Abstract
Forward reaching is an integral part of many essential daily activities. It is often performed while standing quietly or after standing up from a seated position. This study sought to determine how a preceding balance task and aging would affect the task performance and movement strategy. Twenty-two healthy young and 20 older adults participated in this study and performed forward reaching under two task conditions. In forward reach (FR), reaching was performed during quiet standing. In up-and-reach (UR), subjects stood up from a seated position and then reached forward. A motion analysis system was used to calculate the location of the center of mass (COM) and joint angles at the initial and final positions, and the finger, COM, and joint angular displacements during the reaching task. For both groups, UR was initiated in a more flexed posture and had a significantly shorter reach distance and greater ankle dorsiflexion angle, compared to FR. The location of the COM, however, did not differ between the two task conditions. Older adults were found to significantly slow down their downward and forward COM motions in UR but not young adults. These findings showed that a preceding balance task increased the task demand and required modifications in the movement strategy. For older adults, the impact of increased task demand was greater, and adopting a cautious strategy could help to complete the task safely.
Keywords: Standing balance, Movement strategies, Center of mass, Kinematics
Introduction
The ability to perform activities of daily living is critical for independent living and associated with health, quality of life, and mortality in older adults (Agmon et al. 2014; Manton 1988; Tran et al. 2013). How best to improve or regain this ability is one of the primary goals of rehabilitation. The understanding of the risks and strategies that associated the performance of daily activities in healthy older adults can help clinicians better advise or develop intervention protocols for their older clients.
Among the daily activities commonly affected in old age, reaching is particularly noteworthy. It is an integral part of many essential daily activities, such as cooking, shopping, and housework. Limitations in reaching could occur early in older adults and can predict future disability. They are also among the most recognized functional losses for older adults, only second to walking (Kaut et al. 2011; Seidel et al. 2011). The problem can be caused by impaired ability in performing guided upper limb motion and/or moving the body’s center of mass (COM) toward the target. Specifically, when reaching is performed in standing, it is the latter that is believed to be the primary restricting factor (Pozzo et al. 2002; Row and Cavanagh 2007; Wallmann 2001).
The task of reaching forward is widely used clinically and in research to measure balance ability. Limitation in reaching forward, reflected by a shorter reach distance, is well accepted to indicate poorer balance and has been found to be associated with aging, as well as impaired sensorimotor functions, such as caused by stroke, vestibular dysfunctions, diabetes neuropathy, or Parkinson’s disease (Behrman et al. 2002; Brusse et al. 2005; Intiso et al. 2012; Lin et al. 2010; Mann et al. 1996; Smith et al. 2004). On the contrary, a longer reach distance is indicative of better balance and has been found to be associated with better functional ability and reduced risk of falling in older adults (Chase et al. 2012; Duncan et al. 1990; Lam et al. 2012; Wallmann 2001; Weiner et al. 1992).
Another indicator of balance ability involving reaching forward is movement strategies. While healthy young adults often adopt an ankle strategy for reaching forward, older adults, patients with vestibular loss, and healthy young adults with experimentally induced somatosensory loss of the lower legs have been found to prefer a hip strategy (Camicioli et al. 1997; Horak et al. 1990; Horak et al. 1994; Lin and Yang 2011). A hip strategy could restrict the forward leaning of the body by bending at the hips and moving the COM backward and subsequently reduce the plantarflexing torque required to counteract the torque associated with forward leaning of the body. Thus, although adopting a hip strategy could be an indication of limited balance ability, it is also a compensatory strategy to reduce the risk of loss of balance and has been recommended to be included in balance training (Martin et al. 2013).
In addition to adopting different movement strategies, older adults have also been found to simply avoid tasks that would increase the risk of loss of balance. When instructed to reach forward as fast as possible while standing at the edge of an elevated surface, older adults did not actually increase their reaching speeds, while young adults significantly increased their reaching speeds and resulted in more frequent loss of balance (Kozak et al. 2003). These findings suggest that for older adults, there are multiple ways to overcome their physiological constraints, and different task demands may require different solutions.
The performance and movement strategies for reaching forward while standing quietly have been widely studied and fairly well understood. However, reaching is frequently executed immediately after standing up from a seated position. How such a preceding balance task would affect reach performance and how individuals, especially older adults, modify their behaviors to meet the task demand are unclear. The purpose of this study was to investigate the performance and movement strategies of reaching forward during quiet standing and immediately after standing up in young and older adults. It was hypothesized that the task of reaching immediately after standing up would be more challenging and result in shorter reach distance. It was further hypothesized that for older adults, greater modifications in the movement strategies would be adopted in the up-and-reach task in order to reduce balance threats and improve safety.
Methods
Subjects
Twenty-two young (12 males and 10 females) and 20 older (10 males and 10 females) adults participated in this study. Healthy young adults were recruited from a university campus. Community-dwelling older adults who were over 65 years old and independent in standing and walking were recruited. None of the subjects had histories of neuromuscular or musculoskeletal disorders, pain, or other medical conditions that could affect the performance of the tasks. This study was approved by the Institutional Review Board of the National Cheng Kung University Hospital. All the subjects gave their informed consents.
Sensorimotor evaluation
The sensorimotor function of both sides was measured, and their means were used for data analysis. The plantar touch-pressure (cutaneous) sensitivity was assessed using the Semmes-Weinstein monofilaments (Patterson Company, IL, USA). Filament markings of 2.83, 3.61, 4.31, and 6.65 were used to classify the level of plantar sensitivity into 1, 2, 3, and 4, respectively. A grade of 5 was given when the subject was unable to correctly sense the 6.65 filament. The filament was applied perpendicularly and slowly to the test site for 1.5 s until the filament bowed, and the subject was asked to indicate if the pressure was felt. The smallest filament that the subject was able to perceive indicated the touch-pressure sensitivity. Subjects were tested in the supine position with the eyes closed to eliminate visual cues. A total of ten sites for the plantar sides of both feet were assessed, including distal phalange of the hallux, metatarsal head of the third and fifth toes, the midpoint of the lateral border of the foot, and the center of the heel.
The handgrip strength was assessed using a calibrated JAMAR hand dynamometer (Sammons Preston Rolyan, IL, USA). Subjects seated with the dominant arm by the side and in neutral rotation, elbow in 90° flexion, and forearm in neutral position, and then exerted maximum volitional contraction for 3 s. The maximal isometric strength of the hip flexors, knee flexors, knee extensors, ankle dorsiflexors, and big toe flexors were measured using a handheld dynamometer (MicroFET2, HOGGAN Health Industries, UT, USA) following standardized test procedures (Gine-Garriga et al. 2014). The grip and strength were measured bilaterally and normalized to the body weight. The strength of ankle plantarflexors was tested using the manual muscle testing with a 25-level grade (Gine-Garriga et al. 2014).
General procedures
Subjects wore tight-fitting clothes and stood barefoot in front of a height adjustable chair. After making sure that the subjects had adopted their natural comfortable standing position, the outline of the feet was traced to mark the starting position where the subjects were required to return to for every trial. The two reaching tasks were performed in a random order with each task repeated twice. If the subject raised the heel or took a step during the test, the trial would be discarded and the task repeated. No reach strategy or performance feedback was given to the subjects.
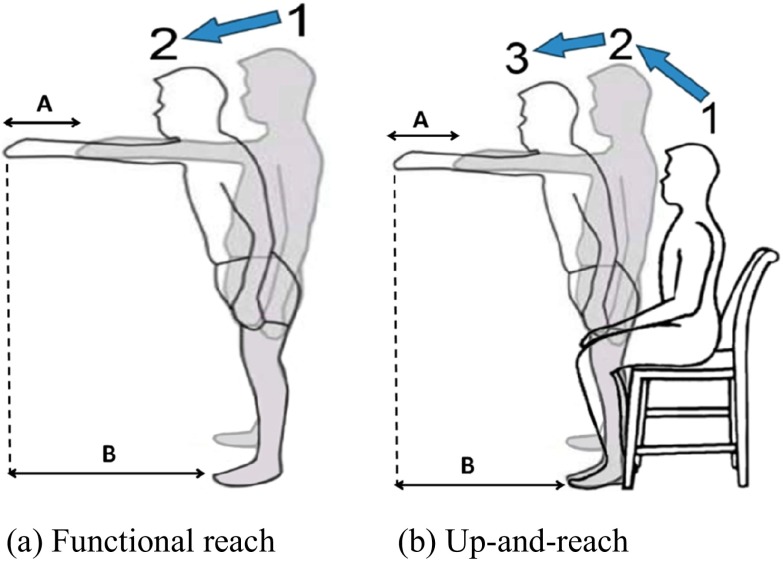
Forward reach (FR) test
For the forward reach task (FR, Fig. 1a), subjects first stood naturally at the starting position and raised the right arm to 90°, parallel to a yardstick suspended horizontally at the height of the acromion process. Subjects were then instructed to reach forward with the raised arm as far as possible at their own speed without moving their feet or losing balance as proposed by Duncan et al. (Duncan et al. 1990).
Fig. 1.
Illustrations of the functional reach (a) and up-and-reach (b) tasks. The finger-finger distance (A) is defined as the finger displacement from position 1 to position 2 in Fig. 1a, and from position 2 to position 3 in Fig. 1b, respectively. The finger-toe distance (B) is defined as the distance between finger and toe in the final position for both conditions
Up-and-reach (UR) test
For the up-and-reach task (UR, Fig. 1b), subjects first sat erect in an armless chair with the chair height adjusted to the popliteal line, the feet at the starting position and the midpoint of the thigh at the edge of the chair. The instruction was the same as for FR, except that subjects were to stand up to their full body height without using the hand for support before raising the arm. No instruction was given regarding if there should be any adjustment or pause during the task.
Instrumentation
The body kinematic data were recorded using a six-camera motion analysis system (VICON, V 624, Oxford Metrics Ltd., Oxford, UK) with a sampling rate of 100 Hz. Thirty-seven reflective markers were attached to the bilateral upper and lower extremities and the trunk according to the guidelines of the PlugInGait kinematics model (VICON, Oxford Metrics Ltd., Oxford, UK). For the estimation of joint centers to be used for the calculation of the kinematics, the body height and weight, leg length, hand thickness, and elbow, wrist, ankle, and knee width were measured first. Reflective markers were then attached to the following anatomical landmarks: bilateral sides of the anterior temple, posterior lateral head, acromion process, upper arm, lateral epicondyle, medial and lateral wrist, third metacarpal phalangeal joint, anterior superior iliac spine, posterior superior iliac spine, lateral thigh, lateral femoral epicondyle, lateral malleolus, heel, and dorsal second toe. Additional markers were attached to the seventh cervical and tenth thoracic vertebrae, right upper posterior trunk, sterno-clavicular notch, and inferior sternum for the estimation of the location of the total body COM.
Data reduction and analysis
Kinematic data were processed using the VICON 624 Workstation software (VICON, Oxford Metrics Ltd., Oxford, UK) and filtered using a Woltering quintic spline filter with a predicted mean square error of 20 mm. PlugInGait kinematics model with a 15-component link-segment was used to estimate the location of the total body COM and calculate the angular displacement. Computer algorithms written in the MATLAB language (V. 17, The MathWorks Inc., Natick, MA, USA) were used to calculate the variables of interest (as below).
The primary performance variable is reach distance. Two types of reach distance, finger-finger and finger-toe, were examined. Finger-finger distance is commonly measured clinically and in research and was analyzed in this study to allow for comparisons with the literature and providing clinical relevance. It was defined as the horizontal displacement of the finger marker (third metacarpal phalangeal joint) from the initial to final position (i.e., the farthest position in the anterior-posterior direction, Fig. 1). The initial position for FR was defined as the body alignment at the time when the finger marker began to move forward, i.e., the moment when the anteroposterior speed of the finger marker exceeded zero. The initial position for UR was defined as the body alignment at the time when the finger marker reached its highest level vertically after a period of upward motion (i.e., when the subject was standing up) and raising the arm and then began to move forward, i.e., the anteroposterior speed of the finger marker exceeding zero. Finger-toe distance was defined as the horizontal distance between the finger and second toe markers at the final position (Fig. 1). This measure was not affected by the initial posture and suitable for between-group or between-task comparisons when there were differences in the initial posture.
The movement patterns of the COM and lower extremity were also analyzed. The range of the COM displacement and averaged instantaneous COM velocity from the initial to final position in the anteroposterior and vertical directions were calculated. The angular displacement of the hip, knee, and ankle joints and thorax segment in the sagittal plane was also calculated. Furthermore, since the initial position may influence the calculation of the COM displacement (Hirose et al. 2004; Lin and Yang 2011; Shubert 2011), the COM location in relation to the second toe marker (COM-toe distance) in the anteroposterior and vertical directions and the lower limb joint angles and segmental orientation in the sagittal plane at both the initial and final positions were calculated. To control the effect of body stature and facilitate between-subject comparisons, reach distance, COM motion, and COM-toe distance were normalized to the body height for statistical analysis.
Statistical analysis
The differences in the anthropometric characteristics and lower extremity muscle strengths (except ankle plantarflexors) between the two age groups were compared using the independent t tests. The between-group differences in plantar sensitivity and ankle plantarflexor strength measures were compared using the nonparametric Mann-Whitney tests. To control the inflation of Type I error and account for the correlations among the dependent variables, multivariate analysis of variance (MANOVA) with factors of age group (between-subjects) and task condition (repeated within-subjects) was conducted for reach distance, COM displacement and velocity, COM-toe distance, and joint or segment angular displacement and orientation separately. For all the MANOVAs, the levels of correlation for their dependent variables were suitable (Brace et al. 2012; Mayers 2013). Post hoc univariate analysis and independent or paired t tests were conducted as indicated. All the analyses were conducted using the SPSS Statistics 17.0 software (SPSS, Chicago, IL, USA). A significance level of 0.05 was set for all statistical comparisons.
Results
The anthropometric characteristics and sensorimotor function of the two groups are presented in Table 1. Older adults had significantly smaller body height (p < 0.001) and weight (p = 0.022) than young adults. Older adults also had significantly poorer plantar sensitivity at all five testing sites and decreased strength in handgrip and the lower extremity muscle groups except the knee extensors (Table 1).
Table 1.
Means and standard deviations (parenthesis) of the anthropometric characteristics and sensorimotor functions for young and older adults
| Young adults | Older adults | p value | |||
|---|---|---|---|---|---|
| Anthropometric characteristics | |||||
| Age (years) | 22.55 | (2.42) | 74.10 | (7.50) | <0.001 |
| Gender (female/male)a | 10/12 | 10/10 | 0.374 | ||
| Height (cm) | 167.27 | (8.00) | 155.20 | (6.46) | <0.001 |
| Weight (kg) | 62.95 | (11.50) | 56.18 | (6.13) | 0.022 |
| Leg length (cm) | 84.44 | (5.19) | 81.37 | (5.14) | 0.062 |
| Foot length (cm) | 24.26 | (1.35) | 23.55 | (1.02) | 0.063 |
| Touch-pressure thresholdb | |||||
| Hallux | 2.59 | (0.52) | 3.30 | (0.44) | <0.001 |
| Third metatarsal head | 2.52 | (0.47) | 3.20 | (0.59) | <0.001 |
| Fifth metatarsal head | 2.66 | (0.52) | 3.58 | (0.61) | <0.001 |
| Lateral border of foot | 2.52 | (0.47) | 3.37 | (0.42) | <0.001 |
| Heel | 3.09 | (0.37) | 4.00 | (0.39) | <0.001 |
| Strength (% body weight) | |||||
| Grip | 51.11 | (11.81) | 39.99 | (9.97) | <0.001 |
| Hip flexors | 41.31 | (8.69) | 30.40 | (8.45) | <0.001 |
| Knee flexors | 33.61 | (9.31) | 25.13 | (8.12) | 0.003 |
| Knee extensors | 45.67 | (6.71) | 41.45 | (9.18) | 0.095 |
| Ankle dorsiflexors | 45.64 | (7.19) | 39.78 | (7.87) | 0.016 |
| Ankle plantarflexorb | 25.00 | (0.00) | 23.3 | (4.99) | 0.030 |
| Toe flexors | 16.56 | (6.32) | 11.00 | (4.94) | 0.003 |
aChi-square test
bNonparametric Mann-Whitney tests
Reach distance
The descriptive statistics of reach distance are summarized in Table 2. The results of MANOVA showed significant task (F = 9.507, p < 0.001) main effects, but not age effects (F = 1.966, p = 0.150) or interactions (F = 0.539, p = 0.587). Both the finger-finger and finger-toe distances in UR were significantly shorter than in FR (F = 19.052, p < 0.001 and F = 7.138, p = 0.011, respectively).
Table 2.
Means and standard deviations (parenthesis) of reach distance, center of mass (COM) motion, and angular displacement of the thorax and lower extremity joints in the sagittal plane between functional reach (FR) and up-and-reach (UR) tasks for young and older adults
| Young adults | Old adults | |||
|---|---|---|---|---|
| FR | UR | FR | UR | |
| Reach distance/height | ||||
| Finger-finger distance** | 0.2076 (0.0332) | 0.1780 (0.0482) | 0.1822 (0.0396) | 0.1571 (0.0588) |
| Finger-toe distance** | 0.5212 (0.0329) | 0.5095 (0.0305) | 0.5113 (0.0343) | 0.5058 (0.0286) |
| COM motion/height | ||||
| Anterior displacement*,** | 0.0827 (0.0161) | 0.0656 (0.0220) | 0.0660 (0.0200) | 0.0520 (0.0198) |
| Downward displacement** | 0.0477 (0.0248) | 0.0421 (0.0313) | 0.0564 (0.0303) | 0.0380 (0.0284) |
| Anterior velocity (1/s)*** | 0.0220 (0.0115) | 0.0250 (0.0122) | 0.0119 (0.0074) | 0.0080 (0.0053) |
| Downward velocity (1/s)*** | 0.0121 (0.0080) | 0.0141 (0.0092) | 0.0093 (0.0063) | 0.0056 (0.0045) |
| Angular displacement (degree) | ||||
| Thorax flexion** | 42.64 (12.41) | 28.83 (26.68) | 44.98 (17.88) | 26.22 (19.14) |
| Hip flexion** | 31.17 (15.44) | 22.49 (19.49) | 38.88 (22.06) | 29.07 (23.08) |
| Knee extension | 1.69 (2.46) | 1.13 (15.91) | 1.81 (6.66) | 4.74 (15.04) |
| Ankle plantarflexion | 5.85 (3.29) | 6.37 (4.74) | 7.29 (3.81) | 7.76 (7.03) |
*p < 0.05 for age main effect; **p < 0.05 for task main effect; ***p < 0.05 for age × task interactions
Movement strategies during reaching
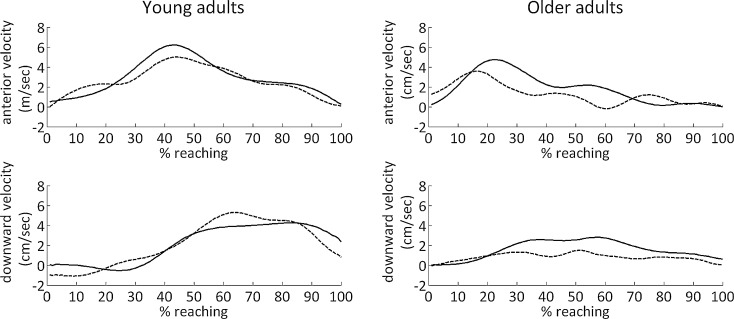
The averaged COM displacement and velocity data are summarized in Table 2. The results of MANOVA showed significant age (F = 5.877, p = 0.001) and task (F = 10.731, p < 0.001) main effects as well as interactions (F = 5.288, p = 0.002). Univariate analyses for the interactions showed that COM velocity in both the anteroposterior (F = 9.616, p = 0.004) and vertical (F = 5.860, p = 0.020) directions reached the significant level. Post hoc analyses showed that the COM anterior (t = 3.621, p = 0.002) and downward (t = −3.479, p = 0.003) velocity in UR were significantly smaller than FR for older adults, but not young adults (t = −1.067 p = 0.123; t = 0.996, p = 0.331, respectively) (Fig. 2). For the COM anterior and downward velocity, the task effects were nonsignificant (F = 0.144, p = 0.706; F = 0.498, p = 0.484, respectively), while the age effects were significant (F = 24.033, p < 0.001; F = 8.594, p = 0.006, respectively). The COM displacement did not reach the significant level in the univariate analysis for task × group interactions, and thus its task and age main effects were considered. Post hoc univariate analyses showed that older adults had significantly smaller COM anterior displacement than young adults (F = 8.281, p = 0.006) and UR had significantly smaller COM anterior (F = 27.074, p < 0.001) and downward displacements (F = 9.686, p = 0.003) than FR.
Fig. 2.
Representative examples of the anterior (top) downward (bottom) velocities of the center of mass (COM) during functional reaching (solid line) and up-and-reach (dashed line) for a young (left) and an older (right) adult. A reaching event is defined from the initial position (0 %) to the farthest position (100 %) of the finger marker. For the young adult, the difference between functional reach (solid line) and up-and-reach (dashed line) was minimal, while for the older adult, the difference was more apparent
The analysis of the movement patterns showed that overall, reaching forward primarily consisted of thorax and hip flexion and ankle plantarflexion motions (Table 2). The results of MANOVA showed significant task main effects (F = 6.647, p < 0.001), but not age main effects (F = 1.861, p = 0.138) or interactions (F = 0.549, p = 0.701). Univariate analyses showed significantly less thorax and hip flexion movements in UR, compared to FR (F = 25.602, p < 0.001; F = 5.222, p = 0.028, respectively).
Body alignment at initial and final positions
The descriptive statistics of the COM-toe distances, and joint angles or segmental orientation at the initial and final positions are summarized in Table 3. For the initial position, the results of MANOVA for COM-toe distances showed significant task main effects (F = 13.846, p < 0.001) but not age main effects (F = 0.560, p = 0.576) or interactions (F = 1.183, p = 0.317). Univariate analyses showed significantly smaller COM-toe anteroposterior distance in UR (F = 28.402, p < 0.001). For joint angles or segmental orientation, the results of MANOVA showed significant task main effects (F = 2.716, p = 0.044), but not age main effects (F = 0.297, p = 0.878) or interactions (F = 1.074, p = 0.383). Univariate analyses showed significantly greater thorax and hip flexion, and ankle dorsiflexion (F = 4.225, p = 0.046; F = 6.153, p = 0.017; F = 5.363, p = 0.026, respectively) in UR.
Table 3.
Means and standard deviations (parenthesis) of COM-toe distance, joint angles, or segmental orientations of the lower extremity joints and thorax in the sagittal plane at the initial and final positions between functional reach and up-and-reach tasks for young and older adults
| Young adults | Old adults | |||
|---|---|---|---|---|
| FR | UR | FR | UR | |
| Initial position | ||||
| COM-toe distance/height | ||||
| Anterior-posterior direction** a | −0.0151 (0.0156) | −0.0005 (0.0159) | −0.0125 (0.0116) | 0.0005 (0.0160) |
| Vertical direction | 0.5444 (0.0079) | 0.5434 (0.0110) | 0.5444 (0.0082) | 0.5358 (0.0270) |
| Joint angles and segmental orientations (degree) | ||||
| Thorax flexion**b | −1.03 (6.80) | 8.41 (26.52) | −0.45 (5.61) | 5.38 (11.67) |
| Hip flexion** | 1.04 (6.63) | 4.33 (13.09) | 0.79 (10.62) | 15.01 (38.55) |
| Knee flexion | 0.84 (5.35) | 3.57 (9.11) | 1.24 (8.56) | 3.91 (18.21) |
| Ankle dorsiflexion** | 8.29 (3.35) | 10.64 (3.35) | 9.02 (4.27) | 10.18 (5.40) |
| Final position | ||||
| COM-toe distance/height | ||||
| Anterior-posterior direction* | 0.0669 (0.0148) | 0.0640 (0.0155) | 0.0530 (0.0202) | 0.0517 (0.0193) |
| Vertical direction | 0.4960 (0.0276) | 0.5009 (0.0315) | 0.4874 (0.0305) | 0.4966 (0.0349) |
| Joint angles and segmental orientations (degree) | ||||
| Thorax flexion** | 41.12 (12.67) | 37.24 (19.35) | 43.66 (18.00) | 31.60 (20.34) |
| Hip flexion | 32.21 (16.50) | 32.34 (19.42) | 39.45 (23.51) | 36.39 (24.39) |
| Knee extension | 0.88 (5.76) | 7.39 (24.31) | 0.68 (10.10) | 1.12 (12.37) |
| Ankle dorsiflexion** | 2.38 (4.85) | 4.20 (5.58) | 1.69 (5.40) | 2.56 (6.48) |
aNegative value indicates that the COM is posterior to the toe
bNegative value indicates that the thorax is in an extended position
*p < 0.05 for age main effect; **p < 0.05 for task main effect
At the final position, the COM was located anteriorly to the toe marker in both reaching conditions for both groups. The results of MANOVA for COM-toe distances showed significant age main effects (F = 6.430, p = 0.004), but not task main effects (F = 2.147, p = 0.130) or interactions (F = 0.358, p = 0.702). The COM-toe anterior distance in older adults was significantly shorter than young adults (F = 6.435, p = 0.015). For joint angles and segmental orientation, the results of MANOVA showed significant task main effects (F = 2.590, p = 0.05), but not age main effects (F = 1.432, p = 0.243) or interactions (F = 1.821, p = 0.145). Univariate analyses showed significantly less thorax flexion and more ankle dorsiflexion in UR (F = 7.019, p = 0.011; F = 7.295, p = 0.010, respectively).
Discussion
Performing the same task under different conditions is likely to impose different levels of balance threats. The impact imposed by the increased balance threat and the movement patterns adopted to meet the balance demands might differ between young and older adults. This study found that compared to reaching forward from a quiet standing position, reaching immediately after standing up was associated with poorer task performance and modifications in movement strategy in both young and older adults. It was further noted that the extent of movement modification was greater in older adults. These findings support our hypotheses and are clinically relevant.
Reach distance, when defined as the distance the finger traveled while reaching forward, has been found to be shorter in older adults in previous studies (Duncan et al. 1990; Intiso et al. 2012). However, when reach distance was adjusted to the body height, the age differences were found to decrease (Isles, 2004; Lin and Liao 2011). In this study, for both FR and UR, there were no significant between-group differences in height-adjusted reach distances for both task conditions. These findings implied that the well-accepted notion of age-related declines in reach distance may, at least partly, be attributed to differences in the body stature and that aging may not necessarily result in a decline in reach distance.
In this study, although the instruction for UR did not specify if there should be a pause between standing up and reaching, the subjects, young and old alike, performed the task without a pause. Thus in UR, the reaching movement was performed under a more dynamic and hence less stable condition. It was found that UR had a significantly shorter reach distance. Because the initial location of the finger marker would affect the calculation of reach distance and was different between FR and UR, the finger-toe distance at the final position was further examined. It was found that the finger-toe distance was also significantly shorter in UR, indicating that the ability to move the arm forward was affected by the preceding standing up task.
Furthermore, although UR had shorter reach distance, its COM location, in relation to the anterior edge of the base of support, at the final position did not differ from FR. These findings were interesting for they suggested that the limitation in reaching forward in UR was not a result of inability in moving the COM forward. What appeared to be limited was the ability to manipulate the upper limb when the COM was near the boundary of stability. This reasoning is in line with a commonly accepted notion that the performance of focal movement can be affected by postural stability: Unstable posture is associated with poorer goal-directed target movement performance (Bouisset and Do 2008; Frank and Earl 1990; Massion 1992). These findings also suggested that learning to perform goal-directed movements while the body weight is shifted to more challenging positions or adding a preceding task to increase the task demand in balance training may help to improve the training effects and deserve to be considered clinically.
The task of reaching forward primarily consists of counter-clockwise rotation of the body, including thorax and hip flexion, and some ankle plantarflexion that is associated with trunk forward movement (Lin and Liao 2011; Suttanon et al. 2013). In this study, subjects went through a significantly smaller range of thorax and hip flexion, and their COM anterior and downward displacement was also smaller in UR. These findings were expected since the subjects initiated UR in a more flexed posture. Interestingly, there was no corresponding reduction in the ankle plantarflexion during reaching, resulting in a significantly greater ankle dorsiflexion angle at the final position in UR. To counter such a greater forward leaning around the ankle, a greater ankle plantarflexion torque would be needed. For healthy older adults such as those participated in this study, the increased demand in muscle torque in UR seemed to be manageable since none of the older adults lost balance during the experiment. However, for older adults with reduced plantarflexion strength, this strategy could possibly lead to loss of balance. Further studies examining the performance of up-and-reach in patient populations or frail older adults are needed to determine if UR is associated with a greater chance of falls.
In addition to the differences between UR and FR that were consistent across the two age groups, there were also between-task differences only observed in older adults: The COM anterior and downward velocity were significantly smaller in UR in older but not young adults. Such slowness did not seem to be caused by a limitation in the ability to move the COM quickly, since the velocity of the COM motion in FR did not show significant age effect. Moving the COM more slowly has been found when older adults were required to walk under more challenging conditions (Buracchio et al. 2011; Maki et al. 2011; Renfro and Fehrer 2011; Tsai and Lin 2013). Thus, the slowness observed in older adults in this study was likely to be a strategy specifically adopted to meet the increased task demand associated with UR. Based on these findings, older adults or individuals with impaired balance abilities should be advised to reach forward at a slower than their usual speed when the task is preceded by a dynamic task.
Several limitations of this study need to be acknowledged. The motion of some body segments, such as the scapulae or cervical spine, was not analyzed. Also, although subjects in this study did not pause between standing up and reaching in UR, individuals with impaired balance abilities might do so and thus the effects of a preceding dynamic task found in this study might not be applicable. Further studies are needed to address the above issues. Finally, the young and older subjects in this study differed significantly in their body height, a factor that could possibly affect reach performance (Isles et al. 2004; Lin and Liao 2011). This study hence adjusted the reach distance to the body height. However, the exact impact of such anthropometric differences is unclear.
Conclusion
Reaching forward immediately after standing up is a common daily task and was found to lead to shorter reach distances, but not limitations in the COM forward motion. In this task condition, the movement pattern placed a greater demand in the ability to generate ankle plantarflexion torque, and older adults were found to adopt a cautious strategy in moving the COM. Based on these findings, upper limb manipulation near the boundary of stability, adding a preceding dynamic task, ankle strengthening exercises, and/or safety precautions should be considered in balance training for older adults.
Acknowledgments
This study was supported by research grants from the National Science Council of Taiwan (NSC 100-2314-B-006-007 and NSC 100-2320-B-006-025).
References
- Agmon M, Belza B, Nguyen HQ, Logsdon RG, Kelly VE. A systematic review of interventions conducted in clinical or community settings to improve dual-task postural control in older adults. Clin Interv Aging. 2014;9:477–492. doi: 10.2147/CIA.S54978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman AL, Light KE, Flynn SM, Thigpen MT. Is the functional reach test useful for identifying falls risk among individuals with Parkinson’s disease? Arch Phys Med Rehabil. 2002;83(4):538–542. doi: 10.1053/apmr.2002.30934. [DOI] [PubMed] [Google Scholar]
- Bouisset S, Do MC. Posture, dynamic stability, and voluntary movement. Neurophysiol Clin. 2008;38(6):345–362. doi: 10.1016/j.neucli.2008.10.001. [DOI] [PubMed] [Google Scholar]
- Brace N, Kemp R, Snelgar R. SPSS for psychologists: a guide to data analysis using SPSS for Windows. 5. UK: Palgrave Macmillan; 2012. [Google Scholar]
- Brusse KJ, Zimdars S, Zalewski KR, Steffen TM. Testing functional performance in people with Parkinson disease. Phys Ther. 2005;85(2):134–141. [PubMed] [Google Scholar]
- Buracchio TJ, Mattek NC, Dodge HH, Hayes TL, Pavel M, Howieson DB, Kaye JA. Executive function predicts risk of falls in older adults without balance impairment. BMC Geriatr. 2011;11:74. doi: 10.1186/1471-2318-11-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camicioli R, Panzer VP, Kaye J. Balance in the healthy elderly: posturography and clinical assessment. Arch Neurol. 1997;54(8):976–981. doi: 10.1001/archneur.1997.00550200040008. [DOI] [PubMed] [Google Scholar]
- Chase CA, Mann K, Wasek S, Arbesman M. Systematic review of the effect of home modification and fall prevention programs on falls and the performance of community-dwelling older adults. Am J Occup Ther. 2012;66(3):284–291. doi: 10.5014/ajot.2012.005017. [DOI] [PubMed] [Google Scholar]
- Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):192–197. doi: 10.1093/geronj/45.6.M192. [DOI] [PubMed] [Google Scholar]
- Frank JS, Earl M. Coordination of posture and movement. Phys Ther. 1990;70(12):855–863. doi: 10.1093/ptj/70.12.855. [DOI] [PubMed] [Google Scholar]
- Gine-Garriga M, Roque-Figuls M, Coll-Planas L, Sitja-Rabert M, Salva A. Physical exercise interventions for improving performance-based measures of physical function in community-dwelling, frail older adults: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(4):753–769. doi: 10.1016/j.apmr.2013.11.007. [DOI] [PubMed] [Google Scholar]
- Hirose D, Ishida K, Nagano Y, Takahashi T, Yamamoto H. Posture of the trunk in the sagittal plane is associated with gait in community-dwelling elderly population. Clin Biomech (Bristol, Avon) 2004;19(1):57–63. doi: 10.1016/j.clinbiomech.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Horak FB, Nashner LM, Diener HC. Postural strategies associated with somatosensory and vestibular loss. Exp Brain Res. 1990;82(1):167–177. doi: 10.1007/BF00230848. [DOI] [PubMed] [Google Scholar]
- Horak FB, Shupert CL, Dietz V, Horstmann G. Vestibular and somatosensory contributons to responses to head and body displacements in stance. Exp Brain Res. 1994;100(1):93–106. doi: 10.1007/BF00227282. [DOI] [PubMed] [Google Scholar]
- Intiso D, Di Rienzo F, Russo M, Pazienza L, Tolfa M, Iarossi A, Maruzzi G. Rehabilitation strategy in the elderly. J Nephrol. 2012;25(Suppl 19):S90–95. doi: 10.5301/jn.5000138. [DOI] [PubMed] [Google Scholar]
- Isles RC, Choy NL, Steer M, Nitz JC. Normal values of balance tests in women aged 20–80. J Am Geriatr Soc. 2004;52(8):1367–1372. doi: 10.1111/j.1532-5415.2004.52370.x. [DOI] [PubMed] [Google Scholar]
- Kaut O, Allert N, Coch C, Paus S, Grzeska A, Minnerop M, Wullner U. Stochastic resonance therapy in Parkinson’s disease. NeuroRehabilitation. 2011;28(4):353–358. doi: 10.3233/NRE-2011-0663. [DOI] [PubMed] [Google Scholar]
- Kozak K, Ashton-Miller JA, Alexander NB. The effect of age and movement speed on maximum forward reach from an elevated surface: a study in healthy women. Clin Biomech (Bristol, Avon) 2003;18(3):190–196. doi: 10.1016/S0268-0033(02)00205-X. [DOI] [PubMed] [Google Scholar]
- Lam FM, Lau RW, Chung RC, Pang MY. The effect of whole body vibration on balance, mobility and falls in older adults: a systematic review and meta-analysis. Maturitas. 2012;72(3):206–213. doi: 10.1016/j.maturitas.2012.04.009. [DOI] [PubMed] [Google Scholar]
- Lin SI, Liao CF. Age-related changes in the performance of forward reach. Gait Posture. 2011;33(1):18–22. doi: 10.1016/j.gaitpost.2010.09.013. [DOI] [PubMed] [Google Scholar]
- Lin SI, Yang WC. Effect of plantar desensitization on postural adjustments prior to step initiation. Gait Posture. 2011;34(4):451–456. doi: 10.1016/j.gaitpost.2011.06.016. [DOI] [PubMed] [Google Scholar]
- Lin SI, Chen YR, Liao CF, Chou CW. Association between sensorimotor function and forward reach in patients with diabetes. Gait Posture. 2010;32(4):581–585. doi: 10.1016/j.gaitpost.2010.08.006. [DOI] [PubMed] [Google Scholar]
- Maki BE, et al. Reducing fall risk by improving balance control: development, evaluation and knowledge-translation of new approaches. J Saf Res. 2011;42(6):473–485. doi: 10.1016/j.jsr.2011.02.002. [DOI] [PubMed] [Google Scholar]
- Mann GC, Whitney SL, Redfern MS, Borello-France DF, Furman JM. Functional reach and single leg stance in patients with peripheral vestibular disorders. J Vestib Res. 1996;6(5):343–353. doi: 10.1016/0957-4271(96)00027-4. [DOI] [PubMed] [Google Scholar]
- Manton KG. A longitudinal study of functional change and mortality in the United States. J Gerontol. 1988;43(5):S153–161. doi: 10.1093/geronj/43.5.S153. [DOI] [PubMed] [Google Scholar]
- Martin JT, Wolf A, Moore JL, Rolenz E, DiNinno A, Reneker JC. The effectiveness of physical therapist-administered group-based exercise on fall prevention: a systematic review of randomized controlled trials. J Geriatr Phys Ther. 2013;36(4):182–193. doi: 10.1519/JPT.0b013e3182816045. [DOI] [PubMed] [Google Scholar]
- Massion J. Movement, posture and equilibrium: interaction and coordination. Prog Neurobiol. 1992;38(1):35–56. doi: 10.1016/0301-0082(92)90034-C. [DOI] [PubMed] [Google Scholar]
- Mayers A. Introduction to statistics and SPSS in psychology. 1. UK: Pearson Education Limited; 2013. [Google Scholar]
- Pozzo T, Stapley PJ, Papaxanthis C. Coordination between equilibrium and hand trajectories during whole body pointing movements. Exp Brain Res. 2002;144(3):343–350. doi: 10.1007/s00221-002-1052-6. [DOI] [PubMed] [Google Scholar]
- Renfro MO, Fehrer S. Multifactorial screening for fall risk in community-dwelling older adults in the primary care office: development of the fall risk assessment & screening tool. J Geriatr Phys Ther. 2011;34(4):174–183. doi: 10.1519/JPT.0b013e31820e4855. [DOI] [PubMed] [Google Scholar]
- Row BS, Cavanagh PR. Reaching upward is more challenging to dynamic balance than reaching forward. Clin Biomech (Bristol, Avon) 2007;22(2):155–164. doi: 10.1016/j.clinbiomech.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Seidel D, Brayne C, Jagger C. Limitations in physical functioning among older people as a predictor of subsequent disability in instrumental activities of daily living. Age Ageing. 2011;40(4):463–469. doi: 10.1093/ageing/afr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shubert TE. Evidence-based exercise prescription for balance and falls prevention: a current review of the literature. J Geriatr Phys Ther. 2011;34(3):100–108. doi: 10.1519/JPT.0b013e31822938ac. [DOI] [PubMed] [Google Scholar]
- Smith PS, Hembree JA, Thompson ME. Berg balance scale and functional reach: determining the best clinical tool for individuals post acute stroke. Clin Rehabil. 2004;18(7):811–818. doi: 10.1191/0269215504cr817oa. [DOI] [PubMed] [Google Scholar]
- Suttanon P, Hill KD, Said CM, Dodd KJ. A longitudinal study of change in falls risk and balance and mobility in healthy older people and people with Alzheimer disease. Am J Phys Med Rehabil. 2013;92(8):676–685. doi: 10.1097/PHM.0b013e318278dcb3. [DOI] [PubMed] [Google Scholar]
- Tran M, Bedard M, Dubois S, Weaver B, Molloy DW. The influences of psychotic symptoms on the activities of daily living of individuals with Alzheimer disease: a longitudinal analysis. Aging Ment Health. 2013;17(6):738–747. doi: 10.1080/13607863.2013.770446. [DOI] [PubMed] [Google Scholar]
- Tsai YJ, Lin SI. Older adults adopted more cautious gait patterns when walking in socks than barefoot. Gait Posture. 2013;37(1):88–92. doi: 10.1016/j.gaitpost.2012.06.034. [DOI] [PubMed] [Google Scholar]
- Wallmann HW. Comparison of elderly nonfallers and fallers on performance measures of functional reach, sensory organization, and limits of stability. J Gerontol A Biol Sci Med Sci. 2001;56(9):M580–583. doi: 10.1093/gerona/56.9.M580. [DOI] [PubMed] [Google Scholar]
- Weiner DK, Duncan PW, Chandler J, Studenski SA. Functional reach: a marker of physical frailty. J Am Geriatr Soc. 1992;40(3):203–207. doi: 10.1111/j.1532-5415.1992.tb02068.x. [DOI] [PubMed] [Google Scholar]