Abstract
Objective
To implement and evaluate the impact of a Teachable Moment Communication Process (TMCP) training intervention on clinicians’ smoking cessation counseling behaviors in practice.
Method
Using a group randomized trial, 31 community-based, primary care clinicians in Northeast Ohio received either TMCP training or an attention control (2010–2012). TMCP training consisted of two, three-hour sessions involving didactic instruction, skill practice with standardized patients, and coaching. Clinician performance of TMCP elements was assessed by coding audio-recordings of routine visits with smokers at baseline and post-intervention (n=806).
Results
Baseline performance of all TMCP elements were similar in the two groups. After the intervention, TMCP-trained clinicians were more often observed advising patients to quit while linking smoking to the patient’s concern (58% vs. 44%, p=0.01), expressing optimism (36% vs. 3%, p<0.001), expressing partnership (40% vs. 12%, p=0.003) and eliciting the patient’s readiness to quit (84% vs. 65%, p=0.006) than clinicians in the comparison group. TMCP-trained clinician responses were also better aligned with patients’ expressed readiness to quit smoking than comparison group clinicians (p<0.001).
Conclusion
The intervention significantly changed the content of clinicians’ smoking cessation communication in ways consistent with the TMCP model for health behavior change.
Keywords: Tobacco counseling, primary care, brief advice, cluster randomized trial, audio recordings
Introduction
Tobacco use is the leading cause of preventable death in the United States (Mokdad et al., 2004; U.S. Department of Health and Human Services, 2011), yet nearly 20% of adult Americans smoke (Centers for Disease Control and Prevention, 2012a). Since the majority of U.S. smokers report seeing a primary care clinician at least once per year (Centers for Disease Control and Prevention, 2012b), these clinicians are uniquely positioned to provide effective brief smoking cessation counseling (Gorin and Heck, 2004; Katz et al., 2004; Stead et al., 2013). However, less than a third of visits with smokers include counseling about smoking (Coleman and Wilson, 2000; Thorndike et al., 2007).
Current treatment guidelines recommend using the 5 A’s (Ask, Advise, Assess, Assist, and Arrange) heuristic (The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives, 2000) to address smoking at every visit, complemented by motivational interviewing (MI) (Hettema et al., 2005) for patients unwilling to attempt cessation (Fiore et al., 2008). While the 5 A’s offers a concise treatment algorithm to guide clinical decision making at the point of care, research shows clinicians have not fully adopted the approach due to barriers that include competing visit priorities, lack of skills, concern for the clinician-patient relationship, and perceptions of insufficient patient motivation (Association of American Medical Colleges, 2007; Stead et al., 2009; Tong et al., 2010). Further, although MI has shown promise as a technique for encouraging cessation in the primary care setting (Butler et al., 1999; Lai et al., 2010; Soria et al., 2006; VanBuskirk and Wetherell, 2014), notable concerns exist regarding the amount of formal training and time needed to use the technique effectively (Emmons and Rollnick, 2001; Rubak et al., 2005; VanBuskirk and Wetherell, 2014)
The Teachable Moment Communication Process (TMCP) draws from these approaches and communication theory to offer an innovative communication technique designed to fit into the progression of the primary care visit. The TMCP makes use of naturally occurring opportunities to stimulate health behavior change, known as “teachable moments” (Cohen et al., 2011; Lawson and Flocke, 2009; McBride et al., 2008, 2003). While initially conceived as unpredictable or serendipitous events, recent research suggests that teachable moments can be initiated during primary care visits when the clinician initiates discussion of a problematic health behavior, such as smoking, and links that behavior to a concern that the patient has identified as salient (Cohen et al., 2011; Lawson and Flocke, 2009). The clinician attempts to motivate behavior change using this transition by portraying smoking as germane to the patient’s salient concern and as problematic. Patient resistance at this point can lead to ineffective behavior change scenarios, (Pilnick and Coleman, 2003), and clinician skill to navigate such resistance may be insufficient (Carroll et al., 2011; Cohen et al., 2011; Werner et al., 2013). Therefore, the TMCP guides clinicians to provide a brief quit message conveying concern, optimism, and partnership first, then elicits the patient’s honest perspective about smoking cessation so that the clinician can counsel in alignment with the patient’s expressed level of readiness to change (Flocke et al., 2012). The approach draws on other health behavior change strategies including solutions focused therapy and motivational interviewing, but the TMCP is distinct in that it is very brief, it is designed for a context where discussing smoking is not the primary reason bringing the clinician and the patient together, and the way in which the smoking talk is initiated is opportunistic and fits the flow of addressing multiple problems during a primary care visit. The TMCP training intervention is intended to impart primary care clinicians communication skills to address smoking that are theory- and evidence-based, effective, and feasible within the clinical setting (Flocke et al., 2012). The purpose of this study was to implement and evaluate the impact of a TMCP training intervention on clinicians’ smoking cessation counseling behaviors in practice.
Materials and Methods
Study design
This study represents a group randomized trial with clinicians as the unit of randomization and a 1-to-1 allocation ratio (see Figure 1). Cross-sectional cohorts of patients who reported smoking tobacco represent baseline and post-training cohorts for the intervention and comparison group of clinicians.
Figure 1.
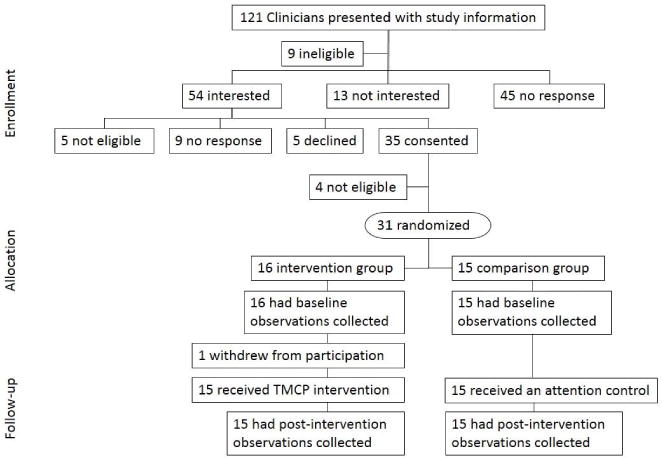
Clinician enrollment, randomization in 2010, and follow-up CONSORT flow diagram. Data collection with clinicians and patients in Northeast Ohio.
Clinician participants
Thirty-one community-based primary care clinicians in northeastern Ohio were recruited using a practice-based research network and invitations made to all community-based, primary care practices affiliated with any of the area’s three largest hospital systems from May 2010 to December 2010. Criteria for clinician participation included 1) being a family medicine or general internal medicine physician or nurse practitioner who, 2) provided care for adults 3) in a community-based practice (i.e. not residency or hospital based) for 4) a minimum of two days per week 5) within 25 miles of the research office. Incentives offered included CME credit and maintenance of board certification credits. Covariate adaptive randomization (Kang et al., 2008) was used to balance clinician gender and healthcare system affiliation when assigning clinicians to receive the TMCP intervention for smoking cessation (n=16) or an attention control consisting of a multimedia educational resource for colon cancer screening (n=15). Group allocation was generated by the study data manager. The PI enrolled clinician participants; research staff enrolled patient participants. Clinicians were blinded to group assignment during baseline data collection. Patient participants and qualitative data analysts were blinded to clinician group assignments throughout the study.
Patient participants
Between July 2010 and December 2011, all patients presenting to the practice of an enrolled clinician during data collection were approached and screened for eligibility prior to seeing the clinician. Participation was limited to patients who were 1) seeing a participating clinician, 2) 18–70 years old, 3) spoke either English or Spanish, and 4) reported currently smoking cigarettes or small cigars ‘some days’ or ‘every day’ and, on average, at least one cigarette per day or small cigar per week. Participants were informed only that the study focused on doctor-patient communication about health behaviors like smoking, exercise, and diet; no specific study hypotheses were shared. Informed consent and a survey were completed by all patients in the privacy of the exam room prior to the beginning of the visit, which was audio recorded. Target recruitment was 12 patients per clinician per enrollment period. The institutional review boards of University Hospitals Case Medical Center, MetroHealth Medical Center, and the Cleveland Clinic approved all study procedures.
The TMCP training intervention
After baseline data collection, clinicians in the intervention group received training in the TMCP. A thorough description of the TMCP intervention’s theoretical framework, development process, and content was published previously (Flocke et al., 2012). In brief, the clinicians were trained to perform the five core skills of the TMCP (see Figure 2) during two, three-hour long sessions at the Mount Sinai Skills and Simulation Center in Cleveland, Ohio. For each core skill, classroom-based didactic instruction was combined with video demonstrations of the TMCP. Additionally, clinician participants were partnered and took turns practicing each core skill in structured exercises with trained, standardized patients. Each session culminated with skill practice exercises with new standardized patients in simulated exam rooms. Exercises focused on using the TMCP elements in sequence and were video recorded for participant review. TMCP trainers provided ongoing feedback to participants, and clinician participants both provided and received feedback from fellow participants. The format and content of the training were standardized through the use of presentation scripts, a presenter’s teaching guide, a participant’s workbook, and detailed training for all standardized patients.
Figure 2.
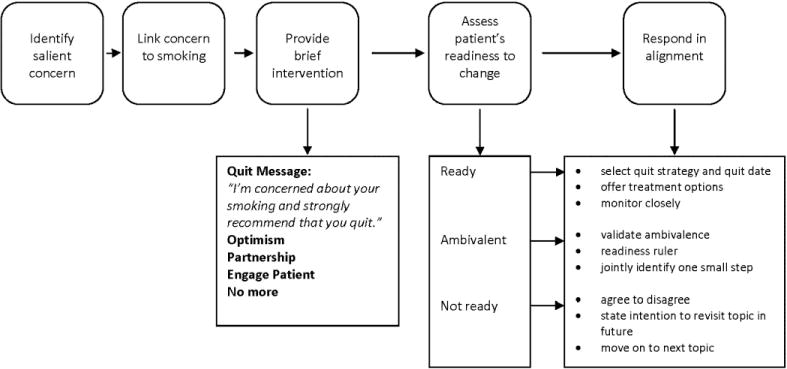
Schematic of the Teachable Moment Communication Process.
Note: Figure reproduced with permission (BioMed Central Open Access license); originally published by BioMed Central in Flocke et al. BMC Health Services Research 2012, 12:109.
Of the 16 clinicians randomized to receive the TMCP intervention, one withdrew from participation after randomization and baseline data collection but prior to receiving the intervention. Three other clinicians did not attend one or both sessions with the group, but were given the complete TMCP intervention during one-on-one training with a TMCP instructor. On average, observations of intervention group clinicians in the post-training period occurred 35 days (SD=21) after TMCP training.
Analytic coding of audio-recorded visits
Experienced qualitative data analysts developed a comprehensive coding system to determine the extent to which the key elements of the TMCP were present in the audio-recorded visits. An example case is in the Appendix and the coding manual is available upon request. The systematic coding process generated the variables representing clinician smoking cessation counseling behaviors (definitions reported below) used in the subsequent quantitative analyses. Coding reliability of the TMCP element variables, calculated using Krippendorff’s alpha (Krippendorff, 2004, 1970), was good (0.57–1.00).
Key variables
Clinician group assignment (intervention or comparison group) and time period of patient enrollment (baseline or post-training) represent the main independent variables, and performance of each of the TMCP elements represent the primary outcome variables. TMCP elements included: Linking smoking to a salient concern, defined as identifying a symptom discussed during the visit that the patient was concerned about and linking it to smoking; brief advice including a quit statement, defined as a directive statement urging the patient to quit smoking, an expression of concern about the effects of smoking, an expression of optimism that the patient could eventually quit, and an expression of partnership in the quitting process; and engaging the patient, or asking the patient their thoughts about quitting smoking in an open-ended format, and giving the patient an opportunity to speak regarding their readiness to change, or eliciting level of readiness to quit. The patient’s response regarding their level of readiness was rated as “not ready,” “ambivalent,” “ready,” or “unclear/unknown.” Finally, the extent to which the clinician’s responses were aligned with the patient’s expressed level of readiness was computed using an algorithm that assigned weighted values to clinician communication actions based on the patient’s expressed level of readiness. Actions consistent with TMCP training were assigned positive values, while inconsistent actions were assigned negative values. The values were summed and the resulting responding in alignment scores were then standardized across patient readiness levels so that the possible range was 0 (low alignment) to 10 (high level of alignment). (See Appendix for alignment score computation)
Other descriptive variables, collected by survey at enrollment, include patient and clinician demographics, patient’s self-reported health status, number of cigarettes smoked per day, reason for visit, and whether or not the enrolled clinician was the patient’s regular clinician.
Data management and quantitative analyses
All survey and coding data were entered and stored using REDCap (Harris et al., 2009) and data merging, cleaning, and quantitative analyses were conducted using SAS v9.3 (Cary, NC). Descriptive statistics were used to examine the distribution of demographic characteristics of clinician and patient participants. Characteristics of eligible patients who declined to participate in the study were compared to those who agreed to participate. T-tests and chi-squared tests were used to evaluate differences between groups.
The main analyses compared performance of each of the key TMCP elements by clinician randomization group by time period of data collection (baseline or post-training). An intention to treat strategy was used. Analyses were adjusted for the clustering of multiple patient-level observations for each clinician using STATA v12 (College Station, TX). Patient characteristics found to significantly differ between intervention and comparison groups were evaluated as potential covariates. Including these variables did not alter the findings; therefore, the results of the simplest models (without covariates) are reported. Rates of uptake for each TMCP element were also examined by calculating the proportion of visits each behavior was observed for each intervention group clinician, post-training.
This study was powered with a target of 30 clinicians and a minimum of 10 patients on average per clinician per time point. For the planned analyses, this sample size has 90% power to detect differences between groups in the magnitude of greater than 0.35 of a standard deviation or odds ratio of greater than 1.5. Effect sizes were computed using Cohen’s d for continuous variables and Phi for categorical variables. All associations were evaluated at the p<0.05 level. Analyses were completed in 2013.
Results
Clinicians randomized to the intervention and comparison groups were similar (see Table 1). A total of 7414 patients were screened for eligibility, and 1204 (16%) were eligible to participate; of those eligible, 840 (70%) enrolled in the study. Patients who declined participation were largely similar to those who enrolled, with the exception that participants were more likely to be female (61% vs. 54%, p=0.02), African-American (35% vs. 24%, p<0.001), and visiting their regular clinician (81% vs. 75%, p=0.03). Of the 840 patients who enrolled, 34 audio-recordings (4%) were unusable due to equipment failure or inaudible recording, leaving 806 cases for the analyses described below.
Table 1.
Characteristics of participating clinicians randomized to the intervention and comparison groups.
| Total (n=31) |
Comparison (n=15) |
Intervention (n=16) |
P | |
|---|---|---|---|---|
| Female (%) | 48 | 47 | 50 | 0.85 |
| Agea, mean (SD) | 47.0 (9.9) | 47.3 (8.0) | 46.6 (11.7) | 0.85 |
| Race, white (%) | 87 | 87 | 88 | 1.00b |
| Training (%) | 0.51b | |||
| Internal Medicine | 23 | 20 | 25 | |
| Family Medicine | 71 | 80 | 63 | |
| Nurse Practitioner | 6 | 0 | 13 | |
| Safety net practice (%) | 65 | 67 | 63 | 0.81 |
| Years since residency completeda, mean (SD) | 15.4 (9.0) | 17.1 (8.1) | 13.7 (9.8) | 0.32 |
| Patient care days per weeka, mean (SD) | 4.1 (1.1) | 4.0 (1.1) | 4.1 (1.0) | 0.75 |
| Spanish-speaking (%) | 19 | 20 | 19 | 1.00b |
Note: Content of table reproduced with permission (BioMed Central Open Access license); originally published by BioMed Central in Flocke et al. BMC Health Services Research 2012, 12:109.
Data updated from originally published version: age reported; standard deviations reported; additional data collection conducted to replace missing values for years since residency.
P-values updated from originally published version: Fisher exact test p-value is reported.
Table 2 shows patient participant demographics and visit characteristics for the baseline and post-training cohorts of both the intervention and comparison groups. Patients seen by intervention clinicians at baseline were not significantly different from those seen by clinicians in the comparison group at baseline, with the exception that patients in the comparison group were more likely to report a diagnosis of hypertension. In the post-training enrollment period, patient cohorts were also largely similar, although patients seen by a clinician in the intervention group were more likely to be Hispanic and to report the clinician was their regular doctor. Average visit duration with an intervention clinician was 2.1 minutes longer than with a comparison group clinician at baseline (p=0.03) and 3.2 minutes longer in the post-training period (p<0.001).
Table 2.
Intervention and comparison group patient participant characteristics and visit context by enrollment period.
| Baseline Period | Post-Training Period | |||||
|---|---|---|---|---|---|---|
| Comparison (n=193) |
Intervention (n=200) |
P | Comparison (n=206) |
Intervention (n=207) |
P | |
| Patient Characteristics | ||||||
| Age, mean (SD) | 44.9 (12.8) | 44.5 (12.8) | 0.76 | 45.0 (13.4) | 44.3 (12.5) | 0.59 |
| Female (%) | 63 | 58 | 0.29 | 65 | 59 | 0.24 |
| Hispanic (%) | 7 | 9 | 0.39 | 8 | 14 | 0.03 |
| Race (%) | 0.09 | 0.14 | ||||
| White | 55 | 65 | 54 | 57 | ||
| Black / African-American | 40 | 30 | 39 | 31 | ||
| Other / more than one | 5 | 6 | 8 | 12 | ||
| Education (%) | 0.19 | 0.05 | ||||
| Less than high school graduate | 14 | 22 | 22 | 27 | ||
| High school graduate or GED | 38 | 34 | 41 | 28 | ||
| Some college | 33 | 33 | 26 | 31 | ||
| College graduate | 16 | 12 | 11 | 15 | ||
| Self-reported health status (%) | 0.86 | 0.78 | ||||
| Excellent | 5 | 7 | 6 | 6 | ||
| Very good | 16 | 16 | 15 | 13 | ||
| Good | 34 | 34 | 29 | 33 | ||
| Fair | 32 | 29 | 28 | 30 | ||
| Poor | 14 | 16 | 21 | 18 | ||
| Chronic conditions (%) | ||||||
| Diabetes | 17 | 13 | 0.32 | 17 | 18 | 0.81 |
| High Cholesterol | 30 | 29 | 0.74 | 25 | 28 | 0.45 |
| Hypertension | 44 | 32 | 0.01 | 36 | 37 | 0.79 |
| Heart Disease | 8 | 7 | 0.50 | 7 | 9 | 0.48 |
| None of the above | 40 | 49 | 0.09 | 54 | 51 | 0.46 |
| Cigarettes smoked per daya, median (IQR) | 10 (10) | 10 (14) | 0.01 | 10 (15) | 10 (13) | 0.66 |
|
| ||||||
| Visit Context | ||||||
| Seeing regular clinician (%) | 82 | 83 | 0.70 | 74 | 84 | 0.02 |
| Reason for visit (%) | 0.64 | 0.54 | ||||
| New illness or problem | 26 | 22 | 28 | 28 | ||
| Continued care | 41 | 47 | 45 | 47 | ||
| Well care, physical | 26 | 26 | 24 | 21 | ||
| Other | 7 | 7 | 2 | 5 | ||
| Duration of visit (min)b, mean (SD) | 18.9 (8.8) | 21.0 (10.0) | 0.03 | 17.3 (7.8) | 20.5 (8.6) | <0.001 |
| Visit included discussion of smokingb (%) | 65 | 66 | 0.96 | 70 | 88 | <0.001 |
| Patient’s level of readiness to quitbc (%) | 0.77 | 0.74 | ||||
| Not ready | 16 | 13 | 14 | 16 | ||
| Ambivalent | 36 | 34 | 41 | 43 | ||
| Ready | 48 | 53 | 45 | 40 | ||
One small cigar considered equivalent to three cigarettes.
Derived from audio recording of visit.
Only includes cases with discussion of smoking during the visit; cases where patient’s level of readiness was Unclear/Unknown are excluded from the denominator.
With regard to the smoking-related variables, patients in the intervention and comparison groups expressed similar readiness to quit smoking in both the baseline and post-training cohorts. While smoking was discussed at similar rates in the intervention and comparison groups at baseline, in the post-training period, a significantly larger proportion of visits with clinicians in the intervention group contained some discussion of smoking (88% vs. 70%, p<0.001).
Of the 806 cases analyzed, 583 (72%) overall contained some talk of smoking and were thus able to be analyzed for the presence of specific TMCP elements. Table 3 summarizes the performance of the TMCP elements for clinicians in the intervention and comparison groups at baseline and post-training. As anticipated, intervention and comparison clinicians performed TMCP elements at similar rates at baseline, and the general rate of performance was low. In the post-training period, clinicians in the intervention group performed nearly all of the TMCP elements at significantly higher rates than comparison group. For example, clinicians who had received the TMCP training intervention for smoking cessation used the TMCP brief advice elements of expressing concern, optimism, and partnership 3 to 12 times as often as comparison group clinicians. Clinicians who received the intervention were more likely to elicit level of readiness to quit from patients, when compared to comparison group clinicians in the post-training period (84% vs. 65%, p=0.006). Overall, clinicians in the intervention group were more likely to provide smoking cessation advice in a way that aligned with the patient’s level of readiness to quit smoking, as indicated by their responding in alignment scores. However, intervention clinicians’ performance was only significantly better than comparison clinicians’ performance when patients’ expressed level of readiness was “ambivalent” (p=0.007) or “ready” (p=0.001) to quit. After training, intervention clinicians’ average smoking discussion was 1.4 minutes longer than that of comparison clinicians (p=0.01), and the proportion of the total visit spent discussing smoking was greater (18% vs. 13%, p=0.01).
Table 3.
Rates of TMCP elements during visits with smoking discussion in intervention and comparison groups by enrollment period.
| Baseline Period | Post-Training Period | |||||||
|---|---|---|---|---|---|---|---|---|
| Comparison (n=126) |
Intervention (n=131) |
Pd | ES (95% CI)e | Comparison (n=144) |
Intervention (n=182) |
Pd | ES (95% CI)e | |
| Link smoking to salient concern (%) | 39 | 39 | 0.99 | 0.00 (−0.12,0.12) | 44 | 58 | 0.01 | 0.14 (0.04,0.25) |
| Brief advice elements (%) | ||||||||
| Quit statement | 33 | 34 | 0.83 | 0.02 (−0.10,0.14) | 38 | 44 | 0.50 | 0.06 (−0.05,0.17) |
| Concern | 2 | 1 | 0.40 | −0.07 (−0.19,0.06) | 2 | 18 | 0.007 | 0.25 (0.14,0.36) |
| Optimism | 2 | 6 | 0.18 | 0.09 (−0.03,0.21) | 3 | 36 | <0.001 | 0.41 (0.30,0.51) |
| Partnership | 10 | 9 | 0.94 | −0.01 (−0.13,0.12) | 12 | 40 | 0.003 | 0.31 (0.21,0.42) |
| Engage patienta | 20 | 15 | 0.51 | −0.06 (−0.21,0.09) | 22 | 51 | 0.005 | 0.30 (0.17,0.44) |
| Elicit level of readiness to quitb (%) | 63 | 68 | 0.64 | 0.05 (−0.08,0.17) | 65 | 84 | 0.006 | 0.21 (0.10,0.32) |
| Responding in Alignment scorebc, mean (SD) | 4.6 (1.9) | 4.2 (2.0) | 0.36 | −0.17 (−0.47,0.14) | 4.1 (1.8) | 5.3 (2.2) | <0.001 | 0.57 (0.31,0.82) |
| Not ready | 5.5 (1.3) | 5.2 (1.4) | 0.56 | −0.24 (−1.06,0.58) | 6.0 (1.3) | 6.6 (1.9) | 0.32 | 0.33 (−0.33,0.99) |
| Ambivalent | 3.0 (1.2) | 2.7 (1.4) | 0.38 | −0.27 (−0.79,0.25) | 3.0 (1.4) | 4.0 (1.7) | 0.007 | 0.63 (0.23,1.02) |
| Ready | 5.4 (1.8) | 5.0 (1.9) | 0.31 | −0.22 (−0.66,0.21) | 4.6 (1.6) | 6.2 (2.0) | 0.001 | 0.85 (0.44,1.25) |
|
| ||||||||
| Duration of smoking discussion (min), mean (SD) | 2.5 (2.6) | 2.3 (2.1) | 0.68 | −0.10 (−0.35,0.15) | 2.2 (2.0) | 3.6 (2.7) | 0.01 | 0.58 (0.36,0.80) |
| Not ready | 2.1 (1.9) | 2.6 (2.1) | 0.61 | 0.26 (−0.56,1.08) | 1.3 (0.9) | 2.5 (1.7) | 0.01 | 0.81 (0.13,1.49) |
| Ambivalent | 4.0 (3.8) | 2.4 (1.8) | 0.19 | −0.53 (−1.06,0.00) | 3.6 (2.7) | 4.2 (2.9) | 0.52 | 0.22 (−0.17,0.60) |
| Ready | 3.1 (2.0) | 3.2 (2.5) | 0.84 | 0.05 (−0.39,0.48) | 2.3 (1.5) | 4.3 (2.6) | 0.002 | 0.88 (0.47,1.29) |
| Unclear/Unknown | 1.2 (1.1) | 1.0 (1.2) | 0.49 | −0.15 (−0.58,0.27) | 1.3 (1.2) | 1.9 (1.8) | 0.31 | 0.39 (−0.06,0.84) |
| Proportion of visit discussing smoking, mean (SD) | 0.12 (0.11) | 0.11 (0.11) | 0.64 | −0.11 (−0.35,0.14) | 0.13 (0.11) | 0.18 (0.13) | 0.01 | 0.45 (0.23,0.67) |
Visits where patients provided their readiness level are excluded from the denominator.
Responding in Alignment score not computed for visits where patient’s level of readiness was not elicited (i.e. where Unclear/Unknown).
Scores standardized so that possible range for any level of readiness is 0–10.
P-values adjusted for the clustering of multiple patient-level observations for each clinician.
Effect sizes computed using Phi for categorical variables and Cohen’s d for continuous variables.
The uptake of each of the TMCP elements among the intervention group clinicians varied widely, ranging from 30% to 77% for linking to a salient concern, 0% to 100% for providing a quit statement, 0% to 87% for expression of concern and optimism, and 0–79% for partnership (data not shown). Excluding the intervention group clinicians completed the TMCP training one-on-one with a TMCP instructor did not change the range of uptake of the TMCP elements.
Discussion
Effective patient-clinician communication about modifiable health behaviors, such as smoking, is an important strategy for promoting health and preventing disease. While research has shown that brief advice from a clinician increases the likelihood of quit attempts and smoking cessation (Gorin and Heck, 2004; Katz et al., 2004; Stead et al., 2013), this has not translated into improved uptake of counseling in the primary care setting. The TMCP model provides clinicians with a brief approach for both delivering health behavior change advice that is patient-centered and navigating patient resistance to change, that can be realistically translated into busy primary care practices. The TMCP intervention significantly influenced the clinicians’ approaches to communication about smoking. Specifically, this study showed that TMCP training significantly increased clinician rates of linking smoking to a patient’s salient concern, expressing optimism and partnership, and eliciting the patient’s current readiness to engage in a quit attempt. The approach appears feasible for use in real world clinical settings. We hypothesized that the TMCP approach would increase the time efficiency of counseling, however, we found this was not the case. Use of the TMCP was associated with an increase in time spent discussing smoking during the visit. This may be due to greater patient engagement in discussion of readiness to change and greater discussion of potential next steps for those patients who expressed ambivalence about quitting smoking among those using the TMCP approach.
Clinician’s use of specific TMCP elements varied. For example, TMCP-trained clinicians made a link between smoking and a concern salient to the patient in 58% of discussions, while only 18% of discussions included an expression of concern about the patient’s smoking. The lower implementation rates on some of these elements could reflect insufficient emphasis during training, clinician adaptation of the TMCP (e.g., focusing on elements that were least divergent from their current approaches), or other practice/system constraints (e.g., work flow of documentation required by the electronic health record). Each of these is worth further exploration and could inform future work to refine the TMCP training and implementation. Nonetheless, the relatively brief, communication-focused training resulted in large and meaningful change in the communication behavior of clinicians in actual practice with patients.
It is also worth noting that, while all of the clinicians in the intervention group demonstrated the skills to deploy the TMCP with standardized patients in the training facility, the degree to which they used the TMCP skills with their own patients varied dramatically. The highest performing clinician implemented the majority of TMCP behaviors in over 85% of smoking cessation discussions. However, implementation was poor among several clinicians with rates averaging below 40% and one clinician failing to implement any key elements. Perhaps some clinician participants were unconvinced that the TMCP would help overcome perceived barriers such as inadequate time and patient motivation to change (Association of American Medical Colleges, 2007). Additional training in the form of “booster” sessions or additional coaching could potentially offer supplemental support for these clinicians to use the TMCP. It also may be the case that some features of a practice setting can support or hinder clinicians’ use of the TMCP. A recent review of strategies to increase smoking cessation treatment in primary care (Papadakis et al., 2010) suggests that multi-component interventions (e.g., clinician training combined with practice-level interventions such as electronic health record reminders) hold the most promise for affecting both clinician and patient behavior leading to smoking cessation. Further, the TMCP approach could be integrated with supports to easily connect patients with additional resources for cessation, such as tobacco quit lines (Cummins et al., 2007; Vidrine et al., 2013a, 2013b) or other forms of electronic cessation assistance (Chen et al., 2012).
Strengths and limitations
This study’s strengths lie in the careful design of the intervention to teach several specific communication skills grounded in observation and supported by communication theory and health behavior change research. Further, the study’s group randomized design along with audio recording and systematic coding of clinician smoking discussions allowed for a rigorous evaluation of change in clinician behavior. This is particularly important because changing clinical practice can be difficult. Use of audio-recordings of actual patient visits reduces biases that may be present in patient reports and medical record review and allows behavior change counseling fidelity to be assessed directly, providing an accurate measure of clinician competence when adhering to a specific approach like the TMCP. Additional strengths of the current study include a large, diverse patient sample and the representation of multiple health care systems, including federally-qualified health centers, within the clinician sample.
A few limitations to the study also deserve mention. First, one clinician dropped out of the study after randomization. The reason for dropout was due to time limitations and not the focus of the intervention, so this is unlikely to bias the findings. Second, the period of post-intervention evaluation was relatively short, thus the extent of clinicians’ sustained use of the TMCP approach is unknown. Third, during recruitment the study was described as focusing on doctor-patient communication about health behaviors, and while the study recruitment process was purposeful in not sharing the topic area of smoking cessation during recruitment, clinicians who agreed to participate may have been more inclined to emphasize communication skills or health promotion as part of their practice or professional development than clinicians in the general population. However, significant efforts were made to reduce any potential Hawthorne effect bias: neither the focus on smoking nor the particulars of the communication approach were shared during baseline data collection or with the comparison group post-intervention until completion of data collection.
Conclusion
Informed by multiple frameworks and current guidelines, the TMCP is intended to enhance clinician communication skills for creating tailored and partnership-oriented health behavior change discussions during routine visits. The TMCP training intervention significantly changed the content of clinicians’ smoking cessation communication in ways consistent with the TMCP model for health behavior change. The TMCP approach is feasible in real world settings, and thus represents a potentially powerful tool for clinicians to prompt patient behavior change.
Supplementary Material
Highlights.
The Teachable Moment Communication Process (TMCP) is a brief counseling approach for primary care.
We evaluated the impact of TMCP training on clinicians’ smoking cessation counseling.
Smoking cessation counseling changed in ways consistent with the TMCP approach after training.
The TMCP is feasible in primary care settings.
Acknowledgments
The authors thank all clinician and patient participants who made this study possible. This project was funded by a grant to Susan Flocke, R01 CA 105292, and was also supported by the Behavioral Measurement Core and the Practice Based Research Network Core of the Case Comprehensive Cancer Center (P30 CA43703).
We also wish to acknowledge the hard work and dedication of the study coordinators, analysts, and field data collection team: Mary Jane Mason, Marcia Moreno, Julie Gardner, Michelle Fakler, Erin Hanahan, Jelena Pokimica, Emmanuelle Noar, Jenny Shin, Shilp Shah, Vanessa Clemens, and Katherine Kleinberg.
FINANCIAL SUPPORT: NIH/NCI, R01 CA 105292 (PI: Flocke)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
TRIAL REGISTRATION: ClinicalTrials.gov, NCT01575886, Enhancing Teachable Moment Communication for Smoking Cessation and Weight Management
Conflict of interest statement
The authors report no current or prior conflicts of interest. No financial disclosures were reported by the authors of this paper.
References
- Association of American Medical Colleges. Physician Behavior and Practice Patterns Related to Smoking Cessation, Workforce. Washington DC: 2007. [Google Scholar]
- Butler CC, Rollnick S, Cohen D, Bachmann M, Russell I, Stott N. Motivational consulting versus brief advice for smokers in general practice: a randomized trial. Br J Gen Pract. 1999;49:611–616. [Google Scholar]
- Carroll JK, Antognoli E, Flocke SA. Evaluation of physical activity counseling in primary care using direct observation of the 5As. Ann Fam Med. 2011;9:416–22. doi: 10.1370/afm.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Current Cigarette Smoking Among Adults — United States, 2011. MMWR. 2012a;61:889–907. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Health Interview Survey, 2011 Data Release [WWW Document] 2012b URL ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHIS/2011/samadult.zip (accessed 11.5.12)
- Chen YF, Madan J, Welton N, Yahaya I, Aveyard P, Bauld L, Wang D, Fry-Smith A, Munafò MR. Effectiveness and cost-effectiveness of computer and other electronic aids for smoking cessation: a systematic review and network meta-analysis. Health Technol Assess (Rockv) 2012;16:1–205. iii–v. doi: 10.3310/hta16380. [DOI] [PubMed] [Google Scholar]
- Cohen DJ, Clark EC, Lawson PJ, Casucci BA, Flocke SA. Identifying teachable moments for health behavior counseling in primary care. Patient Educ Couns. 2011;85:e8–15. doi: 10.1016/j.pec.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman T, Wilson A. Anti-smoking advice from general practitioners: is a population-based approach to advice-giving feasible? Br J Gen Pract. 2000;50:1001–1004. [PMC free article] [PubMed] [Google Scholar]
- Cummins SE, Bailey L, Campbell S, Koon-Kirby C, Zhu SH. Tobacco cessation quitlines in North America: a descriptive study. Tob Control. 2007;16:i9–i15. doi: 10.1136/tc.2007.020370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmons K, Rollnick S. Motivational interviewing in health care settings: Opportunities and limitations. Am J Prev Med. 2001;20:68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB. Clinical Practice Guideline. US Department of Health and Human Services. Public Health Service; Rockville, MD: 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- Flocke SA, Antognoli E, Step MM, Marsh S, Parran T, Mason MJ. A teachable moment communication process for smoking cessation talk: description of a group randomized clinician-focused intervention. BMC Health Serv Res. 2012;12:109. doi: 10.1186/1472-6963-12-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin SS, Heck JE. Meta-Analysis of the Efficacy of Tobacco Counseling by Health Care Providers. Cancer Epidemiol Biomarkers Prev. 2004;13:2012–2022. [PubMed] [Google Scholar]
- Harris PA, Ph D, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research Electronic Data Capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010.Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annu Rev Clin Psychol. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Kang M, Ragan BG, Park JH. Issues in outcomes research: an overview of randomization techniques for clinical trials. J Athl Train. 2008;43:215–21. doi: 10.4085/1062-6050-43.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz DA, Muehlenbruch DR, Brown RL, Fiore MC, Baker TB. Effectiveness of implementing the agency for healthcare research and quality smoking cessation clinical practice guideline: a randomized, controlled trial. J Natl Cancer Inst. 2004;96:594–603. doi: 10.1093/jnci/djh103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krippendorff K. Bivariate agreement coefficients for reliability data. Sociological Methodology. 1970:139–150. [Google Scholar]
- Krippendorff K. Reliability in Content Analysis. Hum Commun Res. 2004;30:411–433. doi: 10.1111/j.1468-2958.2004.tb00738.x. [DOI] [Google Scholar]
- Lai DT, Cahill K, Qin Y, Tang JL. Motivational interviewing for smoking cessation. Cochrane Database Syst Rev. 2010;10 doi: 10.1002/14651858.CD006936.pub2. [DOI] [PubMed] [Google Scholar]
- Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns. 2009;76:25–30. doi: 10.1016/j.pec.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride CM, Emmons KM, Lipkus IM. Understanding the potential of teachable moments: the case of smoking cessation. Health Educ Res. 2003;18:156–70. doi: 10.1093/her/18.2.156. [DOI] [PubMed] [Google Scholar]
- McBride CM, Puleo E, Pollak KI, Clipp EC, Woolford S, Emmons KM. Understanding the role of cancer worry in creating a “teachable moment” for multiple risk factor reduction. Soc Sci Med. 2008;66:790–800. doi: 10.1016/j.socscimed.2007.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. J Am Med Assoc. 2004;291:1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Papadakis S, McDonald P, Mullen KA, Reid R, Skulsky K, Pipe A. Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Prev Med (Baltim) 2010;51:199–213. doi: 10.1016/j.ypmed.2010.06.007. [DOI] [PubMed] [Google Scholar]
- Pilnick A, Coleman T. “I’ll give up smoking when you get me better” patients’ resistance to attempts to problematise smoking in general practice (GP) consultations. Soc Sci Med. 2003;57:135–45. doi: 10.1016/s0277-9536(02)00336-2. [DOI] [PubMed] [Google Scholar]
- Rubak S, Sandbaek A, Lauritzen T, Christensen B. Motivational interviewing: a systematic review and meta-analysis. Br J Gen Pract. 2005;55:305–312. [PMC free article] [PubMed] [Google Scholar]
- Soria R, Legido A, Escolano C, López Yeste A, Montoya J. A randomised controlled trial of motivational interviewing for smoking cessation. Br J Gen Pract. 2006;56:768–74. [PMC free article] [PubMed] [Google Scholar]
- Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation (Review) Cochrane Database Syst Rev. 2013 doi: 10.1002/14651858.CD000165.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stead M, Angus K, Holme I, Cohen D, Tait G. Factors influencing European GPs’ engagement in smoking cessation: a multi-country literature review. Br J Gen Pract. 2009;59:682–90. doi: 10.3399/bjgp09X454007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service report. JAMA. 2000;283:3244–54. [PubMed] [Google Scholar]
- Thorndike AN, Regan S, Rigotti Na. The treatment of smoking by US physicians during ambulatory visits: 1994–2003. Am J Public Health. 2007;97:1878–83. doi: 10.2105/AJPH.2006.092577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong EK, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of U.S. health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12:724–33. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Vital Signs: Current Cigarette Smoking Among Adults Aged ≥18 Years — United States, 2005–2010. MMWR. 2011;60:1207–12. [PubMed] [Google Scholar]
- VanBuskirk Ka, Wetherell JL. Motivational interviewing with primary care populations: a systematic review and meta-analysis. J Behav Med. 2014;37:768–80. doi: 10.1007/s10865-013-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Shete S, Cao Y, Greisinger A, Harmonson P, Sharp B, Miles L, Zbikowski SM, Wetter DW. Ask-Advise-Connect A New Approach to Smoking Treatment Delivery in Health Care Settings. JAMA Intern Med. 2013a;173:458–64. doi: 10.1001/jamainternmed.2013.3751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidrine JI, Shete S, Li Y, Cao Y, Alford MH, Galindo-Talton M, Rabius V, Sharp B, Harmonson P, Zbikowski SM, Miles L, Wetter DW. The ask-advise-connect approach for smokers in a safety net healthcare system: a group-randomized trial. Am J Prev Med. 2013b;45:737–41. doi: 10.1016/j.amepre.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner JJ, Lawson PJ, Panaite V, Step MM, Flocke SA. Comparing Primary Care Physicians’ Smoking Cessation Counseling Techniques to Motivational Interviewing. J Addict Med. 2013;7:139–142. doi: 10.1097/ADM.0b013e3182879cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


