken S, Portillo CJ, Grimes R, Welch J, Wantland D, Mullan JT. Testing a nurse-tailored HIV medication adherence intervention. Nurs. Res. 2006;55:189–97. doi: 10.1097/00006199-200605000-00005. [DOI] [PubMed] [Google Scholar]
- Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: A review from the patient's perspective. Ther. Clin. Risk Manag. 2008;4:269–86. doi: 10.2147/tcrm.s1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Kalichman MO, Cherry C, Swetzes C, Amaral CM, White D, Jones M, Grebler T, Eaton L. Brief behavioral self-regulation counseling for HIV treatment adherence delivered by cell phone: An initial test of concept trial. AIDS Patient Care STDS. 2011;25:303–10. doi: 10.1089/apc.2010.0367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kellaway GS, McCrae E. The effect of counselling on compliance-failure in patient drug therapy. N. Z. Med. J. 1979;89:161–5. [PubMed] [Google Scholar]
- Koenig LJ, Pals SL, Bush T, Pratt Palmore M, Stratford D, Ellerbrock TV. Randomized controlled trial of an intervention to prevent adherence failure among HIV-infected patients initiating antiretroviral therapy. Health Psychol. 2008;27:159–69. doi: 10.1037/0278-6133.27.2.159. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, McClure SM. The role of culture in health communication. Annu. Rev. Public Health. 2004;25:439–55. doi: 10.1146/annurev.publhealth.25.101802.123000. [DOI] [PubMed] [Google Scholar]
- Kripalani S, Schmotzer B, Jacobson TA. Improving medication adherence through graphically enhanced interventions in coronary heart disease (IMAGE-CHD): A randomized controlled trial. J. Gen. Intern. Med. 2012:1–9. doi: 10.1007/s11606-012-2136-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumanyika SK, Yancey AK. Physical activity and health equity: evolving the science. Am. J. Health Promot. 2009;23:S4–7. doi: 10.4278/ajhp.23.6.S4. [DOI] [PubMed] [Google Scholar]
- Laine L, Estrada R, Trujillo M, Fukanaga K, Neil G. Randomized comparison of differing periods of twice-a-day triple therapy for the eradication of Helicobacter pylori. Aliment. Pharmacol. Ther. 1996;10:1029–33. doi: 10.1046/j.1365-2036.1996.111282000.x. [DOI] [PubMed] [Google Scholar]
- Lau AS. Making the case for selective and directed cultural adaptations of evidence-based treatments: examples from parent training. Clin. Psychol. (New York) 2006;13:295–310. [Google Scholar]
- Lewis LM, Schoenthaler AM, Ogedegbe G. Patient factors, but not provider and health care system factors, predict medication adherence in hypertensive black men. J. Clin. Hypertens. 2012;14:250–5. doi: 10.1111/j.1751-7176.2012.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- Lipsey M, Wilson D. Practical Meta-Analysis. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- Manias E, Williams A. Medication adherence in people of culturally and linguistically diverse backgrounds: a meta-analysis. Ann. Pharmacother. 2010;44:964–82. doi: 10.1345/aph.1M572. [DOI] [PubMed] [Google Scholar]
- Mann T. Effects of future writing and optimism on health behaviors in HIV-infected women. Ann. Behav. Med. 2001;23:26–33. doi: 10.1207/S15324796ABM2301_5. [DOI] [PubMed] [Google Scholar]
- Martin MY, Kim YI, Kratt P, Litaker MS, Kohler CL, Schoenberger YM, Clarke SJ, Prayor-Patterson H, Tseng TS, et al. Medication adherence among rural, low-income hypertensive adults: A randomized trial of a multimedia community-based intervention. Am. J. Health Promot. 2011;25:372–78. doi: 10.4278/ajhp.090123-QUAN-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenney JM, Slining JM, Henderson HR, Devins D, Barr M. The effect of clinical pharmacy services on patients with essential hypertension. Circulation. 1973;48:1104–11. doi: 10.1161/01.cir.48.5.1104. [DOI] [PubMed] [Google Scholar]
- McPherson-Baker S, Malow RM, Penedo F, Jones DL, Schneiderman N, Klimas NG. Enhancing adherence to combination antiretroviral therapy in non-adherent HIV-positive men. AIDS Care. 2000;12:399–404. doi: 10.1080/09540120050123792. [DOI] [PubMed] [Google Scholar]
- Migneault J, Dedier J, Wright J, Heeren T, Campbell M, Morisky D, Rudd P, Friedman R. A culturally adapted telecommunication system to improve physical activity, diet quality, and medication adherence among hypertensive African–Americans: A randomized controlled trial. Ann. Behav. Med. 2012:1–12. doi: 10.1007/s12160-011-9319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitrani V. Reducing health disparities for Hispanics through the development of culturally tailored interventions. Hisp. Health Care Int. 2009;7:2–4. doi: 10.1891/1540-4153.7.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moitra E, Herbert JD, Forman EM. Acceptance-based behavior therapy to promote HIV medication adherence. AIDS Care. 2011;23:1660–7. doi: 10.1080/09540121.2011.579945. [DOI] [PubMed] [Google Scholar]
- Muir KW, Ventura A, Stinnett SS, Enfiedjian A, Allingham RR, Lee PP. The influence of health literacy level on an educational intervention to improve glaucoma medication adherence. Patient Educ. Couns. 2012;87:160–4. doi: 10.1016/j.pec.2011.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundy LM. Effective Antiretroviral Drug Delivery to Promote HIV-Related Population Health. Saint Louis University; St. Louis, MO: 2009. [Google Scholar]
- Murphy DA, Marelich WD, Rappaport NB, Hoffman D, Farthing C. Results of an antiretroviral adherence intervention: STAR (Staying Healthy: Taking Antiretrovirals Regularly) J. Int. Assoc. Physicians AIDS Care. 2007;6:113–24. doi: 10.1177/1545109707301243. [DOI] [PubMed] [Google Scholar]
- Newsome JM. Shaping Behaviors Associated with Hypertension Management Among African American Women. University of Michigan; Ann Arbor, MI: 1995. [Google Scholar]
- Orwin R, Vevea J, Valentine J. Evaluating coding decisions. In: Cooper H, Hedges L, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 177–203. [Google Scholar]
- Ostini R, Kairuz T. Investigating the association between health literacy and non-adherence. International Journal of Clinical Pharmacy. 2014;36:36–44. doi: 10.1007/s11096-013-9895-4. [DOI] [PubMed] [Google Scholar]
- Parsons JT, Golub SA, Rosof E, Holder C. Motivational interviewing and cognitive-behavioral intervention to improve HIV medication adherence among hazardous drinkers: A randomized controlled trial. J. Acquir. Immune Defic. Syndr. 2007;46:443–50. doi: 10.1097/qai.0b013e318158a461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeters B, Van Tongelen I, Boussery K, Mehuys E, Remon JP, Willems S. Factors associated with medication adherence to oral hypoglycaemic agents in different ethnic groups suffering from type 2 diabetes: a systematic literature review and suggestions for further research. Diabet. Med. 2011;28:262–75. doi: 10.1111/j.1464-5491.2010.03133.x. [DOI] [PubMed] [Google Scholar]
- Pigott T. Methods for handling missing data in research synthesis. In: Cooper H, Hedges L, editors. The handbook of research synthesis. Russell Sage Foundation; New York, NY: 1994. pp. 163–76. [Google Scholar]
- Powell KW. Strategy to Improve Blood Pressure Control and Medication Adherence. Rush University; Chicago, IL: 2002. p. 224. [Google Scholar]
- Purcell DW, Latka MH, Metsch LR, Latkin CA, Gómez CA, Mizuno Y, Arnsten JH, Wilkinson JD, Knight KR, et al. Results from a randomized controlled trial of a peer-mentoring intervention to reduce HIV transmission and increase access to care and adherence to HIV medications among HIV-seropositive injection drug users. J. Acquir. Immune Defic. Syndr. 2007;46:S35–S47. doi: 10.1097/QAI.0b013e31815767c4. [DOI] [PubMed] [Google Scholar]
- Raudenbush S. Random effects models. In: Cooper H, Hedges L, editors. The Handbook of Research Synthesis. Russell Sage Foundation; New York, NY: 1994. pp. 301–21. [Google Scholar]
- Remien RH, Stirratt MJ, Dolezal C, Dognin JS, Wagner GJ, Carballo-Dieguez A, El-Bassel N, Jung TM. Couple-focused support to improve HIV medication adherence: A randomized controlled trial. AIDS. 2005;19:807–14. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn. Dis. 1999;9:10–21. [PubMed] [Google Scholar]
- Rimal RN, Adkins AD. Using computers to narrowcast health messages: the role of audience segmentation, targeting and tailoring in health promotion. In: Thompson TL, Dorsey A, Miller KI, Parrott R, editors. Handbook of Health Communication. Routledge; New York, NY: 2003. pp. 498–99. [Google Scholar]
- Rothstein HR, Hopewell S. Grey literature. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 103–25. [Google Scholar]
- Saha S, Freeman M, Toure J, Tippens KM, Weeks C, Ibrahim S. Racial and ethnic disparities in the VA health care system: a systematic review. J. Gen. Intern. Med. 2008;23:654–71. doi: 10.1007/s11606-008-0521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanders Thompson VL, Cavazos-Rehg PA, Jupka K, Caito N, Cratzke J, Tate KY, Deshpande A, Kreuter MW. Evidential preferences: cultural appropriateness strategies in health communications. Health Educ. Res. 2008;23:549–59. doi: 10.1093/her/cym029. [DOI] [PubMed] [Google Scholar]
- Sewell JL, Velayos FS. Systematic review: The role of race and socioeconomic factors on IBD healthcare delivery and effectiveness. Inflamm. Bowel Dis. 2013;19:627–43. doi: 10.1002/ibd.22986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Pantalone DW, Plummer MD, Huang B. A randomized controlled trial of a peer support intervention targeting antiretroviral medication adherence and depressive symptomatology in HIV-positive men and women. Health Psychol. 2007;26:488–95. doi: 10.1037/0278-6133.26.4.488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutton AJ. Publicaton bias. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 435–52. [Google Scholar]
- Tagliacozzo DM, Luskin DB, Lashof JC, Ima K. Nurse intervention and patient behavior: An experimental study. Am. J. Public Health. 1974;64:596–603. doi: 10.2105/ajph.64.6.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valentine J. Judging the quality of primary research. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 129–46. [Google Scholar]
- van Servellen G, Nyamathi A, Carpio F, Pearce D, Garcia-Teague L, Herrera G, Lombardi E. Effects of a treatment adherence enhancement program on health literacy, patient-provider relationships, and adherence to HAART among low-income HIV-positive Spanish-speaking Latinos. AIDS Patient Care STDS. 2005;19:745–59. doi: 10.1089/apc.2005.19.745. [DOI] [PubMed] [Google Scholar]
- Viswanathan M, Golin CE, Jones CD, Ashok M, Blalock SJ, Wines RC, Coker-Schwimmer EJ, Rosen DL, Sista P, et al. Interventions to improve adherence to self-administered medications for chronic diseases in the United States: a systematic review. Ann. Intern. Med. 2012;157:785–95. doi: 10.7326/0003-4819-157-11-201212040-00538. [DOI] [PubMed] [Google Scholar]
- Vivian EM. Improving blood pressure control in a pharmacist-managed hypertension clinic. Pharmacotherapy. 2002;22:1533–40. doi: 10.1592/phco.22.17.1533.34127. [DOI] [PubMed] [Google Scholar]
- Walker CC. An educational intervention for hypertension management in older African Americans. Ethn. Dis. 2000;10:165–74. [PubMed] [Google Scholar]
- Webel AR. Testing a peer-based symptom management intervention for women living with HIV/AIDS. AIDS Care. 2010;22:1029–40. doi: 10.1080/09540120903214389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger M, Tierney WM, Booher P, Katz BP. The impact of increased contact on psychosocial outcomes in patients with osteoarthritis: A randomized, controlled trial. J. Rheumatol. 1991;18:849–54. [PubMed] [Google Scholar]
- Werner RT., Sr. The effects of health education on the compliance of hypertensive patients to medical regimens. Temple University; Philadelphia, PA: 1979. [Google Scholar]
- White H. Scientific communication and literature retrieval. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 51–71. [Google Scholar]
- Wilson D. Systematic coding. In: Cooper H, Hedges L, Valentine J, editors. The Handbook of Research Synthesis and Meta-Analysis. 2nd Russell Sage Foundation; New York: 2009. pp. 159–76. [Google Scholar]
- Wohl AR, Garland WH, Valencia R, Squires K, Witt MD, Kovacs A, Larsen R, Hader S, Anthony MN, et al. A randomized trial of directly administered antiretroviral therapy and adherence case management intervention. Clin. Infect. Dis. 2006;42:1619–27. doi: 10.1086/503906. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Adherence to Long-Term Therapies: Evidence for Action. World Health Organization; 2003. pp. 1–198. [Google Scholar]
- Wyatt GE, Longshore D, Chin D, Carmona JV, Loeb TB, Myers HF, Warda U, Liu H, Rivkin I. The efficacy of an integrated risk reduction intervention for HIV-positive women with child sexual abuse histories. AIDS Behav. 2004;8:453–62. doi: 10.1007/s10461-004-7329-y. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.