Abstract
Optimal strategies to improve food security and nutrition for people with HIV (PLHIV) may differ in settings where overweight and obesity are prevalent and cardiovascular disease risk is a concern. However, no studies among PLHIV have investigated the impact of food support on nutritional outcomes in these settings. We therefore assessed the effect of food support on food insecurity and body weight in a population of PLHIV with high prevalence of overweight and obesity. We implemented a pilot intervention trial in 4 government-run HIV clinics in Honduras. The trial tested the effect of a monthly household food ration plus nutrition education (n=203), compared to nutrition education alone (n=197), over 12 months. Participants were clinic patients receiving antiretroviral therapy (ART). Assessments were obtained at baseline, 6 and 12 months. Primary outcomes for this analysis were food security, using the validated Latin American and Caribbean Food Security Scale, and body weight (kg). Thirty-one percent of participants were overweight (22%) or obese (8%) at baseline. At 6 months, the probability of severe food insecurity decreased by 48.3% (p < 0.01) in the food support group, compared to 11.6% in the education-only group (p<0.01). Among overweight or obese participants, food support led to average weight gain of 1.13 kg (p<0.01), while nutrition education alone was associated with average weight loss of 0.72 kg (p<0.10). Nutrition education alone was associated with weight gain among underweight and normal weight participants. Household food support may improve food security but not necessarily nutritional status of ART recipients above and beyond nutrition education. Improving nutritional tailoring of food support and testing the impact of nutrition education should be prioritized for PLHIV in Latin America and similar settings.
Keywords: food security, nutrition, HIV, antiretroviral therapy, food support, intervention, obesity, Latin America
INTRODUCTION
The negative relationship between food insecurity and HIV outcomes is now well recognized in resource-limited settings (Weiser et al., 2009; Weiser et al., 2012; Weiser et al., 2013; Young, Wheeler, McCoy, & Weiser, 2013). Yet strategies to improve food security and nutrition in order to achieve better HIV outcomes are still underdeveloped. Furthermore, optimal strategies may differ in settings where overweight and obesity are prevalent among food insecure people living with HIV (PLHIV). Food insecurity may contribute to obesity through both behavioral and biological pathways (Laraia, 2013). Yet, implications for food security programming among overweight or obese PLHIV for who weight gain is undesirable have not yet been explored.
Over the last 10 years, the World Health Organization (WHO) and other international organizations have issued recommendations that nutritional assessment, counseling and support be a standard part of comprehensive care for HIV (FANTA, 2004; World Bank, 2007; World Health Organization, 2008). While research generally finds a positive effect of supplemental feeding on the nutritional status and HIV outcomes of underweight PLHIV (Koethe, Chi, Megazzini, Heimburger, & Stringer, 2009; Tirivayi & Groot, 2011), providing food support to overweight or obese PLHIV may result in further weight gain even if food security improves (Larson & Story, 2011; Leroy, Gadsden, de Cossío, & Gertler, 2013), putting PLHIV at risk for chronic comorbidities such as diabetes and cardiovascular disease.
With data from a pilot intervention study in Honduras, we investigated how food support combined with nutrition education influences food security and body weight, compared to nutrition education alone, in a population with high food insecurity and diverse nutritional statuses.
METHODS
We pair matched four urban government-run HIV care centers by region and patient number. Within each pair, clinics were randomly assigned to provide 12 months of food support (monthly household food ration from the UN World Food Programme) plus nutrition education, or nutrition education only. Nutrition education consisted of monthly nutritional counselling and assessment, and group education sessions. Patient eligibility criteria included: local residence, age 18+, receiving ART, and food insecurity and/or BMI ≤ 18.5. Assessments were conducted at baseline, 6 and 12 months. The study was approved by RAND’s Human Subjects Protection Committee and the Institutional Review Board at the National Autonomous University of Honduras. Written informed consent was obtained from all participants. A fuller description of the study design has been published elsewhere (Martinez et al., 2014).
Measures
We used the validated 15-item Latin American and Caribbean Food Security Scale (Comité Científico de la ELCSA & United Nations Food and Agriculture Organization, 2012) to assess household food security. Weight and height measurements were taken by study nutritionists using methods to promote standardization (Habicht, 1974). Nutritional status based on body mass index (BMI) (kg/m2) was classified as underweight (< 18.5), normal (18.5 to 25), overweight (25 to 30), and obese (≥ 30) (World Health Organization).
We considered the following as potential confounding variables: sex, race/ethnicity, age, presence of children in the household, having primary school education or above, having paid work in the last month, receiving economic support from a relative, friend or other source, CD4 count (in cells/μL), taking protease inhibitors, and being on ART less than 100 days.
Analysis
We used multilevel mixed effects linear regression analysis to investigate intervention effects on food insecurity and weight, and to take into account correlations within clinic clusters and within individuals across time. We specified our food insecurity regression using a linear probability model (LPM) in order to ease interpretation of the program effect interaction term. We stratified the weight regressions by baseline BMI classification to identify differential effects of the intervention for underweight, normal, and overweight or obese participants. We controlled for factors differentiating the intervention groups at baseline. Finally, we included clinic indicators to account for clustering, and the month-of-interview to account for seasonal changes in food availability. All statistical analyses were conducted in STATA/IC 11.1 (StataCorp: College Station, Texas).
RESULTS
The sample consisted of 400 participants (203 receiving food support). Table 1 describes baseline sociodemographic and health characteristics of the sample. Eighty-eight percent of the food support group and 76% of the education-only group completed the 12-month assessment.
Table 1.
Demographic, health and socio-economic characteristics at baseline
| Intervention Group
|
||||
|---|---|---|---|---|
| All participants | Food support + Nutrition education | Nutrition education only | p-value | |
|
|
||||
| Demographics | ||||
| Female, % | 69 | 74 | 62 | <0.01 |
| Afrodescendent, % | 12 | 4 | 19 | <0.01 |
| Primary school or more, % | 54 | 49 | 58 | 0.06 |
| Age in years, mean [SD] | 40 [9.8] | 40 [9.9] | 41 [9.6] | 0.12 |
| HH w/children < 18 y.o, % | 82 | 87 | 77 | <0.01 |
| HH size incl. participant, mean [SD] | 4.9 [2.5] | 5.1 [2.5] | 4.7 [2.5] | 0.05 |
| HIV-related health | ||||
| Years since HIV diagnosis, mean [SD] | 5.3 [3.9] | 5.1 [3.7] | 5.4 [4.1] | 0.25 |
| Years receiving ART, mean [SD] | 3.7 [2.4] | 3.6 [2.3] | 3.8 [2.6] | 0.24 |
| Receiving ART < 100 days, % | 9 | 7 | 11 | 0.14 |
| Takes protease inhibitors, % | 7 | 8 | 6 | 0.14 |
| CD4 (cells/mm3) category, % | 28 | 26.1 | 30 | 0.46 |
| 200–349 | 27.5 | 26.1 | 28.9 | |
| 350–499 | 19.8 | 22.7 | 16.8 | |
| ≥500 | 24.8 | 25.1 | 24.4 | |
| Socio-economic status | ||||
| Had paid work in last month, % | 38 | 33 | 44 | 0.02 |
| Material support from family or friends, % | 32 | 28 | 35 | 0.04 |
| Number of observations | 400 | 203 | 197 | |
Note: HH = “household”. p-values denote significance of comparison in baseline characteristics between the food support group and education-only group. Bolded values are significant at p<0.05.
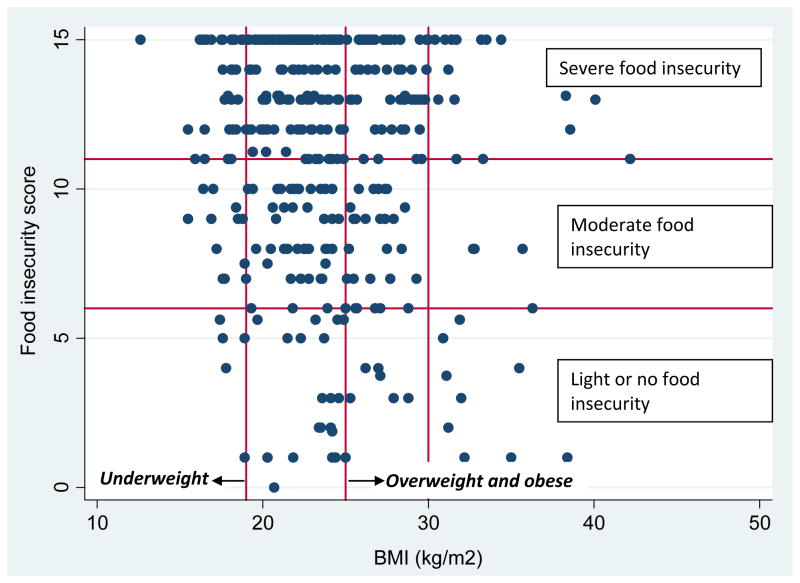
Two-thirds of study participants were severely food insecure [65%] (Table 2) and approximately one-third were either overweight [23%] or obese [8%]. Only 11% of participants were underweight. We found significant co-occurance of food insecurity and high BMI (i.e. overweight or obesity) in the study population at baseline (Figure 1).
Table 2.
Food security and nutrition characteristics at baseline
| Intervention Group
|
||||
|---|---|---|---|---|
| All participants | Food support + nutrition education | Nutrition education only | p-value | |
|
|
||||
| Household food insecurity | ||||
| Mean standard score [SD] | 11.4 [3.9] | 12.0 [3.3] | 10.7 [4.4] | <0.01 |
| Severe, % | 65 | 72 | 58 | <0.01 |
| Moderate, % | 24 | 22 | 26 | |
| Light, % | 10 | 5 | 15 | |
| None, % | 1 | 0 | 1 | |
| Body mass index (BMI) | ||||
| Mean BMI [SD] | 24 [4.5] | 23 [4.3] | 24 [4.7] | 0.12 |
| Underweight, % | 11 | 12 | 9 | 0.47 |
| Normal, % | 58 | 58 | 58 | |
| Overweight, % | 23 | 23 | 24 | |
| Obese, % | 8 | 7 | 9 | |
| Weight (kg) [SD] | 58.4 [12.2] | 57.0 [11.4] | 60.0 [12.8] | <0.01 |
| Number of observations | 400 | 203 | 197 | |
Note: p-values denote significance of comparison in baseline characteristics between the food support group and education-only group.
Figure 1. Correlation between food insecurity and BMI at baseline.
Note: Correlation = − 0.12 (p < 0.01)
In the multivariable regression models, the probability of severe food insecurity (Table 3) was 11.6% lower on average for the education-only group (p<0.01) and an additional 36.7% lower (p<0.01) (i.e. 48.3% total decrease) for the food support group at 6 months. There was no significant change in the probability of severe food insecurity from 6 to 12 months.
Table 3.
Effect of food support on the probability of severe food insecurity
| Outcome: Severe food insecurity | ||
|---|---|---|
| Months: | 0–6 | 6–12 |
| β (SE) | ||
| Time | −0.116*** (0.039) | 0.005 (0.054) |
| Food support group X Time | −0.367*** (0.051) | 0.043 (0.070) |
| Baseline covariates: | ||
| Food support group | 0.353*** (0.124) | −0.504** (0.226) |
| Female | 0.032 (0.030) | 0.080* (0.042) |
| Afrodescendent | −0.014 (0.048) | −0.029 (0.065) |
| Child dependents in household | 0.010 (0.035) | 0.029 (0.051) |
| Completed primary school | −0.031 (0.026) | −0.024 (0.036) |
| Severe food insecurity | 0.707*** (0.027) | 0.311*** (0.038) |
| Had paid work in the last month | −0.003 (0.026) | 0.011 (0.037) |
| Material support from family/friends | 0.013 (0.028) | −0.004 (0.039) |
| CD4 category (cells/μL) | ||
| <200 | ||
| 200–349 | −0.018 (0.035) | −0.049 (0.049) |
| 350–499 | −0.074* (0.039) | −0.114** (0.054) |
| ≥500 | 0.007 (0.038) | −0.008 (0.053) |
| Observations | 684 | 611 |
| Number of groups | 4 | 4 |
p<0.01,
p<0.05,
p<0.10;
Notes: Food support group also received the nutrition education. Regressions in Table 3 use linear probability models with the binary food insecurity outcome. Beta coefficients represent the change of probability of the outcome with one unit increase in the independent variable. In addition to the covariates shown here, we adjusted for clinic and a set of indicators for month of interview.
In the multivariable regression models for weight (Table 4), underweight participants in both study groups gained 3.15 kg (p<0.01) on average after 6 months, while normal weight participants in both study groups gained 1.34 kg in the same time period. Among overweight or obese participants, the education-only group lost −0.72 kg on average (p=0.068) after 6 months, while the food support group gained an average of 1.13 kg (i.e. 2.03 – 0.72). There were no significant program effects for any of the weight analyses between 6 and 12 months.
Table 4.
Effect of food support on body weight (kg), stratified by baseline BMI classifications
|
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Baseline BMI classification | ||||||||
|
| ||||||||
| Outcome: Weight (kg) | Full sample | Underweight (BMI<18.5) | Normal weight (18.5≤ BMI<25) | Overweight or obese (BMI≥25) | ||||
| Months: | 0–6 | 6–12 | 0–6 | 6–12 | 0–6 | 6–12 | 0–6 | 6–12 |
| Column | (1) | (2) | (3) | (4) | (5) | (6) | (7) | (8) |
| β (SE) | ||||||||
| Time | 0.863*** (0.282) | −0.140 (0.488) | 3.150*** (1.083) | −0.251 (1.678) | 1.343*** (0.367) | −0.002 (0.595) | −0.724* (0.397) | −0.328 (0.855) |
| Food support group X Time | 0.632* (0.370) | −0.045 (0.634) | 1.639 (1.421) | 1.997 (2.263) | −0.321 (0.477) | 0.361 (0.766) | 2.027*** (0.536) | −1.180 (1.145) |
| Baseline covariates: | ||||||||
| Food support group | −0.925 (0.909) | 0.031 (2.025) | −3.666 (3.263) | −5.245 (6.771) | 0.254 (1.168) | −0.936 (2.442) | −2.227* (1.350) | 2.669 (3.699) |
| Female | −0.446** (0.216) | −1.167*** (0.376) | 0.240 (1.260) | −0.394 (2.153) | −0.533* (0.303) | −1.353*** (0.491) | 0.369 (0.479) | 1.206 (1.147) |
| Afrodescendent | −0.145 (0.356) | −0.164 (0.605) | −1.949 (1.775) | −6.812** (2.822) | −0.577 (0.478) | −0.661 (0.772) | 0.562 (0.535) | 0.263 (1.110) |
| Child dependents in household | −0.462* (0.250) | −1.203*** (0.449) | −2.011* (1.195) | −1.532 (2.265) | −0.695** (0.310) | −1.498*** (0.517) | 0.014 (0.433) | −1.051 (1.018) |
| Completed primary school | 0.021 (0.188) | 0.428 (0.325) | −1.792** (0.909) | −0.562 (1.526) | 0.148 (0.241) | 0.640 (0.390) | −0.216 (0.297) | −0.079 (0.655) |
| Severe food insecurity | 0.010 (0.198) | 0.100 (0.343) | 0.276 (0.806) | 2.641** (1.290) | −0.050 (0.264) | 0.007 (0.423) | 0.285 (0.290) | 0.500 (0.639) |
| Weight | 0.977*** (0.008) | 0.927*** (0.015) | 0.986*** (0.084) | 1.077*** (0.141) | 0.983*** (0.020) | 0.934*** (0.033) | 0.990*** (0.014) | 0.967*** (0.032) |
| Had paid work in the last month | −0.144 (0.193) | −0.142 (0.336) | −0.850 (1.041) | −1.012 (1.831) | −0.448* (0.249) | −0.603 (0.414) | 0.320 (0.285) | 0.505 (0.629) |
| Material support from family/friends | 0.195 (0.201) | 0.071 (0.353) | −0.494 (0.833) | 0.956 (1.439) | 0.545** (0.273) | 0.932** (0.448) | 0.258 (0.322) | 0.324 (0.713) |
| CD4 category (cells/μL) | ||||||||
| 200–349 | −0.546** (0.253) | −1.411*** (0.444) | 0.015 (1.027) | −2.930* (1.563) | −0.405 (0.319) | −1.184** (0.521) | −0.295 (0.436) | −0.324 (1.026) |
| 350–499 | −0.439 (0.278) | −1.082** (0.482) | −0.545 (1.197) | −4.231** (1.996) | −0.628* (0.371) | −1.249** (0.588) | −0.057 (0.456) | (1.062) |
| ≥500 | −0.082 (0.272) | 0.012 (0.480) | 3.198*** (1.045) | 6.533*** (1.932) | −0.119 (0.362) | −0.016 (0.590) | −0.394 (0.450) | 0.130 (1.045) |
| Observations | 704 | 629 | 78 | 68 | 401 | 363 | 225 | 198 |
| Number of groups | 4 | 4 | 4 | 4 | 4 | 4 | 4 | 4 |
p<0.01,
p<0.05,
p<0.10;
Notes: Food support group also received the nutrition education. Beta coefficients represent the change in the magnitude of the outcome with one unit increase in the independent variable. In addition to the covariates shown here, we adjusted for clinic and a set of indicators for month of interview.
DISCUSSION
In our study of PLHIV in Honduras with high dual prevalence of food insecurity and overweight and obesity, we find that food support plus nutrition education improves food security compared to education alone, but also leads to weight gain for overweight or obese participants in contrast to weight loss among those who received education only. These results emphasize growing concern over the ability of targeted food support to improve the health of food insecure overweight PLHIV, particularly when calorically-dense provisions are typically used in emergency food aid to populations at risk of undernutrition.
Improving food security through food support may play an important role in alleviating suffering and improving the mental and physical health of PLHIV. However, our results suggest that improving nutritional tailoring of food support by reducing excessive calories and favoring micronutrient-rich foods including fruits and vegetables may be needed to fully benefit food insecure PLHIV with higher BMI. Excess weight can exacerbate metabolic syndrome which is sometimes a side effect of ART and is associated with increased risk of type 2 diabetes mellitus and cardiovascular disease (Friis-Møller et al., 2003). Obesity is also associated with poorer immunologic response to ART (Crum-Cianflone et al., 2010). However, changing food support composition may be difficult if the agencies providing food support are constrained by policy or logistical considerations to rely on calorically-dense staple foods.
We found improved weight and food security among PLHIV who received only nutrition education. It is plausible that nutrition education could improve food insecurity and weight via improved diet quality, the ability to make the most of existing food resources, and decreased anxiety about procuring healthy food (Eicher-Miller, Mason, Abbott, McCabe, & Boushey, 2009). However, without a comparable control group of PLHIV not receiving any intervention, we cannot formally test these effects.
Limitations of our study included that the food support group differed systematically from the nutrition education group, including in their level of food insecurity. While we controlled for observed characteristics that differentiated the study groups at baseline in the analysis, unobserved variables may still bias our regressions. In addition, while we implemented multilevel mixed models to deal with clinic-level clustering, the small number of clusters is a limitation and our results should be taken as preliminary.
Despite positive results of the food support intervention on food security, resource constraints and the rise of food prices makes it increasingly difficult for HIV treatment programs to provide adequate and sustainable food support to those in need (Sztam, Fawzi, & Duggan, 2010). Thus, while nutritional tailoring of food support is an important step to improve its efficacy for overweight or obese PLHIV, sustainable interventions such as locally-tailored nutrition education may have significant benefits and should be made more widely available.
Acknowledgments
We thank the study coordinator, Blanca Ramírez, and the interviewers for their hard work and dedication in the field. Sheri Weiser (UCSF) provided critical feedback on earlier versions of this paper. Most importantly, we offer deep appreciation to the study participants who gave so generously of their time and personal information.
FUNDING
This work was funded by the National Institutes of Mental Health (NIMH) under R34MH084675 (PI: Dr. Martinez). Dr. Palar received dissertation support from the Pardee Dissertation Award (RAND) and postdoctoral salary support from the Agency for Healthcare Research and Quality (AHRQ) T32HS00046. The contents of this paper are solely the responsibility of the authors and do not represent the official views of NIMH or AHRQ.
LIST OF ABBREVIATIONS
- ART
antiretroviral therapy
- PLHIV
people living with HIV
- WHO
World Health Organization
- BMI
body mass index
- CD4
cluster of differentiation 4
- LPM
linear probability model
Footnotes
DISCLOSURE STATEMENT
The author(s) declare that they have no competing interests
Contributor Information
Kartika Palar, Email: kpalar@ucsf.edu, Division of HIV/AIDS, Department of Medicine, University of California, San Francisco, San Francisco, CA; Tel: (310)-741-8492.
Kathryn Pitkin Derose, Email: derose@rand.org, RAND Corporation, Santa Monica, CA USA; Tel: (310) 393-0411.
Sebastian Linnemayr, Email: slinnema@rand.org, RAND Corporation, Santa Monica, CA USA; Tel: (310) 393-0411.
Alexandria Smith, Email: asmith@rand.org, RAND Corporation, Santa Monica, CA USA; Tel: (310) 393-0411.
Hugo Farías, Email: hugo.farias@wfp.org, United Nations World Food Program, Regional Office for Latin America and the Caribbean, Panama City, Panama; Tel: (507) 317-3939.
Glenn Wagner, Email: gwagner@rand.org, RAND Corporation, Santa Monica, CA USA; Tel: (310) 393-0411.
Homero Martinez, Email: homero@rand.org, RAND Corporation, Santa Monica, CA USA and Hospital Infantil de Mexico Federico Gomez, Mexico City, Mexico; Tel: (310) 393-0411.
References
- Comité Científico de la ELCSA, & United Nations Food and Agriculture Organization. Escala Latinoamericana y Caribeña de Seguridad Alimentaria (ELCSA): Manual de Uso y Aplicaciones. Rome: United Nationas Food and Agriculture Organization (FAO); 2012. ( http://www.fao.org/alc/file/media/pubs/2012/elcsa.pdf) [Google Scholar]
- Crum-Cianflone NF, Roediger M, Eberly LE, Vyas K, Landrum ML, Ganesan A, Agan BK. Obesity among HIV-infected persons: impact of weight on CD4 cell count. AIDS. 2010;24(7):1069. doi: 10.1097/QAD.0b013e328337fe01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eicher-Miller HA, Mason AC, Abbott AR, McCabe GP, Boushey CJ. The effect of Food Stamp Nutrition Education on the food insecurity of low-income women participants. Journal of Nutrition Education and Behavior. 2009;41(3):161–168. doi: 10.1016/j.jneb.2008.06.004. [DOI] [PubMed] [Google Scholar]
- FANTA. HIV/AIDS: A guide for nutritional care and support. 2. Washington, DC: Academy for Educational Development; 2004. [Google Scholar]
- Friis-Møller N, Weber R, Reiss P, Thiébaut R, Kirk O, Monforte AA, Law M. Cardiovascular disease risk factors in HIV patients-association with antiretroviral therapy. Results from the DAD study. AIDS. 2003;17(8):1179. doi: 10.1097/01.aids.0000060358.78202.c1. [DOI] [PubMed] [Google Scholar]
- Habicht J. Estandarización de metodos epidemiológicos cuantitativos sobre el terreno; Standardization of quantitative epidemiological methods in the field. Boletín de la Oficina Sanitaria Panamericana (OSP) 1974;76(5):375–384. [PubMed] [Google Scholar]
- Koethe J, Chi B, Megazzini K, Heimburger D, Stringer J. Macronutrient supplementation for malnourished HIV-infected adults: a review of the evidence in resource-adequate and resource-constrained settings. Clinical Infectious Diseases. 2009;49(5):787–798. doi: 10.1086/605285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia BA. Food Insecurity and Chronic Disease. Advances in Nutrition: An International Review Journal. 2013;4(2):203–212. doi: 10.3945/an.112.003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Story MT. Food Insecurity and Weight Status Among US Children and Families:: A Review of the Literature. American Journal of Preventive Medicine. 2011;40(2):166–173. doi: 10.1016/j.amepre.2010.10.028. [DOI] [PubMed] [Google Scholar]
- Leroy JL, Gadsden P, de Cossío TG, Gertler P. Cash and in-kind transfers lead to excess weight gain in a population of women with a high prevalence of overweight in rural Mexico. The Journal of nutrition. 2013;143(3):378–383. doi: 10.3945/jn.112.167627. [DOI] [PubMed] [Google Scholar]
- Martinez H, Palar K, Linnemayr S, Smith A, Derose KP, Ramírez B, Wagner G. Tailored Nutrition Education and Food Assistance Improve Adherence to HIV Antiretroviral Therapy: Evidence from Honduras. AIDS and Behavior. 2014:1–12. doi: 10.1007/s10461-014-0786-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sztam KA, Fawzi WW, Duggan C. Macronutrient supplementation and food prices in HIV treatment. Journal of Nutrition. 2010;140(1):213S–223S. doi: 10.3945/jn.109.110569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tirivayi N, Groot W. Health and welfare effects of integrating AIDS treatment with food assistance in resource constrained settings: a systematic review of theory and evidence. Social Science & Medicine. 2011;73(5):685–692. doi: 10.1016/j.socscimed.2011.06.056. [DOI] [PubMed] [Google Scholar]
- Weiser SD, Fernandes KA, Brandson EK, Lima VD, Anema A, Bangsberg DR, Hogg RS. The association between food insecurity and mortality among HIV-infected individuals on HAART. J Acquir Immune Defic Syndr. 2009;52(3):342–349. doi: 10.1097/QAI.0b013e3181b627c2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Gupta R, Tsai AC, Frongillo EA, Grede N, Kumbakumba E, Bangsberg DR. Changes in food insecurity, nutritional status, and physical health status after antiretroviral therapy initiation in rural Uganda. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;61(2):179–186. doi: 10.1097/QAI.0b013e318261f064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiser SD, Palar K, Frongillo EA, Tsai AC, Kumbakumba E, Depee S, Bangsberg D. Longitudinal assessment of associations between food insecurity, antiretroviral adherence and HIV treatment outcomes in rural Uganda. AIDS (London, England) 2013 doi: 10.1097/01.aids.0000433238.93986.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank. HIV/AIDS, Nutrition and Food Secuirty: What We Can Do - A Synthesis of International Guidance. Washington DC: World Bank; 2007. [Google Scholar]
- World Health Organization. BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Retrieved April 17, 2012, from http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- World Health Organization. Essential prevention and care interventions for adults and adolescents living with HIV in resource-limited settings. Geneva: World Health Organization; 2008. [Google Scholar]
- Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS and Behavior. 2013:1–11. doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]