Abstract
Objectives
For attention-deficit hyperactivity disorder (ADHD), treatment seeking is a critical first step in treatment initiation and remains insufficiently understood. The aims of this study were to estimate ADHD treatment-seeking probabilities over the lifetime and to identify predictors of treatment seeking for ADHD separately for males and females.
Methods
Data were drawn from 2001 to 2005 as part of the National Epidemiologic Survey on Alcohol and Related Conditions, a two-wave face-to-face survey conducted by the National Institute on Alcohol Abuse and Alcoholism (N=34,653).
Results
The lifetime cumulative probability of ADHD treatment seeking was estimated at 55%. Males identifying as African American, with less than 12 years of education, or paranoid personality disorder or in an older cohort (>30 years old) at the time of interview were more likely to experience delays, whereas males with comorbid alcohol dependence, dysthymic disorder, borderline personality disorder, or histrionic personality disorder were less likely. Among females, older age (>44 years) was the only predictor of a delay to first treatment seeking, whereas bipolar disorder was associated with more rapid treatment seeking. Age of onset had opposite effects on treatment-seeking delays by gender; males but not females with early-onset ADHD were more likely to experience treatment-seeking delays.
Conclusions
A large proportion of persons with ADHD do not seek treatment. Furthermore, treatment seeking by males was affected by a greater number of identifiable characteristics, suggesting that males might be more responsive to efforts directed toward expediting treatment entry. Future research should explore how to facilitate early access to treatment for individuals with ADHD.
Attention-deficit hyperactivity disorder (ADHD) is the most common childhood-onset neuro-behavioral disorder (1,2) and is associated with a wide range of psychosocial problems, including increased interpersonal conflict (3,4), unintentional injuries, impaired driving (5,6), substance use, low educational attainment, occupational impairment (7,8), and criminal involvement (9). Given that ADHD often persists beyond childhood (10) and that many of the associated impairments may be diminished by early diagnosis and management (11), improving the timely entry of individuals with ADHD into treatment remains an important public health goal (12).
Although there has been a rise in stimulant use in the United States (13–15), substantial barriers to the diagnosis and treatment of ADHD persist. Up to half of all children with ADHD are not properly diagnosed (16,17), and among those with ADHD persisting into adulthood, only about one-quarter report having received treatment for their symptoms in the past year (18). In addition, the median period from ADHD onset to first treatment contact exceeds a decade, with older cohort, late symptom onset, and perhaps low socioeconomic status appearing to increase delays (19–22).
Treatment seeking for ADHD, however, remains inadequately understood. Gender differences have not been adequately studied, and vulnerable sub-populations among males and females have not been determined. These are important areas of inquiry given that ADHD presents with a variable course by gender, with males more likely to have impairments that elicit attention, such as hyperactivity and behavioral disturbances (16,23). Another substantial gap in knowledge is how any comorbid psychiatric disorders might affect ADHD treatment seeking.
We therefore aimed to address these gaps by examining life time ADHD treatment seeking as reported in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (24). First, we estimated the cumulative probability of lifetime treatment seeking, expecting probabilities and median delays to be consistent with a previous analysis (22). Second, we evaluated whether gender significantly influences treatment seeking and assessed the effect of psychiatric comorbidity and demographic characteristics on time to treatment seeking separately for males and females. Because boys are more likely than girls to attract clinical attention to ADHD and related behavioral disturbances (16,23), and yet treatment of psychiatric disorders generally follows the opposite pattern among adults (22,25), we had no hypothesis regarding the effect of gender on treatment seeking. However, we expected that many of the same variables that influence treatment seeking in other medical settings, such as race-ethnicity, psychiatric comorbidity, education level, and age of onset, would be influential here as well (16,17,22) and that treatment seeking by males, which is more precarious than treatment seeking by females (26), would be more likely to be affected by these characteristics.
Methods
Sample
The 2001–2002 NESARC, and the 2004–2005 follow-up, is a nationally representative sample of the adult population of the United States. The survey is conducted by the U.S. Census Bureau under the direction of the National Institute on Alcohol Abuse and Alcoholism, as detailed elsewhere (24,27). Face-to-face interviews were conducted with 43,093 wave 1 participants and yielded a response rate of 81%. Excluding ineligible (deceased) respondents, the wave 2 response rate was 70% of the original sample, for a total sample for this study of 34,653.
Assessment
Sociodemographic measures included sex, race-ethnicity, nativity (U.S. born or foreign born), age, education, and marital status; data were adjusted to be representative of the civilian U.S. population on these variables (28). The diagnostic interview was the Alcohol Use Disorder and Associated Disabilities Interview Schedule–DSM-IV version (AUDADIS-IV) (29), wave 2 version (24), designed for administration by experienced professional interviewers who are not clinicians (27). Diagnoses included in the AUDADISIV can be separated into five main groups: substance use disorders (including alcohol abuse and dependence, substance abuse and dependence, and nicotine dependence); mood disorders (including major depressive disorder, dysthymia, and bipolar disorders); anxiety disorders (including panic disorder, social anxiety disorder, specific phobia, generalized anxiety disorder, and posttraumatic stress disorder); ADHD, including all subtypes; and personality disorders.
At wave 2, respondents were queried about the symptoms of ADHD as outlined in DSM-IV. Twenty symptom items operationalized the 18 ADHD criteria. Consistent with the DSM-IV criteria, respondents were required to meet DSM-IV symptom thresholds for at least six months and with significant social, academic, or occupational impairment. Symptom onset must have occurred before age 12, which represents a deviation from the current DSM-IV conceptualization of symptoms prior to age 7 but is consistent with the ADHD committee for DSM-5 (10,30). Test-retest reliability for ADHD was good (k=.71), and internal consistency reliability of the ADHD symptom items was excellent (Cronbach's α=.89) (31).
Test-retest reliabilities for AUDADISIV mood, anxiety, and personality disorders in the general population and clinical settings were fair to good (k=.40–.77) (31–34). Convergent validity and test-retest reliability were good to excellent for all affective, anxiety, and personality diagnoses (31,35–39). The test-retest reliability of AUDADISIV for substance use disorder diagnoses has been documented as good to excellent (k=.70–.91) in clinical and general population samples (31,35,40,41), and its convergent, discriminant, and construct validity has been rated as good to excellent (42–44).
Respondents were also asked whether they had ever seen a general medical or mental health professional for ADHD. Affirmative responses were followed by a question to assess the age at which the respondent first had contact with a professional for ADHD treatment. In the absence of information on the type or quality of care received, we refer to affirmative responses as ADHD treatment seeking. This query did not ascertain what brought the respondent into contact (such as self-referral, referral, or parental accompaniment).
Statistical analyses
Among respondents with lifetime ADHD, weighted cross-tabulations were used to calculate the proportion who had sought treatment for ADHD by wave 2 both overall and specifically by respondent sociodemographic characteristics and psychiatric comorbidity diagnoses, with adjustments for certain significant variables by the time of the assessment. Correlations between demographic and comorbidity characteristics and wave 2 treatment seeking were investigated independently for males and females.
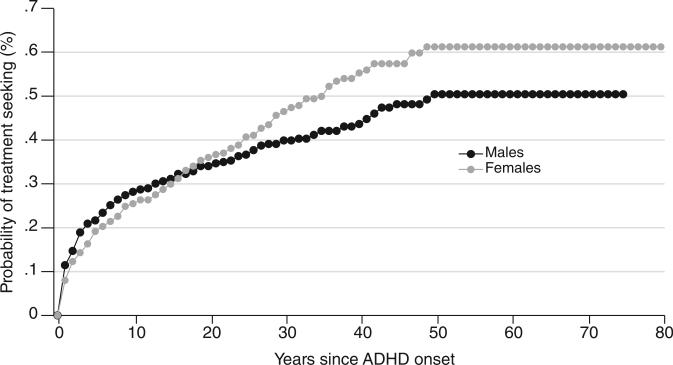
To examine the effect of gender on time to treatment seeking, a Cox proportional-hazard regression model with time-varying covariates (years of education, marital status, and presence or absence of each comorbid disorder) was performed to investigate whether gender was a significant predictor. The time span started at age of ADHD onset and terminated at age of first treatment contact. A Kaplan-Meier analysis was also conducted to compare the lifetime cumulative probability of treatment seeking by gender.
Cox proportional-hazard regression models with time-varying covariates (years of education, marital status, and presence or absence of each comorbid disorder) were then run separately for males and females. The probability of treatment seeking was first modeled separately for each individual socio-demographic and comorbid predictor and again in a single model that controlled for the potentially confounding effects of age, race-ethnicity, nativity, education, marital status, and comorbidity. Results are reported, respectively, as hazard ratios and adjusted hazard ratios with 95% confidence intervals.
Standard errors and 95% confidence limits for all analyses were estimated with SUDAAN software (45). We considered odds ratios and hazard ratios significant when confidence intervals did not cross 1 (46).
Results
The cumulative probability of lifetime treatment seeking was 55%. Gender did not have a significant effect on time to treatment seeking nor on the cumulative probability of treatment seeking (Figure 1).
Figure 1.
Estimated cumulative lifetime probability of ADHD treatment seeking after onset of the disorder, by gender
Treatment seeking for ADHD
By wave 2, less than half (46%, N=284) of respondents with lifetime ADHD reported having sought treatment for ADHD. Table 1 shows the sociodemo-graphic characteristics associated with treatment seeking at wave 2, and Table 2 shows associated comorbid psychiatric disorders.
Table 1.
Demographic characteristics as predictors of ADHD treatment seeking at wave 2 of the NESARC, by gendera
| Males (N=409, 58.49%, weighted) |
Females (N=355, 41.51%, weighted) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | N | % of total | SE | OR | 95% CI | AORb | 95% CI | N | % of total | SE | OR | 95% CI | AORb | 95% CI |
| Total | 322 | 45.6 | 3.1 | 294 | 48.0 | 3.7 | ||||||||
| Years of education | ||||||||||||||
| 0–12 | 152 | 38.5 | 4.8 | .57 | .34–.96 | .47* | .25–.88 | 114 | 39.9 | 5.7 | .59 | .33–1.07 | .50* | .25–1.00 |
| >12 (reference) | 170 | 52.4 | 4.1 | 1.00 | 1.00 | 180 | 52.9 | 4.7 | 1.00 | 1.00 | ||||
| Age of ADHD onset | ||||||||||||||
| 0–11 | 293 | 44.7 | 3.4 | .66 | .25–1.73 | 262 | 51.6 | 3.8 | 4.87* | 1.94–12.23 | ||||
| 12–18 (reference) | 29 | 54.9 | 10.9 | 1.00 | 32 | 17.9 | 6.5 | 1.00 | ||||||
| Cohort | ||||||||||||||
| 18–29 (reference) | 89 | 58.6 | 6.4 | 1.00 | 1.00 | 69 | 45.3 | 7.1 | 1.00 | 1.00 | ||||
| 30–44 | 101 | 44.4 | 5.1 | .57 | .29–1.11 | 1.12 | .44–2.84 | 115 | 55.8 | 6.0 | 1.53 | .73–3.20 | 1.59 | .74–3.41 |
| 45–60 | 109 | 37.7 | 5.2 | .43 | .21–.87 | .71 | .25–2.01 | 91 | 44.5 | 6.3 | .97 | .45–2.08 | 1.28 | .56–2.93 |
| >60 | 23 | 10.9 | 5.7 | .09 | .02–.31 | .12* | .03–.60 | 19 | 29.1 | 11.3 | .50 | .14–1.73 | .80 | .22–2.97 |
| Race-ethnicity | ||||||||||||||
| White (reference) | 224 | 47.6 | 3.7 | 1.00 | 1.00 | 196 | 47.9 | 4.4 | 1.00 | 1.00 | ||||
| African American | 27 | 32.2 | 11.3 | .52 | .18–1.54 | .81 | .22–2.93 | 38 | 37.7 | 9.4 | .66 | .27–1.61 | .32* | .11–.91 |
| Asian | 3 | .0 | .0 | — | — | — | — | 5 | 56.6 | 27.3 | 1.42 | .15–13.46 | 1.74 | .19–16.10 |
| Hispanic | 55 | 37.2 | 9.1 | .65 | .28–1.52 | .73 | .27–1.97 | 49 | 50.2 | 8.8 | 1.10 | .49–2.45 | 1.59 | .58–4.41 |
| Native American | 13 | 58.9 | 15.7 | 1.58 | .41–6.12 | 2.51 | .59–10.8 | 6 | 68.5 | 19.0 | 2.37 | .40–13.91 | 3.41 | .63–18.5 |
| Marital status | ||||||||||||||
| Unmarried | 102 | 61.6 | 5.8 | 2.83 | 1.49–5.37 | 3.20* | 1.33–7.67 | 63 | 48.3 | 9.0 | .99 | .42–2.36 | 1.35 | .61–3.02 |
| Married (reference) | 144 | 36.2 | 4.2 | 1.00 | 1.00 | 154 | 48.4 | 4.8 | 1.00 | 1.00 | ||||
| Separated | 76 | 43.4 | 6.8 | 1.35 | .69–2.64 | 1.71 | .71–4.16 | 77 | 46.4 | 7.2 | .92 | .49–1.75 | 1.12 | .54–2.32 |
| Nativity | ||||||||||||||
| U.S. born (reference) | 301 | 47.0 | 3.2 | 1.00 | 1.00 | 274 | 48.1 | 3.7 | 1.00 | 1.00 | ||||
| Foreign born | 21 | 17.6 | 7.9 | .20 | .10–.80 | .40 | .00–2.00 | 20 | 44.8 | 14.1 | .90 | .28–2.70 | .64 | .21–1.99 |
NESARC, National Epidemiologic Survey on Alcohol and Related Conditions
Adjusted for race-ethnicity, nativity, age of onset, years of education (time varying), marital status (time varying), and comorbidity
Confidence intervals do not cross 1 (p<.05).
Table 2.
Comorbid psychiatric disorders as predictors of ADHD treatment seeking at wave 2 of the NESARC, by gendera
| Males (N=409, 58.49%, weighted) |
Females (N=355, 41.51%, weighted) |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Comorbidity | N | % | SE | OR | 95% CI | AORb | 95% CI | N | % | SE | OR | 95% CI | AORb | 95% CI |
| Any alcohol use disorder | 223 | 40.9 | 3.8 | .57 | .33–1.00 | 131 | 58.6 | 5.6 | 2.14 | 1.21–3.78 | ||||
| Alcohol abuse | 78 | 29.3 | 5.9 | .40 | .21–.78 | .22* | .09–.52 | 43 | 46.4 | 9.8 | .93 | .41–2.13 | 1.15 | .47–2.78 |
| Alcohol dependence | 145 | 47.2 | 4.8 | 1.12 | .66–1.91 | .39* | .17–.91 | 88 | 65.3 | 6.4 | 2.67 | 1.38–5.17 | 2.55* | 1.16–5.60 |
| Any drug use disorder | 136 | 52.6 | 4.8 | 1.63 | .95–2.77 | 82 | 62.7 | 6.5 | 2.27 | 1.19–4.36 | ||||
| Drug abuse | 109 | 54.7 | 5.5 | 1.75 | .99–3.07 | 2.15* | 1.09–4.24 | 63 | 61.0 | 8.0 | 1.96 | .93–4.13 | 1.28 | .56–2.92 |
| Drug dependence | 57 | 48.9 | 7.5 | 1.18 | .61–2.25 | 1.50 | .59–3.78 | 34 | 72.8 | 8.0 | 3.30 | 1.43–7.62 | 2.91 | .71–11.90 |
| Nicotine dependence | 153 | 44.9 | 4.5 | .95 | .57–1.57 | .73 | .35–1.51 | 122 | 47.6 | 5.8 | .98 | .54–1.76 | .54 | .26–1.11 |
| Any mood disorder | 178 | 49.3 | 4.6 | 1.38 | .79–2.41 | 210 | 53.7 | 4.2 | 2.39 | 1.34–4.25 | ||||
| Major depressive disorder | 69 | 55.2 | 7.9 | 1.64 | .79–3.39 | 2.62* | 1.18–5.79 | 99 | 43.3 | 5.3 | .75 | .44–1.26 | 1.66 | .81–3.40 |
| Bipolar disorder | 105 | 46.2 | 5.9 | 1.03 | .58–1.85 | .88 | .37–2.08 | 109 | 64.0 | 5.5 | 2.83 | 1.60–4.98 | 5.25* | 2.07–13.30 |
| Dysthymia | 17 | 43.5 | 15.5 | .91 | .26–3.24 | .30 | .07–1.35 | 27 | 44.1 | 11.4 | .84 | .31–2.29 | .94 | .26–3.33 |
| Any anxiety disorder | 158 | 49.9 | 4.5 | 1.39 | .78–2.47 | 224 | 49.6 | 4.2 | 1.33 | .65–2.71 | ||||
| Panic disorder | 56 | 50.1 | 7.6 | 1.24 | .63–2.43 | .45 | .17–1.16 | 105 | 44.3 | 5.5 | .80 | .45–1.40 | .61 | .30–1.25 |
| Social anxiety disorder | 73 | 57.5 | 6.4 | 1.83 | .94–3.54 | 1.62 | .66–3.97 | 81 | 51.9 | 6.7 | 1.26 | .68–2.31 | .90 | .42–1.91 |
| Specific phobia | 81 | 59.7 | 5.9 | 2.14 | 1.20–3.82 | 3.40* | 1.71–6.76 | 141 | 51.7 | 5.6 | 1.35 | .75–2.42 | .65 | .31–1.37 |
| Posttraumatic stress disorder | 57 | 37.1 | 7.3 | .66 | .33–1.35 | .59 | .23–1.52 | 89 | 54.4 | 6.0 | 1.45 | .78–2.69 | 1.57 | .77–3.19 |
| Generalized anxiety disorder | 56 | 39.9 | 7.7 | .75 | .37–1.54 | .50 | .20–1.20 | 113 | 50.8 | 5.7 | 1.20 | .64–2.25 | .79 | .40–1.55 |
| Any personality disorder | 209 | 49.9 | 3.9 | 1.60 | .89–2.90 | 189 | 52.8 | 4.9 | 1.63 | .85–3.15 | ||||
| Schizotypal | 81 | 50.2 | 6.6 | 1.28 | .69–2.37 | .60 | .26–1.41 | 72 | 57.0 | 6.9 | 1.59 | .87–2.92 | .98 | .39–2.47 |
| Schizoid | 27 | 40.1 | 11.8 | .78 | .27–2.27 | 1.09 | .29–4.16 | 33 | 62.7 | 10.3 | 1.96 | .77–4.99 | 2.59 | .73–9.21 |
| Paranoid | 39 | 33.4 | 8.5 | .57 | .25–1.30 | .45 | .14–1.44 | 69 | 51.4 | 7.2 | 1.20 | .62–2.29 | .43 | .18–1.02 |
| Borderline | 102 | 55.6 | 5.7 | 1.76 | .99–3.12 | 2.50* | 1.09–5.72 | 109 | 58.3 | 6.1 | 1.89 | 1.03–3.46 | 1.55 | .65–3.65 |
| Narcissistic | 92 | 39.4 | 5.7 | .71 | .40–1.29 | .50 | .24–1.04 | 71 | 52.8 | 8.5 | 1.28 | .60–2.74 | .99 | .42–2.35 |
| Histrionic | 31 | 54.2 | 9.4 | 1.46 | .63–3.35 | .84 | .23–3.05 | 34 | 46.9 | 12.0 | .96 | .34–2.67 | .56 | .16–1.99 |
| Antisocial | 78 | 50.9 | 6.7 | 1.33 | .70–2.51 | 1.47 | .62–3.50 | 40 | 55.7 | 9.7 | 1.43 | .61–3.34 | 1.70 | .53–5.45 |
| Obsessive-compulsive | 65 | 55.1 | 7.6 | 1.62 | .79–3.32 | 2.85* | 1.07–7.61 | 65 | 49.9 | 8.0 | 1.10 | .54–2.23 | .95 | .38–2.37 |
| Avoidant | 34 | 46.8 | 9.9 | 1.05 | .44–2.54 | .41 | .12–1.45 | 48 | 57.9 | 8.8 | 1.61 | .73–3.54 | 1.17 | .38–3.63 |
| Dependent | 4 | 85.8 | 13.2 | 7.36 | .81–66.60 | 29.10* | 2.16–393.00 | 16 | 58.5 | 13.9 | 1.57 | .49–5.05 | .85 | .19–3.86 |
NESARC, National Epidemiologic Survey on Alcohol and Related Conditions
Adjusted for race-ethnicity, nativity, age of onset, years of education (time varying), and marital status (time varying)
Confidence intervals do not cross 1 (p<.05).
Sociodemographic and comorbidity characteristics positively associated with treatment seeking by males at wave 2 included being single and having a specific phobia, major depressive disorder, borderline personality disorder, obsessive-compulsive personality disorder, and dependent personality disorder, and characteristics inversely associated with treatment seeking were being in an older cohort (>60 years old) and having education below the 12th grade and alcohol abuse or dependence. Characteristics positively associated with treatment seeking by females at wave 2 were younger age of onset (by age 11), alcohol dependence, and bipolar disorder, whereas factors inversely associated with treatment seeking were less than 12 years of education and identifying as African American.
Predictors of ADHD treatment seeking
Being in an older cohort (>44) was the only characteristic that increased delays in treatment seeking by both males and females; the median delay for the youngest cohort (ages 18–29) was 10.5 years, and the delay for those over 44 was 28 years. Among males, significant sociodemographic predictors of increased delays to treatment seeking were lower education, younger age of onset, identifying as African American, and inclusion in an older cohort at the time of interview (≥30 years old) (Table 3). Males with ADHD and comorbid alcohol dependence, dysthymic disorder, borderline personality disorder, or histrionic personality disorder sought treatment for ADHD more rapidly than males without these comorbidities (Table 4), but those with comorbid paranoid personality disorder were slower to seek treatment. Among females, older cohort at the time of interview (>44 years) was the only predictor of slower treatment seeking, and bipolar disorder and earlier age of onset were associated with more rapid treatment seeking for ADHD.
Table 3.
Demographic characteristics as predictors of delays in ADHD treatment seeking at wave 2 of the NESARC, by gendera
| Treatment-seeking males (N=409, 58.49%, weighted) |
Treatment-seeking females (N=355, 41.51%, weighted) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | HR | 95% CI | Adjusted HRb | 95% CI | HR | 95% CI | Adjusted HRb | 95% CI |
| Education 0–12 years (reference: >12 years) | .28 | .12–.65 | .17* | .06–.47 | .95 | .52–1.74 | .79 | .41–1.51 |
| Age of onset 0–11 (reference: 12–18) | .32* | .16–.67 | 3.26* | 1.31–8.11 | ||||
| Cohort (reference: 18–29) | ||||||||
| 30–44 | .45 | .27–.76 | .39* | .23–.67 | .67 | .40–1.11 | .64 | .37–1.12 |
| 45–60 | .26 | .14–.50 | .22* | .11–.43 | .30 | .15–.59 | .31* | .15–.62 |
| >60 | .05 | .01–.19 | .04* | .01–.17 | .13 | .03–.54 | .14* | .03–.59 |
| Race-ethnicity (reference: white) | ||||||||
| African American | .42 | .16–1.09 | .37* | .14–1.00 | .84 | .38–1.84 | .65 | .27–1.55 |
| Asian | — | — | — | — | .89 | .23–3.37 | 1.45 | .41–5.13 |
| Hispanic | .90 | .47–1.72 | .70 | .30–1.61 | 1.05 | .58–1.93 | 1.31 | .66–2.58 |
| Native American | 1.26 | .54–2.97 | 1.71 | .59–4.94 | 1.52 | .68–3.41 | 1.55 | .53–4.55 |
| Marital status (reference: married) | ||||||||
| Unmarried | 1.59 | .52–4.84 | 1.30 | .46–3.66 | 1.17 | .65–2.10 | .90 | .45–1.82 |
| Separated | 1.39 | .53–3.59 | 1.39 | .52–3.74 | 1.56 | .79–3.08 | 1.35 | .64–2.89 |
| Foreign born (reference: U.S. born) | .32 | .11–.94 | .59 | .15–2.29 | .87 | .33–2.28 | .90 | .34–2.35 |
NESARC, National Epidemiologic Survey on Alcohol and Related Conditions
Hazard ratio (HR) adjusted for race-ethnicity, nativity, age of onset, years of education (time varying), marital status (time varying), and comorbidity
Confidence intervals do not cross 1 (p<.05).
Table 4.
Predictors of ADHD treatment seeking among males and females, by time-varying lifetime comorbidity
| Treatment-seeking males (N=409, 58.49%, weighted) |
Treatment-seeking females (N=355, 41.51%, weighted) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Comorbidity | HR | 95% CI | Adjusted HRa | 95% CI | HR | 95% CI | Adjusted HRa | 95% CI |
| Substance use | ||||||||
| Alcohol abuse | .93 | .28–3.07 | 1.91 | .59–6.18 | .84 | .19–3.65 | .93 | .21–4.18 |
| Alcohol dependence | 2.64 | 1.24–5.61 | 3.63* | 1.37–9.66 | 1.59 | .75–3.38 | .93 | .32–2.67 |
| Drug abuse | 1.50 | .59–3.82 | 1.23 | .05–3.00 | 1.78 | .84–3.75 | 1.24 | .40–3.86 |
| Drug dependence | .90 | .13–6.48 | .58 | .08–4.39 | 2.72 | .66–11.26 | 2.06 | .39–10.78 |
| Nicotine dependence | 1.33 | .57–3.08 | .55 | .20–1.48 | 1.52 | .79–2.92 | 1.01 | .45–2.27 |
| Mood disorder | ||||||||
| Major depression | 1.32 | .62–2.80 | .61 | .28–1.33 | 1.23 | .59–2.59 | 1.67 | .73–3.82 |
| Bipolar | .99 | .40–2.46 | .91 | .32–2.59 | 2.99 | 1.44–6.20 | 2.93* | 1.16–7.38 |
| Dysthymia | 2.10 | .77–5.71 | 3.50* | 1.23–9.95 | .71 | .22–2.26 | .63 | .15–2.60 |
| Anxiety disorder | ||||||||
| Panic | 3.07 | .87–10.85 | 1.36 | .29–6.49 | 1.41 | .57–3.45 | .97 | .36–2.66 |
| Social anxiety | 1.72 | .81–3.65 | 1.19 | .44–3.19 | 1.03 | .58–1.84 | .77 | .37–1.62 |
| Specific phobia | 1.73 | .87–3.43 | 1.42 | .64–3.16 | 1.00 | .62–1.63 | .76 | .46–1.25 |
| Posttraumatic stress | .88 | .28–2.78 | 1.00 | .27–3.74 | 1.66 | .86–3.19 | 1.88 | .92–3.83 |
| Generalized anxiety | 2.03 | .64–6.44 | 1.37 | .26–7.15 | 1.16 | .49–2.76 | .85 | .24–3.06 |
| Personality disorder | ||||||||
| Schizotypal | 1.95 | .88–4.30 | 2.23 | .9–5.53 | 1.92 | 1.12–3.28 | 1.17 | .42–3.23 |
| Schizoid | .77 | .24–2.53 | .61 | .12–3.17 | 1.71 | .75–3.88 | 1.49 | .48–4.64 |
| Paranoid | .26 | .05–1.39 | .02* | <.01–.15 | 1.29 | .60–2.73 | .75 | .31–1.81 |
| Borderline | 3.02 | 1.41–6.48 | 4.47* | 1.80–11.12 | 1.97 | 1.08–3.58 | 2.06 | .91–4.64 |
| Narcissistic | .97 | .41–2.30 | .68 | .25–1.87 | 1.25 | .57–2.71 | .80 | .31–2.06 |
| Histrionic | 2.30 | .93–5.67 | 4.12* | 1.23–13.80 | 1.21 | .48–3.03 | .81 | .26–2.50 |
| Antisocial | .89 | .27–2.90 | .36 | .13–1.01 | 1.16 | .40–3.42 | .58 | .20–1.68 |
| Obsessive-compulsive | 2.28 | .91–5.69 | 2.15 | .83–5.58 | .89 | .42–1.87 | .75 | .30–1.90 |
| Avoidant | 2.44 | .99–6.01 | 3.03 | .97–9.45 | 1.40 | .67–2.90 | .63 | .22–1.84 |
| Dependent | <.01 | < .01–.01 | <.01 | <.01–<.01 | 1.80 | .57–5.70 | 1.49 | .26–8.43 |
Hazard ratio (HR) adjusted for race-ethnicity, nativity, age of onset, years of education (time varying), and marital status (time varying)
Confidence intervals do not cross 1 (p<.05).
Discussion
This is the first study to investigate the effects of comorbid psychiatric disorders on delays to ADHD treatment seeking and the first to investigate predictors of ADHD treatment seeking separately for males and females. We found that the cumulative probability of ADHD treatment seeking was low, at 55%, which is consistent with a previous analysis (22). Although gender did not significantly affect treatment seeking, ADHD treatment seeking by males was influenced by a greater number of characteristics than that by females, with age of ADHD onset having opposite effects on time to treatment seeking among males and females. We also found that comorbid psychiatric disorders variably influenced the time to ADHD treatment seeking. We discuss each of these main findings in turn.
Treatment seeking for ADHD
The cumulative probability of 55% estimated in this study underscores the substantial gap between lifetime treatment seeking for ADHD and treatment seeking for psychiatric disorders in general, which is estimated at 87% in the United States (47). Although it was not possible from this analysis to determine the reasons for these differences, previous studies have indicated that disorders with a chronic course characterized by low to moderate impairment and by the absence of acute exacerbations are less likely to lead to timely treatment than are more disabling and progressive disorders punctuated by crises (48,49). The median delay to treatment seeking from ADHD onset was estimated at over 20 years, which is greater than that for general psychiatric disorders in the United States (47) but consistent with estimates for childhood-onset disorders (22,50).
Addressing these challenges to early ADHD intervention for children and adolescents continues to be important (12). These findings also indicate the need for increased proficiency of practitioners working with older adolescents and young adults at detecting or diagnosing ADHD, because many cases may not present until well after childhood. Along with facilitating treatment entry for ADHD, efforts to improve the diagnosis and management of ADHD across the lifetime may resolve current problems with the overprescription of stimulants, which has been attributed to inappropriate ADHD diagnoses, and may lead to more focused and diagnosis-driven prescribing patterns (14).
Gender differences
Gender was not a significant predictor of ADHD treatment seeking, which is consistent with a previous analysis (22). Nonetheless, several variables appeared to differentially influence treatment seeking by males and females, including various comorbid psychiatric disorders. Older cohorts were the only group with significantly longer delays in treatment seeking for both genders, as found in previous studies (22). Several characteristics emerged as significant predictors of treatment seeking by males, however, that were unapparent in the Wang and colleagues (22) analysis of treatment seeking, which grouped outcomes of males and females together. Predictors included two characteristics found to place individuals at risk for inadequate medical care in other contexts—low education and an African-American background. The reasons why these characteristics place individuals at risk are complex and may include lower access to care, insufficient exposure to teachers adequately trained in ADHD detection and referral, and cultural or attitudinal barriers to seeking help from a mental health professional (22,47). These attributes, in any case, led to greater disruptions in ADHD treatment seeking for males than for females.
Although we did not find gender to be a significant predictor of treatment seeking in our analysis, other researchers have found that males are significantly less likely than females to seek treatment for mental disorders (25) and more likelytoexperience treatment delays (22). This discrepancy in treatment seeking has been attributed to greater facility of females to translate nonspecific perceptions of distress into a conscious recognition that they have a problem meriting attention (26). Males may therefore be more susceptible than females to the influence of various characteristics on treatment seeking because the process of symptom recognition, and of treatment initiation more generally, is more tenuous for them (51). Accordingly, a greater number of variables affected treatment seeking by males compared with females in this analysis, including the demographic characteristics mentioned above.
Roles that individuals other than the designated patient might play in the treatment-seeking process are important to consider. This is relevant to treatment seeking when it occurs both before and after age 18. Studies have found that boys are more likely than girls to attract concern for ADHD symptoms and to enter treatment (52), but these differences become less pronounced as they entered late adolescence and young adulthood (21). The diminishing role of parents and teachers in regard to ADHD treatment seeking as individuals age can explain, to some extent, this changing pattern, particularly because affected boys are more likely than girls to show ADHD-related disruptive behavior that attracts the concern of others (16). Similarly, males with certain comorbid psychiatric disorders may be more likely than males without comorbidity to bring attention to their ADHD symptoms and thereby initiate treatment by virtue of their exposure to health professionals providing psychiatric treatment, monitoring, and ongoing assessments.
An important and novel finding is that earlier age of onset was associated with faster time to treatment seeking by females but with a longer delay in treatment seeking by males. Earlier age of ADHD onset has been associated with more significant impairment in prior studies (53), which may explain why girls, with whom ADHD is generally less conspicuous (16), may be more likely to seek treatment if they have an early-onset, more impairing disorder. Moreover, this may explain why bipolar disorder, associated with disruptive symptoms that clinically overlap with those of ADHD (54), was the only disorder associated with a shorter delay to treatment seeking by females. Conversely, boys may be more likely to experience parental or social normalization of their ADHD symptoms if the disorder emerges at a younger age (50).
Effect of psychiatric comorbidity among males
The effect of psychiatric comorbidity on ADHD treatment seeking, again most salient among males, generally served to shorten the delay to first contact. This effect is consistent with other investigations of treatment seeking for psychiatric disorders. Comorbid psychiatric disorders may increase the perceived need for treatment and treatment seeking, particularly when they are associated with impairment (51) or with short delays to treatment (47,55). Receiving treatment for one disorder may also promote treatment seeking for other disorders. Along with benefiting from the monitoring afforded by regular contact with a health professional, individuals in treatment may have increased access to other treatment providers, greater willingness to seek help for distress, and improved insight regarding when mental health treatment is needed (51,56).
Paranoid personality disorder was the only comorbid condition associated with longer delays to seeking treatment. Paranoid personality disorder is characterized by social withdrawal as well as suspiciousness and distrust of others (57). Cluster A personality disorders as a group have been associated with deficits in emotional processing, restricted affective range, and blunted perception of internal states (58,59), perhaps leading to a reduced awareness of dysfunction. Conversely, borderline and histrionic personality disorders, which served to shorten delays, are typically associated with heightened distress in regard to various aspects of daily functioning, including greater sensitivity to personal dysfunction (60).
It is also important to note that antisocial personality disorder was not associated with a shorter delay to treatment seeking, in contrast to previous investigations restricted to childhood and adolescence (52,61), which have found that co-occurring conduct disorder and oppositional defiant disorder are positively associated with timely and adequate ADHD treatment. Further, the hazard ratio for antisocial personality disorder for first treatment contact was low and nearly significant at .36 (95% confidence interval=.13–1.01). The impact of sociopathy on ADHD treatment seeking therefore appeared to change as individuals entered adulthood and may reflect a greater cultural inclination to approach persistent rule breaking from a medical perspective facilitated by parent and school involvement for boys and from a punitive one for adolescents and adults. In light of prevalence rates of ADHD among prison inmates found to be as high as 45% (62,63), it is important for future studies to further examine the effects of sociopathy and criminal justice system involvement on treatment seeking for ADHD.
Limitations
These results should be interpreted within the context of several limitations. First, information on disorder onset, diagnosis, and treatment seeking was obtained by self-report and may therefore be beset by problems with recall failure or inaccuracy. Disorder onset and past treatment in particular may be recalled as occurring later than they actually did (64); administrative records would have provided more reliable information. Information on family history of ADHD was also unavailable. Similarly, the diagnosis of ADHD was made without collateral information, which may have led to decreased diagnostic sensitivity (2,18). The prevalence of ADHD in our sample, however, was comparable with that obtained in other analyses (2,65). Third, the diagnostic criterion for age of onset (before age 12), although consistent with DSM-5 criteria (10,30), differs from the DSM-IV definition (before age seven). Even though this conceptualization allowed us to study ADHD is a manner congruent with evolving definitions, it limited our ability to compare these findings with those that relied on prior diagnostic criteria.
Conclusions
As expected, a large proportion of persons with ADHD did not seek treatment. Further, treatment seeking often did not begin until well after childhood, decades after the disorder had emerged, with older cohorts of either gender at greater risk for long delays in treatment seeking. Communitywide efforts at public outreach, greater treatment access, and psychoeducation remain important to facilitate the timely entry of affected children into treatment (12), although research is needed to better understand how to optimize receipt of treatment for cases that persist beyond childhood, including how to focus the prescription of stimulants to appropriately diagnosed cases. Further, because delayed treatment seeking among males was influenced by a greater number of identifiable factors compared with treatment seeking among females, this analysis is especially relevant to vulnerable male populations, as in the case of males with an African American background, paranoid personality disorder, low education, or younger age of ADHD onset.
Acknowledgments
The NESARC was sponsored by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and funded, in part, by the Intramural Program, NIAAA, with supplementary funding from the National Institute on Drug Abuse. This study was supported by grants DA007294, DA019606, DA020783, DA023200, DA029647, DA031771, and U18 HS016097.
Footnotes
Disclosures
Dr. Levin is a consultant to GW Pharmaceuticals and has received medication for a National Institutes of Health–funded study from U.S. World Meds. The other authors report no competing interests.
Contributor Information
Elias Dakwar, New York State Psychiatric Institute and the Department of Psychiatry, Columbia University College of Physicians and Surgeons, New York City..
Frances R. Levin, New York State Psychiatric Institute and the Department of Psychiatry, Columbia University College of Physicians and Surgeons, New York City..
Mark Olfson, New York State Psychiatric Institute and the Department of Psychiatry, Columbia University College of Physicians and Surgeons, New York City..
Shuai Wang, New York State Psychiatric Institute and the Department of Psychiatry, Columbia University College of Physicians and Surgeons, New York City..
Bradley Kerridge, School of Public Health, University of Maryland, College Park, Maryland..
Carlos Blanco, New York State Psychiatric Institute and the Department of Psychiatry, Columbia University College of Physicians and Surgeons, New York City..
References
- 1.Centers for Disease Control and Prevention Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children—United States, 2003 and 2007. Morbidity and Mortality Weekly Report. 2010;59:1439–1443. [PubMed] [Google Scholar]
- 2.Polanczyk G, de Lima MS, Horta BL, et al. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. American Journal of Psychiatry. 2007;164:942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 3.Able SL, Johnston JA, Adler LA, et al. Functional and psychosocial impairment in adults with undiagnosed ADHD. Psychological Medicine. 2007;37:97–107. doi: 10.1017/S0033291706008713. [DOI] [PubMed] [Google Scholar]
- 4.Barkley RA, Fischer M, Smallish L, et al. Young adult outcome of hyperactive children: adaptive functioning in major life activities. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 5.Barkley RA, Guevremont DC, Anastopoulos AD, et al. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3- to 5-year follow-up survey. Pediatrics. 1993;92:212–218. [PubMed] [Google Scholar]
- 6.Swensen A, Birnbaum HG, Ben Hamadi R, et al. Incidence and costs of accidents among attention-deficit/hyperactivity disorder patients. Journal of Adolescent Health. 2004;35:e1–e9. [PubMed] [Google Scholar]
- 7.Mannuzza S, Klein RG, Bessler A, et al. Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Archives of General Psychiatry. 1993;50:565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Lane M, Stang PE, et al. The prevalence and workplace costs of adult attention deficit hyperactivity disorder in a large manufacturing firm. Psychological Medicine. 2009;39:137–147. doi: 10.1017/S0033291708003309. [DOI] [PubMed] [Google Scholar]
- 9.Barkley RA, Fischer M, Smallish L, et al. Young adult follow-up of hyperactive children: antisocial activities and drug use. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2004;45:195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 10.Faraone SV, Biederman J, Spencer T, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? American Journal of Psychiatry. 2006;163:1720–1729. doi: 10.1176/ajp.2006.163.10.1720. [DOI] [PubMed] [Google Scholar]
- 11.Dopheide JA, Pliszka SR. Attention-deficit-hyperactivity disorder: an update. Pharmacotherapy. 2009;29:656–679. doi: 10.1592/phco.29.6.656. [DOI] [PubMed] [Google Scholar]
- 12.Epstein JN, Langberg JM, Lichtenstein PK, et al. Community-wide intervention to improve the attention-deficit/hyperactivity disorder assessment and treatment practices of community physicians. Pediatrics. 2008;122:19–27. doi: 10.1542/peds.2007-2704. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein S. Is ADHD a growth industry? Journal of Attention Disorders. 2006;9:461–464. doi: 10.1177/1087054705283678. [DOI] [PubMed] [Google Scholar]
- 14.Okie S. ADHD in adults. New England Journal of Medicine. 2006;354:2637–2641. doi: 10.1056/NEJMp068113. [DOI] [PubMed] [Google Scholar]
- 15.Zuvekas SH, Vitiello B, Norquist GS. Recent trends in stimulant medication use among US children. American Journal of Psychiatry. 2006;163:579–585. doi: 10.1176/ajp.2006.163.4.579. [DOI] [PubMed] [Google Scholar]
- 16.Froehlich TE, Lanphear BP, Epstein JN, et al. Prevalence, recognition, and treatment of attention-deficit/hyperactivity disorder in a national sample of US children. Archives of Pediatrics and Adolescent Medicine. 2007;161:857–864. doi: 10.1001/archpedi.161.9.857. [DOI] [PubMed] [Google Scholar]
- 17.Visser SN, Lesesne CA, Perou R. National estimates and factors associated with medication treatment for childhood attention-deficit/hyperactivity disorder. Pediatrics. 2007;119(suppl 1):S99–S106. doi: 10.1542/peds.2006-2089O. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brinkman WB, Sherman SN, Zmitrovich AR, et al. Parental angst making and revisiting decisions about treatment of attention-deficit/hyperactivity disorder. Pediatrics. 2009;124:580–589. doi: 10.1542/peds.2008-2569. [DOI] [PubMed] [Google Scholar]
- 20.Sayal K, Goodman R, Ford T. Barriers to the identification of children with attention deficit/hyperactivity disorder. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2006;47:744–750. doi: 10.1111/j.1469-7610.2005.01553.x. [DOI] [PubMed] [Google Scholar]
- 21.Winterstein AG, Gerhard T, Shuster J, et al. Utilization of pharmacologic treatment in youths with attention deficit/hyperactivity disorder in Medicaid database. Annals of Pharmacotherapy. 2008;42:24–31. doi: 10.1345/aph.1K143. [DOI] [PubMed] [Google Scholar]
- 22.Wang PS, Berglund P, Olfson M, et al. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:603–613. doi: 10.1001/archpsyc.62.6.603. [DOI] [PubMed] [Google Scholar]
- 23.Graetz BW, Sawyer MG, Baghurst P. Gender differences among children with DSM-IV ADHD in Australia. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:159–168. doi: 10.1097/00004583-200502000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Grant B, Dawson D, Hasin D. The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, Md: 2007. Available at www.niaaa.nih.gov. [Google Scholar]
- 25.Fikretoglu D, Liu A, Pedlar D, et al. Patterns and predictors of treatment delay for mental disorders in a nationally representative, active Canadian military sample. Medical Care. 2010;48:10–17. doi: 10.1097/MLR.0b013e3181bd4bf9. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Brown RL, Broman CL. Sex differences in psychiatric help-seeking: evidence from four large-scale surveys. Journal of Health and Social Behavior. 1981;22:49–64. [PubMed] [Google Scholar]
- 27.Grant BF, Stinson FS, Dawson DA, et al. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- 28.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Molecular Psychiatry. 2009;14:1051–1066. doi: 10.1038/mp.2008.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grant B, Dawson D, Hasin D. The Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version. National Institute on Alcohol Abuse and Alcoholism; Bethesda, Md: 2007. Available at www.niaaa.nih.gov. [Google Scholar]
- 30.Kieling C, Kieling RR, Rohde LA, et al. The age at onset of attention deficit hyperactivity disorder. American Journal of Psychiatry. 2010;167:14–16. doi: 10.1176/appi.ajp.2009.09060796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Dependence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Petry NM, Stinson FS, Grant BF. Comorbidity of DSM-IV pathological gambling and other psychiatric disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:564–574. doi: 10.4088/jcp.v66n0504. [DOI] [PubMed] [Google Scholar]
- 33.Grant B, Moore T, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Bethesda, MD: 2003. [Google Scholar]
- 34.Canino G, Bravo M, Ramírez R, et al. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability and concordance with clinical diagnoses in a Hispanic population. Journal of Studies on Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- 35.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule–IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 36.Grant BF, Hasin DS, Stinson FS, et al. Prevalence, correlates, and disability of personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2004;65:948–958. doi: 10.4088/jcp.v65n0711. [DOI] [PubMed] [Google Scholar]
- 37.Grant BF, Hasin DS, Blanco C, et al. The epidemiology of social anxiety disorder in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:1351–1361. doi: 10.4088/jcp.v66n1102. [DOI] [PubMed] [Google Scholar]
- 38.Grant BF, Hasin DS, Stinson FS, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:363–374. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- 39.Hasin DS, Goodwin RD, Stinson FS, et al. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 40.Hasin D, Carpenter KM, McCloud S, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- 41.Grant BF, Harford TC, Dawson DA, et al. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- 42.Hasin D, Paykin A. Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcoholism, Clinical and Experimental Research. 1999;23:144–150. [PubMed] [Google Scholar]
- 43.Hasin DS, Grant B, Endicott J. The natural history of alcohol abuse: implications for definitions of alcohol use disorders. American Journal of Psychiatry. 1990;147:1537–1541. doi: 10.1176/ajp.147.11.1537. [DOI] [PubMed] [Google Scholar]
- 44.Hasin DS, Schuckit MA, Martin CS, et al. The validity of DSM-IV alcohol dependence: what do we know and what do we need to know? Alcoholism, Clinical and Experimental Research. 2003;27:244–252. doi: 10.1097/01.ALC.0000060878.61384.ED. [DOI] [PubMed] [Google Scholar]
- 45.Software for Survey Data Analysis (SUDAAN), Version 9.0. Research Triangle Institute; Research Triangle Park, NC: 2004. [Google Scholar]
- 46.Agresti A. Categorical Data Analysis. Wiley; Hoboken, NJ: 2002. [Google Scholar]
- 47.Wang PS, Angermeyer M, Borges G, et al. Delay and failure in treatment seeking after first onset of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry. 2007;6:177–185. [PMC free article] [PubMed] [Google Scholar]
- 48.Olfson M, Kessler RC, Berglund PA, et al. Psychiatric disorder onset and first treatment contact in the United States and Ontario. American Journal of Psychiatry. 1998;155:1415–1422. doi: 10.1176/ajp.155.10.1415. [DOI] [PubMed] [Google Scholar]
- 49.Kessler RC, Olfson M, Berglund PA. Patterns and predictors of treatment contact after first onset of psychiatric disorders. American Journal of Psychiatry. 1998;155:62–69. doi: 10.1176/ajp.155.1.62. [DOI] [PubMed] [Google Scholar]
- 50.Wang PS, Berglund PA, Olfson M, et al. Delays in initial treatment contact after first onset of a mental disorder. Health Services Research. 2004;39:393–415. doi: 10.1111/j.1475-6773.2004.00234.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mojtabai R, Olfson M, Mechanic D. Perceived need and help-seeking in adults with mood, anxiety, or substance use disorders. Archives of General Psychiatry. 2002;59:77–84. doi: 10.1001/archpsyc.59.1.77. [DOI] [PubMed] [Google Scholar]
- 52.Sayal K, Ford T, Goodman R. Trends in recognition of and service use for attention-deficit hyperactivity disorder in Britain, 1999–2004. Psychiatric Services. 2010;61:803–810. doi: 10.1176/ps.2010.61.8.803. [DOI] [PubMed] [Google Scholar]
- 53.Karam RG, Bau CH, Salgado CA, et al. Late-onset ADHD in adults: milder, but still dysfunctional. Journal of Psychiatric Research. 2009;43:697–701. doi: 10.1016/j.jpsychires.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 54.Zepf FD. Attention deficit-hyperactivity disorder and early-onset bipolar disorder: two facets of one entity? Dialogues in Clinical Neuroscience. 2009;11:63–72. doi: 10.31887/DCNS.2009.11.1/fdzepf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Olfson M, Liu SM, Grant BF, et al. Influence of comorbid mental disorders on time to seeking treatment for major depressive disorder. Medical Care. 2012;50:227–232. doi: 10.1097/MLR.0b013e318241eb5e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kirana PS, Rosen R, Hatzichristou D. Subjective well-being as a determinant of individuals’ responses to symptoms: a bio-psychosocial perspective. International Journal of Clinical Practice. 2009;63:1435–1445. doi: 10.1111/j.1742-1241.2009.02183.x. [DOI] [PubMed] [Google Scholar]
- 57.Cohen AS, Emmerson LC, Mann MC, et al. Schizotypal, schizoid and paranoid characteristics in the biological parents of social anhedonics. Psychiatry Research. 2010;178:79–83. doi: 10.1016/j.psychres.2008.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Linden M, Vilain M. Minimal emotional dysfunction and first impression formation in personality disorders [in German]. Der Nervenarzt. 2011;82:25–36. doi: 10.1007/s00115-010-3160-z. [DOI] [PubMed] [Google Scholar]
- 59.Mann MC, Vaughn AG, Barrantes-Vidal N, et al. The schizotypal ambivalence scale as a marker of schizotypy. Journal of Nervous and Mental Disease. 2008;196:399–404. doi: 10.1097/NMD.0b013e3181710900. [DOI] [PubMed] [Google Scholar]
- 60.van Manen JG, Andrea H, van den Eijnden E, et al. Relationship between patient characteristics and treatment allocation for patients with personality disorders. Journal of Personality Disorders. 2011;25:656–667. doi: 10.1521/pedi.2011.25.5.656. [DOI] [PubMed] [Google Scholar]
- 61.Martényi F, Treuer T, Gau SS, et al. Attention-deficit/hyperactivity disorder diagnosis, co-morbidities, treatment patterns, and quality of life in a pediatric population in central and eastern Europe and Asia. Journal of Child and Adolescent Psychopharmacology. 2009;19:363–376. doi: 10.1089/cap.2008.0148. [DOI] [PubMed] [Google Scholar]
- 62.Ginsberg Y, Hirvikoski T. Lindefors N: Attention Deficit Hyperactivity Disorder (ADHD) among longer-term prison inmates is a prevalent, persistent and disabling disorder. BMC Psychiatry. 2010;10:112. doi: 10.1186/1471-244X-10-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rösler M, Retz W, Retz-Junginger P, et al. Prevalence of attention deficit-/hyperactivity disorder (ADHD) and comorbid disorders in young male prison inmates. European Archives of Psychiatry and Clinical Neuroscience. 2004;254:365–371. doi: 10.1007/s00406-004-0516-z. [DOI] [PubMed] [Google Scholar]
- 64.Pickles A, Pickering K, Simonoff E, et al. Genetic “clocks” and “soft” events: a twin model for pubertal development and other recalled sequences of developmental milestones, transitions, or ages at onset. Behavior Genetics. 1998;28:243–253. doi: 10.1023/a:1021615228995. [DOI] [PubMed] [Google Scholar]
- 65.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication—Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]