Abstract
We describe the first case of Pseudoclavibacter species endocarditis in a 44-year-old patient. This genus, rarely isolated from humans, confirms here its role as a human pathogen.
CASE REPORT
A 44-year-old man was admitted to Angers University Hospital in November 2013 for a 20-min episode of regular heart flutters and left facial palsy. This patient, a worker in a poultry slaughterhouse, had a history of degenerative mitral valve insufficiency since 2008 and underwent mitral valve repair with an annuloplasty ring (Carpentier-Edwards Phisio II mitral annuloplasty ring; Edwards Lifesciences LLC, Irvine, CA) in 2011. In 2012, he suffered an ischemic cerebrovascular stroke attributed to atrial fibrillation. At the time of admission, the patient had a fever (body temperature, 38.0°C) and was hemodynamically stable. Nothing unusual was noticed in the biological test results, with a normal C-reactive protein level (<3 mg/liter; reference range, <5 mg/liter) and a normal white blood cell count (7 × 109/liter; reference range, 4 × 109 to 10 × 109/liter). Cerebral computed tomography showed no recent ischemic or hemorrhagic lesions. Endocarditis was suspected, and transesophageal echocardiography in the emergency department revealed a mitral stenosis and embolizing mitral vegetations, which could explain the transient ischemic attack (1). Five peripheral blood cultures collected in aerobic and anaerobic bottles (BacT/Alert; bioMérieux, Marcy l'Etoile, France) first on admission and then after transfer of the patient to the cardiology department remained sterile after 5 days of incubation. In view of the risk of embolism, 13 days after his admission, he underwent a mechanical bileaflet mitral valve replacement (ATS Medical, Plymouth, MI). Three valve specimens and the removed mitral annuloplasty ring were sent for microbiological analysis. Gram staining of the valve specimens showed short, Gram-positive rods. These samples were cultured on sheep blood agar (COLS+; Oxoid, Dardilly, France) in aerobic and anaerobic atmospheres, on chocolate agar (CHOCV; Oxoid), in an air atmosphere with 5% CO2, and on Schaedler and brain heart enrichment broths (bioMérieux). Forty-eight hours after inoculation, the culture was positive with little, smooth, gray colonies of nonmotile, catalase-positive, oxidase-negative, coryneform Gram-positive rods. The isolate grew on blood and chocolate agars, in an aerobic atmosphere, and in an air atmosphere with 5% CO2. No growth was observed under anaerobic conditions. Identification by matrix-assisted laser desorption-ionization time of flight mass spectrometry (Vitek MS; bioMérieux) with the Vitek MS IVD system (database V2.0) or the Vitek MS RUO system (Saramis database) retrieved no identification and no match with any of the species in these databases. The strain was also tested with the Vitek2 phenotypic system (bioMérieux) with the anaerobic bacteria-corynebacterium identification card (ANC card; bioMérieux), but this method failed to identify the strain. The antimicrobial in vitro susceptibility of this strain was tested by the agar diffusion method performed on blood agar with incubation at 37°C in air supplemented with 5% CO2 for 48 h. Results were interpreted according to the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines (http://www.eucast.org/clinical_breakpoints/). Since no EUCAST breakpoints have been defined for Pseudoclavibacter species, Corynebacterium species breakpoints were used. The strain was susceptible to imipenem, vancomycin, and aminoglycosides and was resistant to erythromycin and trimethoprim-sulfamethoxazole. Etests (bioMérieux) were also performed for penicillin (MIC, 0.015 mg/liter), amoxicillin (MIC, 0.03 mg/liter), and cefotaxime (MIC, 0.06 mg/liter). Identification of the strain was then performed by 16S rRNA gene sequencing with universal primers fD1 (5′-AGAGTTTGATCCTGGCTCAG-3′) and rP2 (5′-ACGGCTACCTTGTTACGACTT-3′) (2). The 1,429-bp sequencing product was compared with sequences deposited in the GenBank database by using the Basic Local Alignment Tool program through the National Center for Biotechnology Information (NCBI) server (http://blast.ncbi.nlm.nih.gov). The best match retrieved Pseudoclavibacter species strain Timone (GenBank accession no. FJ375951.1) with a similarity of 99.7% and an identity overlap of 1,421 of 1,425 bp. The second-best match obtained was Pseudoclavibacter bifida, with a similarity of 97.6% (overlap of 1,400 of 1,434 bp). 16S rRNA gene sequencing carried out directly with the valve samples produced the same result. The patient responded favorably to 2 weeks of intravenous antibiotic therapy with 12 g of amoxicillin given intravenously (i.v.) daily and 210 mg of gentamicin given i.v. daily and then 4 weeks of treatment with 12 g of amoxicillin given i.v. daily.
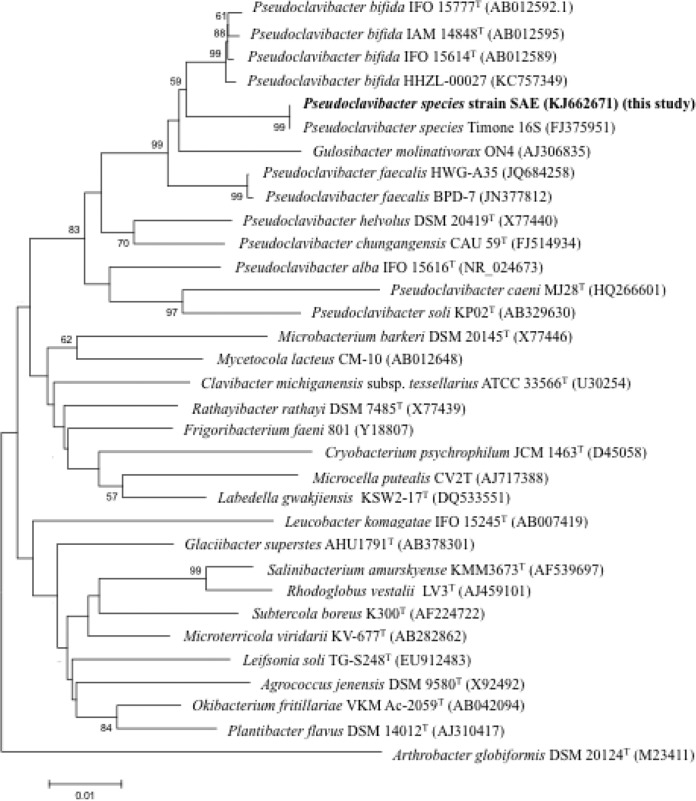
This is, to our knowledge, the first report describing a case of endocarditis due to a Pseudoclavibacter species. This genus belongs to the Microbacteriaceae family (Fig. 1), which is a member of the order Actinomycetales and the class Actinobacteria. The genus Pseudoclavibacter was recently described by Manaia et al. (3). Indeed, the latter reclassified the species Brevibacterium helvolum as the novel genus and species Pseudoclavibacter helvolus on the basis of low 16S rRNA gene sequence similarity to the previously described genus Brevibacterium and the distinctive phenotypic characteristics. Shortly after that, Lin et al. also proposed a new genus, Zimmermanella, and a different name for this same species, Zimmermanella helvola (4). But because of the earlier publication of Pseudoclavibacter by Manaia et al., Zimmermanella is now considered an illegitimate name for the genus.
FIG 1.
Neighbor-joining tree showing the relationship between the clinical Pseudoclavibacter species isolate and type strains within the Pseudoclavibacter genus and the Microbacteriaceae family. Sequences were aligned by using BioEdit software, and the construction of a neighbor-joining phylogenetic tree was performed with the MEGA 5 software. Bootstrap values are expressed as percentages of 500 replicates obtained with the Kimura two-parameter test, and percentages of bootstrap values higher than 50% are shown at the branching points. The branches of the tree are indicated by the genus and species names of the type strains followed by the NCBI gene accession numbers. The bar indicates 0.01 substitution per nucleotide position.
Pseudoclavibacter species seem to be prevalent in the environment. Species of this genus have been isolated from soil, activated-sludge, and fish fillet samples (5–7). Furthermore, Pseudoclavibacter species have been isolated from human specimens (4, 8) but infections due to this bacterium have rarely been described in the literature; a subcutaneous Pseudoclavibacter infection (9) and more recently a case of P. bifida bacteremia (10) have been reported. In these cases, as in our case, 16S rRNA gene sequencing was an essential diagnostic tool. Pseudoclavibacter bacteria have been reported as Gram-positive, strictly aerobic, catalase-positive, oxidase-negative, alkaline phosphatase-positive, inconstantly rhamnose-fermenting, and β-glucosidase-positive rods (4, 10). However, accurate identification of this species by the phenotypic method is challenging. Indeed, Pseudoclavibacter species are not included in the Vitek2 database, in the API Coryne test, or in the Vitek MS IVD or Saramis database. This is why molecular methods such as 16S rRNA gene sequencing are needed for the final identification of these organisms. This case report confirms the difficulty of Pseudoclavibacter species identification, and because of this difficulty, we can suppose that many Pseudoclavibacter infections may go undetected. This could explain, in part, the paucity of reported Pseudoclavibacter infections.
Pseudoclavibacter species is considered the cause of the endocarditis reported here. Indeed, this bacterium was identified in all of the valve samples both by culture and by 16S rRNA gene sequencing directly on the samples. This study emphasizes the real pathogenic potential of this species. Interestingly, Pseudoclavibacter species did not expose the previously repaired valve to extended tissue destruction such as that frequently encountered with other bacteria (11). Indeed, the mitral valve remained competent but was covered with mobile and obstructive vegetations.
In conclusion, this case describes the first case of Pseudoclavibacter species endocarditis. This enhances the potential involvement of Pseudoclavibacter species in such infections.
Nucleotide sequence accession number.
The 16S nucleotide sequence of the isolate described here (strain SAE) has been deposited in the GenBank database under accession number KJ662671.
Footnotes
Published ahead of print 2 July 2014
REFERENCES
- 1.Gould FK, Denning DW, Elliott TS, Foweraker J, Perry JD, Prendergast BD, Sandoe JA, Spry MJ, Watkin RW, Working Party of the British Society for Antimicrobial Chemotherapy 2012. Guidelines for the diagnosis and antibiotic treatment of endocarditis in adults: a report of the Working Party of the British Society for Antimicrobial Chemotherapy. J. Antimicrob. Chemother. 67:269–289. 10.1093/jac/dkr450. [DOI] [PubMed] [Google Scholar]
- 2.Weisburg WG, Barns SM, Pelletier DA, Lane DJ. 1991. 16S ribosomal DNA amplification for phylogenetic study. J. Bacteriol. 173:697–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manaia CM, Nogales B, Weiss N, Nunes OC. 2004. Gulosibacter molinativorax gen. nov., sp. nov., a molinate-degrading bacterium, and classification of “Brevibacterium helvolum” DSM 20419 as Pseudoclavibacter helvolus gen. nov., sp. nov. Int. J. Syst. Evol. Microbiol. 54:783–789. 10.1099/ijs.0.02851-0. [DOI] [PubMed] [Google Scholar]
- 4.Lin Y-C, Uemori K, de Briel DA, Arunpairojana V, Yokota A. 2004. Zimmermannella helvola gen. nov., sp. nov., Zimmermannella alba sp. nov., Zimmermannella bifida sp. nov., Zimmermannella faecalis sp. nov. and Leucobacter albus sp. nov., novel members of the family Microbacteriaceae. Int. J. Syst. Evol. Microbiol. 54:1669–1676. 10.1099/ijs.0.02741-0. [DOI] [PubMed] [Google Scholar]
- 5.Kim MK, Jung H-Y. 2009. Pseudoclavibacter soli sp. nov., a {beta}-glucosidase-producing bacterium. Int. J. Syst. Evol. Microbiol. 59:835–838. 10.1099/ijs.0.65627-0. [DOI] [PubMed] [Google Scholar]
- 6.Cho S-L, Jung MY, Park M-H, Chang Y-H, Yoon J-H, Myung SC, Kim W. 2010. Pseudoclavibacter chungangensis sp. nov., isolated from activated sludge. Int. J. Syst. Evol. Microbiol. 60:1672–1677. 10.1099/ijs.0.015552-0. [DOI] [PubMed] [Google Scholar]
- 7.Alfaro B, Hernandez I. 2013. Evolution of the indigenous microbiota in modified atmosphere packaged Atlantic horse mackerel (Trachurus trachurus) identified by conventional and molecular methods. Int. J. Food Microbiol. 167:117–123. 10.1016/j.ijfoodmicro.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Mages IS, Frodl R, Bernard KA, Funke G. 2008. Identities of Arthrobacter spp. and Arthrobacter-like bacteria encountered in human clinical specimens. J. Clin. Microbiol. 46:2980–2986. 10.1128/JCM.00658-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lemaitre F, Stein A, Raoult D, Drancourt M. 2011. Pseudoclavibacter-like subcutaneous infection: a case report. J. Med. Case Rep. 5:468. 10.1186/1752-1947-5-468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oyaert M, De Baere T, Breyne J, De Laere E, Mariën S, Waets P, Laffut W. 2013. First case of Pseudoclavibacter bifida bacteremia in an immunocompromised host with chronic obstructive pulmonary disease (COPD). J. Clin. Microbiol. 51:1973–1976. 10.1128/JCM.00138-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Habib G, Hoen B, Tornos P, Thuny F, Prendergast B, Vilacosta I, Moreillon P, de Jesus Antunes M, Thilen U, Lekakis J, Lengyel M, Müller L, Naber CK, Nihoyannopoulos P, Moritz A, Zamorano JL, ESC Committee for Practice Guidelines 2009. Guidelines on the prevention, diagnosis, and treatment of infective endocarditis (new version 2009): the Task Force on the Prevention, Diagnosis, and Treatment of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) and the International Society of Chemotherapy (ISC) for Infection and Cancer. Eur. Heart J. 30:2369–2413. 10.1093/eurheartj/ehp285. [DOI] [PubMed] [Google Scholar]