Abstract
Objective
To evaluate the mediating effect of depressive symptoms on the relationship between physical symptoms and health-related quality of life (HRQOL) in hematopoietic stem cell transplant survivors (HSCT); and to test a conceptual model of psychosocial factors, in addition to physical and psychological symptoms, that might contribute to HRQOL.
Methods
This is a secondary data analysis using subjects (N=662) identified from the Center for International Blood and Marrow Transplant Research for HSCT survivors who were treated in 40 North American Medical Centers. Data were collected through mailed surveys, phone interviews, and medical records. We used structural equation modeling to test the mediating role of depressive symptoms on the relationship of physical symptoms with HRQOL. We also tested comprehensive pathways from physical symptoms to HRQOL by adding other psychosocial factors including optimism, coping, and social constraints.
Results
In the depressive symptom mediation analyses, physical symptoms had a stronger direct effect on physical HRQOL (b=−0.98, p<0.001) than depressive symptoms (b=0.23, p>0.05). Depressive symptoms were associated with mental HRQOL and mediated the relationship between physical symptoms and mental HRQOL. In the comprehensive pathway analyses, physical symptoms remained the most significant factor to be associated with physical HRQOL. In contrast, depressive symptoms had a direct effect (b=−0.76, p<0.001) on mental HRQOL and were a significant mediator. Psychosocial factors were directly associated with mental HRQOL and indirectly associated with mental HRQOL through depressive symptoms.
Conclusion
Physical symptoms are most strongly associated with physical HRQOL; while depressive symptoms and psychosocial factors impact mental HRQOL more than physical HRQOL. Interventions targeting physical/psychological symptoms and psychosocial factors may improve HRQOL of HSCT survivors.
Keywords: Hematopoietic stem cell transplant, cancer survivor, symptoms, psychosocial factors, health-related quality of life
Introduction
The success of hematopoietic stem cell transplantation (HSCT) as a treatment for cancer has shifted the research focus from how long survivors are living to how well they are living (1). HSCT survivors are at risk of developing chronic conditions and other late effects that influence survivors’ symptoms, functional status, and health-related quality of life (HRQOL) (2-4). While many survivors recover to a health status similar to pre-treatment or comparable to the general population, a portion of survivors have persistent long-term late effects as a result of HSCT (5). This group of survivors living with long-term effects, particularly physical (e.g., pain, sleep problems) and psychological symptoms (e.g., depressive symptoms), are likely to experience a significant decrease in in physical and mental HRQOL (4, 6, 7).
Although individual physical and depressive symptoms strongly influence physical and mental HRQOL in HSCT survivors (8, 9), respectively, little is known about the influence of the relationship between physical and depressive symptoms on HRQOL. For example, the persistence of physical symptoms increases depressive symptoms experienced by a survivor (5), subsequently negatively impacting HRQOL. In addition to symptoms, intrapersonal and psychosocial factors, such as optimism, coping or social constraints, have been found to be independently associated with both the symptoms (10-12) and HRQOL in HSCT survivors (13-15). Dispositional optimism refers to a person's tendency to perceive positive outcomes within a negative experience (16). Evidence suggests that optimism is a predictor of lower symptom reports, and better overall HRQOL in HSCT survivors (14, 17). Social constraints refer to the withholding or modifying of disclosures to an individual's social network, such as friends or spouses, due to a lack of receptiveness to their disclosures, contributing to increased post-transplant distress (18, 19). In the context of HSCT, coping strategies are theorized to be the consequence of having to manage the physically and psychologically demanding experience of HSCT and the resulting symptoms (20). Experiencing fewer physiological effects or fewer symptoms of HSCT contributes to the use of more problem-focused coping strategies while experiencing greater symptoms results in avoidant coping strategies (11, 20).
Research on the complex interrelationships between symptom factors and psychosocial factors and their effects on HRQOL among long-term HSCT survivors is sparse (12). It is important to develop and test a conceptual model of the relationship between different factors and HRQOL in HSCT survivors (12, 21). Previous studies on HSCT survivors have examined the effects of a subset of the symptoms and psychosocial factors on HRQOL (22-25), which limits the ability to examine the relationships among a comprehensive set of factors (12). The purpose of the present study was to test a conceptual model describing the relationships between physical symptoms, depressive symptoms, psychosocial variables (e.g., optimism, social constraints, and coping), and HRQOL through two specific aims. Aim 1 evaluated whether depressive symptoms mediated the relationship between physical symptoms and HRQOL in long-term survivors of HSCT. We hypothesized that physical symptoms would be associated with physical and mental HRQOL typically through the influence of depressive symptoms. Aim 2 evaluated the contribution of psychosocial variables (optimism, social constraints, coping) to HRQOL in addition to physical and depressive symptoms. We proposed a conceptual model and evaluated the pathways through which the psychosocial variables influence the relationships between physical symptoms, depressive symptoms and HRQOL. We hypothesized that psychosocial variables are more significantly associated with mental HRQOL than with physical HRQOL.
Methods
Participants and Data Collection
This study used secondary data collected from long-term cancer/HSCT survivors who were enrolled in a multi-site study (26). A detailed description of patient characteristics and data collection has been described in previous studies (26-28). Briefly, potential participants were HSCT recipients at 40 participating North American transplant centers with records identified from the Center for International Blood and Marrow Transplant Research (CIBMTR). Eligibility criteria included an age of 18 years or older, a single allogeneic or autologous HSCT for a specific diagnosis of cancer (chronic myelogenous leukemia, acute leukemia, lymphoma, or breast cancer), survival at least 12 months post-HSCT, continuous remission since HSCT, and able to read and understand English. Among 2,447 survivors initially identified from the Registry, 1,946 were randomly selected, 1,399 were confirmed as eligible, 960 were contacted for recruitment, and 662 provided verbal and written consent for the study participation. Questionnaires were completed through the mailing and phone interview; medical records were abstracted from CIBMTR to determine the type of initial diagnosis, type of HSCT, and the nature of donor relationship and other clinical variables.
Study Measures
HRQOL outcomes
HRQOL outcome were measured by two component scales (Physical Component Summary (PCS) and Mental Component Summary (MCS)) of the Medical Outcomes Study 36-item Short Form Health Survey (MOS SF-36) (29). The MOS SF-36 measures generic HRQOL of 8 domains: physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, energy/vitality, social functioning, role limitations due to emotional problems, and mental health. PCS summarizes physical aspects of HRQOL including physical functioning, role limitations due to physical health problems, bodily pain, and general health perceptions; MCS summarizes mental aspects of HRQOL including role limitations due to emotional health problems, social functioning, energy/vitality, and mental health. In this study, the latent constructs of physical HRQOL and mental HRQOL were measured by the scores of each domain within the PCS and MCS, respectively (29) with higher scores indicating better HRQOL.
Physical symptoms
Physical symptoms related to HSCT were measured using a refined version of the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) (30). The refined scale is comprised of a subset of 13 items capturing long-term symptoms related to HSCT based on classical test theory (31) and item response theory (32). Higher scores indicate more physical symptoms. The 13 items measure a unidimensional latent construct of physical symptoms including items such as “have trouble with my bowels”, “trouble concentrating”, and “bothered by a change in the way food tastes”.
Depressive symptoms
Depressive symptoms were assessed using the Center for Epidemiologic Studies-Depression (CES-D) (33). The CES-D scale has 20 items measuring four domains: depressed affect, somatic complaints, interpersonal difficulties, and low positive affect. Respondents are asked to indicate how often the depressive symptoms are experienced in the past week based on a 4-point Likert scale. Domain scores were calculated by summing the item responses within each domain. Higher domain scores indicate more depressive symptoms.
Psychosocial variables
The Life Orientation Test (LOT) is a 12-item unidimensional scale measuring an individual's disposition to generalized optimism (34). Respondents indicate agreement with the statement based on a Likert-type scale of 5 response categories. Higher scores indicate greater optimism.
The Social Constraints Scale (SCS) is a 16-item unidimensional scale measuring the degree to which individuals feel their social relationships are strained and the degree to which they feel constrained in discussing their trauma-related thoughts at the time of the survey (18). Social constraints is distinct from the concept of social support in that it focuses on the presence of individuals causing negative interactions (criticism, minimization, avoidance), independent of the people who provide support (19). Higher scores indicate more social constraint.
The Brief COPE is a 28-item scale capturing the concept of coping strategies in stressful situations (35): 1) active coping, 2) planning, 3) using instrumental support, 4) using emotional support, 5) venting, 6) behavioral disengagement, 7) self-distraction, 8) self-blame, 9) positive reframing, 10) humor, 11) denial, 12) acceptance, 13) religion, and 14) substance use. Items are scored on 4-point Likert scale. Following recommendations of the developer (35), empirical studies (36, 37), and our exploratory factor analysis (EFA), the domains of problem-focused/approach coping (7 items) and avoidant/maladaptive coping (7 items) were generated and included in this study.
Covariates
Important demographic and clinical variables suggested by the literature were included in the analyses. Demographic variables are current age, gender, occupational status, education, and marital status (12, 13, 38, 39) and clinical variables include time since HSCT (unit: years), severity of treatment experience, and comorbidities (12, 13, 38). Severity of treatment experience was defined as low severity for autologous and no chronic graft-versus-host-disease (cGVHD); moderate severity for allogeneic and no cGVHD; high severity for allogeneic and cGVHD. The presence of comorbidities at the time of the survey was dichotomized by yes/no.
Analytic Strategy
We used structural equation modeling (SEM) to evaluate the direct and indirect effects (or pathways) among variables of interests (40). Direct effects are the direct relationships between the variables. Indirect effects are the effects of one variable on another through mediating variables. A total effect is the sum of the direct and indirect effects. SEM is comprised of measurement and structural components (40, 41). The measurement component represents the relationship between measured indicators (i.e., items for unidimensional scales and domain scores for multidimensional scales; see below) and the corresponding latent constructs/latent variables the scales intend to measure. The structural component represents the relationships among different latent variables which are displayed by circles in all Figures. The covariates (demographic and clinical variables) are observed variables hypothesized to confound the associations among the variables of interests. We treated unidimensional scales (the modified FACT-BMT scale, LOT, SCS, and problem-focused and avoidant coping domains) as latent constructs and individual items of the corresponding scales as measured indicators. We treated multidimensional scales (CES-D, PCS and MCS) as latent constructs and used specific domain scores of the corresponding scales as measured indicators.
Modification indices (MI), overall model fit indices (i.e., confirmatory fit index (CFI) and root mean square error of approximation (RMSEA)) were used to guide the improvement of measurement models (42, 43). MIs are the predicted decrease in the chi-square (χ 2) value after freely estimating the relationship between two variables. Starting with the largest MI, measured indicators capturing the same latent construct were allowed to be freely estimated. For overall model fit indices, a CFI value ≥0.95 is preferred and ≥0.90 is deemed acceptable (42, 43) and a RMSEA ≤0.05 indicates close fit and ≤0.08 indicates fair fit (44). Mplus version 7 (45) was used with the mean- and variance-adjusted weight least squares (WLSMV) robust estimator (46).
Aim 1
The relationships among physical symptoms, depressive symptoms, and physical (Figure 1A) and mental (Figure 1B) HRQOL were evaluated separately based on the structural component of the SEM. Model fit was evaluated based on χ2 statistic, CFI and RMSEA. Direct, indirect, and total effects in Figures 1A and 1B were assessed using the INDIRECT command in Mplus. Unstandardized (b) and standardized (b) path estimates were estimated for each latent variable. The estimates were standardized using the variances of the continuous latent variables and outcome variables (physical HRQOL and mental HRQOL). All analyses were adjusted for covariates: age at survey, gender, race, marital status, education, occupational status, years since HSCT, and severity of treatment experience.
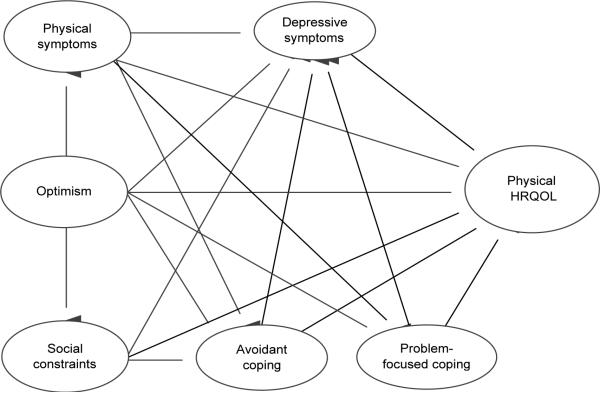
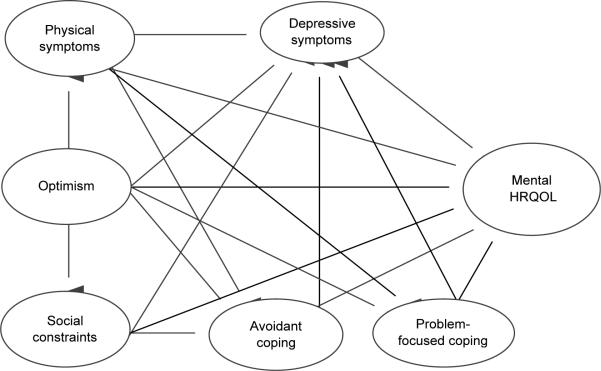
Figure 1.
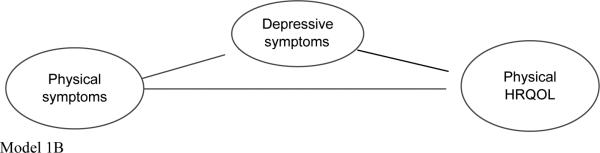
A) Physical HRQOL B) Mental HRQOL symptom pathway. Significant direct effects; Non-significant direct effects; *p <0.05, **p<0.01, ***p<0.001.
Aim 2
The pathways depicting the hypothesized associations among physical and depressive symptoms, optimism, social constraints, problem-focused and avoidant coping, and physical and mental HRQOL were tested in the full conceptual models (i.e., baseline models). The direct and indirect effects in the baseline models were tested separately for physical (Figure 2A) and mental HRQOL (Figure 3A). Iteratively, relationships between symptoms, psychosocial variables, and HRQOL were constrained to zero (i.e., coefficients constrained to zero) in the subsequent models (i.e., the reduced models) (Figure 2B for physical HRQOL and Figure 3B for mental HRQOL) if the relationships were not statistically significant in the baseline models. The order of constraining insignificant relationships was based on the magnitude of association and less theoretical importance. The DIFFTEST procedure was used to determine if the constrained model was significantly worse from the baseline models using a χ 2 test (46). The DIFFTEST procedure is a χ 2 difference test that determines whether the nested (or more restrictive model) has worse fitting-function (p<0.05) and fewer parameters than the full model. A p-value >0.05 indicates that the more restrictive model is a significantly better fit and that no additional relationships need to be constrained.
Figure 2.
Physical HRQOL Model 2A) Full Model 2B) Reduced Model. Significant direct effects; Non-significant direct effects; *p <0.05, **p<0.01, ***p<0.001.
Figure 3.
Mental HRQOL Model 3A) Full Model 3B) Reduced Model. Significant direct effects; Non-significant direct effects; *p <0.05, **p<0.01, ***p<0.001.
The model INDIRECT command in Mplus was used to obtain direct, indirect, and total effect information for the pathways between symptoms, psychosocial variables, and HRQOL. All models were adjusted for age at survey, gender, race, marital status, education, occupational status, time HSCT, and severity of treatment experience.
Results
Study Sample Characteristics
The mean age of participants was 42 years old (SD=11), the majority of the sample was White (92%) and over half was female (62%) (Table 1). One-third of the sample (32%) reported some college or technical education and another 30% reported a high school education or less. The mean number of years since HSCT was 7 years with a range of 2 to 22 years. The majority of the participants had low severity of treatment experience (60%) and a less intense previous treatment (66%). Among the participants, 16% reported the presence of comorbid conditions at the time of the survey. Due to missing data on covariates, 45 (6.8%) cases were excluded, leaving a sample of 617 observations for the analyses.
Table 1.
Study Characteristics
| N | % | |
|---|---|---|
| Demographics | ||
| Age, years | 662 | |
| Mean (SD) | 42.1 (11) | |
| Median (Range) | 42.4(18-71) | |
| <35 | 182 | 28 |
| 35-39 | 95 | 14 |
| 40-44 | 106 | 16 |
| 45-49 | 120 | 18 |
| >50 | 159 | 24 |
| Sex | ||
| Male | 251 | 38 |
| Female | 411 | 62 |
| Race | ||
| White | 603 | 92 |
| Other | 56 | 8 |
| Education | 658 | |
| High school or below | 194 | 30 |
| Some college/technical education | 209 | 32 |
| College degree | 122 | 18 |
| > College degree | 133 | 20 |
| Marital status | 659 | |
| Married/living with partner/committed | 483 | 73 |
| Other | 176 | 27 |
| Occupational status | ||
| Working or student | 484 | 73 |
| Not working | 100 | 15 |
| Retired | 75 | 11 |
| Annual family income | ||
| < $20,000 | 70 | 11 |
| $20,000 - $40,000 | 141 | 22 |
| $40,000 - $60,000 | 156 | 24 |
| $60,000 - $80,000 | 100 | 15 |
| >$80,000 | 181 | 28 |
| Clinical variables | ||
| Years since diagnosis | ||
| Mean (SD) | 662 | 7.0 (3.1) |
| Median (Range) | 6.6(1.8-22) | |
| Severity of treatment | ||
| Low- autologous no GVHD | 390 | 60 |
| Moderate-allogeneic no GVHD | 168 | 26 |
| High – allogeneic GVHD | 88 | 14 |
| Presence of comorbid conditions at survey | 104 | 16 |
| PROs | ||
| Modified FACT-BMT† score(observed) | ||
| Mean (SD) | 658 | 37.4 (4.7) |
| Median (Range) | 21(13-39) | |
| MOS-SF 36‡ Physical Component Summary(PCS) | ||
| Mean (SD) | 658 | 44.5 (11.6) |
| Median (Range) | 48(6.4-64.5) | |
| MOS-SF 36 Mental component summary (MCS) | ||
| Mean (SD) | 658 | 50.6 (10.4) |
| Median (Range) | 54(10.1-70.2) |
Bivariate Correlations
In the bivariate associations, physical symptoms were strongly correlated with depressive symptoms (r=0.85), physical HRQOL (r=−0.79), and mental HRQOL (r=−0.89) (Table 2). Depressive symptoms were strongly correlated with mental HRQOL (r=−0.97), avoidant coping (r=0.61), optimism (r=−0.74), and physical HRQOL (r=−0.65). Additionally, optimism was strongly correlated with mental HRQOL (r=0.66). The remaining pair-wise correlations among latent variables were moderate (0.4 < r < 0.6) or small (r<0.4) in magnitude.
Table 2.
Bivariate correlations between latent variables of interests
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Physical HRQOL† | 1.00 | ||||||
| 2. Mental HRQOL† | 0.83*** | 1.00 | |||||
| 3. Depressive symptoms‡ | −0.65*** | −0.97*** | 1.00 | ||||
| 4. Physical symptoms‡ | −0.79*** | −0.89*** | 0.85*** | 1.00 | |||
| 5. Avoidant coping‡ | −0.33*** | 0.50*** | −0.61*** | 0.55*** | 1.00 | ||
| 6. Problem-focused coping† | 0.14** | 0.19*** | −0.22*** | −0.22*** | −0.32*** | 1.00 | |
| 7. Social constraints‡ | −0.42*** | −0.49*** | 0.53*** | 0.52*** | 0.44*** | −0.02 | 1.00 |
| 8. Optimism† | 0.39*** | 0.66*** | −0.74*** | −0.35*** | 0.55*** | 0.39*** | −0.40*** |
Latent variable is positively scored so higher scores mean better health
negatively scored with higher scores meaning worse health.
* p<0.05
p<0.01
p<0.001
The Depressive Symptom Mediation Model
Symptom-physical HRQOL pathways
Figure 1A shows the associations between physical symptoms, depressive symptoms, and physical HRQOL. The direct effect indicates that an increase in physical symptoms by 1 SD was significantly associated with a decrease in physical HRQOL by 0.98 SD and an increase in depressive symptoms by 0.94 SD (b=0.94). However, the indirect effect of physical symptoms on physical HRQOL through depressive symptoms was not statistically significant (b=0.21) (Table 3).
Table 3.
| Physical HRQOL^ | Mental HRQOL^ | |||
|---|---|---|---|---|
| Unstandardized b | STDYX b | Unstandardized b | STDYX b | |
| Physical symptoms → HRQOL | −25.33*** | −0.98 | −4.28*** | −0.26 |
| Specific indirect effects | ||||
| Physical symptoms → depressive symptoms → HRQOL | 5.52 | 0.21 | −10.10*** | −0.62 |
| Total indirect effects | 5.52 | 0.21 | 14.38*** | 0.62 |
| Total effects | −19.81*** | −0.77 | −10.10*** | −0.88 |
| Model Fit | CFI/TLI | RMSEA | CFI/TLI | RMSEA |
| 0.92/0.91 | 0.04 | 0.91/0.90 | 0.05 | |
Latent variable is negatively scored with higher scores meaning worse symptoms
positively scored so higher scores mean better
Adjusted for age at survey, gender, race, marital status, education, occupational status, severity of treatment experience, years since HSCT
*p<0.05
**p<0.01
p<0.001
#p <0.1
Symptom-mental HRQOL pathways
Figure 1B shows the associations between physical symptoms, depressive symptoms, and mental HRQOL. The direct effect indicates that an increase in physical symptoms by 1 SD was significantly associated with a decrease in mental HRQOL by 0.26 SD (b=−0.26) and an increase in depressive symptoms by 0.86 SD (b=0.86). Additionally, greater depressive symptoms were significantly associated with poorer mental HRQOL (b=−0.72). The indirect effect indicates that an increase in physical symptoms by 1 SD was significantly associated with a decrease in mental HRQOL by 0.62 SD through decreasing depressive symptoms (b=−0.62) (Table 3).
The Comprehensive Conceptual Model
Pathways to physical HRQOL
The baseline physical HRQOL model in Figure 2A demonstrates an adequate model fit of the data (CFI=0.95, RMSEA=0.03) despite several insignificant pathways. The increase in physical symptoms was significantly associated with a decrease in physical HRQOL (b= −0.72). For indirect effects, optimism increased physical HRQOL through physical symptoms significantly (b=0.40) while pathways stemming from physical symptoms, avoidant and problem-focused coping on physical HRQOL were not statistically significant (Table 3). The DIFFTEST procedure indicated that the final reduced model (Figure 2B) was more parsimonious compared to the full model (p-value >0.05; χ 2 (7) =10.04, p=0.19) (Table 5). In the reduced model, both physical symptoms and optimism had significant direct effects on physical HRQOL (b=−0.79 and b=−0.15, respectively) (Figure 2B). Although optimism was negatively associated with physical HRQOL in the reduced model, the indirect effect of optimism through physical symptoms on physical HRQOL was positive and statistically significant (b=0.45) (Table 5).
Table 5.
Reduced model for the effects^ of physical symptoms (PHY)†, depressive symptoms (DEP)†, optimism (OPT)‡, SOC (SOC)†, avoidant coping (AC) and problem-focused coping (PFC) on HRQOL‡
| Physical HRQOL^ | Mental HRQOL^ | |||
|---|---|---|---|---|
| Unstandardized b | STDYX b | Unstandardized b | STDYX b | |
| Path from physical symptoms: Indirect effects | ||||
| PHY → DEP → HRQOL | −5.70** | −0.49 | ||
| PHY → AC → HRQOL | 0.38# | 0.03 | ||
| Total indirect effects | −5.32*** | −0.46 | ||
| Total Effects | −8.35*** | −0.72 | ||
| Path from optimism: Indirect effects | ||||
| OPT → DEP → HRQOL | 3.40*** | 0.22 | ||
| OPT → AC → HRQOL | −0.46* | −0.03 | ||
| OPT → PHY → HRQOL | 7.49*** | 0.45 | 2.19** | 0.14 |
| OPT → SOC → DEP → HRQOL | 0.36** | 0.02 | ||
| OPT → PHY → DEP → HRQOL | 4.12*** | 0.27 | ||
| OPT → SOC → AC → HRQOL | −0.09# | −0.01 | ||
| OPT → PHY → AC → HRQOL | −0.27# | −0.02 | ||
| Total indirect effects | 7.49*** | 0.45 | 9.23*** | 0.61 |
| Total effects | 4.99*** | 0.30 | 9.23*** | 0.61 |
| Path from social constraints: Indirect effects | ||||
| SOC → DEP → HRQOL | −0.93** | −0.07 | ||
| SOC → AC → HRQOL | 0.24# | 0.02 | ||
| Total indirect effects | −0.70* | −0.05 | ||
| Total effects | −0.70* | −0.05 | ||
| Total direct effects on HRQOLa | −12.39 | −0.94 | −21.52 | −0.92 |
| Model Fit | CFI/TLI | RMSEA | CFI/TLI | RMSEA |
| 0.95/0.95 | 0.03 | 0.94/0.94 | 0.03 | |
| DIFFTEST | X2 (df) | p-value | X2(df) | p-value |
| 10.04(7) | 0.19 | 7.12(6) | 0.31 | |
Latent variable is negatively scored with higher scores meaning worse symptoms
positively scored so higher scores mean better
adjusted for age at survey, gender, race, marital status, education, occupational status, severity of treatment experience, years since HSCT
p<0.05
p<0.01
p<0.001
p <0.1.
Pathways to mental HRQOL
The baseline mental HRQOL model in Figure 3A demonstrates an adequate model fit of the data (CFI=0.94, RMSEA=0.03). For the direct effects, greater physical symptoms (b=−0.23), depressive symptoms (b=−0.85), and avoidant coping (b=0.13) were directly and significantly associated with poorer mental HRQOL, respectively. For indirect effects in the baseline model, several significant pathways from optimism to mental HRQOL were identified, including the pathway of optimism-social constraints-depressive symptoms-mental HRQOL and the pathway of optimism-avoidant coping-mental HRQOL). Depressive symptoms and avoidant coping typically acted as mediators in several significant pathways from optimism and physical symptoms to mental HRQOL (Table 4). However, some insignificant pathways were identified including physical symptoms to problem-focused coping; both avoidant coping and problem-focused coping to depressive symptoms; and optimism to mental HRQOL. After removing the insignificant relationships, the DIFFTEST procedure indicated that the reduced model was more parsimonious than the full model with a p-value >0.05 (χ 2(6) =7.12, p=0.31) (Table 5). For the direct effects in the reduced model, the magnitudes of the coefficients representing the increase in physical symptoms and avoidant coping associated with a decrease in mental HRQOL were small (b=−0.26 and b=0.10, respectively) while the increase in depressive symptoms associated with a decrease in mental HRQOL was large (b=−0.76) (Figure 3B). The effect of optimism on mental HRQOL through physical symptoms, depressive symptoms and avoidant coping remained statistically significant in the reduced model. Avoidant coping and physical symptoms were significant mediators in the reduced model (i.e., optimism to mental HRQOL through avoidant coping and optimism to mental HRQOL through physical symptoms); however the magnitudes of these indirect effects were small. In contrast, depressive symptoms were a significant mediator in five pathways with indirect effects on mental HRQOL that were moderate or strong. For example, the indirect effect of physical symptoms to mental HRQOL through depressive symptoms was −0.491 and the indirect effects from optimism to mental HRQOL through depressive symptoms was 0.22(Table 5).
Table 4.
Baseline model for the effects^ of physical symptoms (PHY)†, depressive symptoms (DEP)†, optimism (OPT)‡, social constraints (SOC)†, avoidant coping (AC) and problem-focused coping (PFC) on HRQOL‡
| Physical HRQOL^ | Mental HRQOL^ | |||
|---|---|---|---|---|
| Unstandardized b | STDYX b | Unstandardized b | STDYX b | |
| Path from physical symptoms: Indirect effects | ||||
| PHY → DEP→ HRQOL | −0.44 | −0.04 | −6.05*** | −0.52 |
| PHY → AC → HRQOL | 0.28 | 0.02 | 0.42* | 0.04 |
| PHY → PFC→ HRQOL | −0.01 | −0.001 | 0.01 | 0.001 |
| PHY → AC → DEP→ HRQOL | −0.02 | −0.001 | −0.24# | −0.02 |
| PHY → PFC→ DEP → HRQOL | 0.003 | 0.000 | 0.04 | 0.003 |
| Total indirect effects | −0.19 | −0.02 | −5.83*** | −0.50 |
| Total effects | −9.32*** | −0.74 | −8.50*** | −0.73 |
| Path from coping: Indirect effects | ||||
| AC → DEP → HRQOL | −0.14 | −0.01 | −1.81 | −0.07 |
| Total effects | 2.14 | 0.08 | 1.32 | 0.05 |
| Total direct | 2.28 | 0.08 | 3.11 | 0.13 |
| PFC → DEP → HRQOL | −0.11 | −0.003 | −1.00 | −0.04 |
| Total effects | 0.26 | 0.01 | −1.25 | −0.05 |
| 0.36 | 0.01 | −0.25 | −0.01 | |
| Path from optimism: Indirect effects | ||||
| OPT → DEP → HRQOL | 0.33 | 0.02 | 3.76*** | 0.25 |
| OPT → AC → HRQOL | −0.46 | −0.03 | −0.59** | −0.04 |
| OPT → PFC → HRQOL | 0.08 | 0.01 | −0.05 | −0.003 |
| OPT → SOC → HRQOL | 0.34 | 0.02 | −0.18 | −0.01 |
| OPT → PHY → HRQOL | 6.69*** | 0.40 | 1.90*** | 0.01 |
| OPT → AC → DEP → HRQOL | 0.03 | 0.002 | 0.34 | 0.02 |
| OPT → PFC → DEP → HRQOL | −0.02 | −0.001 | −0.21 | −0.01 |
| OPT → SOC → DEP → HRQOL | 0.03 | 0.002 | 0.35* | 0.02 |
| OPT → PHY → DEP → HRQOL | 0.33 | 0.20 | 4.30*** | 0.28 |
| OPT → SOC→ AC → HRQOL | −0.09 | −0.01 | −0.12* | −0.01 |
| OPT→ SOC → PFC → HRQOL | −0.01 | −0.001 | 0.01 | 0.01 |
| OPT → PHY → AC → HRQOL | −0.20 | −0.01 | −0.30* | −0.02 |
| OPT → PHY → PFC → HRQOL | −0.01 | 0.001 | −0.01 | 0.000 |
| OPT → SOC → AC → DEP → HRQOL | 0.01 | 0.000 | 0.07 | 0.004 |
| OPT → SOC → PFC → DEP → HRQOL | 0.003 | 0.000 | 0.03 | 0.002 |
| OPT → PHY → AC → DEP → HRQOL | 0.01 | 0.001 | 0.17 | 0.01 |
| OPT → PHY → PFC → DEP → HRQOL | −0.003 | 0.000 | −0.03 | −0.002 |
| Total indirect effects | 7.05*** | 0.80 | 9.27*** | 0.62 |
| Total effects | 4.96*** | 0.30 | 9.45*** | 0.61 |
| Path from social constraints: Indirect effects | ||||
| SOC → DEP → HRQOL | −0.07 | −0.01 | −0.91* | −0.06 |
| SOC → AC → HRQOL | 0.22 | 0.014 | 0.30* | 0.02 |
| SOC → PFC → HRQOL | 0.03 | 0.002 | −0.02 | −0.001 |
| SOC → AC → DEP → HRQOL | −0.01 | −0.001 | −0.18 | −0.01 |
| SOC → PFC → DEP → HRQOL | −0.01 | −0.001 | −0.08 | −0.01 |
| Total indirect effects | 0.16 | 0.01 | −0.88* | −0.06 |
| Total effects | −0.69 | −0.04 | −0.42 | −0.03 |
| Total direct effects on HRQOLa | −12.06 | −1.14 | −23.12 | −1.00 |
| Model Fit | CFI/TLI | RMSEA | CFI/TLI | RMSEA |
| 0.95/0.95 | 0.03 | 0.94/0.94 | 0.03 | |
Latent variable is negatively scored with higher scores meaning worse symptoms
positively scored so higher scores mean better
adjusted for age at survey, gender, race, marital status, education, occupational status, severity of treatment experience, years since HSCT
p<0.05
p<0.01
p<0.001
p <0.1.
Discussion
This study examined the relationships among physical symptoms, depressive symptoms, psychosocial factors and HRQOL in long-term HSCT survivors using SEM technique while controlling for important demographic and clinical characteristics. Our results from Aim 1 found greater physical symptoms significantly decreased physical HRQOL of survivors more than depressive symptoms. In contrast, greater depressive symptoms decreased mental HRQOL in survivors more than physical symptoms. After adding psychosocial factors into the relationships between physical and mental symptoms and HRQOL our results found that physical symptoms remain the strongest factor directly contributing to physical HRQOL; depressive symptoms and physical symptoms remain the strongest factors directly contributing to mental HRQOL. Depressive symptoms and avoidant coping played the role of significant mediators in the pathways stemming from physical symptoms, optimism and social constraints to mental HRQOL.
The findings that physical symptoms had the strongest direct effect on physical HRQOL compared to depressive symptoms, even accounting for the mediation effect of psychosocial variables, are consistent with previous studies (10, 47). Although optimism was the only psychosocial variable significantly associated with physical HRQOL, the negative association with physical HRQOL in the path analysis was inversed from the bivariate analysis. This finding is in contrast to previous studies (14, 15); one of which examined the relationships of pre-HSCT optimism and physical well-being one year after HSCT without a measure of physical symptoms (14). We replicated the approach in the previous study (14) and found that analyzing physical HRQOL and optimism without the physical symptom measure resulted in a positive relationship. Our findings imply that the majority of influence of optimism is through the perception of physical symptoms (e.g. higher optimism may lead to lower perception of physical symptoms) resulting in higher physical HRQOL. One study found that an optimistic perspective prior to transplantation was associated with higher HRQOL in HSCT post-transplant recipients (17). Acknowledgement of the “mind-body connection” in survivorship care may be important in providing comprehensive care (48). Overall, addressing physical symptoms through pharmacologic or non-pharmacologic approaches (i.e. exercise programs, sleep therapy) (49) might be the most direct strategy to improve physical HRQOL in long-term survivors.
In the pathways toward mental HRQOL, the significant relationship between depressive symptoms and mental HRQOL are supported by previous studies (23, 50). Although optimism was not significantly directly associated with mental HRQOL, the increase in mental HRQOL from optimism through decreases in physical symptoms, depressive symptoms, and avoidant coping contributes to the extant literature that relies on the regression models to examine the association between optimism and mental HRQOL (51, 52). Particularly, our study provides new insight into the mechanisms (e.g., social constraints-depressive symptoms pathway) through which optimism has a positive influence on mental HRQOL. That is, optimism, physical symptoms, depressive symptoms, and avoidant coping may be important factors to intervene upon to improve mental HRQOL of HSCT survivors. Interventions targeting both psychological symptoms and psychosocial issues include psycho-educational interventions, cognitive-behavioral therapy, support groups, and complementary and alternative medicine (53-55). Cognitive-behavioral therapy has demonstrated the effectiveness in addressing issues related to avoidant coping strategies and depressive symptoms which indirectly and directly influence mental HRQOL (53).
The relationships of social constraints and coping strategies with symptoms and physical and mental HRQOL are complex. The positive association between greater social constraints and increased avoidant coping echoes some evidence for the social support deterioration model suggesting that experiencing a constant stressor over time (i.e. presence of physical symptoms) may decrease the perception of social support (56), leading to poor coping strategies such as cognitive avoidance (19). The significant relationship between avoidant coping with physical symptoms is consistent with the hypothesis that physical symptoms influence a survivor's ability to cope (6, 20). We did not identify a significant relationship between avoidant or problem-focused coping and depressive symptoms. This is consistent with evidence from some studies (57) but in contrast to other studies (58). However, these previous studies did not include coping, depressive symptoms and physical symptoms simultaneously. Overall, psychosocial factors played a larger role in mental HRQOL than physical HRQOL. Symptoms, social constraints or coping strategies are potentially useful for tailoring care or interventions for a survivor (53). For example, support group interventions may counteract social constraints, leading to improved coping strategies (53).
Limitations
Several limitations are present in this study. First, the composition of our sample is largely homogenous (92% White), limiting generalizability to other racial or ethnic groups. Second, the use of cross-sectional data prevents the estimation of causal relationship between variables of interests. Our findings must be interpreted as associations rather than causal relationships. Third, there are other possible contributing factors such as cognitive functioning, self-efficacy, self-esteem and health behaviors that were not addressed (9, 14, 59). Finally, we proposed pathways that are theoretically sound and testable per the availability of the dataset. Several other plausible pathways with differences in directionality of the relationships exist.
Conclusion
Developing a robust conceptual model is important to evaluate the complex factors influencing HRQOL in survivorship research. While the impact of physical and depressive symptoms on physical and mental HRQOL, respectively, was evident, the relationships were not straightforward. We found psychosocial factors did not play a significant role with physical HRQOL. In contrast, psychosocial variables were associated with mental HRQOL, specifically through their relationship with depressive symptoms. Interventions targeting physical or depressive symptoms may benefit from addressing a survivors’ optimism, coping strategies and social resources to create an effective health care strategy.
Acknowledgments
Source of Funding:
This work was partially supported by the National Cancer Institute NCI R01 CA81320 07/1999-07/2003 (PI: Dr. John Wingard)
Abbreviations
- HSCT
hematopoietic stem cell transplant
- HRQOL
health-related quality of life
- PCS
Physical Component Summary
- MCS
Mental Component Summary
- CFI
Confirmatory fit index
- RMSEA
Root mean square error of approximation
Footnotes
Conflicts of Interest:
No conflicts of interest were declared.
Contributor Information
Kelly Kenzik, University of Alabama-Birmingham, School of Medicine.
I-Chan Huang, University of Florida, College of Medicine.
J. Douglas Rizzo, Center for International Blood and Marrow Transplant Research, Medical College of Wisconsin.
Elizabeth Shenkman, University of Florida, College of Medicine.
John Wingard, University of Florida, College of Medicine.
References
- 1.Jacobsen PB, Jim HSL. Consideration of Quality of Life in Cancer Survivorship Research. Cancer Epidem Biomar. 2011;20:2035–2041. doi: 10.1158/1055-9965.EPI-11-0563. [DOI] [PubMed] [Google Scholar]
- 2.Khera N, Storer B, Flowers MED, Carpenter PA, Inamoto Y, Sandmaier BM, Martin PJ, Lee SJ. Nonmalignant Late Effects and Compromised Functional Status in Survivors of Hematopoietic Cell Transplantation. J Clin Oncol. 2012;30:71–77. doi: 10.1200/JCO.2011.38.4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Syrjala KL, Martin PJ, Lee SJ. Delivering Care to Long-Term Adult Survivors of Hematopoietic Cell Transplantation. J Clin Oncol. 2012;30:3746–3751. doi: 10.1200/JCO.2012.42.3038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wingard JR. Functional ability and quality of life of patients after allogeneic bone marrow transplantation. Bone Marrow Transplant. 1994;14(Suppl 4):S29–33. [PubMed] [Google Scholar]
- 5.Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers ME, Martin PJ. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–2343. doi: 10.1001/jama.291.19.2335. [DOI] [PubMed] [Google Scholar]
- 6.Stein KD, Syrjala KL, Andrykowski MA. Physical and psychological long-term and late effects of cancer. Cancer. 2008;112:2577–2592. doi: 10.1002/cncr.23448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wingard JR, Huang I, Sobocinski KA, Andrykowski MA, Cella D, Rizzo JD, Brady M, Horowitz MM, Bishop MM. Factors Associated with Self-Reported Physical and Mental Health after Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant. 2010;16:1682–1692. doi: 10.1016/j.bbmt.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pidala J, Anasetti C, Jim H. Health-related quality of life following haematopoietic cell transplantation: patient education, evaluation and intervention. Br J Haematol. 2010;148:373–385. doi: 10.1111/j.1365-2141.2009.07992.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mosher CE, Lepore SJ, Wu L, Austin J, Valdimarsdottir H, Rowley S, Isola L, Redd WH, Rini C. Social Correlates of Distress Following Hematopoietic Stem Cell Transplantation: Exploring the Role of Loneliness and Cognitive Processing. J Health Psychol. 2012;17:1022–1032. doi: 10.1177/1359105311432490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bevans MF, Mitchell SA, Barrett AJ, Bishop M, Childs R, Fowler D, Krumlauf M, Prince P, Shelburne N, Wehrlen L. Function, adjustment, quality of life and symptoms (FAQS) in allogeneic hematopoietic stem cell transplantation (HSCT) survivors: a study protocol. Health Qual Life Outcomes. 2011;9:24. doi: 10.1186/1477-7525-9-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molassiotis A, Van Den Akker OB, Milligan DW, Goldman JM. Symptom distress, coping style and biological variables as predictors of survival after bone marrow transplantation. J Psychosom Res. 1997;42:275–285. doi: 10.1016/s0022-3999(96)00298-x. [DOI] [PubMed] [Google Scholar]
- 12.Mosher CE, Redd WH, Rini CM, Burkhalter JE, DuHamel KN. Physical, psychological, and social sequelae following hematopoietic stem cell transplantation: a review of the literature. Psychooncology. 2009;18:113–127. doi: 10.1002/pon.1399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Slovacek L, Slovackova B. Quality of life in oncological and hematooncological patients after hematopoietic stem cell transplantation: The effect of selected psychosocial and health aspects on quality of life: A review of the literature. Reports of Practical Oncology & Radiotherapy. 2007;12:53–59. [Google Scholar]
- 14.Hochhausen N, Altmaier EM, McQuellon R, Davies SM, Papadopolous E, Carter S, Henslee-Downey J. Social support, optimism, and self-efficacy predict physical and emotional well-being after bone marrow transplantation. J Psychosoc Oncol. 2007;25:87–101. doi: 10.1300/J077v25n01_05. [DOI] [PubMed] [Google Scholar]
- 15.Friedman LC, Kalidas M, Elledge R, Chang J, Romero C, Husain I, Dulay MF, Liscum KR. Optimism, social support and psychosocial functioning among women with breast cancer. Psychooncology. 2006;15:595–603. doi: 10.1002/pon.992. [DOI] [PubMed] [Google Scholar]
- 16.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67:1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 17.Lee SJ, Loberiza FR, Rizzo JD, Soiffer RJ, Antin JH, Weeks JC. Optimistic expectations and survival after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2003;9:389–396. doi: 10.1016/s1083-8791(03)00103-4. [DOI] [PubMed] [Google Scholar]
- 18.Lepore SJ, Silver RC, Wortman CB, Wayment HA. Social constraints, intrusive thoughts, and depressive symptoms among bereaved mothers. J Pers Soc Psychol. 1996;70:271–282. doi: 10.1037//0022-3514.70.2.271. [DOI] [PubMed] [Google Scholar]
- 19.Lepore S. In: A social-cognitive processing modelof emotional adjustment to cancer. Baum A, Andersen BL, editors. Vol. 12. American Psychological Association; Washington, D.C.: 2001. pp. 99–118. [Google Scholar]
- 20.Molassiotis A. A conceptual model of adaptation to illness and quality of life for cancer patients treated with bone marrow transplants. J Adv Nurs. 1997;26:572–579. doi: 10.1046/j.1365-2648.1997.t01-18-00999.x. [DOI] [PubMed] [Google Scholar]
- 21.Byar KL, Eilers JE, Nuss SL. Quality of life 5 or more years post-autologous hematopoietic stem cell transplant. Cancer Nurs. 2005;28:148–157. doi: 10.1097/00002820-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Wingard JR, Majhail NS, Brazauskas R, Wang Z, Sobocinski KA, Jacobsohn D, Sorror ML, Horowitz MM, Bolwell B, Rizzo JD, Socie G. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29:2230–2239. doi: 10.1200/JCO.2010.33.7212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mosher CE, DuHamel KN, Rini C, Corner G, Lam J, Redd WH. Quality of life concerns and depression among hematopoietic stem cell transplant survivors. Support Care Cancer. 2011;19:1357–1365. doi: 10.1007/s00520-010-0958-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rusiewicz A, DuHamel KN, Burkhalter J, Ostroff J, Winkel G, Scigliano E, Papadopoulos E, Moskowitz C, Redd W. Psychological distress in long-term survivors of hematopoietic stem cell transplantation. Psychooncology. 2008;17:329–337. doi: 10.1002/pon.1221. [DOI] [PubMed] [Google Scholar]
- 25.Schoulte JC, Lohnberg JA, Tallman B, Altmaier EM. Influence of coping style on symptom interference among adult recipients of hematopoietic stem cell transplantation. Oncol Nurs Forum. 2011;38:582–586. doi: 10.1188/11.ONF.582-586. [DOI] [PubMed] [Google Scholar]
- 26.Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ, Horowitz MM, Sobocinski KA, Rizzo JD, Wingard JR. Long-Term Health-Related Quality of Life, Growth, and Spiritual Well-Being After Hematopoietic Stem-Cell Transplantation. J Clin Oncol. 2005;23:599–608. doi: 10.1200/JCO.2005.03.189. [DOI] [PubMed] [Google Scholar]
- 27.Bishop MM, Lee SJ, Beaumont JL, Andrykowski MA, Rizzo JD, Sobocinski KA, Wingard JR. The Preventive Health Behaviors of Long-Term Survivors of Cancer and Hematopoietic Stem Cell Transplantation Compared with Matched Controls. Biol Blood Marrow Transplant. 2010;16:207–214. doi: 10.1016/j.bbmt.2009.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bishop MM, Beaumont JL, Hahn EA, Cella D, Andrykowski MA, Brady MJ, Horowitz MM, Sobocinski KA, Rizzo JD, Wingard JR. Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. J Clin Oncol. 2007;25:1403–1411. doi: 10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Jr., Sherbourne CD. The MOS 36-Item Short-Form Health Survey (SF-36): I. Conceptual Framework and Item Selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 30.McQuellon RP, Russell GB, Cella DF, Craven BL, Brady M, Bonomi A, Hurd DD. Quality of life measurement in bone marrow transplantation: development of the Functional Assessment of Cancer Therapy-Bone Marrow Transplant (FACT-BMT) scale. Bone Marrow Transplant. 1997;19:357–368. doi: 10.1038/sj.bmt.1700672. [DOI] [PubMed] [Google Scholar]
- 31.Huang I, Bishop M, Rizzo D, Andrykowski MA, Wingard JR. Development of the Functional Assessment of Cancer Therapy-Bone Marrow Transplant Survivor (FACT-BMTS) scale. Abstract 1738. Qual Life Res. 2009:A–43-A-44. [Google Scholar]
- 32.Kenzik KM. Patient-Reported Outcomes in Hematopoietic Stem Cell Transplant Survivors. University of Florida; 2013. unpublished doctoral dissertation. [Google Scholar]
- 33.Radloff LS. The CES-D Scale. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 34.Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. Health Psychol. 1985;4:219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- 35.Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 36.Krageloh CU. A systematic review of studies using the Brief COPE: Religious Coping in Factor Analyses. Religions. 2011;2:216–246. [Google Scholar]
- 37.Moore BC, Biegel DE, McMahon TJ. Maladaptive Coping as a Mediator of Family Stress. J Soc Work Pract Addict. 2011;11:17–39. doi: 10.1080/1533256X.2011.544600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pidala J, Anasetti C, Jim H. Quality of life after allogeneic hematopoietic cell transplantation. Blood. 2009;114:7–19. doi: 10.1182/blood-2008-10-182592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maurice-Stam H, Oort FJ, Last BF, Grootenhuis MA. A predictive model of health-related quality of life in young adult survivors of childhood cancer. Eur J Cancer Care (Engl) 2009;18:339–349. doi: 10.1111/j.1365-2354.2007.00916.x. [DOI] [PubMed] [Google Scholar]
- 40.Kline RB. Third ed. Guilford Publications; New York, NY: 2011. Principles and Practice of Structural Equation Modeling. [Google Scholar]
- 41.Ullman JB, Bentler PM. Structural Equation Modeling. John Wiley & Sons, Inc.; New York: 2003. pp. 607–634. Anonymous. [Google Scholar]
- 42.Bentler P. Comparative Fit Indices in Structural Models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 43.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. [Google Scholar]
- 44.Browne MW, Cudeck R. Alternative Ways of Assessing Model Fit. Sociol Method Res. 1992;21:230–258. [Google Scholar]
- 45.Muthen B, Muthen LK. Mplus Version 7.1. 2012:7. [Google Scholar]
- 46.Muthen LK, Muthen B. Statistical analysis with latent variables. User's guide. Mplus. 1998-2012:7. [Google Scholar]
- 47.Kav S, Aslan O, Tekin F, Yesil H, Meral C, Ozturk U, Bulut Z, Enaboifo A, Yazar B. Quality of life and difficulties of patients encountered after autologous stem cell transplantation. J BUON. 2009;14:673–680. [PubMed] [Google Scholar]
- 48.Ray O. How the mind hurts and heals the body. Am Psychol. 2004;59:29–40. doi: 10.1037/0003-066X.59.1.29. [DOI] [PubMed] [Google Scholar]
- 49.Wanchai A, Armer JM, Stewart BR. Nonpharmacologic supportive strategies to promote quality of life in patients experiencing cancer-related fatigue: a systematic review. Clin J Oncol Nurs. 2011;15:203–214. doi: 10.1188/11.CJON.203-214. [DOI] [PubMed] [Google Scholar]
- 50.Braamse AM, Gerrits MM, van Meijel B, Visser O, van Oppen P, Boenink AD, Cuijpers P, Huijgens PC, Beekman AT, Dekker J. Predictors of health-related quality of life in patients treated with auto-and allo-SCT for hematological malignancies. Bone Marrow Transplant. 2012;47:757–769. doi: 10.1038/bmt.2011.130. [DOI] [PubMed] [Google Scholar]
- 51.Helgeson VS, Snyder P, Seltman H. Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol. 2004;23:3–15. doi: 10.1037/0278-6133.23.1.3. [DOI] [PubMed] [Google Scholar]
- 52.Carver CS, Smith RG, Antoni MH, Petronis VM, Weiss S, Derhagopian RP. Optimistic personality and psychosocial well-being during treatment predict psychosocial well-being among long-term survivors of breast cancer. Health Psychol. 2005;24:508–516. doi: 10.1037/0278-6133.24.5.508. [DOI] [PubMed] [Google Scholar]
- 53.Stanton AL. Psychosocial Concerns and Interventions for Cancer Survivors. J Clin Oncol. 2006;24:5132–5137. doi: 10.1200/JCO.2006.06.8775. [DOI] [PubMed] [Google Scholar]
- 54.Schou BI, Karesen R, Smeby NA, Espe R, Sorensen EM, Amundsen M, Aas H, Ekeberg O. Effects of a Psychoeducational Versus a Support Group Intervention in Patients With Early-Stage Breast Cancer: Results of a Randomized Controlled Trial. Cancer Nurs. 2013 doi: 10.1097/NCC.0b013e31829879a3. [DOI] [PubMed] [Google Scholar]
- 55.Matsuda A, Yamaoka K, Tango T, Matsuda T, Nishimoto H. Effectiveness of psychoeducational support on quality of life in early-stage breast cancer patients: a systematic review and meta-analysis of randomized controlled trials. Qual Life Res. 2014;23:21–30. doi: 10.1007/s11136-013-0460-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Norris FH, Kaniasty K. Received and perceived social support in times of stress: A test of the social support deterioration deterrence model. J Pers Soc Psychol. 1996;71:498–511. doi: 10.1037//0022-3514.71.3.498. [DOI] [PubMed] [Google Scholar]
- 57.Wells KJ, Booth-Jones M, Jacobsen PB. Do coping and social support predict depression and anxiety in patients undergoing hematopoietic stem cell transplantation?. J Psychosoc Oncol. 2009;27:297–315. doi: 10.1080/07347330902978947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fife BL, Huster GA, Cornetta KG, Kennedy VN, Akard LP, Broun ER. Longitudinal Study of Adaptation to the Stress of Bone Marrow Transplantation. J Clin Oncol. 2000;18:1539–1549. doi: 10.1200/JCO.2000.18.7.1539. [DOI] [PubMed] [Google Scholar]
- 59.Wu LM, Austin J, Hamilton JG, Valdimarsdottir H, Isola L, Rowley S, Warbet R, Winkel G, Redd WH, Rini C. Self-efficacy beliefs mediate the relationship between subjective cognitive functioning and physical and mental well-being after hematopoietic stem cell transplant. Psychooncology. 2012;21:1175–1184. doi: 10.1002/pon.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]