Abstract
Background
Although fear of falling is prevalent among older adults recovering from hip fracture, current instruments are inadequate due to focus on specific situations and measurement of self-efficacy rather than fear.
Methods
The authors revised and tested a form of the Fear of Falling Questionnaire with three groups of older adults: 405 recovering from hip fracture, 89 healthy community-dwelling, and 42 with severe fear of falling. Test-retest reliability was evaluated in a subsample of 16 hip fracture patients. Internal consistency was compared across all groups Construct validity was established through factor analysis, convergent validity with a measure of fall-related self-efficacy, and discriminant validity with measures of depression and affect.
Results
A revised two-factor, 6-item scale appears to have adequate psychometric properties. Scores were lower among the healthy comparison group relative to the hip fracture and fear of falling groups. Cronbach’s alphas ranged from .72–.83, with test-retest reliability of .82. Correlations with a measure of fall-related self-efficacy were moderate for the hip fracture group (.42) and high with the healthy comparison (.68) and fear of falling (.70) groups. Correlations with depression, negative, and positive affect were low to moderate.
Conclusions
The Fear of Falling Questionnaire - Revised shows promise as a self-report measure of fear of falling, and is one of the first to be tested in older adults recovering from hip fracture. Advantages are that it is global rather than situation-specific and measures fear rather than self-efficacy. Future research on this scale is recommended in other older adult samples for whom fear of falling is relevant.
Keywords: fear of falling, assessment, hip fracture, questionnaire
Introduction
Approximately one-third of community-dwelling adults over 65 years old experience at least one fall every year (Campbell et al., 1981; Stevens et al., 2008), and falls are the leading cause of injury-related hospitalization in older adults (Alexander et al., 1992). Hip fractures are one of the most serious injuries related to falls in older adults, often leading to permanent disability and death (Marottoli et al., 1992). Older adults recovering from a hip fracture are at increased risk of falling (Sherrington and Lord, 1998). Of those who fall, as many as 48% report having a fear of falling again (Tinetti et al., 1988). Although there is a lack of published research on the prevalence of fear of falling in hip fracture patients, one study found that 63% reported at least some degree of fear of falling (Visschedijk et al., 2013). Thus, fear of falling is particularly relevant to older adults recovering from a hip fracture.
Fear of falling predicts future falls and is associated with restriction in activity, decreased life satisfaction, and frailty (Arfken et al., 1994; Friedman et al., 2002). Furthermore, prevalence of fear of falling increases with age (Arfken et al., 1994). Accurate assessment of fear of falling in older adults is essential to identify those who may be at greater risk for falling, and to develop interventions that will effectively treat fear of falling. However, available assessments for fear of falling may be too complex for older adults recovering from hip fracture and there is a lack of evidence for their psychometric performance in this high-risk group (Visschedijk et al., 2010).
Currently available instruments for measuring fear of falling range from single-item measures to more detailed assessments, and span a variety of definitions including fall-related self-efficacy, balance confidence, fear, and activity avoidance (Jørstad et al., 2005; Scheffer et al., 2008). In an attempt to standardize measurement, the Prevention of Falls Network Europe (ProFaNE) consensus group recommended conceptualizing psychological consequences of falls in terms of fall-related self-efficacy. Members of the ProFaNE group subsequently developed the now widely used Falls Efficacy Scale International (FES-I), which assesses perceived self-efficacy to complete specific tasks without falling (Yardley et al., 2005). One of the many strengths of the FES-I is that it is based on social cognitive theory, which provides strong theoretical support for the scale. Furthermore, the FES-I and other self-efficacy scales demonstrate excellent reliability and adequate validity in community samples (Scheffer et al.). However, due to the multi-dimensional nature of fear of falling, self-efficacy may not capture the entire experience of fear of falling. Furthermore, ratings are based on specific activities, which may lack relevance or practicality in some contexts (Jørstad et al.). The Survey of Activities and Fear of Falling in the Elderly (SAFFE; Lachman et al., 1998) is another widely used measure that captures the dimension of activity restriction in relation to fear of falling. The SAFFE demonstrated adequate validity in community samples, but like the FES-I ratings are situation-specific and the length of the assessment makes it impractical for some settings (Jørstad et al.). Other options, such as single item measures and visual analogue scales, may be useful in situations where assessment time is very limited, but these scales demonstrate weak to adequate validity and lack sensitivity to change (Jørstad et al.). Finally, many measures that claim to assess fear of falling use the terms “concern” or “worry” in place of “fear.” While these words may be salient to older adults, it is not clear whether they are measuring the same construct as fear (Jørstad et al.). Therefore, measurement selection should be based on consideration of the construct to be measured as well as the practicality of administration within the group or setting of interest (Jørstad et al.).
Importantly, despite the need for valid instruments to assess fear of falling in older adults after hip fracture, no studies have reported the psychometric properties of available measures in hip fracture patients (Visschedijk et al., 2010). Additionally, there are practical limitations to using many of the available scales with older adults undergoing rehabilitation for hip fracture. For example, some items on the FES-I (e.g., “Going up or down stairs”) may not be relevant to fear of falling in individuals with reduced mobility due to hip fracture. Specifically, concern about going up or down stairs may be realistic for someone recovering from hip fracture depending on their level of physical health and functional ability. Furthermore, available instruments that assess the construct of fear tend to be single-item measures (Jørstad et al., 2005). Single-item measures do not provide information about degree of fear, which would be particularly relevant for measuring change across the recovery period in older adults with hip fracture.
Given the limitations discussed above, a multi-item scale that assesses concepts related to fear of falling independent of specific activities or situations would be useful for measuring fear of falling in patients recovering from hip fracture. One option is the multi-item Fear of Falling Questionnaire (FFQ; Dayhoff et al., 1994), which was not included in the review by Jørstad et al. (2005). Dayhoff et al. (1994) developed the FFQ based on the cognitive appraisal model of emotion by Lazarus (1991) in which fear of falling is a function of the emotion of fear and appraisals of potential outcome of harm from a fall, seriousness of harm from a fall, and coping potential to prevent harm. The FFQ demonstrated adequate reliability as well as convergent and discriminant validity in older, community-dwelling adults (Dayhoff et al.). The authors found support for a four-factorial structure, which they interpreted as representing appraisals of harm outcomes, degree of threat, coping potential, and future expectancy related to falling. Additionally, the FFQ differentiated between those who endorsed a fear of falling and those who did not, indicating adequate criterion validity. In a review of measurement tools for fear of falling, Greenberg (2012) noted that the FFQ is not widely known and suggested the need for further studies assessing the utility of the FFQ in older adults at higher risk for falls. To our knowledge, the FFQ has not been used in any published research, so data from other samples is unavailable. It is possible that the FFQ lacked publicity because it was published in a nursing trade journal that ceased publication two years after the article was printed (Spasser et al., 2006). Despite this limitation, the FFQ represents a potentially useful multi-dimensional measure for assessing fear of falling.
The purpose of the current study was to assess the psychometric properties of a revised version of the Fear of Falling Questionnaire (FFQ-R) in older adults recovering from a hip fracture. Revisions to the original FFQ were made to improve readability as well as improve validity for patients rehabilitating from a hip fracture. Construct validity was assessed by comparing performance of the FFQ in hip fracture patients to performance in two extreme samples: older adults with severe fear of falling and healthy older adults. We hypothesized that older adults recovering from hip fracture and those with severe fear of falling would score higher on the FFQ-R than healthy older adults. Because several items related to the construct of self-efficacy were included in the FFQ-R, it was hypothesized that scores on the FFQ-R would correlate positively and moderately with scores on the FES-I. Furthermore, since depression and mood represent distinct constructs from fear, FFQ-R scores were not expected to be strongly associated with scores from measures of depression, negative affect, or positive affect. If the psychometric properties of the FFQ-R were found to be inadequate, we planned to explore potential modifications that would improve the structure and utility of the scale. Specifically, we hypothesized that reverse-scored items included in the original FFQ may introduce method bias since older adults tend to have more difficulty recognizing and altering their response to reflect changes in the direction of wording for reverse-scored items (Carlson et al., 2011). Thus, for post hoc analyses we proposed removing reverse-scored items in addition to other items that performed poorly on preliminary reliability and validity analyses.
Improving methods for assessing fear of falling will enhance identification of those individuals who would benefit from treatment and improve research efforts by reducing measurement error. The FFQ-R is a potentially useful multi-dimensional measure of fear of falling that may be a more comprehensive alternative to currently available single-dimension or single-item scales.
Methods
Participants
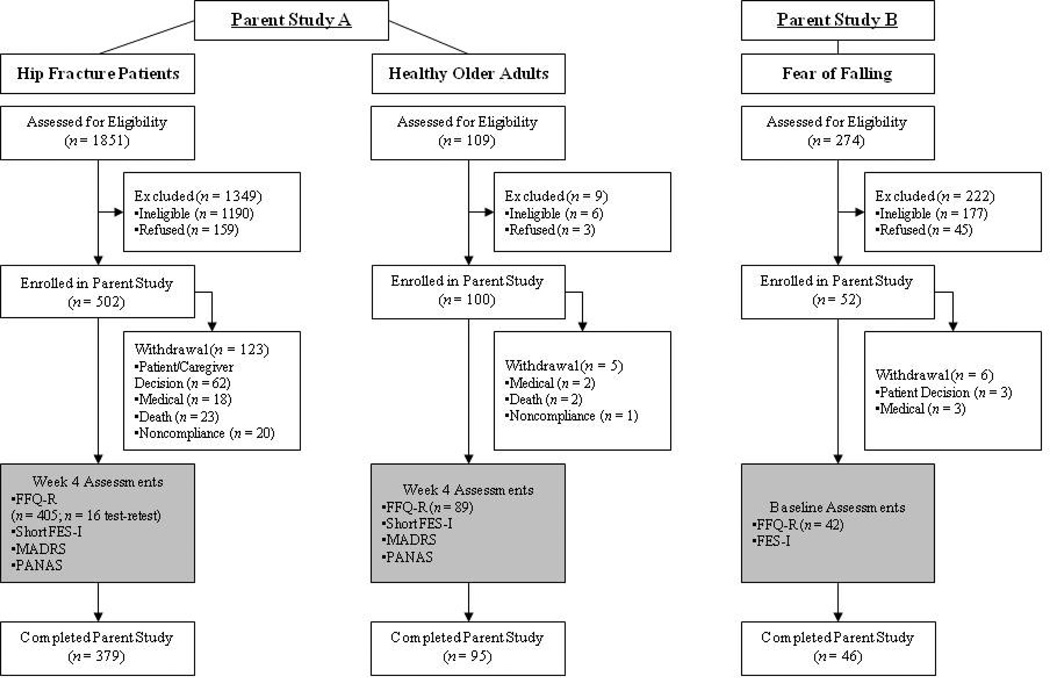
Study participants were drawn from two independent parent studies that administered the FFQ-R as part of a larger assessment battery (see Figure 1). Parent Study A provided two samples: older adults recovering from a hip fracture and healthy community-dwelling older adults. Parent Study B provided a sample of older adults with severe fear of falling. The hip fracture and healthy comparison group were recruited over 4 years (2008–2012) from an urban Midwestern community as part of a study to assess risk factors for mental health problems following a hip fracture (E. Lenze, outcome paper in preparation). To be eligible for the study, patients had to be 60 years of age or older and able to provide informed consent. Patients with current Major Depressive Disorder, a lifetime diagnosis of Bipolar Disorder or Schizophrenia, moderate to severe cognitive impairment, or metastatic cancer were excluded. In addition, participants in the healthy comparison group were excluded if they had hip fracture or other disabling medical or stressful life events within six months of enrollment. Healthy older adult participants were recruited through newspaper advertisements while participants in the hip fracture group were recruited from the hospital approximately 2 days after surgical hip repair. After surgery, participants were admitted to a rehabilitation facility or skilled nursing facility for rehabilitation within approximately 5–6 days. For the current study, all participants who completed the FFQ-R four weeks after study enrollment (i.e., first time-point of fear of falling assessment) were included in the analyses (Hip Fracture: n = 405; Healthy Comparison: n = 89). A random subsample of 16 hip fracture patients were selected to test the temporal consistency of scores used in the parent study. Data regarding the FFQ-R were analyzed for test-retest reliability in the current study.
Figure 1.
Participant flow. CIRSG = Cumulative Illness Rating Scale Geriatrics; FFQ-R = Fear of Falling Questionnaire Revised; FES-I = Falls Efficacy Scale International; MADRS = Montgomery Åsberg Depression Rating Scale; PANAS = Positive and Negative Affect Schedule; HFRS = Hip Fracture Recovery Scale.
Participants for the fear of falling group were recruited from a Southern California community as part of a larger study of treatment for excessive fear of falling (J. Wetherell, outcome paper in preparation). Participants were recruited through presentations at community events and meetings (48%), flyers posted in the community (29%), mailings (14%), and word of mouth (9%). Inclusion criteria required participants be 65 years or older, endorse severe concern of falling as measured by a FES-I score of greater than 27, report distress or functional impairment due to fear of falling, and have excessive fear and avoidance relative to physical health and functional limitations based on clinical judgment. Potential participants were excluded if they experienced 2 or more falls in the past year, had a history of osteoporotic fracture, were currently receiving professional rehabilitation services, were legally blind, were unable to walk unassisted, had a body mass index of 17.0 or under, had significant orthostasis, were experiencing psychosocial factors or had a medical condition that would compromise study participation. Additionally, potential participants were excluded if they were diagnosed with dementia or scored 10 or more on the Short Blessed Test, were experiencing active suicidal ideation, had a lifetime diagnosis of Bipolar I or II disorder or any psychotic disorder, had alcohol or other substance abuse or dependence within six months of study enrollment, or were currently receiving psychotherapy. For the current study, all participants who completed the FFQ-R at baseline assessment were included in the analyses (n = 42).
Procedure
Scale revision
Revisions to the original FFQ were made based on face validity by clinicians who are experts in geriatric mental health and fear of falling. The original FFQ included five items that confounded with disability (e.g., “If I fall, I would have to stop doing activities, such as shopping, that am doing now.”) or were biased by current recovery processes (e.g., “I do not have the help I need to recover from any injury due to a fall.”) in adults who are recovering from an injury. Thus, these items were removed from the FFQ-R. One additional item was removed due to poor item to total correlation in the initial study by Dayhoff et al. (1994). Minor wording adjustments and revisions to the instructions, the format, and the rating scale were made to improve readability.
Study Design
Hip fracture and healthy comparison participants were first administered the FFQ-R four weeks after study enrollment. In addition, participants in these two groups completed the short FES-I (Kempen et al., 2008), Montgomery-Åsberg Depression Rating Scale (MADRS; Montgomery and Asberg, 1979), and a 10-item version of the Positive and Negative Affect Schedule (PANAS; Mackinnon et al., 1999) at four weeks. The fear of falling group was administered the FFQ-R and full FES-I at baseline, along with other assessments were not included in the current study. In order to compare premorbid functional and health status in the hip fracture group to the healthy comparisons, we obtained information using the Hip Fracture Recovery Score (HFRS; Zuckerman et al., 2000; Zuckerman et al., 2000) and the Cumulative Illness Rating Scale – Geriatrics (CIRSG; Miller, et al., 1992).
The FFQ-R is a 15-item self-report questionnaire for measuring fear of falling. Each item is rated on a Likert-type scale from 1 (strongly disagree) to 4 (strongly agree). The total possible score ranges from 15–60, with higher scores indicating greater fear of falling.
The short FES-I is a 7-item self-report questionnaire for measuring perceived self-efficacy to avoid a fall in various situations (e.g., “taking a bath or shower”). Each item is rated on a 4-point Likert-type scale from 1 (not at all concerned) to 4 (very concerned). The total possible score ranges from 7–28, with higher scores indicating lower perceived self-efficacy to avoid a fall. The short FES-I was found to correlate strongly with the full FES-I and demonstrated excellent reliability over 4 weeks (Kempen et al., 2008). The short FES-I demonstrated excellent internal consistency in the hip fracture and healthy comparison groups (α = 0.83–0.98). The full FES-I was used for evaluating eligibility for the fear of falling participants, and includes 16 items with a possible score range of 16–64. To allow for comparison with the hip fracture and healthy comparison group, only the seven items included in the short FES-I were used to assess convergent validity in this group. For the fear of falling group, internal consistency of the full FES-I was good (α = .84).
The MADRS is a 10-item physician-rated scale for measuring degree of depression symptoms (e.g., “Concentration Difficulties”). Each item is rated on a 6-point scale with 0 indicating absence of the symptom and 6 indicating highest degree of the symptom. The total score ranges from 0–60, with higher scores indicating more depression symptomology. The MADRS is often used to assess change in depression symptoms, and demonstrates strong psychometric properties in outpatients (Uher et al., 2008).
The short form of the PANAS is a 10-item version of the 20-item PANAS for measuring positive and negative affect. Items are rated on a 5-point scale indicating the extent that the participant felt each item in the past week from “not at all” to “extremely”. Subscale scores for positive affect and negative affect range from 5–25, with higher scores indicating higher degree of positive or negative affect, respectively. Mackinnon et al. (1999) found that the structural characteristics of the scale were robust to age and gender differences in a large probability sample. For the current sample, internal consistency were acceptable (Positive = .71–.79; Negative: α = .67–.82).
The HFRS is a physician-administered interview that consists of 11 items covering three domains: basic activities of daily living (BADL), instrumental activities of daily living (IADL), and mobility. Lower scores indicate more assistance needed, with BADL scores ranging from 0–44, IADL from 0–23, and mobility from 0–33. Good reliability and validity were established in a group of older patients following surgery for hip fracture (Zuckerman et al., 2000).
The CIRSG is a physician-rated scale for assessing medical burden in elderly populations. The scale consists of 14 categories of illness, and for the current study, the number of categories endorsed were summed for a total score ranging from 0–14. The scale demonstrated good reliability and validity in elderly outpatients (Miller et al., 1992).
Statistical Analyses
Descriptive statistics were analyzed by group to determine group characteristics. In the case of unequal variances, the Satterthwaite test was used. Internal consistency was established using Cronbach’s alpha coefficient and item-to-item as well as item-to-total Pearson’s correlation coefficient. To assess whether reliability differed across groups, we calculated alpha’s standard error and compared coefficient alphas using the test of independent sample alphas described in Duhachek and Iacobucci (2004). Test-retest reliability was established in a subsample of hip fracture patients using the Intraclass Correlation Coefficient (ICC). Pearson’s correlation coefficient was used to assess convergent and discriminant validity. Exploratory factor analysis with principal axis factoring was used to determine the internal structure of the scores for the hip fracture patients (internal structure was not examined for the healthy comparison or fear of falling group scores due to insufficient sample size). A threshold of > .5 for the Kaiser-Meyer-Olkin (KMO) Measure of Sampling Adequacy was used to determine whether the proportion of common variance was adequate for factoring. Four factors were initially specified per the four-factor solution hypothesized by Dayhoff et al. (1994). Factors were retained if they explained approximately 10% of the common variance and were interpretable based on factor pattern coefficients. Oblique promax rotation was used to improve factor interpretation, and interpretation was based on rotated factor pattern coefficients of .3 or more.
Post hoc revisions began with removal of reverse-scored items due to findings that these items can be problematic for older adults (see Carlson et al., 2011). Next, item-total correlations were examined and items correlating ≤ .30 were evaluated for retention or deletion based on theoretical relevance with the dimensions of the scale. The number of remaining items was insufficient for a four-factor scale (i.e., < 3 items per factor), so exploratory factor analysis was conducted to determine the number of latent factors. Factor coefficients were evaluated for factor interpretation and items with low factor coefficients (<.45, indicating < 20% overlapping variance with other items) were evaluated for retention or deletion based on theoretical relevance with the factor. Reliability and validity were assessed post hoc on the abbreviated version as described above. All statistical analyses were performed using SAS version 9.3.
Results
Participant Characteristics
Groups were similar in terms of age and gender. Hip fracture patients ranged in age from 60–101 years (M = 78.0, SD = 8.7; 74.6% female), while participants in the healthy comparison group ranged from 60–93 years (M = 77.6, SD = 7.6; 67.4% female) and older adults with fear of falling ranged from 65–91 years (M = 77.9, SD = 7.3; 73.8% female). The hip fracture patients completed fewer years of education on average (M = 13.1, SD = 2.9, range 2–26 years) than the healthy comparison (M = 15.0, SD = 2.8, range 9–22 years) and fear of falling groups (M = 15.1, SD = 2.8, range 3–20 years). Older adults with fear of falling were more ethnically diverse (69.1% non-Hispanic White, 11.9% Asian, 9.5% Black or African American, 9.5% Hispanic White) than the hip fracture patients (93.1% non-Hispanic White, 6.2% Black or African American, 0.7% Asian) or healthy comparison group (94.4% non-Hispanic White, 5.6% Black or African American).
Table 1 displays clinical characteristics by group. The fear of falling group did not complete the CIRSG, HFRS, MADRS or PANAS so data are not available. Hip fracture patients were more functionally impaired and scored higher on the measures of depression and negative affect than the healthy comparison group. Conversely, the healthy comparison group scored higher on the measure of positive affect than the hip fracture patients.
Table 1.
Clinical Characteristics and Correlations with the Fear of Falling Questionnaire - Revised (FFQ-R)
| Variable | Hip Fracture | n | Healthy Comparison | n | Fear of Falling | n |
|---|---|---|---|---|---|---|
| CIRSG, M (SD) | 4.8 (1.9)c | 404 | 4.2 (1.9)d | 87 | -- | |
| Functional Ability, M (SD) | ||||||
| BADL | 39.3 (6.9) | 405 | 43.9 (1.0) | 89 | -- | |
| IADL | 14.6 (5.4) | 405 | 22.3 (1.2) | 89 | -- | |
| Mobility | 19.2 (9.7) | 405 | 31.8 (2.8) | 89 | -- | |
| FFQ-R (15-item) | ||||||
| M (SD) | 37.63 (4.93)a | 405 | 31.82 (5.60)b | 89 | 37.83 (5.73)a | 42 |
| Range | 21–52 | 405 | 21–43 | 89 | 25–50 | 42 |
| FFQ-R (6-item) | ||||||
| M (SD) | 16.18 (3.14)a | 405 | 12.67 (3.33)b | 89 | 15.95 (3.73)a | 42 |
| Range | 6–24 | 405 | 6–19 | 89 | 6–23 | 42 |
| r with FFQ-R | .93*** | 405 | .93*** | 89 | .85*** | 42 |
| Short FES-I | ||||||
| M (SD) | 13.01 (4.43)a | 261 | 9.31 (2.94)b | 36 | 17.31 (3.37)c | 42 |
| r with FFQ-R | .43*** | 261 | .70*** | 36 | .89*** | 42 |
| r with 6-Item FFQ-R | .42*** | 261 | .68*** | 36 | .70*** | 42 |
| MADRS | ||||||
| M (SD) | 5.59 (5.44) | 392 | 3.03 (3.37) | 88 | -- | -- |
| r with FFQ-R | .25*** | 392 | .33** | 88 | -- | -- |
| r with 6-Item FFQ-R | .26*** | 392 | .31** | 88 | ||
| PANAS - Positive | ||||||
| M (SD) | 13.92 (3.97) | 391 | 15.35 (3.77) | 88 | -- | -- |
| r with FFQ-R | −.25*** | 391 | −.31** | 88 | -- | -- |
| r with 6-Item FFQ-R | −.17*** | 391 | −.30** | 88 | ||
| PANAS - Negative | ||||||
| M (SD) | 8.17 (3.6) | 391 | 7.49 (2.38) | 87 | -- | -- |
| r with FFQ-R | .32*** | 391 | .28* | 87 | -- | -- |
| r with 6-Item FFQ-R | .34*** | 391 | .25* | 87 |
Note. Means sharing a common subscript are not statistically different at α = .05 according to the Satterthwaite method for group comparison with unequal population variances. BADL = Basic Activities of Daily Living, scores range from 0–44, lower scores indicate more assistance needed; CIRSG = Cumulative Illness Rating Scale Geriatrics, scores range from 0–14, higher scores indicate greater medical burden; FFQR = Fear of Falling Questionnaire Revised, scores range from 15–60 for 15-Item and 6–24 for 6-Item, higher scores indicate greater fear of falling; FES-I = Short Falls Efficacy Scale International, scores range from 7–28, higher scores indicate lower perceived self-efficacy to avoid a fall; IADL = Instrumental Activities of Daily Living, scores range from 0–23, lower scores indicate more assistance needed; MADRS = Montgomery Åsberg Depression Rating Scale, scores range from 0–60, higher scores indicate more depression symptomology; Mobility scores range from 0–33, lower scores indicate moer assistance needed; PANAS = Positive and Negative Affect Schedule, scores range from 5–25, higher scores indicate higher degree of positive or negative affect; r = Pearson Correlation Coefficent.
p < .05.
p < .01.
p < .001.
Reliability
Test-retest reliability was assessed on a subsample of hip fracture participants (n = 16) who completed the FFQ-R twice over an interval of three days. The ICC for this subsample was .93, 95% CI [.85, 1.0], indicating excellent temporal reliability of the scale.
Across all groups, the absolute value of Pearson correlations between items ranged from .0 to .67 (tables available upon request). The FFQ-R demonstrated acceptable internal consistency (see Table 2). Coefficient alpha values did not differ significantly between the hip fracture and fear of falling groups, but were significantly higher in the healthy comparison group compared to the other two groups. As shown in Table 3, items 1, 8, 9, 11, 13, 14, and 15 correlated weakly (i.e., < .30) with the FFQ-R total score in at least one group. The change in alpha if each item were deleted was minimal, however removing item 9 produced improvements across all groups.
Table 2.
Item Correlations with Total Score and Cronbach’s Coefficient Alpha with Item Deleted
|
Hip Fracturea |
15-Item Healthy Comparisonb |
Fear of Fallingc |
Hip Fracturea |
6-Item Healthy Comparisonb |
Fear of Fallingc |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Deleted Item | r | α | r | α | r | α | r | α | r | α | r | A |
| 1. It is likely I will fall in the next month. | .21 | .76 | .49 | .79 | .35 | .71 | ||||||
| 2. If I fall chances are I will be hurt in some way. | .45 | .74 | .46 | .79 | .33 | .71 | .46 | .79 | .53 | .81 | .36 | .79 |
| 3. I cannot prevent a fall. | .31 | .76 | .44 | .79 | .49 | .69 | ||||||
| 4. I am afraid of falling again. | .63 | .72 | .74 | .77 | .40 | .70 | .67 | .75 | .63 | .79 | .50 | .76 |
| 5. If I fall, my life would change greatly. | .53 | .73 | .59 | .78 | .69 | .66 | .52 | .78 | .60 | .80 | .65 | .72 |
| 6. The thought of falling really frightens me. | .66 | .72 | .68 | .77 | .46 | .69 | .66 | .75 | .71 | .77 | .64 | .72 |
| 7. I will probably fall if I get dizzy or trip. | .43 | .75 | .43 | .79 | .48 | .69 | .44 | .80 | .48 | .82 | .48 | .76 |
| 8. I can probably prevent myself from falling. | .33 | .75 | .43 | .79 | −.18 | .75 | ||||||
| 9. I could make some changes in my life to prevent a fall. | .03 | .78 | −.09 | .83 | −.03 | .74 | ||||||
| 10. I frequently limit my activities to prevent a fall. | .33 | .75 | .53 | .78 | .33 | .71 | ||||||
| 11. I seldom think about the possibility of falling. | .26 | .76 | .43 | .79 | −.21 | .76 | ||||||
| 12. One of my worst fears is that I will fall. | .63 | .72 | .68 | .77 | .49 | .69 | .62 | .76 | .63 | .79 | .58 | .74 |
| 13. It is very likely that I could fall without being injured. | .14 | .77 | .08 | .81 | .31 | .71 | ||||||
| 14. I know many people in situations similar to mine who have fallen. | .20 | .77 | .31 | .80 | .54 | .68 | ||||||
| 15. The older people get the more likely they are to fall. | .23 | .76 | −.05 | .82 | .35 | .71 | ||||||
| Cronbach's Coefficient Alpha, 95% CI [upper, lower] | .76 [.73, .80] | .81 [.75, .86] | .72 [.61, .84] | .80 [.77, .83] | .83 [.77, .88] | .78 [.68, .88] | ||||||
Note. CI = Confidence Interval. r = Correlation with Total. α = Cronbach's Alpha Coefficient if item is deleted.
n = 405.
n = 89.
n = 42.
Table 3.
Rotated Factor Pattern, Eigenvalues, and Inter-Factor Correlations of the 15-Item and 6-Item Fear of Falling Questionnaire - Revised in Hip Fracture Patients (n = 405)
| 15-Item | 6-Item | |||||
|---|---|---|---|---|---|---|
| Factor 1 |
Factor 2 |
Factor 3 |
Factor 4 |
Factor 1 |
Factor 2 |
|
| Item | ||||||
| 1. It is likely I will fall in the next month. | .19 | .04 | .31 | −.30 | ||
| 2. If I fall chances are I will be hurt in some way. | .01 | .12 | .15 | .42 | .05 | .53 |
| 3. I cannot prevent a fall. | −.15 | .13 | .57 | −.10 | ||
| 4. I am afraid of falling again. | .58 | .15 | .03 | .13 | .72 | .07 |
| 5. If I fall, my life would change greatly. | .06 | .28 | .10 | .34 | .18 | .47 |
| 6. The thought of falling really frightens me. | .65 | .17 | .05 | .02 | .79 | .00 |
| 7. I will probably fall if I get dizzy or trip. | −.13 | .36 | .21 | .23 | .08 | .48 |
| 8. I can probably prevent myself from falling. | −.04 | .32 | −.60 | −.10 | ||
| 9. I could make some changes in my life to prevent a fall. | −.11 | .48 | −.30 | −.09 | ||
| 10. I frequently limit my activities to prevent a fall. | .00 | .54 | .01 | −.01 | ||
| 11. I seldom think about the possibility of falling. | −.65 | .18 | .15 | .00 | ||
| 12. One of my worst fears is that I will fall. | .44 | .30 | .17 | −.04 | .60 | .14 |
| 13. It is very likely that I could fall without being injured. | −.01 | .11 | .14 | −.52 | ||
| 14. I know many people in situations similar to mine who have fallen. | .09 | .31 | .06 | −.17 | ||
| 15. The older people get the more likely they are to fall. | .01 | .38 | −.11 | .08 | ||
| Eigenvalues | ||||||
| Variance Explained (Ignoring Other Factors) | 2.61 | 2.22 | 2.24 | 1.78 | 2.26 | 1.84 |
| Variance Explained (Eliminating Other Factors) | 0.79 | 0.88 | 0.54 | 0.50 | 0.83 | 0.41 |
| Chronbach's Alpha Coefficient | .77 | .27 | .42 | .42 | .82 | .62 |
| Inter-Factor Correlations | ||||||
| Factor 1 | 1.00 | -- | -- | -- | 1.00 | -- |
| Factor 2 | .53 | 1.00 | -- | -- | −.68 | 1.00 |
| Factor 3 | .61 | .45 | 1.00 | -- | -- | -- |
| Factor 4 | .47 | .40 | .57 | 1.00 | -- | -- |
Note. Factor pattern coefficients greater than or equal to .30 are shown in boldface.
Validity
An exploratory factor analysis was conducted to determine the internal structure of the FFQ-R. The KMO Measure of Sampling Adequacy was .82, indicating the proportion of common variance in the items was adequate for performing a factor analysis. The rotated factor pattern (standardized regression coefficients), eigenvalues (λ), and correlations between factors are listed in Table 3. Four factors each accounted for approximately 10% or more of the common variance (0.83, 0.18, 0.14, 0.09) and were retained in the initial analysis due to theoretical relevance to the proposed model. Cumulative variance explained by the four factors was greater than 1.0 due to the use of common variance rather than total variance for the target matrix. Root Mean Squared Error (RMSE) was 0.03, indicating that the residuals were relatively small on average. Four items (1, 8, 9, and 12) loaded on two factors after rotation. Interpretation of the factors based on the rotated factor pattern were consistent with the results of Dayhoff et al.(1994), which suggested the four latent factors related to degree of threat (Factor 1), future expectancy (Factor 2), coping potential (Factor 3), and harm outcomes (Factor 4). As shown in Table 3, Cronbach’s alpha coefficients were poor for Factors 2–3, but adequate for Factor 1.
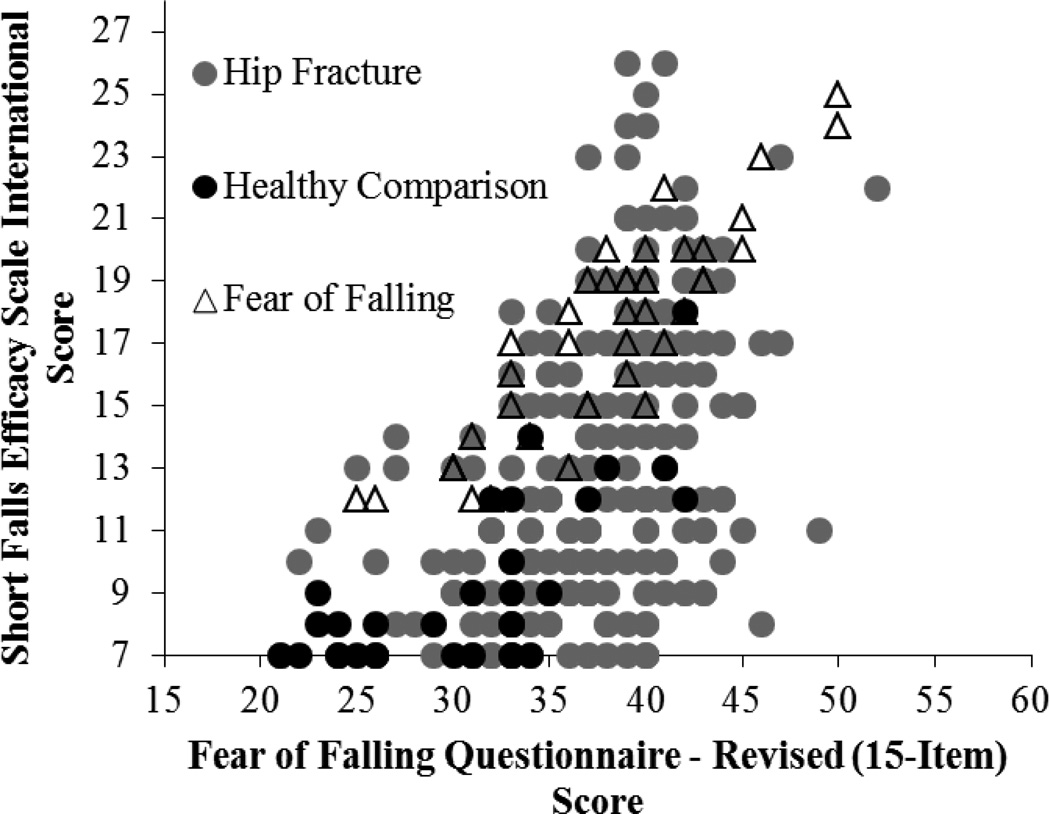
The hip fracture group scored higher on the FFQ-R than the healthy comparison group (see Table 1). Conversely, mean FFQ-R scores for the hip fracture group were similar to scores for the fear of falling group. Convergent validity of the FFQ-R was explored using the short FES-I while divergent validity was assessed using the MADRS and PANAS in the hip fracture and healthy comparison groups (see Table 1). As hypothesized, the FFQ-R was moderately and positively associated with the FES-I in the hip fracture group, and strongly correlated in both the healthy comparison group and in the fear of falling group (see Figure 2). The FFQ-R was weakly and positively associated with depression as measured by the MADRS in the hip fracture group, and moderately correlated in the healthy comparison group. Correlations with the PANAS were weak and negative in the hip fracture group, and moderately associated in the healthy comparison group while correlations with negative affect were moderate and positive in both the hip fracture and healthy comparison group.
Figure 2.
Scatterplot indicating the association between the Fear of Falling Questionnaire – Revised (15-Item) and the short Falls Efficacy Scale International in the hip fracture, healthy comparison, and fear of falling groups at baseline assessment.
Post Hoc Analyses
Reverse-scored items were removed (four items) and item-total correlations were evaluated for poor performance. Item 15 was removed due to weak correlations with the total score across all three groups and weak relevance with the underlying theory (i.e., assessing beliefs about age-related risk for falls rather than individual appraisals). A factor analysis suggested a two-factor solution (results not shown) corresponding to appraisals of degree of threat (Factor 1) and harm outcomes (Factor 2). Items 1, 3, 10, and 14 were assessing other latent factors and were removed, resulting in a 6-item scale.
Test-retest reliability for the 6-item scale was strong, ICC = .82, 95% CI [.65, .99]. Internal consistency across groups was acceptable (Table 2) and did not differ significantly between groups. Exploratory factor analysis with oblique rotation (KMO = .82) suggested a two-factor solution (Table 3). Factor pattern coefficients suggested that three items loaded univocally on each factor corresponding to appraisals of degree of threat (Factor 1) and harm outcomes (Factor 2). Convergent and divergent validity of the 6-item scale was similar to that of the 15-item version (see Table 1).
Discussion
The purpose of this study was to examine the psychometric properties of the FFQ-R in hip fracture patients. The FFQ-R is a revised version of a multi-item, multi-dimensional self-report questionnaire to measure fear of falling. The original FFQ was identified as a promising but under-utilized fear of falling measure that could address limitations of currently available measures by including multiple activity-independent items that measured the dimension of fear. Revisions to the original scale were made to improve readability and validity of the items for older adults recovering from hip fracture. The questionnaire was also administered to a group of healthy older adults and a group of uninjured older adults with severe fear of falling in order to compare extreme group scores for construct validation.
The FFQ-R demonstrated acceptable reliability as evidenced by test-retest and internal consistency. The original FFQ exhibited moderate stability over three weeks in community-dwelling older adults (Pearson’s r = .57; Dayhoff et al., 1994). In the current study, test-retest of the FFQ-R over several days in hip fracture patients was very strong (ICC = .93), which was comparable to that of the FES-I in a community sample over one week (ICC = .96; Yardley et al., 2005). Internal consistency of the FFQ-R in the current study was similar to the original scale (α = .81; Dayhoff et al.), although slightly lower in hip fracture patients and older adults with fear of falling. It should be noted that internal consistency of the FFQ-R was slightly lower than estimates for the FES-I in our sample of hip fracture patients (α = 0.83) and in a community sample of older adults (α = 0.95; Yardley et al., 2005).
Construct validity of the FFQ-R was supported based on convergence with scores on the FES-I and divergence from scores on the MADRS and PANAS. As expected, findings suggest that the FFQ-R is measuring a similar construct as the FES-I while capturing some unique variance. Furthermore, scores on the FFQ-R were not strongly related to scores on measures for depression and positive or negative affect, which are potentially related but unique constructs. Importantly, associations between the FFQ-R and FES-I were lower for hip fracture patients than for healthy older adults or adults with fear of falling. This was true despite the fact that the hip fracture group scored similarly to the fear of falling group on the FFQ-R. These findings are in line with the hypothesis that the FES-I may be problematic for those with limited mobility. Further research is needed to explore this issue, but the discrepancy suggests that the FFQ-R may be a useful alternative to the FES-I for assessing fall-related psychological outcomes in older adults recovering from injury.
An exploratory factor analysis of scores from the hip fracture patients suggested a four-factor solution, which was comparable to findings from the original FFQ in community-dwelling older adults as reported by Dayhoff et al. (1994). Specifically, the factor pattern coefficients were consistent with themes of appraisals of degree of threat (Factor 1), future expectancy (Factor 2), coping potential (Factor 3), and harm outcomes (Factor 4). Factor pattern coefficients and Cronbach’s alpha were strongest for Factor 1 compared to the other factors. Factor 1 included items related to preoccupation with falling and fear of falling. This corresponds with the theory by Lazarus and Folkman (1984) that appraisal of threat is the extent to which an individual anticipates that harm or loss will have an impact on future functioning, which they posit is characterized by the emotion of fear. Notably, although Factors 2 and 3 appeared to correspond most closely to appraisals of future expectancy and coping potential (Lazarus, 1991), respectively, items measuring perceived ability to prevent a fall loaded on both factors, with some items cross-loading. Given the poor internal consistency for three of the four factors, subscale scores should not be calculated or interpreted. This finding is consistent with the original scale proposed by Dayhoff et al.
Items 1 (“It is likely I will fall in the next month”) and 14 (“I know many people in situations similar to mine who have fallen”) did not perform as well in the hip fracture group as in the fear of falling and healthy comparison groups, based on item-total correlations. Furthermore, factor pattern coefficients were lowest for these items. There are several possible reasons for this difference. The hip fracture participants were all residing in a rehabilitation or skilled nursing facility, which may have biased their responses. Specifically, hip fracture patients may feel they are less likely to fall in the next month due to increased support while hospitalized, whether or not they experience fear of falling. Similarly, knowing others in similar situations who have fallen might have been less related to fear of falling status and more related to contextual factors (i.e., hospitalized with other hip fracture patients) in this group.
Post-hoc analysis of a 6-item scale that did not include the reverse-scored items or items relating to the dimensions of coping potential and future expectancy demonstrated improved internal consistency and comparable validity in relation to the 15-item scale. Adjusting responses to reverse-scored items can be challenging for some older adults (Carlson et al., 2011), so deleting these items may improve measurement accuracy. Despite these improvements, the 6-item scale demonstrated reduced test-retest and dimensionality compared to the 15-item scale. There is a need for further research with independent samples to confirm these findings and empirically evaluate the underlying theoretical structure. However, internal consistency and validity of the modified scale were comparable to the 15-item FFQ-R, and correlations between the two were strong. Based on these findings, we recommend further research and utilization focus on the 6-item FFQ-R.
As with all studies, there are some limitations that should be noted. The smaller sample sizes for the healthy comparison and fear of falling groups relative to the hip fracture group prevented analysis and comparison of the factor structure across all groups. Additional studies are needed to confirm the reliability and validity of the FFQ-R in community-dwelling older adults and noninjured older adults with fear of falling. Furthermore, although post hoc item revisions were based on content analyses, preliminary revisions were based on face validity and did not directly address the structural discrepancy from the original study by Dayhoff et al. (1994). Namely, although Dayhoff et al. found support for the reliability and discriminative validity of their 20-item scale, items did not load as expected based on the proposed 4-factor model. Exploratory factor analysis of FFQ-R scores from hip fracture patients suggests that although four factors are evident, a single factor explains the majority of the common variance. Further exploration of the factor structure of the FFQ-R is warranted to determine whether this finding is an artifact of not including enough items to capture variance in other factors, or whether a two-dimensional model of fear of falling is more parsimonious. Appraisals of degree of threat and harm outcomes may be more directly related to the emotion of fear related to falling than appraisals of coping potential or future expectancy. Thus, the 6-item scale may be useful for measuring fear related to falling specifically, and would be an advantage over single-item measures of fear of falling for discriminating degree of fear.
A primary strength of the study was that the FFQ-R was tested in three discrete samples. Smith et al. (2000) recommend testing revised scales with an independent sample to confirm reliability and validity. The FFQ-R consistently performed well across healthy community-dwelling older adults, a clinical sample of older adults (i.e., those with fear of falling), and a hospitalized sample of older adults recovering from hip fracture. These findings suggest that the FFQ-R may have broad applications. However, additional studies with larger samples are needed to confirm the reliability and validity of scores in community-dwelling older adults with and without fear of falling.
Fear of falling is related to negative health outcomes such as future falls, poor life satisfaction, and mobility. Thus, improving methods for assessing fear of falling can have profound effects on quality of life for older adults. In hip fracture patients, fear of falling complicates rehabilitation and is associated with poorer outcomes, yet measures of fear of falling and related constructs have not previously been validated in hip fracture patients (Visschedijk et al., 2010). Accurate assessment of fear of falling will help to identify those patients who may benefit from incorporating interventions aimed to reduce fear of falling into the rehabilitation process. Although further studies are needed to confirm the current findings and evaluate the factor structure in additional samples, the FFQ-R is one of the first measures of fear of falling to be validated in hip fracture patients. The FFQ-R was found to have acceptable psychometric properties, and may be useful for assessing fear of falling in hip fracture patients given the activity-independent items.
Our findings provide preliminary evidence that the FFQ-R is a reliable and valid instrument for assessing fear of falling in older adults recovering from a hip fracture. Further research with other samples is needed to confirm and extend the current findings. The FFQ-R may be especially useful with injured or mobility impaired older adults because items are not situation-specific. Furthermore, the FFQ-R includes multiple items that inquire about the dimension of fear specifically, making it a useful scale for measuring the construct of fear related to falling.
Acknowledgments
Research supported by NIMH R34 MH086668 and NIMH R01 MH074596.
Footnotes
Conflict of Interest
None.
Description of Author’s Roles
E. Lenze and J. Wetherell designed the studies, supervised data collection, and contributed to editing the final paper. A. Petkus, C. Merz, and E. Bower analyzed the data and assisted with data collection and editing the final paper. E. Bower wrote the first draft of the paper. V. Malcarne edited the paper.
References
- Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. American Journal of Public Health. 1992;82:1020–1023. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. American Journal of Public Health. 1994;84:565–570. doi: 10.2105/ajph.84.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Theoretical Perspectives. In: Bandura A, editor. Self-efficacy: The Exercise of Control. New York: W. H. Freeman and Company; 1997. pp. 1–34. [Google Scholar]
- Campbell AJ, Reinken J, Allan BC, Martinez GS. Falls in old age: a study of frequency and related clinical factors. Age and Ageing. 1981;10:264–270. doi: 10.1093/ageing/10.4.264. [DOI] [PubMed] [Google Scholar]
- Carlson M, et al. Psychometric properties of reverse-scored items on the CES-D in a sample of ethnically diverse older adults. Psychological Assessment. 2011;23:558–562. doi: 10.1037/a0022484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayhoff NE, Baird C, Bennett S, Backer J. Fear of Falling: Measuring fear and appraisals of potential harm. Rehabilitation Nursing Research. 1994;3(3):97–104. [Google Scholar]
- Duhachek A, Iacobucci D. Alpha’s Standard Error (ASE): An accurate and precise confidence interval estimate. Journal of Applied Psychology. 2004;89:792–808. doi: 10.1037/0021-9010.89.5.792. [DOI] [PubMed] [Google Scholar]
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. Journal of the American Geriatrics Society. 2002;50:1329–1335. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- Greenberg SA. Analysis of measurement tools of fear of falling for high-risk, community-dwelling older adults. Clinical Nursing Research. 2012;21:113–130. doi: 10.1177/1054773811433824. [DOI] [PubMed] [Google Scholar]
- Jørstad EC, Hauer K, Becker C, Lamb SE. Measuring the psychological outcomes of falling: A Systematic Review. Journal of American Geriatrics Society. 2005;53:501–510. doi: 10.1111/j.1532-5415.2005.53172.x. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, et al. The Short FES-I: a shortened version of the falls efficacy scale-international to assess fear of falling. Age and Ageing. 2008;37:45–50. doi: 10.1093/ageing/afm157. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: The Survey of Activities and Fear of Falling in the Elderly (SAFE) Journal of Gerontology: Psychological Sciences. 1998;53B:P43–P50. doi: 10.1093/geronb/53b.1.p43. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Emotion and adaptation. New York: Oxford University Press; 1991. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- MacKinnon A, Jorm AF, Christensen H, Korten AE, Jacomb PA, Rodgers B. A short form of the Positive and Negative Affect Schedule: Evaluation of factorial validity and invariance across demographic variables in a community sample. Personality and Individual Differences. 1999;27:405–416. [Google Scholar]
- Marottoli RA, Berkman LF, Cooney LM., Jr Decline in physical function following hip fracture. Journal of the American Geriatrics Society. 1992;40:861–866. doi: 10.1111/j.1532-5415.1992.tb01980.x. [DOI] [PubMed] [Google Scholar]
- Miller MD, et al. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Research. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. British Journal of Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age and Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- Sherrington C, Lord SR. Increased prevalence of fall risk factors in older people following hip fracture. Gerontology. 1998;44:340–344. doi: 10.1159/000022039. [DOI] [PubMed] [Google Scholar]
- Smith GT, McCarthy DM, Anderson KG. On the sins of short-form development. Psychological Assessment. 2000;12:102–111. doi: 10.1037//1040-3590.12.1.102. [DOI] [PubMed] [Google Scholar]
- Spasser MA, Greenblatt RB, Weismantel A. Mapping the literature of rehabilitation nursing. Journal of the Medical Library Association. 2006;94(2 Suppl):E137–E142. [PMC free article] [PubMed] [Google Scholar]
- Stevens JA, Mack KA, Paulozzi LJ, Ballesteros MF. Self-reported falls and fall-related injuries among persons aged ≥ 65 years--United States, 2006. Journal of Safety Research. 2008;39:345–349. doi: 10.1016/j.jsr.2008.05.002. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. New England Journal of Medicine. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- Uher R, et al. Measuring depression: Comparison and integration of three scales in the GENDEP study. Psychological Medicine. 2008;38:289–300. doi: 10.1017/S0033291707001730. [DOI] [PubMed] [Google Scholar]
- Visschedijk J, Achterberg W, van Balen R, Hertogh C. Fear of falling after hip fracture: A systematic review of measurement instruments, prevalence, interventions, and related factors. Journal of the American Geriatrics Society. 2010;58:1739–1748. doi: 10.1111/j.1532-5415.2010.03036.x. [DOI] [PubMed] [Google Scholar]
- Visschedijk J, van Balen R, Hertogh C, Achterberg W. Fear of falling in patients with hip fractures: Prevalence and related psychological factors. Journal of the American Medical Directors Association. 2013;14:218–220. doi: 10.1016/j.jamda.2012.10.013. [DOI] [PubMed] [Google Scholar]
- Yardley L, Beyer N, Hauer K, Kempen G, Piot-Ziegler C, Todd C. Development and initial validation of the Falls Efficacy Scale-International (FES-I) Age and Ageing. 2005;34:614–619. doi: 10.1093/ageing/afi196. [DOI] [PubMed] [Google Scholar]
- Zuckerman JD, Koval KJ, Aharonoff GB, Hiebert R, Skovron ML. A functional recovery score for elderly hip fracture patients: I. Development. Journal of Orthopaedic Trauma. 2000;14:20–25. doi: 10.1097/00005131-200001000-00005. [DOI] [PubMed] [Google Scholar]
- Zuckerman JD, Koval KJ, Aharonoff GB, Scovron ML. A functional recovery score for elderly hip fracture patients: II. Validity and reliability. Journal of Orthopaedic Trauma. 2000;14:26–30. doi: 10.1097/00005131-200001000-00006. [DOI] [PubMed] [Google Scholar]