Abstract
Purpose
To present descriptive epidemiology of cataract surgery among Medicare recipients in the United States.
Setting
Cataract surgery performed on Medicare beneficiaries in 2003 and 2004.
Methods
Medicare claims data were used to identify all cataract surgery claims for procedures performed in the United States in 2003-2004. Standard assumptions were used to limit the claims to actual cataract surgery procedures performed. Summary statistics were created to determine the number of procedures performed for each outcome of interest: cataract surgery rates by age, race, and gender; surgical volume by facility type, surgeon characteristics, and state; time interval between first- and second-eye cataract surgery.
Results
The national cataract surgery rate for 2003-2004 was 61.8 per 1000 Medicare beneficiary person-years. The rate was significantly higher for females and for those 75-84. After adjustment for age and gender, blacks had approximately a 30% lower rate of surgery than whites. While only 5% of cataract surgeons performed more than 500 cataract surgeries annually, these surgeons performed 26% of the total cataract surgeries. Increasing surgical volume was found to be highly correlated with use of ambulatory surgical centers and reduced time interval between first- and second-eye surgery in the same patient.
Conclusions
The epidemiology of cataract surgery in the United States Medicare population documents substantial variation in surgical rates by race, gender, age, and by certain provider characteristics.
Background
Cataract extraction is the most commonly performed surgical procedure in the United States Medicare population, and both the annual total volume and age-adjusted rates of cataract surgery have increased substantially since the 1980's. Estimates suggest that at least eighty percent of cataract surgery in the US is performed on Medicare beneficiaries.1 In 1980, the rate of cataract surgery was estimated at 13.4 per 1000 Medicare beneficiaries; in 1987, it was estimated at 25.42 and in 1995 the rate had increased to 58.7 per 1000 beneficiaries.3 The field of cataract surgery has enjoyed substantial technological improvements, such as reduced surgical time, smaller wounds, and quicker recovery with better quality of vision. Such improvements, which confer an increase in quality of life, together with increasing demand for health care in general, likely have lowered both patients' and surgeons' thresholds for surgery. Since the work in the 1990s by the Cataract Patient Outcomes Research Team (PORT), published information on the epidemiology of cataract surgery in the Medicare population has been limited.2;4-6 The goal of this manuscript is to provide precise estimates of the cataract surgery volume among Medicare beneficieries nationwide and at the state level and to describe the characteristics of patients and providers participating in cataract surgery.
Methods
The Centers for Medicare and Medicaid Services (CMS) Privacy Board and the Johns Hopkins Medicine Institutional Review Board approved the research protocol for this study.
Medicare beneficiary healthcare claims files containing person-specific data on Medicare beneficiaries and providers from the calendar years 2003 and 2004 were obtained from the CMS Research Data Distribution Center. These files included extracts from the standard analytic carrier files (formerly Physician/Supplier Part B file) representing all claims for cataract surgery and associated denominator files during this time period. In addition, we obtained the 2004 Medicare Physician Identification and Eligibility Registry (MPIER) file, which includes provider-specific information such as medical school graduation year, state of medical licensure, and specialty.
The carrier files contain information on dates and place of service, diagnosis and procedure codes, the unique physician identification number (UPIN) for the provider submitting the claim, billing codes and associated charges and payments. In addition to individual provider claims, the carrier file also contains facility claims from ambulatory surgery centers (ASCs). The claims utilized in this analysis included all records (100% sample) with a procedure code of cataract extraction identified using the Current Procedural Terminology (CPT) codes (Table 1). Due to some inaccuracies in the coding of cataract surgeries for the state of Alaska, and the large proportion of surgeries performed on non-residents of DC within the District of Columbia (DC), surgeries were limited to those performed on residents of the 48 contiguous United States.
Table 1. Cataract Extraction Procedure Codes Used in Analyses.
| CPTa code | Description |
|---|---|
|
| |
| 66850 | Removal of lens material; phacofragmentation technique (mechanical or ultrasonic) (e.g., phacoemulsification), with aspiration |
| 66920 | Removal of lens material; intracapsular |
| 66930 | Removal of lens material; intracapsular, for dislocated lens |
| 66940 | Removal of lens material; extracapsular (other than 66840, 66850, 66852) |
| 66982 | Extracapsular cataract removal with insertion of IOLb prosthesis (1-stage procedure), manual or mechanical technique (e.g., irrigation and aspiration or phacoemulsification) complex, requiring devices or techniques not generally used in routine cataract surgery |
| 66983 | Intracapsular extraction with insertion of IOL prosthesis (1-stage procedure) |
| 66984 | Extracapsular cataract removal with insertion of IOL prosthesis (1-stage procedure), manual or mechanical technique (e.g., irrigation and aspiration or phacoemulsification) |
CPT=Current Procedural Terminology
IOL=intraocular lens
Additional information, such as procedure modifier codes, was used to exclude records that indicated only pre-operative or post-operative care. If the provider was an optometrist, the record was excluded, since optometrists are not licensed to perform cataract surgery in the United States and the claim was likely for co-management. Records also were excluded if they indicated that the surgical procedure was not carried out or was discontinued, if the claim was for a return to the operating room for a related procedure during the post-operative period, if the service was not covered by Medicare, or the record was coded as an invalid or duplicate billing claim.
Cataract surgery records from the carrier file were merged with the MPIER file by physician UPIN and state where the cataract surgery was performed. Records were limited to at most two cataract surgeries per patient over the two-year period. Ophthalmologist professional fee claims were preferentially kept when both physician and facility claims were billed for a particular cataract surgery date. For some surgeries, only an ASC facility claim was available.
The denominator file provides eligibility, demographic and residence information for all enrolled Medicare beneficiaries. The denominator file was limited to beneficiaries residing in the 48 contiguous states who were aged 65 or older with continuous Part B eligibility and no health maintenance organization (HMO) enrollment in the two-year period. Because cataract surgery is performed in the outpatient setting, continuous Part A Medicare eligibility was not a requirement, although in July 2004, 99 percent of Medicare beneficiaries with Part B coverage also had Part A benefits.7
Cataract surgery records were merged with the limited denominator file to permit the calculation of national and state-level cataract surgery rates during the two-year period. Rates of cataract surgery vary by age, gender and race and states are not uniform with respect to the demographic characteristics of their residents with Medicare insurance. Therefore, direct adjustment of state rates of cataract surgery by age, gender and race was carried out using eligible beneficiaries in the limited denominator file as the reference population. Cataract surgery was attributed to the state in which it was performed, regardless of the patient's state of residence. A sensitivity analysis was performed to estimate the difference in a state's rate of cataract surgery if out-of-state surgeries were excluded.
Years of surgical experience were estimated by subtracting the year of medical school graduation from 2004. Although first year residents do not perform cataract surgery under their own unique provider numbers, this method of estimation was used to provide a consistent methodology across providers based on the limited available data. Cross-tabulations and Chi-square tests were used to examine associations between surgeon characteristics, surgery location and patient characteristics. A logistic regression model was developed to examine predictors of having a second cataract surgery within 14 days of the first surgery.
Results
Prior to limiting the dataset to the 48 contiguous United States, the combined 2003 and 2004 denominator files included 35,239,002 total aged beneficiaries. Limiting the data set to Medicare beneficiaries covered under the standard fee-for-service (FFS) arrangement and no HMO enrollment during the 2003-2004 time period reduced the sample size by 15 percent. The FFS beneficiaries did not differ on age, gender or race from those enrolled in an HMO during the two-year period.
We estimate that 1,704,197 cataract surgeries were performed in 2003 and 1,742,221 in 2004 on Medicare FFS beneficiaries who resided in the 48 contiguous states. Table 2 provides the unadjusted cataract surgery rate in this population overall, and by age, gender and race. The overall cataract surgery rate in this population was 61.8 per 1000 person-years. The rate was significantly higher for females (p<0.0001), and for beneficiaries aged 75-84 (p<0.0001), compared to beneficiaries aged 65-74 years. The cataract surgery rate among blacks was significantly lower than the rate among other races (p<0.0001, Table 2).
Table 2. Unadjusted Cataract Surgery Rate for Eligible Medicare Beneficiariesa in 2003 and 2004.
| Total Person-Years (2003 + 2004) | Cataract Surgeries (2003 + 2004) | Rate per 1000 Person-Years | p-valueb | |
|---|---|---|---|---|
| Overall | 55,800,184 | 3,446,418 | 61.8 | |
|
| ||||
| Gender | ||||
|
| ||||
| Female | 32,868,760 | 2,177,982 | 66.3 | <0.0001 |
| Male | 22,931,424 | 1,268,436 | 55.3 | |
|
| ||||
| Agec | ||||
|
| ||||
| 65-74 | 29,461,704 | 1,527,817 | 51.9 | |
| 75-84 | 19,591,725 | 1,599,909 | 81.7 | < 0.0001 |
| 85+ | 6,746,751 | 318,692 | 47.2 | |
|
| ||||
| Raced | ||||
|
| ||||
| White | 48,954,425 | 3,106,127 | 63.4 | |
| Black | 4,334,398 | 198,194 | 45.7 | <0.0001 |
| Hispanic | 917,491 | 55,903 | 60.9 | |
| Asian | 804,863 | 46,782 | 58.1 | |
| Other | 709,447 | 35,704 | 50.3 | |
Eligible, aged Medicare beneficiaries include all beneficiaries at least 65 years old with continuous Medicare Part B coverage and no Health Maintenance Organization (HMO) enrollment during the calendar years 2003 and 2004 from point of eligibility until death or end of study period who resided in one of the 48 contiguous states.
Significance level from Student's t-test (gender comparison) or Analysis of Variance (age and race comparisons).
For 9 beneficiaries, age was unknown.
For 84,133 beneficiaries (79,560 person-years and 3,708 cataract surgeries), race was unknown.
Table 3 reports the cataract surgery rates stratified by age, gender and race. After age and gender adjustment, the cataract surgery rate among blacks was nearly 30% percent lower than the corresponding rate among whites for beneficiaries age 65-74 and 75-84 years. The rate among black males was the lowest of any gender/race group. Within the two younger age categories, for each race, women had higher surgery rates than men.
Table 3. Cataract Surgery Rate per 1000 Person-years by Age, Gender and Race and Relative Riska by Age and Race.
| Cataract Surgery Rate | |||||
|---|---|---|---|---|---|
|
|
|||||
| Age Group | |||||
| Race | Cataract Surgeries | Sex | 65-74 | 75-84 | 85+ |
| White | 1,156,079 | Male | 44.1 | 78.5 | 58.4 |
| 1,950,048 | Female | 60.6 | 87.5 | 44.2 | |
| Black | 59,741 | Male | 29.3 | 52.4 | 42.0 |
| 138,453 | Female | 46.1 | 64.7 | 38.0 | |
| Hispanic | 20,716 | Male | 48.1 | 65.9 | 44.6 |
| 35,187 | Female | 63.2 | 73.9 | 36.2 | |
| Asian | 17,279 | Male | 46.8 | 63.3 | 45.4 |
| 29,503 | Female | 60.9 | 69.1 | 35.9 | |
| Other Raceb | 13,502 | Male | 37.7 | 64.8 | 40.5 |
| 22,202 | Female | 51.8 | 73.5 | 35.8 | |
|
| |||||
| Relative Riska (95% CIc) | |||||
|
|
|||||
| Race | All Ages | 65-74 | 75-84 | 85+ | |
| White | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | |
| Black | 0.72 (0.72, 0.72) | 0.74 (0.73, 0.74) | 0.72 (0.72, 0.72) | 0.81 (0.79, 0.82) | |
| Hispanic | 0.96 (0.95, 0.97) | 1.06 (1.05, 1.08) | 0.84 (0.83, 0.85) | 0.80 (0.78, 0.83) | |
| Asian | 0.92 (0.91, 0.92) | 1.04 (1.02, 1.05) | 0.80 (0.78, 0.81) | 0.82 (0.79, 0.84) | |
| Other Raceb | 0.79 (0.79, 0.80) | 0.85 (0.84, 0.86) | 0.84 (0.82, 0.85) | 0.77 (0.74, 0.80) | |
Separate relative risks (RR) were calculated for each age category and for all ages combined. Each RR combined males and females and used white race as the reference group.
Other Race includes North American Natives and “other” from the Medicare classification.
CI = Confidence Interval
Table 4 shows selected provider-related characteristics for the 3,446,418 surgeries from 2003-2004 combined. These surgeries were performed by 11,938 different surgeons, and approximately half were performed in hospital settings and half in ASCs. Surgeons performing more than 500 cataract surgeries annually represented 5 percent of all cataract surgeons during that time period, but accounted for 26 percent of cataract surgeries performed nationally among Medicare beneficiaries. Ninety-seven surgeons performed more than 1000 surgeries annually, with a mean of 1477 surgeries (range: 1010 to 6,485). This group of surgeons, which represented 0.8 percent of surgeons performing cataract surgery in 2003 and 2004, performed approximately 8 percent of all cataract surgeries billed to Medicare. Surgeons with more than 10 years of experience were more likely to perform more than 500 surgeries per year compared to surgeons with 10 or fewer years of experience (p< 0.0001).
Table 4. Characteristics of 3,446,418 Cataract Surgeries in United States billed through Medicare in 2003-2004.
| # of Surgeons | % of Surgeons | # of Surgeries | % of Surgeries | |
|---|---|---|---|---|
| Overall | 11,938 | 100 | 3,446,418 | 100 |
|
| ||||
| Surgical Setting | ||||
|
| ||||
| ASCa | 5,684b | N/a | 1,734,098 | 50.3 |
| Hospital | 9,309b | N/a | 1,634,166 | 47.4 |
| Unknownc | 78,154 | 2.3 | ||
|
| ||||
| Surgeon Annual Cataract Surgery Volume | ||||
|
| ||||
| 1-50 | 4,608 | 38.6 | 144,561 | 4.2 |
| 51-200 | 4,529 | 37.9 | 1,021,987 | 29.7 |
| 201-500 | 2,253 | 18.9 | 1,361,252 | 39.5 |
| 501-1000 | 451 | 3.8 | 594,997 | 17.3 |
| 1001+d | 97 | 0.8 | 286,461 | 8.3 |
| Unknowne | 37,160 | 1.1 | ||
|
| ||||
| Surgeon Years of Experience as of 2004 | ||||
|
| ||||
| 0-10 years | 1,857 | 15.6 | 287,638 | 8.4 |
| 11-20 years | 3,529 | 29.6 | 1,113,713 | 32.3 |
| 21-30 years | 3,544 | 29.7 | 1,228,284 | 35.6 |
| 31+ years | 2,902 | 24.3 | 774,771 | 22.5 |
| Unknowne | 106 | 0.9 | 42,012 | 1.2 |
ASC=Ambulatory Surgery Center
Some surgeons operate in both ASCs and hospitals, and they appear in both totals.
Some service locations were inaccurate.
The 97 very high volume surgeons had a mean annual surgical volume of 1477 (median=1255; range 1010-6485).
These surgeries only had an ASC facility claim and could not be linked to the surgeon or surgeon upins were not valid or were for new physicians without an assigned upin (e.g, ‘EXE000,’ ‘NEW000’).
Surgical volume and site of surgery are tightly correlated (Table 5), with a dose-response relationship between increasing surgical volume and greater likelihood of the surgery being performed in an ASC (p<0.0001; Mantel- Haenszel test for trend). Surgeons' volume was not associated with Medicare beneficiaries' age or gender (data not shown).
Table 5. Association between Surgical Setting and Surgeon Annual Cataract Surgery Volumea.
| Surgeon Annual Cataract Surgery Volume N (%) | |||||
|---|---|---|---|---|---|
| Surgical Setting | 1-50 | 51-200 | 201-500 | 501-1000 | 1001+ |
| ASCb | 39,890 (29.2) | 376,086 (37.8) | 679,835 (51.0) | 386,220 (66.1) | 222,688 (78.8) |
| Hospital | 96,867 (70.8) | 617,556 (62.2) | 654,537 (49.0) | 197,726 (33.9) | 60,058 (21.2) |
Among surgeries where both the surgeon and surgical setting were known (excludes 3.3% of records); p<0.0001 by Mantel-Haenszel test for trend.
ASC=Ambulatory Surgery Center
Overall, approximately 45 percent of Medicare beneficiaries underwent surgery in the second eye during the period of observation, and at least 96% of second-eye surgeries were performed by the surgeon who performed the first eye surgery. Table 6 provides data on the time interval between surgeries and the operating surgeon's annual surgical volume. More than 25% of second-eye surgeries occurred within 14 days of first-eye surgery, and about 53% occurred within 30 days. Eighty-five percent occurred within 90 days of the first-eye surgery. Among patients with the same surgeon for both eyes, a strong, positive relationship was seen between interval between surgeries in the same patient and annual surgical volume. Higher volume surgeons tended to operate within a shorter time interval than lower volume surgeons. Whereas the second surgery was performed within two weeks in 11% of the lowest volume surgeons, those with surgical volumes of 501 to 1,000 or 1,001 or more performed second-eye surgery within two weeks 34 and 47 percent of the time, respectively (p<0.0001; Mantel-Haenszel test for trend).
Table 6. Time between Bilateral Surgeries* by Annual Surgical Volume.
| Annual Surgical Volume # People(%) |
||||||
|---|---|---|---|---|---|---|
| Days between Surgeries | Overall Distribution | 1-50 | 51-200 | 201-500 | 501-1000 | 1001+ |
| 1-14 | 281,943 (27.3) | 2,942 (11.4) | 45,309 (17.2) | 111,890 (26.3) | 71,853 (34.2) | 49,949 (46.8) |
| 15-30 | 268,525 (26.0) | 4,388 (17.0) | 56,560 (21.5) | 115,619 (27.2) | 62,248 (29.6) | 29,710 (27.8) |
| 31-90 | 330,591 (32.0) | 10,190 (39.5) | 101,279 (38.4) | 140,184 (32.9) | 57,849 (27.5) | 21,089 (19.8) |
| 91+ | 150,902 (14.6) | 8,256 (32.0) | 60,438 (22.9) | 58,093 (13.6) | 18,092 (8.6) | 6,023 (5.6) |
Among surgeries where same surgeon performed both surgeries
Multivariable logistic regression analysis was undertaken to predict likelihood of second-eye surgery within 14 days among patients operated by the same surgeon for both surgeries suggests younger Medicare beneficiaries and whites were more likely to undergo second-eye cataract surgery within 14 days (Table 7). Increased annual surgeon volume and use of an ASC also were independently predictive of a greater likelihood of second-eye surgery within 14 days.
Table 7. Association between Patient or Surgeon Characteristics and Second Surgery within 14 days of First Surgery (N=1,031,961patientsa).
| Relative Risk (95% CIb) of 2nd surgery <= 14 days after 1st surgery | ||
|---|---|---|
|
| ||
| Unadjusted | Adjusted | |
| Patient Characteristics | ||
|
| ||
| Female | Reference | Reference |
| Male | 1.13 (1.12, 1.14) | 1.11 (1.10, 1.12) |
| Age (years) | ||
| 65-74 | Reference | Reference |
| 75-84 | 0.80 (0.80, 0.81) | 0.82 (0.81, 0.83) |
| 85+ | 0.70 (0.69, 0.71) | 0.72 (0.71, 0.74) |
| Race | ||
| White | Reference | Reference |
| Black | 0.72 (0.70, 0.73) | 0.73 (0.71, 0.75) |
| Hispanic | 0.76 (0.73, 0.79) | 0.87 (0.83, 0.90) |
| Asian | 0.56 (0.53, 0.59) | 0.69 (0.65, 0.72) |
| Other Racec | 0.76 (0.73, 0.80) | 0.78 (0.74, 0.82) |
|
| ||
| Surgeon Characteristics | ||
|
| ||
| Annual Surgical Volume | ||
| 1-50 | Reference | Reference |
| 51-200 | 1.61 (1.55, 1.68) | 1.56 (1.50, 1.63) |
| 201-500 | 2.77 (2.66, 2.88) | 2.57 (2.47, 2.67) |
| 501-1000 | 4.04 (3.88, 4.20) | 3.63 (3.48, 3.78) |
| 1001+ | 6.82 (6.55, 7.10) | 6.04 (5.81, 6.30) |
| Years of Experience (since med school graduation through 2004) | ||
| 1-10 yrs | Reference | Reference |
| 11-20 yrs | 1.13 (1.11, 1.15) | 0.95 (0.93, 0.96) |
| 21-30 yrs | 1.08 (1.06, 1.10) | 0.84 (0.83, 0.86) |
| 31+ yrs | 1.08 (1.06, 1.10) | 0.83 (0.81, 0.84) |
| Place of Service | ||
| Hospital | Reference | Reference |
| ASCd | 1.66 (1.64, 1.67) | 1.35 (1.33, 1.36) |
Missing data: n=975 with unknown race; n=1086 with unknown surgeon years of experience; n=22548 with inaccurate service location
CI=Confidence Interval
Other Race includes North American Natives and “other” from the Medicare classification.
ASC=Ambulatory Surgery Center
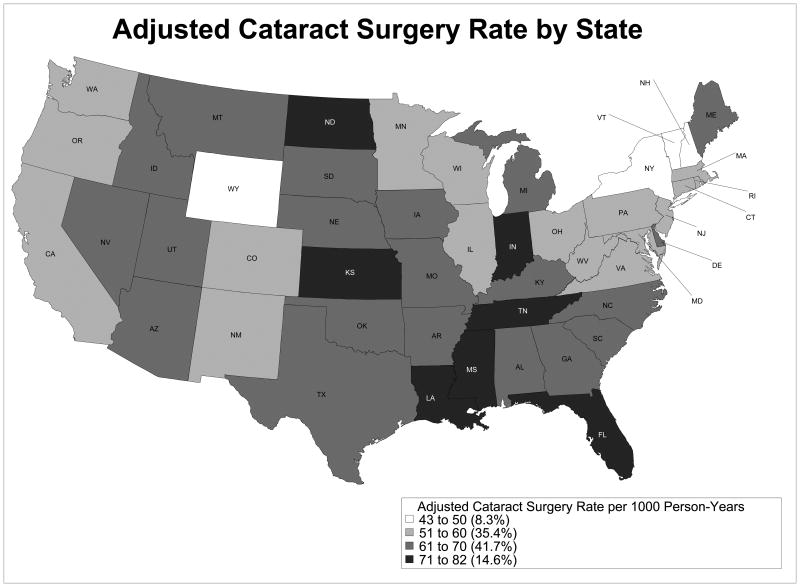
Although the national cataract surgery rate was 61.8 per 1000 Medicare beneficiaries per year, some variation in rate by state was observed. Rates ranged from 42 surgeries per 1000 person-years (Wyoming) to 86 surgeries per 1000 person-years (North Dakota), a greater than two-fold difference. State-to-state variability persisted after adjusting for age, gender and race (Figure 1 and Table 8). When out-of-state cataract surgeries were excluded from the calculation of state rates, adjusted cataract surgery rates were lower, on average, by 4.5 surgeries per 1000 person-years (range of 1 to 17 per 1000 person-years) (data not shown). The largest decreases were seen for North Dakota (decrease of 17 surgeries per 1000 person-years) and South Dakota (decrease of 10 surgeries per 1000 person-years.
Figure 1.
Table 8. Cataract Surgery Rates in 2003-2004 by State.
| State | Person-Years | # Cataract Surgeries | Unadjusted Cataract Surgery rate / 1000 person-years | Unadjusted 95% CI* | Adjusted Cataract Surgery rate / 1000 person-years¶ | Adjusted 95% CI*¶ |
|---|---|---|---|---|---|---|
| AL | 1026441 | 69935 | 68.1 | 67.6 – 68.6 | 69.9 | 69.3 – 70.5 |
| AZ | 859550 | 57146 | 66.5 | 65.9 – 67.0 | 67.5 | 66.9 – 68.1 |
| AR | 710636 | 48649 | 68.5 | 67.9 – 69.1 | 69.2 | 68.5 – 69.8 |
| CA | 4204006 | 235122 | 55.9 | 55.7 – 56.2 | 56.1 | 55.9 – 56.3 |
| CO | 565137 | 32799 | 58.0 | 57.4 – 58.7 | 58.4 | 57.8 – 59.0 |
| CT | 810885 | 46881 | 57.8 | 57.3 – 58.3 | 55.8 | 55.3 – 56.3 |
| DE | 200437 | 12931 | 64.5 | 63.4 – 65.6 | 65.3 | 64.2 – 66.4 |
| FL | 4013540 | 299191 | 74.5 | 74.3 – 74.8 | 73.7 | 73.5 – 74.0 |
| GA | 1497782 | 96612 | 64.5 | 64.1 – 64.9 | 67.0 | 66.5 – 67.4 |
| ID | 269442 | 18660 | 69.3 | 68.3 – 70.2 | 69.0 | 67.3 – 70.7 |
| IL | 2601621 | 143507 | 55.2 | 54.9 – 55.4 | 55.0 | 54.7 – 55.2 |
| IN | 1426873 | 106619 | 74.7 | 74.3 – 75.2 | 73.8 | 73.3 – 74.2 |
| IA | 794617 | 53184 | 66.9 | 66.4 – 67.5 | 65.7 | 64.9 – 66.4 |
| KS | 648862 | 46515 | 71.7 | 71.0 – 72.3 | 70.8 | 70.1 – 71.5 |
| KY | 948297 | 57932 | 61.1 | 60.6 – 61.6 | 61.1 | 60.4 – 61.7 |
| LA | 847322 | 57812 | 68.2 | 67.7 – 68.8 | 70.6 | 70.0 – 71.2 |
| ME | 360974 | 22562 | 62.5 | 61.7 – 63.3 | 63.8 | 62.4 – 65.2 |
| MD | 1062246 | 57796 | 54.4 | 54.0 – 54.9 | 55.2 | 54.7 – 55.6 |
| MA | 1197637 | 69256 | 57.8 | 57.4 – 58.3 | 55.5 | 55.1 – 55.9 |
| MI | 2345517 | 149519 | 63.7 | 63.4 – 64.1 | 63.7 | 63.4 – 64.0 |
| MN | 962787 | 56502 | 58.7 | 58.2 – 59.2 | 58.1 | 57.5 – 58.7 |
| MS | 658091 | 45075 | 68.5 | 67.9 – 69.1 | 71.5 | 70.7 – 72.3 |
| MO | 1230521 | 80037 | 65.0 | 64.6 – 65.5 | 64.5 | 64.0 – 64.9 |
| MT | 241487 | 15233 | 63.1 | 62.1 – 64.1 | 62.7 | 60.9 – 64.5 |
| NE | 421940 | 28490 | 67.5 | 66.7 – 68.3 | 66.7 | 65.8 – 67.6 |
| NV | 305210 | 19848 | 65.0 | 64.1 – 65.9 | 67.6 | 66.7 – 68.5 |
| NH | 292813 | 14026 | 47.9 | 47.1 – 48.7 | 45.5 | 44.6 – 46.4 |
| NJ | 1847928 | 100461 | 54.4 | 54.0 – 54.7 | 53.0 | 52.7 – 53.3 |
| NM | 330382 | 17571 | 53.2 | 52.4 – 54.0 | 54.3 | 53.4 – 55.3 |
| NY | 3491889 | 176060 | 50.4 | 50.2 – 50.7 | 49.8 | 49.6 – 50.1 |
| NC | 1857422 | 119253 | 64.2 | 63.8 – 64.6 | 65.6 | 65.2 – 66.0 |
| ND | 178889 | 15328 | 85.7 | 84.3 – 87.0 | 81.8 | 79.8 – 83.9 |
| OH | 2455740 | 148260 | 60.4 | 60.1 – 60.7 | 60.1 | 59.8 – 60.4 |
| OK | 786561 | 55037 | 70.0 | 69.4 – 70.6 | 70.0 | 69.4 – 70.6 |
| OR | 536822 | 31943 | 59.5 | 58.9 – 60.2 | 59.3 | 58.5 – 60.1 |
| PA | 2542720 | 154615 | 60.8 | 60.5 – 61.1 | 58.3 | 58.0 – 58.6 |
| RI | 162287 | 9225 | 56.8 | 55.7 – 58.0 | 53.6 | 52.5 – 54.8 |
| SC | 966771 | 59252 | 61.3 | 60.8 – 61.8 | 63.5 | 62.9 – 64.1 |
| SD | 210953 | 14967 | 70.9 | 69.8 – 72.1 | 67.7 | 65.8 – 69.7 |
| TN | 1263532 | 90913 | 72.0 | 71.5 – 72.4 | 72.3 | 71.8 – 72.8 |
| TX | 3710002 | 228221 | 61.5 | 61.3 – 61.8 | 62.6 | 62.3 – 62.8 |
| UT | 360868 | 25518 | 70.7 | 69.8 – 71.6 | 69.8 | 68.5 – 71.0 |
| VT | 151490 | 6715 | 44.3 | 43.3 – 45.4 | 42.9 | 41.2 – 44.6 |
| VA | 1507110 | 84854 | 56.3 | 55.9 – 56.7 | 57.2 | 56.8 – 57.6 |
| WA | 1043086 | 59859 | 57.4 | 56.9 – 57.8 | 57.2 | 56.7 – 57.7 |
| WV | 489575 | 26247 | 53.6 | 53.0 – 54.3 | 54.2 | 53.4 – 55.1 |
| WI | 1287768 | 75522 | 58.6 | 58.2 – 59.1 | 57.5 | 57.1 – 58.0 |
| WY | 113718 | 4758 | 41.8 | 40.7 – 43.0 | 43.2 | 41.5 – 44.9 |
CI: Confidence Interval
Adjusted for age, sex, and race
Discussion
We note several interesting features regarding the descriptive epidemiology of Medicare recipients undergoing cataract surgery. First, the overall cataract surgery rate was 61.8 surgeries per 1000 person-years. Although the rate of cataract surgery among Medicare beneficiaries increased dramatically between 1980 and 1995 (from 13.4 to 58.7 surgeries per 1000 person-years,2;3 there was almost no increase in that rate in the following decade. The dramatic increase between 1980 and 1995 likely reflects the lowering of threshold for surgery by both surgeons and patients that accompanied first the introduction of standard extracapsular surgery with posterior chamber intraocular lenses and then phacoemulsification with smaller incisions and foldable intraocular lenses. Females in the United States undergo cataract surgery at a rate about 20 percent higher than males. This increase may be due partly to a higher prevalence of cataract among women8 and perhaps also may be related to higher utilization of health care services by women.9 Second, blacks are almost 30 percent less likely to undergo cataract surgery than whites, and black males had the lowest cataract surgery rates of any ethnic or gender group. This difference cannot be fully explained by an expected difference in the prevalence of cataract.10;11 This finding of reduced utilization of health care by blacks in the United States is consistent with previous research performed nearly 20 years ago, and highlights the lack of progress made on improving the delivery of care in this area. In 1991, Sommer et al. reported cataract as the leading cause of blindness in African Americans in the Baltimore Eye Survey.12
Using 1986-87 Medicare claims data, Javitt et al found that whites were 27% more likely than blacks to undergo cataract surgery and that black males were only 57% as likely to undergo cataract surgery as white females.8 Using data nearly 20 years later, our findings suggest these racial differences persist. Previous reports have also suggested that blacks are less likely to see eye care providers in the first place,13 and may be more resigned to age-related loss of vision and less aware of the potential benefits of cataract surgery.14 As previously documented, socioeconomic status, including level of education of the population, may also be important;2;15 however, this possibility could not be examined in this investigation.
Based on our findings regarding the age, gender and race specific rates of cataract surgery in the Medicare population in 2003 and 2004, we can speculate regarding the volume of cataract surgery anticipated 10 and 20 years from now. Using the United States government's projections of population growth and distribution and current age, race and gender-associated rates of surgery, by applying age-stratified rates of surgery to the projected number of elderly in each age stratification, we estimate that approximately 3.3 million surgeries will be performed in 2020 and 4.4 million cataract surgeries will be performed in 2030 among individuals aged 65 and older in the United States. Of course, this estimate implies that adequate surgical manpower will exist, and should patient and surgeon thresholds for surgery fall as they have done over the past 30 years, then the total number of surgeries in this age group would be higher still.
During the period of 2003-2004, approximately half of the cataract surgeries performed on Medicare beneficiaries occurred in ASCs. Although the complexities regarding hospital costs, financing and reimbursement are well beyond the scope of this investigation, one can readily make rough estimates of the effect on cost to Medicare based on the site of surgery. For example, if the facility costs to Medicare were, on average, $675 dollars greater (Corcoran, Kevin J, Personal Communication, April 2010, Corcoran Consulting Group, San Bernardino, CA) at a hospital than at an ASC, then the annual savings to Medicare would be on the order of six hundred million dollars if cataract surgery were predominantly performed in ASCs.
We found that surgeon volume and surgical location also were closely associated, with lower-volume surgeons more likely to use hospital facilities and higher-volume surgeons more likely to use ASCs. This association may relate to the greater efficiencies typically found in privately-owned ASCs compared with hospitals. Higher-volume surgeons were much more likely to operate on the second eye within the two-year window covered in this analysis and to perform the second surgery within a shorter time period than were lower-volume surgeons who performed second-eye operations within the study time period. This again likely reflects an evolution, over time, towards a lowering of patient and surgeon thresholds for surgery. Whether this difference provides benefit to the patient cannot be analyzed with the current data. Medicare administrative datasets do not provide information related to the quality of care or the appropriateness of the timing of surgery. Certainly, performing second eye surgery within shorter time frames has some potential benefits, given of course, that the first eye is healing uneventfully, and surgery on the second eye is independently indicated. Such benefits include less disruption from anisometropia, quicker improvement in quality of life related to vision, and often reduced travel and costs. The data set we analyzed was limited to Medicare beneficiaries covered under the standard FFS arrangement. Previous research has indicated that insurance payment structure and cataract surgical rates are related, with HMO-managed patients having lower rates.16 Unfortunately, including HMO-managed patient data is not possible since claims are not generated as in the fee-for-service sector.
Finally, we note approximately a two-fold variability in cataract surgery rates by state, which persists after adjustment for age, gender and race. We also could not explain the variability based on the number of optometrists or ophthalmologists in the state. A 1.5 fold variation in cataract surgery across large geographic regions was reported 25 years ago.17 Similar cataract surgical rates and regional variation also have been reported recently from the Province of Ontario in Canada;18 and this modest variability is also consistent with what we reported, based on smaller geographic regions from Medicare data from 1986 and 1987.13 Similar variation in rates has been reported across entire states for cardiovascular procedures, where the rate of coronary artery bypass grafting had a 1.83 fold variation across 11 states,19 and in urological surgical procedures where surgery rates for benign prostatic hyperplasia are at least two-fold higher in Florida as compared to other states.20
Use of the Medicare billing database provides a unique and nationally representative view of the delivery of cataract surgical services to individuals aged 65 and older in the United States. Medicare accounts for the majority of the cataract surgery performed in this age group and covers all states with a uniform administrative methodology. All individuals aged 65 and older eligible for Medicare Part A are automatically enrolled. Enrollment in Part B is optional, but 96% of those enrolled in Part A in July, 2004 also were enrolled in Part B.7 This administrative database provides summary characteristics regarding the population undergoing surgery, the site of surgery and the surgeons performing the surgery.
In summary, the rate of cataract surgery in 2003 and 2004 was 61.8 surgeries per 1,000 person-years with substantial variation by age, gender and race. As the population demography of the United States shifts over the next few decades to ever greater proportions of those 65 and older, rates of cataract surgery will have important implications for estimating ophthalmology manpower needs as well as for the costs of eye care.
Acknowledgments
This research was funded by grant EY016769-01 from the National Eye Institute, National Institutes of Health. Dr. Gower is the recipient of an Ernest and Elizabeth Althouse Special Scholars Award from Research to Prevent Blindness.
Footnotes
Financial Conflicts of Interest: None
Reference List
- 1.Erie JC, Baratz KH, Hodge DO, et al. Incidence of cataract surgery from 1980 through 2004: 25-year population-based study. Journal of Cataract & Refractive Surgery. 2007;33:1273–7. doi: 10.1016/j.jcrs.2007.03.053. [DOI] [PubMed] [Google Scholar]
- 2.Javitt JC, Kendix M, Tielsch JM, et al. Geographic variation in utilization of cataract surgery. Med Care. 1995;33:90–105. doi: 10.1097/00005650-199501000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Kozak LJ, McCarthy E, Pokras R. Changing patterns of surgical care in the United States, 1980-1995. Health Care Financ Rev. 1999;21:31–49. [PMC free article] [PubMed] [Google Scholar]
- 4.Powe NR, Schein OD, Gieser SC, et al. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Cataract Patient Outcome Research Team. Arch Ophthalmol. 1994;112:239–52. doi: 10.1001/archopht.1994.01090140115033. [DOI] [PubMed] [Google Scholar]
- 5.West ES, Behrens A, McDonnell PJ, et al. The incidence of endophthalmitis after cataract surgery among the U.S. Medicare population increased between 1994 and 2001. Ophthalmology. 2005;112:1388–94. doi: 10.1016/j.ophtha.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg EP, Javitt JC, Sharkey PD, et al. The content and cost of cataract surgery. Arch Ophthalmol. 1993;111:1041–9. doi: 10.1001/archopht.1993.01090080037016. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services. Medicare Enrollment - Aged Beneficiaries: as of July 2004. [Accessed 4-7-2009];2010 http://www.cms.hhs.gov/MedicareEnRpts/Downloads/04Aged.pdf. [PubMed]
- 8.Congdon N, Vingerling JR, Klein BE, et al. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004;122:487–94. doi: 10.1001/archopht.122.4.487. [DOI] [PubMed] [Google Scholar]
- 9.Pinkhasov RM, Wong J, Kashanian J, et al. Are men shortchanged on health? Perspective on health care utilization and health risk behavior in men and women in the United States. Int J Clin Pract. 2010;64:475–87. doi: 10.1111/j.1742-1241.2009.02290.x. [DOI] [PubMed] [Google Scholar]
- 10.Munoz B, West SK, Rubin GS, et al. Causes of blindness and visual impairment in a population of older Americans: The Salisbury Eye Evaluation Study. Arch Ophthalmol. 2000;118:819–25. doi: 10.1001/archopht.118.6.819. [DOI] [PubMed] [Google Scholar]
- 11.West SK, Munoz B, Schein OD, et al. Racial differences in lens opacities: the Salisbury Eye Evaluation (SEE) project. Am J Epidemiol. 1998;148:1033–9. doi: 10.1093/oxfordjournals.aje.a009579. [DOI] [PubMed] [Google Scholar]
- 12.Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. N Engl J Med. 1991;325:1412–7. doi: 10.1056/NEJM199111143252004. [DOI] [PubMed] [Google Scholar]
- 13.Orr P, Barron Y, Schein OD, et al. Eye care utilization by older Americans: the SEE Project. Salisbury Eye Evaluation. Ophthalmology. 1999;106:904–9. doi: 10.1016/s0161-6420(99)00508-4. [DOI] [PubMed] [Google Scholar]
- 14.Williams A, Sloan FA, Lee PP. Longitudinal rates of cataract surgery. Arch Ophthalmol. 2006;124:1308–14. doi: 10.1001/archopht.124.9.1308. [DOI] [PubMed] [Google Scholar]
- 15.Brown AF, Gross AG, Gutierrez PR, et al. Income-related differences in the use of evidence-based therapies in older persons with diabetes mellitus in for-profit managed care. J Am Geriatr Soc. 2003;51:665–70. doi: 10.1034/j.1600-0579.2003.00211.x. [DOI] [PubMed] [Google Scholar]
- 16.Goldzweig CL, Mittman BS, Carter GM, et al. Variations in cataract extraction rates in Medicare prepaid and fee-for-service settings. JAMA. 1997;277:1765–8. [PubMed] [Google Scholar]
- 17.Chassin MR, Brook RH, Park RE, et al. Variations in the use of medical and surgical services by the Medicare population. N Engl J Med. 1986;314:285–90. doi: 10.1056/NEJM198601303140505. [DOI] [PubMed] [Google Scholar]
- 18.Hatch WV, Cernat G, Singer S, Bell CM. A 10-year population-based cohort analysis of cataract surgery rates in Ontario. Can J Ophthalmol. 2007;42:552–6. [PubMed] [Google Scholar]
- 19.Hannan EL, Wu C, Chassin MR. Differences in per capita rates of revascularization and in choice of revascularization procedure for eleven states. BMC Health Serv Res. 2006;6:35. doi: 10.1186/1472-6963-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sung JC, Curtis LH, Schulman KA, Albala DM. Geographic variations in the use of medical and surgical therapies for benign prostatic hyperplasia. J Urol. 2006;175:1023–7. doi: 10.1016/S0022-5347(05)00409-X. [DOI] [PubMed] [Google Scholar]