Abstract
Objectives
Acetabular component orientation in total hip arthroplasty (THA) influences results. Intra-operatively, the natural arthritic acetabulum is often used as a reference to position the acetabular component. Detailed information regarding its orientation is therefore essential. The aim of this study was to identify the acetabular inclination and anteversion in arthritic hips.
Methods
Acetabular inclination and anteversion in 65 symptomatic arthritic hips requiring THA were measured using a computer navigation system. All patients were Caucasian with primary osteoarthritis (29 men, 36 women). The mean age was 68 years (SD 8). Mean inclination was 50.5° (SD 7.8) in men and 52.1° (SD 6.7) in women. Mean anteversion was 8.3° (SD 8.7) in men and 14.4° (SD 11.6) in women.
Results
The difference between men and women in terms of anteversion was significant (p = 0.022). In 75% of hips, the natural orientation was outside the safe zone described by Lewinnek et al (anteversion 15° ± 10°; inclination 40° ± 10°).
Conclusion
When using the natural acetabular orientation to guide component placement, it is important to be aware of the differences between men and women, and that in up to 75% of hips natural orientation may be out of what many consider to be a safe zone.
Cite this article: Bone Joint Res 2015;4:6–10.
Keywords: Total hip arthroplasty; THA, Acetabulum; Orientation; Arthritis; Computer, Navigation; Inclination; anteversion
Article focus
Acetabular orientation of 65 arthritic hips requiring total hip arthroplasty (THA) analysed using computer navigation as the method of measurement
Key messages
The mean arthritic acetabular inclination was 50.5° (sd 7.8) in men; 52.1° (sd 6.7) in women.
The mean anteversion was 8.3° (sd 8.7) in men and 14.4° (sd 11.6) in women. The difference between men and women in terms of anteversion was significant (p = 0.022)
In 75% of hips, the natural orientation was outside of the safe zone described by Lewinnek et al (anteversion 15° ± 10°; inclination 40° ± 10°).
Strengths and limitations
Knowledge of arthritic hip orientation can act as a good clinical guide for acetabular component orientation in THA
Accurate measurement machine
If registration of the pelvis is not right, it could potentially cause an error
Introduction
The success of total hip arthroplasty (THA) is closely linked to the positioning of the acetabular component. Malalignment increases rates of impingement, dislocation, acetabular migration, pelvic osteolysis and polyethylene wear.1-8 The natural anatomy of the arthritic acetabulum is used by many surgeons to guide acetabular component orientation. The bony acetabular rim can be used as reference points for orientating the acetabular component this way. Low rates of dislocation have been reported using this technique.9 Detailed understanding of the natural anatomy and orientation of the acetabulum in arthritic hips is therefore of great relevance.
Lewinnek et al4 described a ‘safe zone’ of acetabular component orientation (radiographic anteversion 15° ± 10°; radiographic inclination 40° ± 10°) and reported an increased rate of dislocation from 1.5% to 6.1% in hips falling outside of these ranges. Although not definitive, many surgeons accept this ‘safe zone’ as a target for orientation outcome.10 Other work has identified ‘safe zones’, with various ranges of inclination and anteversion, that also reduce rates of dislocation.5,7,11 Variability, between surgeons, of target angles for acetabular component orientation is influenced by surgical approach and the definition of acetabular component orientation used by the individual surgeon.12-14
The aim of this study was to describe the anteversion and inclination of the natural acetabulum in hips with primary osteoarthritis, in both men and women, and to identify the number that fall outside of the ‘safe zone’ described by Lewinnek et al4(anteversion 15° ± 10°; inclination 40° ± 10°).
Materials and Methods
This study was a retrospective data review and so was carried out under the clinical governance procedures of our institution. All patients with symptomatic primary osteoarthritis undergoing THA under the care of the senior author between January 2009 and May 2010 using one computer navigation system, were included. Patients operated on without using navigation, using a different navigation system or having incomplete data were excluded, as were those diagnosed with dysplastic hips (DDH), rheumatoid arthritis, slipped upper femoral epiphysis and previous trauma to the hip. Demographic data including age, gender, race, side of operation and body mass index (BMI) had been collected. In all cases, post-operative anteroposterior and lateral x-rays were taken. Computer-navigated THA was carried out using a commercially available non-image-based computer navigation system (Orthopilot, B. Braun Aesculap, Tuttlingen, Germany) as part of routine clinical care. Every procedure and therefore all measurements were carried out by a single consultant orthopaedic arthroplasty surgeon who was beyond the learning curve in computer-navigated THA, or by a registrar under his supervision. Rigid bodies (attached to active computer navigation trackers) were fixed to the pelvis and femur.The anterior pelvic plane was registered with a tracker using the two anterior superior iliac spines and pubic symphysis as reference points, in accordance with the navigation system workflow. The femoral head was then dislocated and removed. The fat pad and soft tissue was excised to clear the floor of the acetabulum. The acetabular labrum was excised to expose the bony acetabular rim margin, and any osteophytes were excised back to the level that, in the surgeon’s opinion, represented the original bony anatomy. The inner surface of the empty acetabulum was sized with acetabular component trials. The trial acetabular component of appropriate size, which fitted the acetabular cavity well, was attached to a computer tracker and then aligned in the orientation of the natural acetabulum as defined by the bony acetabular rim. This was done before any reaming of the acetabulum was attempted. This orientation was recorded by the computer software. The inclination and anteversion were calculated and stored by the computer software as radiographic inclination and anteversion in relation to the anterior pelvic plane as defined by Murray.15 Surgery then proceeded as routine with guidance of the computer navigation system.
Statistical analysis
SPSS 17.0 software (SPSS Inc, Chicago, Illinois) was used for statistical analysis. T-tests were used to test for differences between men and women for the measured orientations, and chi-squared tests were used to compare those falling outside of the limits defined by Lewinnek’s ‘safe zone’.4
Results
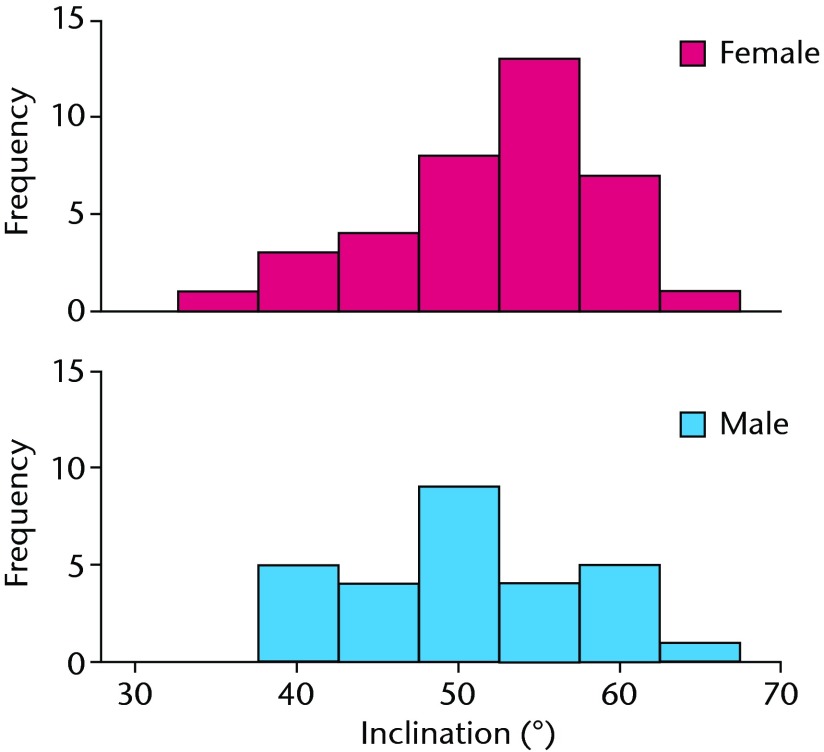
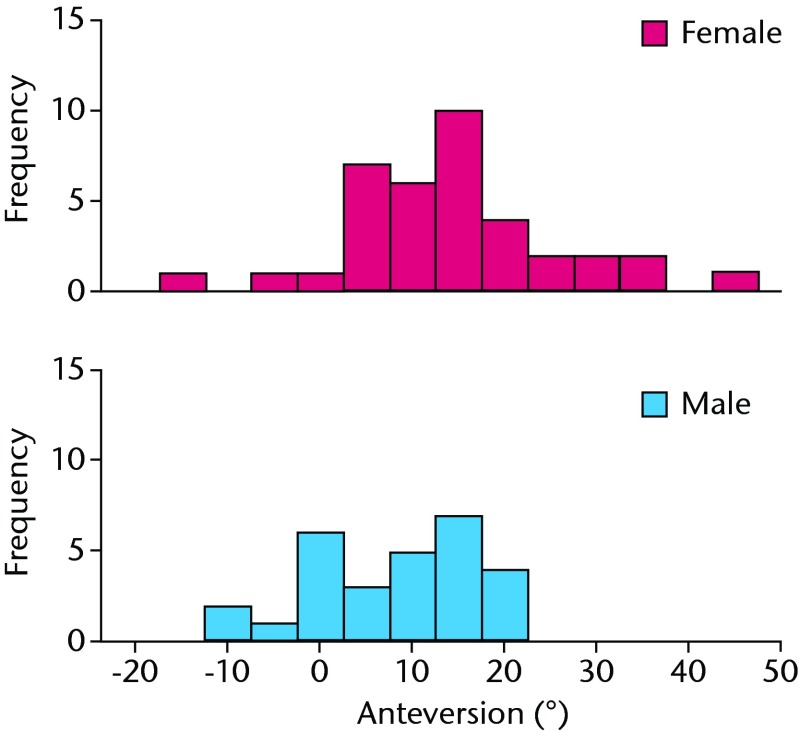
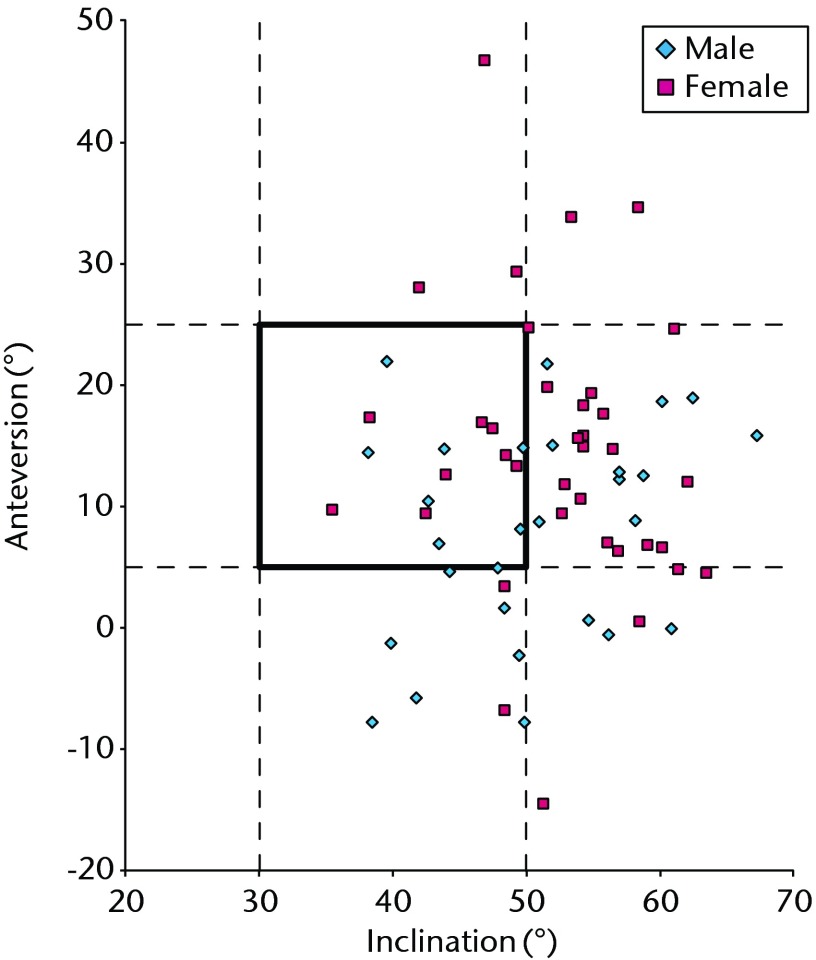
There were 143 THA during the time period. A total of 46 underwent operation without using computer navigation and 14 underwent operation using a different navigation system. Of the 83 patients fulfilling the inclusion criteria, 18 either met one of the exclusion criteria or did not have full data and were therefore excluded. This left a series of 65 hips in the study. There were 29 men and 36 women (33 right hips and 32 left hips). All patients were Caucasian and had primary osteoarthritis. The mean age was 68 years (sd 8) and mean BMI was 29 (sd 6.3). The mean natural acetabular inclination was 51.4° (sd 7.2), and mean anteversion was 11.7° (sd 10.7). There was no significant difference between men and women for inclination (Table I, Fig. 1). However, mean anteversion was significantly greater in women than men (Table I, Fig. 2). This did not equate to a statistically significant difference in the number of women compared with men that fell outside Lewinnek’s ‘safe zone’ (Table I). Overall, 75% of patients had an inclination or anteversion of the native acetabulum that fell outside Lewinnek’s ‘safe zone’ (Fig. 3).
Fig. 1.
Graph showing distribution of native acetabular inclination by gender.
Fig. 2.
Graph showing distribution of native acetabular anteversion by gender.
Fig. 3.
Scatter graph showing the number of male and female native arthritic acetabuli that were outside the Lewinnek4 safe zone.
Table I.
Orientation of native arthritic acetabulum (°) based on radiological reference frame (CI, confidence interval)
| Women | Men | p-value | |
|---|---|---|---|
| n | 36 | 29 | |
| Component size used | |||
| Mean | 51° | 54° | < 0.001 |
| 95% CI | 50 to 52 | 53 to 55 | - |
| sd | 2 | 2 | - |
| Range | 46° to 56° | 52° to 62° | - |
| Inclination | |||
| Mean | 52.2° | 50.4° | 0.333 |
| 95% CI | 50.0 to 54.4 | 47.4 to 53.5 | - |
| sd | 6.6° | 7.9° | - |
| Range | 35.4° to 63.4° | 38.1° to 67.2° | |
| Number of hips not within 30o to 50o range | 24 | 13 | 0.206 |
| Anteversion | |||
| Mean | 14.4° | 8.0° | 0.016 |
| 95% CI | 10.6 to 18.2 | 4.6 to 11.4 | - |
| sd | 11.4° | 8.7° | - |
| Range | -14.4° to 46.8° | -7.7° to 22.0° | |
| Number of hips not within 5o to 25o | 11 | 10 | 0.789 |
| Number outside Lewinnek’s4 safe zone (%) | 29 (78) | 20 (71) | 0.570 |
Discussion
This study of the natural acetabular orientation of 65 hips with primary osteoarthritis found the mean acetabular inclination to be 52.1° (sd 6.7) in women, 50.5° (sd 7.8) in men and mean acetabular anteversion to be significantly different (14.4°; sd 11.6 in women and 8.3°; sd 8.7 in men). Orientation fell outside of Lewinnek’s ‘safe zone’ in 75% of cases.
This study has a number of limitations. Imageless computer navigation can accurately measure acetabular inclination and anteversion. It has been validated to a precision of 1° and bias of 0.02° for inclination and a precision of 1.3° and bias of 0° for anteversion.16 During surgery the accuracy may not be as good because the anterior superior iliac spines and pubic symphysis have to be registered through skin. This can result in errors in the computer measurement of acetabular orientation.17 This can be a particular problem in those patients with a high level of fat over the pelvis. There were no reported problems with registration of anatomical landmarks in the cases in this study but as this study is retrospective these errors are unquantified. However, recent publications and our own data have shown that accuracy of acetabular component placement in navigated THA is not affected by BMI.18 In addition, Fukunishi et al19 found there was good correlation between intra-operative assessment and post-operative CT scan using the same navigation system used in this study. Another limitation is that the reliability of the assessment of the acetabular orientation cannot be calculated as it was only measured once for each patient.
The findings of this study only represent a Caucasian population with primary osteoarthritis. Care must be taken when extrapolating these results to populations in which other pathologies of the hip are present, in particular DDH. The same is true of populations comprising patients of different ethnicity.
Published literature from studies done using CT correlate with a number of our findings in relation to natural acetabular orientation. As we found in our study, Atkinson et al20demonstrated that mean acetabular inclination in arthritic hips falls outside of Lewinnek’s ‘safe zone’ whereas mean anteversion falls within. Merle et al21 also found this in their study. Atkinson et al20 also identified a statistically significant difference between men and women in terms of mean acetabular anteversion. They found the degree of difference to be 5.5°. We found a similar difference of 6.1°.
Murtha et al22used CT imaging to study 42 hips free of arthritic disease and found mean acetabular inclination to be 57.1° in women and 55.5° in men, and the mean acetabular anteversion to be 24.1° in women and 19.3° in men.22 They too identified a significant difference between men and women in terms of anteversion and that the orientation of the natural acetabulum did not match the ‘safe zone’ of acetabular component placement described by Lewinnek et al.4 The mean angles of inclination and anteversion found by Murtha et al22 differ from those identified in our study. Our study was done in arthritic hips and these differences may reflect the differences in acetabular orientation created by degenerative arthritic disease or indicate that the hips that develop arthritis tend to be less anteverted.
Comparison with reported acetabular orientations in the literature can be difficult. This is because many papers use mixed definitions of acetabular component inclination and anteversion.13 Failure to recognise differences between angles measured with respect to the anterior pelvic plane and coronal plane causes discrepancies, as does failure to standardise results as radiographic, anatomical or operative, as defined by Murray et al.15When comparing the orientation of hips to Lewinnek’s safe zone, the values must be represented as ‘radiographic’ values with respect to the anterior pelvic plane.4,13 This again is something that is not done consistently in current published literature.13 Merle et al21 have used anatomic values to represent this, which may explain their relatively higher mean inclination of 62.1° (sd 7.46) compared with other studies (Atkinson20) and our observation of inclination of 51.4° (sd 7.2).
Merle et al21converted the Lewinnek to their anatomical definition and found that 80% of hips were out of the safe zone. Our study found similar numbers (75%) to be outside of the safe zone.
We found that mean acetabular inclination was 50.5° in men and 52.1° in women, and that mean acetabular anteversion was 8.3° in men and 14.4° in women. However, the orientation differs with individuals. When natural acetabular orientation was compared with the ‘safe zone’ described by Lewinnek et al4, 75% fell outside of this range. When using natural acetabular orientation to guide component placement, it is important to be aware of the differences between men and women, and that the natural orientation may fall outside of what many consider to be a safe zone, especially with regard to inclination.
Funding Statement
The Golden Jubilee National Hospital receives funding for research from Stryker, B. Braun Aesculap Convatec and Mathys, none of which is related to this article.
Footnotes
Author contributions:S. T. Goudie: Literature search, Primary article writing, Data handling
A. H. Deakin: Statistical analysis, Paper editing, Data handling
K. Deep: Study design, Data collection, Editing, Oversaw progress of paper.
ICMJE Conflict of Interest:None declared
References
- 1.Kennedy JG, Rogers WB, Soffe KE. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty 1998;13:530–534. [DOI] [PubMed] [Google Scholar]
- 2.Williamson JA, Reckling FW. Limb length discrepancy and related problems following total hip joint replacement. Clin Orthop Relat Res 1978;134:135–138. [PubMed] [Google Scholar]
- 3.Schmalzried TP, Guttmann D, Grecula M, Amstutsz HC. The relationship between the design, position and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg [Am] 1994;76-A:677–688. [DOI] [PubMed] [Google Scholar]
- 4.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip replacement arthroplasties. J Bone Joint Surg [Am] 1978;60-A:217–220. [PubMed] [Google Scholar]
- 5.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop Relat Res 1990;261:159–170. [PubMed] [Google Scholar]
- 6.Kummer FJ, Shah S, Slyer S, DiCesare PE. The effect of acetabular cup orientation on limiting hip rotation. J Arthroplasty 1999;14;509-513. [DOI] [PubMed] [Google Scholar]
- 7.Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty: a multivariate analysis. J Arthroplasty 2002;17:282–288. [DOI] [PubMed] [Google Scholar]
- 8.Biedermann R, Tonin A, Krismer M, et al. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg [Br] 2005;87-B:762–769. [DOI] [PubMed] [Google Scholar]
- 9.Archbold HAP, Mockford B, Molloy D, et al. The transverse acetabular ligament: an aid to orientation of the acetabular component during primary total hip replacement. A preliminary study of 1000 cases investigating post-operative stability. J Bone Joint Surg [Br] 2006;88-B:883–886. [DOI] [PubMed] [Google Scholar]
- 10.Najarian B, Kilgore J, Markel D. Evaluation of component positioning in primary total hip arthroplasty using an imageless navigation device compared with traditional methods. J Arthroplasty 2009;24:15–21. [DOI] [PubMed] [Google Scholar]
- 11.Barrack RL. Dislocation after total hip arthoroplasty. Implant design and orientation. J Am Acad Orthop Surg 2003;11:89–99. [DOI] [PubMed] [Google Scholar]
- 12.Blendea S, Eckman K, Jaramaz B, Levison TJ, Digioia AM. Measurements of acetabular cup position and pelvic spatial orientation after total hip arthroplasty using computed tomography/radiography matching. Comput Aided Surg 2005;10:37–43. [DOI] [PubMed] [Google Scholar]
- 13.Wan Z, Malik A, Jaramaz B, Chao L, Dorr L. Imaging and navigation measurement of acetabular component position in THA. Clin Orthop Relat Res 2009;467:32–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr LD, Malik A, Wan Z, Long WT, Harris M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin Orthop Relat Res 2007;465:92–99. [DOI] [PubMed] [Google Scholar]
- 15.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg [Br] 1993;75-B:228–232. [DOI] [PubMed] [Google Scholar]
- 16.Malik A, Wan Z, Jaramaz B, Bowman G, Dorr LD. A validation model for measurement of acetabular component position. J Arthroplasty 2010;25:812–819. [DOI] [PubMed] [Google Scholar]
- 17.Wolf A, Digioia AM, Mor AB, Jaramaz B. Cup alignment error model for total hip arthroplasty. Clin Orthop Relat Res 2005;437:132–137. [DOI] [PubMed] [Google Scholar]
- 18.Fukui T, Fukunishi S, Nishio S, Shibanuma N, Yoshiya S. Use of Image-Free Navigation in Determination of Acetabular Cup Orientation: Analysis of Factors Affecting Precision. Orthopedics 2010;33:38–42. [DOI] [PubMed] [Google Scholar]
- 19.Fukunishi S, Fukui T, Imamura F, Nishio S. Assessment of accuracy of acetabular cup orientation in CT-free navigated total hip arthroplasty. Orthopaedics 2008;31:pii orthosupersite.com/view.asp?rID=31515. [PubMed] [Google Scholar]
- 20.Atkinson H, Johal KS, Willis-Owen C, Zadow S, Oakeshott RD. Differences in hip morphology between the sexes in patients undergoing hip resurfacing. J Orthop Surg Res 2010;5:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merle C, Grammatopoulos G, Waldstein W, et al. Comparison of native anatomy with recommended safe component orientation in total hip arthroplasty for primary osteoarthritis. J Bone Joint Surg [Am] 2013;95-A:e172(1-7). [DOI] [PubMed] [Google Scholar]
- 22.Murtha PE, Hafez MA, Jaramaz B, DiGioia AM. Variations in acetabular anatomy with reference to total hip replacement. J Bone Joint Surg [Br] 2008;90-B:308–313. [DOI] [PubMed] [Google Scholar]