Abstract
A 45-year-old man was diagnosed with a 3 mm × 3 mm iris cyst located at 9 o’clock behind iris and protruding into temporal angle by slit lamp examination, gonioscopy, and ultrasound biomicroscopy (UBM). Phase-sensitive optical coherence tomography (PhS-OCT) was applied on this case for the quantitative measurements of trabecular meshwork (TM) motion. The frequency of TM motion was with the same rhythm of the patient’s peripheral pulse. Its amplitude on the closed angle region showed significant smaller than the open angle region. PhS-OCT can be a useful tool for the diagnosis and follow-up in ocular diseases surrounding iridocorneal angle.
Keywords: Trabecular meshwork (TM), iris cyst, phase-sensitive optical coherence tomography (PhS-OCT)
A 45-year-old man was noted with an iris lesion in his right eye during the regular eye exam in March 2013. Slit lamp examination revealed a 3 mm × 3 mm bulging mass located at 9 o’clock behind iris and protruding into temporal angle (Figure 1). There was no ectropion uvea or corectopia. Gonioscopy showed temporal iris bulging and obscuring the view of angle approximately 1.5 clock hours. Ciliary body was normal in size and structure. Ultrasound biomicroscopy (UBM) revealed a cystic lesion at 9 o’clock causing anterior bulging of iris (Figure 2). No associated solid mass was noted. All of other eye examinations were within normal limits, including the vision, intraocular pressure, cornea, lens, and posterior segment. Nothing particular was found in the last eye checkup one and a half year ago. No trauma history was reported between these two eye checkups. Unilateral primary iris cyst was diagnosed clinically. Phase-sensitive optical coherence tomography (PhS-OCT) (1) was then used to measure the trabecular meshwork (TM) motion near the iris lesion with closed angle. The setting, data acquisition and processing of PhS-OCT have been previously described (2). Quantitative measurements of the TM motion were clearly visible between the closed angle region and the open angle region of the same eye (Figure 3).
Figure 1.
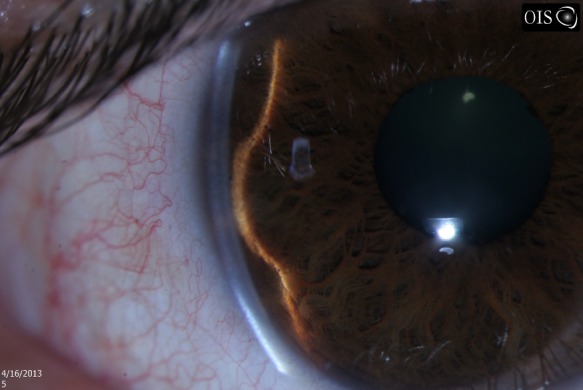
Slit lamp exam photo, right eye. A 3 mm × 3 mm temporal bulging mass appears to be originating from posterior iris causing anterior bowing of the iris.
Figure 2.
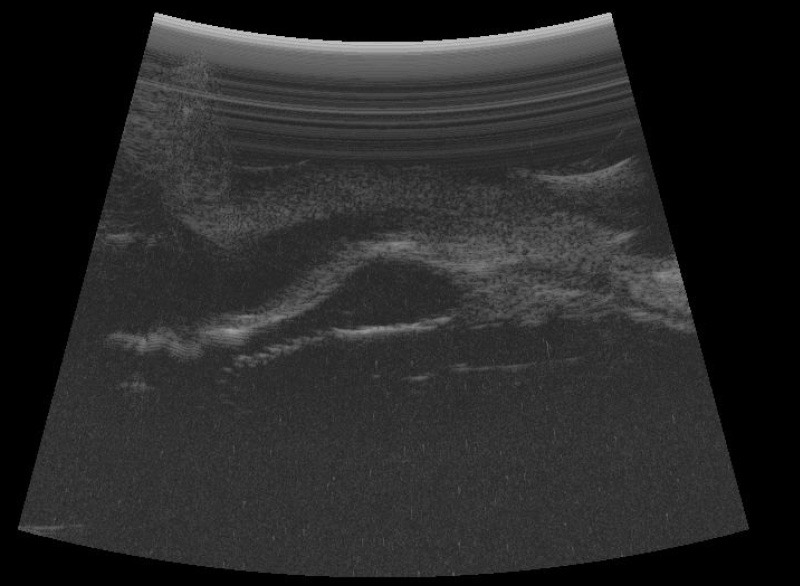
Ultrasound biomicroscopy (UBM) of the anterior chamber shows a 3 mm × 3 mm round, sonolucent lesion occupying the anterior chamber.
Figure 3.
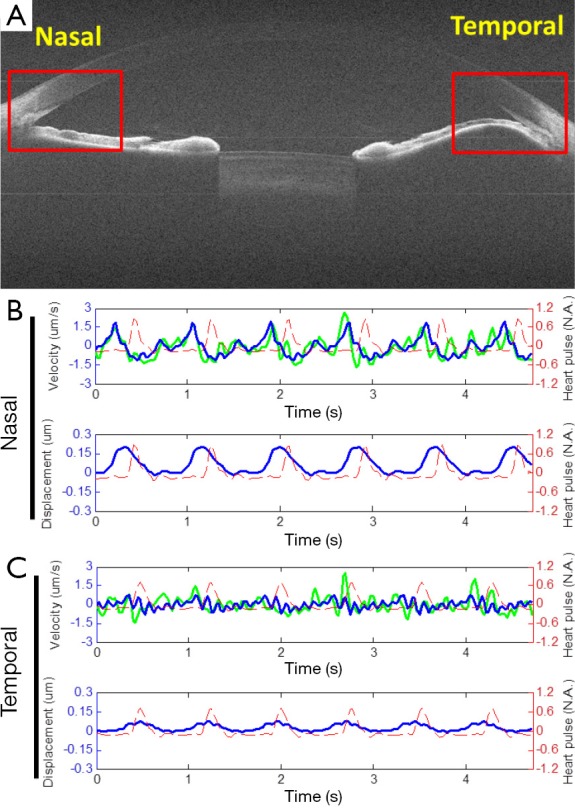
Phase-sensitive optical coherence tomography (PhS-OCT) assessment of dynamic motion of TM in vivo. (A) OCT cross-sectional imaging (size =12 mm × 10 mm). Dynamic motion of TM in (B) nasal and (C) temporal regions, where the frequency of TM motion is with the same rhythm of the patient’s peripheral pulse. Its amplitude on the closed angle region shows significant smaller than the open angle region. TM, trabecular meshwork.
Iris cyst is usually a silent pathological finding unless it causes some inflammatory reaction in the anterior chamber or blocks the aqueous outflow resulting in subsequent glaucoma. It can be classified as primary and secondary iris cyst according to its etiology. Primary iris cyst is the one without recognizable etiology and usually involving the posterior pigment epithelium of the iris. Secondary iris cyst always has a recognizable etiology, such as penetrating trauma, surgery, metastasis, or chronic use of miotics. Iris cyst is difficult to detect because of its hidden location. Slit-lamp examination, gonioscopy, UBM, and anterior segment optical coherence tomography (AS-OCT) are all the means that can be used to detect the lesions around anterior segment of the eye. Slit-lamp examination can clearly visualize the iris lesion located in front of the iris. Gonioscopy is used to evaluate the lesion located at the angle. Until early 1990s (3,4), UBM was introduced for the evaluation of anterior segment and especially the part behind the iris. Patients are examined in the supine position with the eye immersed in saline solution by using an eyecup. After the report of Izatt et al. in 1994 (5), AS-OCT becomes a more popular imaging system which is noninvasive and able to image the patient with an upright position (6,7). PhS-OCT first reported by Wang et al. in 2007 (1) was then utilized to image the anterior segment in the eye (2), that permits in vivo characterization of TM tissue movement with a nanometer level of sensitivity. It is found the relationship between pulsatile TM tissue motion and cardiac pulse. In this case, we could see the frequency of TM motion is with the same rhythm of the patient’s peripheral pulse. Its amplitude on the closed angle region shows significant smaller than the open angle region (Figure 3). PhS-OCT can be a very useful tool for the diagnosis and follow-up of many ocular diseases surrounding iridocorneal angle.
Acknowledgments
Disclosure: The authors declare no conflict of interest.
References
- 1.Wang RK, Kirkpatrick S, Hinds M. Phase sensitive optical coherence elastography for mapping tissue micro-strains in real time. Appl Phys Lett 2007;90:164105. [Google Scholar]
- 2.Li P, Shen TT, Johnstone M, Wang RK. Pulsatile motion of the trabecular meshwork in healthy human subjects quantified by phase-sensitive optical coherence tomography. Biomed Opt Express 2013;4:2051-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pavlin CJ, Sherar MD, Foster FS. Subsurface ultrasound microscopic imaging of the intact eye. Ophthalmology 1990;97:244-50. [DOI] [PubMed] [Google Scholar]
- 4.Pavlin CJ, Harasiewicz K, Sherar MD, Foster FS. Clinical use of ultrasound biomicroscopy. Ophthalmology 1991;98:287-95. [DOI] [PubMed] [Google Scholar]
- 5.Izatt JA, Hee MR, Swanson EA, Lin CP, Huang D, Schuman JS, Puliafito CA, Fujimoto JG. Micrometer-scale resolution imaging of the anterior eye in vivo with optical coherence tomography. Arch Ophthalmol 1994;112:1584-9. [DOI] [PubMed] [Google Scholar]
- 6.Li P, An L, Lan G, Johnstone M, Malchow D, Wang RK. Extended imaging depth to 12 mm for 1050-nm spectral domain optical coherence tomography for imaging the whole anterior segment of the human eye at 120-kHz A-scan rate. J Biomed Opt 2013;18:16012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li P, Johnstone M, Wang RK. Full anterior segment biometry with extended imaging range spectral domain optical coherence tomography at 1340 nm. J Biomed Opt 2014;19:046013. [DOI] [PMC free article] [PubMed] [Google Scholar]


