Abstract
BACKGROUND:
Lower esophageal sphincter vector volume (V-V) was developed in the late 1980’s by Bombeck, as a quantification of sphincter integrity used to select reflux patients with a defective valve who may benefit from surgery. Its calculation required motorized pull-through of an 8-lumen water perfused manometry catheter with subsequent computerized reconstruction of sphincter morphology. Recently, a 3D-high resolution manometry (3D-HRM) assembly (Given Imaging, Duluth, GA) has been developed with the potential to assess real-time V-V.
The aim of this study was to assess the feasibility of the calculation of V-V using the 3D-HRM assembly and to compare measures of its value using real-time 3D-HRM to simulated analogous measures.
METHODS:
Eight asymptomatic controls (4F, ages 26-49) were studied in a supine position with a solid-state 3D-HRM assembly positioned across the esophagogastric junction (EGJ). The 9 cm 3D segment was comprised of 12 rings of 8 radially dispersed pressure sensors, each 2.5 mm long and spaced 7.5 mm apart on center. Recordings were done during normal respiration: 1) with the 3D-HRM segment in a stationary position across the EGJ and 2) during a station pull-through of the 3D-HRM segment withdrawing it across the EGJ at 5-mm increments with each position held for 30 s. EGJ cross sectional vector areas (CSVA) were computed using the irregular polygon area formula: CSVA = sin (360/n)/2×(P1×P2+P2×P3+…+Pn×P1), and n=8 radial sensors. V-V was computed as the sum of CSVAs at inspiration and end-expiration by three methods: real-time 3D-HRM, 3-station composite, and single sensor ring measurements.
RESULTS:
There were no statistic differences among the methods and all methods showed significant differences between inspiration and expiration.
CONCLUSIONS:
Calculation of real-time V-V is feasible using the 3D-HRM. Moreover, the results of this study highlighted the potential primary role of the diaphragmatic hiatus in the pathophysiology of GERD and the under-recognized but crucial role of the crural repair during the anti-reflux surgery.
INTRODUCTION
Characterizing EGJ barrier function is complicated by both its dynamic nature and complex anatomy. Over the years, a variety of manometric methodologies and metrics have been proposed to quantify this enigmatic sphincter: sphincter length and respiratory inversion point (RIP) were described to determine the intra-abdominal lower esophageal sphincter (LES) length as a predictor of fundoplication efficacy 1. However, sphincter length, or intra-abdominal length, speaks nothing to the magnitude of closure forces at the EGJ. Early on, it was recognized that there was substantial asymmetry of these closure forces both radially and along the length of the sphincter. Consequently, Bombeck and colleagues developed the concept of LES vector volume (V-V) in the late 1980s as a quantification of sphincter integrity 1,2. The determination of V-V required a motorized pull-through of an 8-lumen water-perfused manometry catheter with the lumens radially dispersed 45° apart and the rate of pull-though held constant so that the time axis of the plot became indicative of high-pressure zone length. The resultant data were then reconstructed into an 8-sided polygonal solid representing 3D sphincter pressure morphology and quantitative norms were established for the volume of that solid to define reflux patients with a defective valve who may benefit from surgery 1,3,4. However, since the description of the V-V, the method has not been widely used. This may relate to the obsolescence of the requisite apparatus, the impracticality of the testing procedure, and/or the requirement that the V-V measurement be done during suspended respiration.
Recently, a 3D-high resolution manometry (3D-HRM) assembly (Given Imaging, Duluth, GA) has been developed 5 with the potential to greatly simplify the assessment of EGJ V-V. The 3D segment of the array permits high resolution recording both axially and radially while maintaining a stationary position. Consequently, 3D-HRM should allow for the measurement of V-V that was only possible with pull-through maneuvers in the past and this measurement can be made in real time permitting analysis of the respiratory effect. Hence, the aim of this study was to assess the feasibility of the calculation of EGJ V-V using the 3D-HRM assembly and to compare measures of its value using real-time 3D-HRM to analogous measures made using simulations of a conventional manometric catheter and pull-through methodology.
METHODS
Subjects
Eight volunteers were recruited for this study. None of them had a history of prior gastrointestinal surgery, significant medical disease, or current use of medications for upper gastrointestinal symptoms. All subjects underwent a brief interview and examination and gave written informed consent. Dysphagia was assessed using the Impaction Dysphagia Questionnaire (IDQ, maximal score: 50; 95th percentile cutoff in controls: 2). Reflux symptoms were measured using the GerdQ (scale 0-18; positive for GERD if score ≥7) 6. The study protocol was approved by the Northwestern University Institutional Review Board.
Manometric assembly
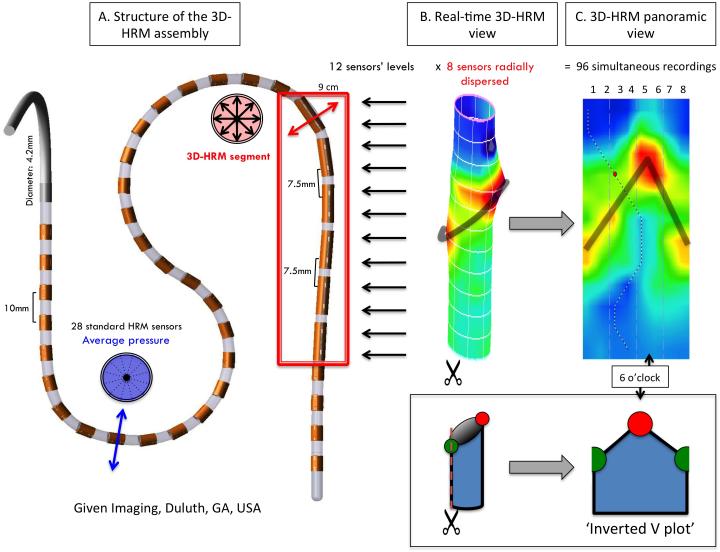
The 3D-HRM assembly (ManoScan 3D, Given Imaging, Duluth, GA) was a 128-channel solid-state device incorporating a 9.0 cm 3D-HRM segment into an otherwise standard HRM array. The 4.2 mm outer diameter assembly had the 3D-HRM segment positioned between 28 proximal and 4 distal standard sensing elements spaced 1 cm apart 5. Each standard sensor averaged the pressure signals from the 12 radially dispersed sensors into a single circumferential pressure value. The 3D segment was comprised of 12 rings of 8 radially dispersed independent pressure sensors with the rings spaced 7.5 mm apart (Figure 1A). The individual 3D sensing elements were 2.5 mm long and separated from the adjacent element by 5 mm. Consequently, the 9 cm 3D segment provided 96 independent pressure recordings with a radial resolution of 45° and an axial resolution of 7.5 mm (Figures 1B&1C). The data acquisition frequency was 100 Hz.
Figure 1.
Characteristics of the 3D-HRM assembly and resulting 3D-HRM views. Panel A is a representation of the 3D-HRM catheter composed of the assembly of 32 standard HRM sensors and 12 levels of 8 radially dispersed sensors. The resulting image is a cylinder (Panel B) that can be unfolded for the 3D-HRM panoramic view (Panel C). The insert shows a schematic representation of a plane that cuts the cylinder and appears as an inverted-V plot in the panoramic view.
Prior to recording, the manometric assembly was calibrated at zero and 300 mmHg using the manufacturer’s calibration chamber. The individual elements of the 3D array had a specified accuracy of ±1 mmHg for the pressure range of 0-50 mmHg and ± 1.5 mmHg in the 50-100 mmHg range. Accuracy was confirmed using the manufacturer’s pressure chamber but also by applying pressure with a sphygmomanometer from 10 to 150 mmHg in increments of 10 mmHg 7. All pressure measurements were referenced to atmospheric pressure.
Manometry protocol
Studies were performed in the supine position after a 6-hour fast. The assembly was passed transnasally and positioned with the 3D-HRM segment straddling the EGJ. After a period of accommodation, five minutes of baseline recording was obtained during which the subjects were asked to breathe normally. A standard 10 water swallow protocol was obtained to verify that the subjects had normal motility according to the Chicago Classification 8.
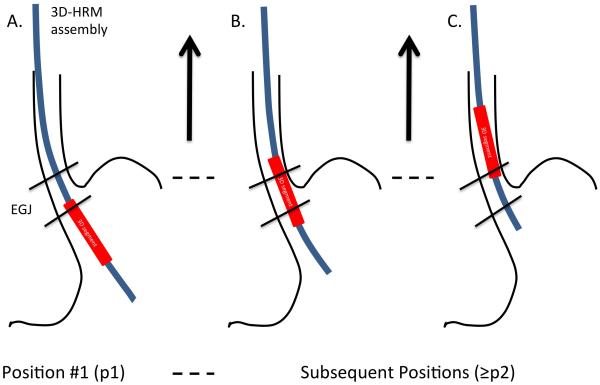
The assembly was then repositioned with the 3D segment in the stomach and a station pull-through was obtained withdrawing the assembly at 5 mm increments with each station held for at least 30 seconds (Figure 2). The pull-through was done maintaining normal respiration, with the patient asked to minimize swallowing. The pull-through was continued until the 3D array had traversed the EGJ and the distance to the nares was recorded for each station.
Figure 2.
Position of the 3D-HRM segment during the station pull-through protocol, utilized for the calculation of vector volume. A) Initial position, with the upper sensors’ level positioned to record the lower part of the EGJ area. B) Intermediate position during the pull-through, used for the 3D real-time calculation of V-V. C) Final position, with lower sensors’ level positioned to record the upper part of the EGJ area.
Data analysis
Data were analyzed after thermal compensation using Manoview software (version 3.0, Given Imaging, Duluth, GA) and/or Excel (Microsoft, Redmond Washington) after transfer of the raw data files. Analyses were constructed to compare calculations of vector volume made with real-time 3D-HRM to the same measures made using 2 different methods for simulating conventional manometry from the pull through protocol.
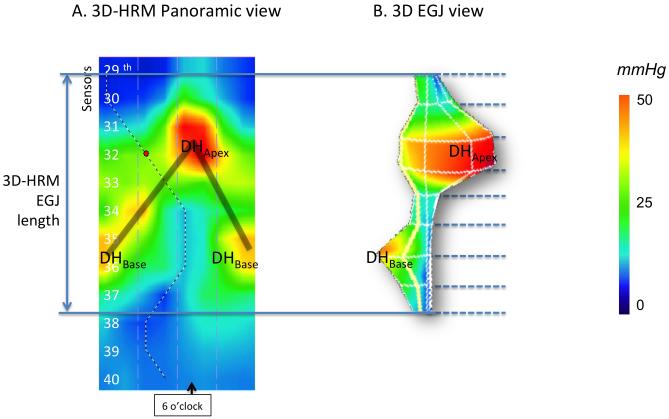
EGJ length was determined as the high pressure zone appearing as an inverted-V shape on 3D-HRM 9, whose upper and lower margins were defined by a 2 mmHg pressure increase relative to gastric pressure. As previously described 9, the method for EGJ length calculation included both the intrinsic sphincter (LES) and the diaphragmatic hiatus (DH) pressure components (Figure 3). The DH pressure signature appeared as an inverted-V at rest (Figure 3A), and LES pressure was almost nonexistent. Thus, measuring the pressurization generated by LES was not possible independently of the pressure attributable to the DH. Thus, the high-pressure zone measured the full EGJ length, representing the extreme limits of the inverted-V plot (Figure 3A), not restricted to the LES length. On the other hand, due to the asymmetric EGJ pressure signature (Figure 3) evident with 3D-HRM, the peak pressure recorded using a single sensor method, might be either the base of the crural diaphragm (DHBase), the apex of the crural diaphragm pressure signature (DHApex), or somewhere in between.
Figure 3.
Panel A. Representative example of 3D-HRM still images, illustrating the discrete pressure peaks within the EGJ at end-expiration. The blue vertical arrows represent the locus of EGJ length in 3D-HRM. The shaded ‘V’ on the topography plots indicates the disposition of the split diaphragm signal, formed by the apex of the hiatal diaphragm (DHApex) and the base of the hiatal diaphragm (DHBase). Panel B. 3D representation of the EGJ, generated by the Manoview™ software is a real time representation of the EGJ V-V (dotted lines separate the EGJ by 0.75 cm sections).
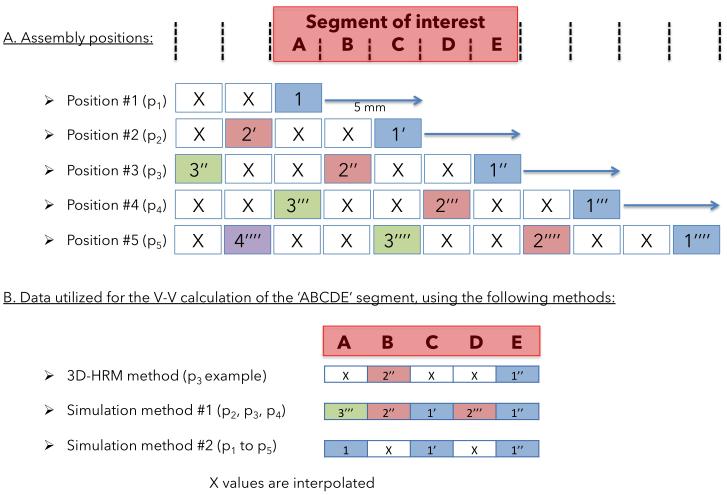
As originally described by Bombeck, Vector Volume is a measure of EGJ integrity calculated from a motorized pull-through across the EGJ with eight radially dispersed pressure sensors 2. At each incremental position, cross sectional vector area (CSVA) was computed using the irregular polygon area formula (CSVA = sin (360/n)/2×(P1×P2 + P2×P3 + … + Pn×P1), with n=8 radial sensors). Hence, the V-V calculation requires that EGJ length be predefined and that radial pressure data be defined for every incremental position within that length. Given that each pressure-sensing element on the 3D-HRM assembly was 2.5 mm in length, we used this as the incremental length for V-V calculations. However, that approach resulted in there being two 2.5 mm gaps between each 2.5 mm sensing element. Three alternative methods were utilized to fill these gaps in the data set (Figure 4):
Figure 4.
Schematic representation of the methodology used for the calculation of EGJ V-V. A. Assembly positions during the pull-through protocol with 5 mm increments. The pressure of the segment of interest (red box) is recorded by the pressure sensors during the pull-through protocol, either by a single sensor or by different sensors. B. Utilization of the recorded data using 3 different methods for the V-V calculation.
The real-time calculation of V-V was a 3D-HRM method using a single assembly position and cubic spline interpolation between pressure sensors;
Simulation method #1 of a conventional manometry pull-through used composite data from three assembly positions during the pull-through done in 5 mm increments; this method required no interpolation;
Simulation method #2 of a conventional manometry pull-through utilized data from a single sensor ring of the assembly at each 5 mm increment of the pull-through; this method required that the 2.5 mm gap not assessed by a pressure sensor be approximated with cubic spline interpolation.
Statistical Analysis
Results between manometric methods were compared using the Wilcoxon and Friedman tests for the dependent variables. Correlation among the different methods for the calculation of V-V was assessed by using the Pearson correlation coefficient. Data were summarized as median [25th-75th percentile], unless stated otherwise. A p<0.05 was considered significant.
RESULTS
Subjects
Eight subjects (4F, ages 31 [26, 49]) were recruited for the study. All had normal IDQ and GerdQ scores. All subjects successfully completed the intended protocol.
Length of the EGJ
Using the 3D-HRM, the full EGJ measured 6.0 cm long [5.8-7.0] representing the extreme limits of the inverted-V plot (Figure 3A), and was used for the calculation of EGJ V-V. The length of the DHApex pressure peak was 3.8cm [3.0-4.2], and the length of the DHBase pressure peak was 2.6cm [2.3-3.4].
Determination of Vector volume
Table 1 illustrates an example of the process for the determination of EGJ V-V using the 3D-HRM real-time method in inspiration and end-expiration. The calculation of EGJ V-V in this table is the sum of the cross sectional vector areas and the interpolated pressures. Thus the EGJ V-V value incrementally increases when we include a progressively longer segment for the EGJ length. Table 1 also highlights the EGJ asymmetry, which is evident on the 3D representation of EGJ V-V (Figure 3B); this asymmetry is both radial and axial with 2 distinct axial pressure peaks.
Table 1.
Example of pressures recorded at inspiration and end-expiration, with corresponding EGJ V-V (mmHg2.mm) calculated using the 3D-HRM real-time method.
| a. Data at inspiration |
| EGJ segments (cm) |
Radial pressure recording (mmHg) |
EGJ V-V(mmHg.mm) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0° | 45° | 90° | 135° | 180° | 225° | 270° | 315° | Segmental Contribution (%) |
Cumulative contribution |
|
|
| ||||||||||
| 0-0.75 | −1.2 | −0.4 | −0.9 | −0.1 | −1.8 | −0.7 | 0.6 | −1.8 | 1.1 (0.1) |
1.1 |
| 0.75-1.5 | 2.9 | 2.9 | 2.8 | 6.6 | 40.4 | 35.7 | 51.8 | 5.4 | 3199.7 (18.0) |
3200.8 |
| 1.5-2.25 | 50.4 | 24.0 | 21.1 | 18.2 | 16.9 | 14.0 | 14.3 | 16.6 | 4147.1 (23.3) |
7347.9 |
| 2.25-3 | 2.0 | 1.1 | 3.8 | 16.3 | 54.7 | 40.3 | 24.2 | 34.2 | 5077.4 (28.6) |
12425.3 |
| 3-3.75 | 2.5 | 2.7 | 5.4 | 8.6 | 12.9 | 8.4 | 2.1 | 0.4 | 1440.4 (8.1) |
13865.7 |
| 3.75-4.5 | −1.8 | −0.6 | 0.6 | −1.8 | 1.2 | 0.9 | 4.4 | 2.1 | 79.4 (0.4) |
13945.1 |
| 4.5-5.25 | 40.1 | 35.7 | 51.8 | 5.4 | −1.2 | −0.2 | −0.8 | −0.1 | 2924.6 (16.4) |
16869.8 |
| 5.25-6 | 1.1 | 0.8 | 4.3 | 2.1 | 2.5 | 2.5 | 5.3 | 8.6 | 911.6 (5.1) | 17781.4 |
| b. Data at end-expiration |
| EGJ segments (cm) |
Radial pressure recording (mmHg) |
EGJ V-V(mmHg.mm) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0° | 45° | 90° | 135° | 180° | 225° | 270° | 315° | Segmental Contribution (%) |
Cumulative contribution |
|
|
| ||||||||||
| 0-0.75 | 3.9 | 7.2 | 4.7 | 4.5 | 4.4 | 5.1 | 5.8 | 5.8 | 74.6 (0.6) |
74.6 |
| 0.75-1.5 | 2.5 | 2.5 | 2.5 | 4.7 | 17.8 | 31.8 | 50.0 | 9.2 | 2313.4 (17.4) |
2388.1 |
| 1.5-2.25 | 21.3 | 15.3 | 14.1 | 12.8 | 11.6 | 8.4 | 8.9 | 10.7 | 1772.4 (13.3) |
4160.5 |
| 2.25-3 | 5.6 | 6.7 | 19.6 | 39.0 | 27.0 | 17.3 | 26.2 | 32.3 | 3564.7 (26.8) |
7725.2 |
| 3-3.75 | 10.3 | 8.8 | 11.9 | 16.2 | 13.6 | 6.0 | 6.1 | 5.8 | 1605.2 (12.0) |
9330.4 |
| 3.75-4.5 | 4.5 | 5.3 | 6.1 | 6.4 | 6.6 | 11.1 | 8.8 | 10.8 | 566.6 (4.3) |
9897.0 |
| 4.5-5.25 | 18.0 | 31.8 | 50.1 | 9.3 | 4.0 | 7.3 | 4.8 | 4.5 | 2442.5 (18.3) |
12339.5 |
| 5.25-6 | 11.6 | 8.4 | 9.0 | 10.7 | 2.5 | 2.5 | 2.5 | 4.7 | 977.5 (7.3) | 13317.0 |
Table 2 compares EGJ-V-V calculations between inspiration and end expiration among the 3 different methods. The Pearson correlation between the different 3 measurements for the calculation of the V-V was excellent; the worst correlation was r> 0.85; p<0.05. There were no statistic differences among the methods and all methods showed significant differences between inspiration and expiration.
Table 2.
Values of EGJ V-V (mmHg2 × mm) in inspiration and expiration using 3 different methods for its calculation (Median [IQR]).
| 3D-HRM | Pull-through method 1 |
Pull-through method 2 |
Worst Correlation |
Friedman’s test | |
|---|---|---|---|---|---|
|
EGJ V-V
Inspiration |
16000 [15350- 17000] |
17200 [16000- 19450] |
15400 [11300- 19300] |
r>0.95; p<0.05 | p=0.311 |
|
EGJ V-V
Expiration |
14400 [13000- 15000] |
15400 [14350- 18400] |
11900 [10600- 17000] |
r>0.85; p<0.05 | p=0.223 |
Wilcoxon test: p<0.05 between inspiration and expiration for the 3 methods
DISCUSSION
This study demonstrated that a novel 3D-HRM manometric device, comprised of a 96-sensor array, permitted the calculation of EGJ vector volume, using either a real-time imaging method or simulation of a pull-through protocol, resulting in statistically similar values.
The key advantages of the 3D-HRM method is that since the data are obtained with the device in a stationary position, instantaneous, dynamic measurements can be made for extended periods. Although this method required interpolation of data between recording sites positioned 7.5 mm apart on center, our findings suggest that this degree of interpolation had no significant impact on the V-V calculations. The dynamic recordings of V-V obtained by 3D HRM graphically illustrated the dominant role of the diaphragmatic hiatus in the overall EGJ pressure morphology 9. Using the characteristic axial and radial asymmetry of the diaphragm as identifying criteria, the diaphragmatic hiatus contributed an estimated 85% to the total EGJ V-V. These observations are very much in line with the ‘pinch-cock’ model of the EGJ originally proposed by Allison in 1951 10. Since perturbations of EGJ anatomy are increasingly recognized as important pathophysiological contributions to GERD pathophysiology 11-13, these observations suggest that real-time recording of V-V may contribute important insights in future pathophysiological studies of GERD subgroups.
The values of EGJ V-V calculated using the 3D-HRM are substantially greater than those previously reported in the original description of the technique (8000 mmHg2.mm [5300-12250] at end expiration 2,14-16. This finding is partly due to the different manometric technology used for data gathering and partly attributable to the methodology used to calculate EGJ length. With respect to manometric technology, the response characteristics of perfusion manometry are such that one would anticipate a greatly dampened signal compared to the solid-state device used in the current study 17; this would lead to an underestimation of the cross-sectional vector area at each locus within the EGJ. However, the larger consideration is probably the spatial EGJ limits used to incorporate into the V-V calculation. Although no mention of the DH contribution was made in the previous literature, we suspect that the measurement was restricted to the first pressure peak surrounding the diaphragmatic apex (DHApex). Consistent with this supposition, when restricting the measurement to the DHApex length (3.8 cm), our methodology finds an EGJ V-V value that numerically correlates with the previously published values (Table 2).
EGJ pressure augmentation observed during inspiration is mainly due to diaphragmatic contraction. However, the radial asymmetry to the EGJ remains even in expiration suggesting that the diaphragmatic component of EGJ pressure can be detected throughout the respiratory cycle. Again, this is consistent with the pinchcock hypothesis put forth by Allison and also with the observation of a persistent high pressure zone at the hiatus in individuals who had previously undergone resection of the distal esophagus inclusive of the LES 18. Moreover, these observations highlight the cardinal contribution of the diaphragmatic hiatus to EGJ pressure morphology 9.
In conclusion, calculation of EGJ V-V is feasible using the 3D-HRM, which permits real-time EGJ V-V recording. Taken together with the more accurate determination of EGJ length and respiratory inversion point 9, the 3D-HRM device appears to be a promising new tool in the study of GERD pathophysiology. Moreover, we can make the assumption that the diaphragmatic hiatus plays an important role in the pathophysiology of GERD and speculate that the crural repair component of anti-reflux surgery might play a crucial, but still underestimated role. Further pathophysiological studies are mandatory in subgroups of GERD patients with reflux and with and without hiatus hernia in the hopes of evolving this into a valuable clinically technique.
ACKNOWLEDGMENT
This work was supported by R01 DK56033 (PJK) and R01 DK079902 (JEP) from the National Institutes of Health, USA.
Abbreviations
- LES
lower esophageal sphincter
- EGJ
esophagogastric junction
- GERD
gastroesophageal reflux disease
- 3D-HRM
three dimensional high resolution manometry
- EPT
esophageal pressure topography
- RIP
respiratory inversion point
- V-V
vector volume
Footnotes
DISCLOSURES
No relevant competing financial and other interests exist for Frédéric Nicodème, Nathaniel J. Soper, Zhiyue Lin, John E. Pandolfino or Peter J. Kahrilas.
REFERENCES
- 1.Stein HJ, DeMeester TR. Who benefits from antireflux surgery? World J Surg. 1992;16(2):313–319. doi: 10.1007/BF02071539. [DOI] [PubMed] [Google Scholar]
- 2.Bombeck CT, Vaz O, DeSalvo J, Donahue PE, Nyhus LM. Computerized axial manometry of the esophagus. A new method for the assessment of antireflux operations. Annals of Surgery. 1987;206(4):465–472. doi: 10.1097/00000658-198710000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stein HJ, Korn O, Liebermann-Meffert D. Manometric vector volume analysis to assess lower esophageal sphincter function. Ann Chir Gynaecol. 1995;84(2):151–158. [PubMed] [Google Scholar]
- 4.Wetscher GJ, Hinder RA, Perdikis G, Wieschemeier T, Stalzer R. Three-dimensional imaging of the lower esophageal sphincter in healthy subjects and gastroesophageal reflux. Dig Dis Sci. 1996;41(12):2377–2382. doi: 10.1007/BF02100131. [DOI] [PubMed] [Google Scholar]
- 5.Kwiatek MA, Pandolfino JE, Kahrilas PJ. 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil. 2011;23(11):e461–e469. doi: 10.1111/j.1365-2982.2011.01733.x. doi:10.1111/j.1365-2982.2011.01733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro□oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30(10):1030–1038. doi: 10.1111/j.1365-2036.2009.04142.x. [DOI] [PubMed] [Google Scholar]
- 7.Nicodème F, Pandolfino JE, Lin Z, Xiao Y, Escobar G, Kahrilas PJ. Adding a radial dimension to the assessment of esophagogastric junction relaxation: validation studies of the 3D-eSleeve. AJP: Gastrointestinal and Liver Physiology. 2012;303(3):G275–80. doi: 10.1152/ajpgi.00063.2012. doi:10.1152/ajpgi.00063.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. doi:10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nicodème F, Lin Z, Pandolfino JE, Kahrilas PJ. Esophagogastric Junction pressure morphology: comparison between a station pull-through and real-time 3D-HRM representation. Neurogastroenterol Motil. 2013;25(9):e591–8. doi: 10.1111/nmo.12168. doi:10.1111/nmo.12168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allison PR. Reflux esophagitis, sliding hiatal hernia, and the anatomy of repair. Surg Gynecol Obstet. 1951;92(4):419–431. [PubMed] [Google Scholar]
- 11.Boeckxstaens GEE. Review article: the pathophysiology of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2007;26(2):149–160. doi: 10.1111/j.1365-2036.2007.03372.x. doi:10.1111/j.1365-2036.2007.03372.x. [DOI] [PubMed] [Google Scholar]
- 12.Pandolfino JE, Kim H, Ghosh SK, Clarke JO, Zhang Q, Kahrilas PJ. High-Resolution Manometry of the EGJ: An Analysis of Crural Diaphragm Function in GERD. Am J Gastroenterol. 2007;102(5):1056–1063. doi: 10.1111/j.1572-0241.2007.01138.x. doi:10.1111/j.1572-0241.2007.01138.x. [DOI] [PubMed] [Google Scholar]
- 13.Kahrilas PJ. GERD pathogenesis, pathophysiology, and clinical manifestations. Cleveland Clinic journal of medicine. 2003;70(Suppl 5):S4. doi: 10.3949/ccjm.70.suppl_5.s4. [DOI] [PubMed] [Google Scholar]
- 14.Andrade CG, Cecconello I, Nasi A, et al. Lower esophageal sphincter analysis using computerized manometry in patients with chagasic megaesophagus. Dis Esophagus. 2006;19(1):31–35. doi: 10.1111/j.1442-2050.2006.00534.x. doi:10.1111/j.1442-2050.2006.00534.x. [DOI] [PubMed] [Google Scholar]
- 15.Stein HJ, DeMeester T, Naspetti R, Jamieson J, Perry RE. Three-dimensional imaging of the lower esophageal sphincter in gastroesophageal reflux disease. Annals of Surgery. 1991;214(4):374. doi: 10.1097/00000658-199110000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Swift GL, Smith PM, McKirdy HC, Lowndes RH. Vector volume analysis of the lower esophageal sphincter in achalasia and the effect of balloon dilation. Dis Esophagus. 2001;14(1):54–56. doi: 10.1111/j.1442-2050.2001.00149.x. [DOI] [PubMed] [Google Scholar]
- 17.Dodds WJ, Stef JJ, Hogan WJ. Factors determining pressure measurement accuracy by intraluminal esophageal manometry. Gastroenterology. 1976;70(1):117–123. [PubMed] [Google Scholar]
- 18.Klein WA, Parkman HP, Dempsey DT, Fisher RS. Sphincterlike thoracoabdominal high pressure zone after esophagogastrectomy. Gastroenterology. 1993;105(5):1362–1369. doi: 10.1016/0016-5085(93)90140-8. [DOI] [PubMed] [Google Scholar]