Abstract
Objectives
Changes in the parameters of inpatient psychiatric care have inspired a sizable literature exploring correlates of prolonged intervention as well as symptom change over varying lengths of hospitalization. However, existing data offer limited insight regarding the nature of symptom change over time. Objectives of this longitudinal research were to (a) model the trajectory of depressive symptoms within an inpatient psychiatric sample, (b) identify characteristics associated with unique patterns of change, and (c) evaluate the magnitude of expected gains using objective clinical benchmarks.
Methods
Participants included psychiatric inpatients treated between April 2008 and December 2010. Latent growth curve modeling was used to determine the trajectory of Beck Depression Inventory II depressive symptoms in response to treatment. Age, gender, trauma history, prior hospitalization, and DSM-IV diagnoses were examined as potential moderators of recovery.
Results
Results indicate a nonlinear model of recovery, with symptom reductions greatest following admission and slowing gradually over time. Female gender, probable trauma exposure, prior psychiatric hospitalization, and primary depressive diagnosis were associated with more severe trajectories. Diagnosis of alcohol/substance use, by contrast, was associated with more moderate trajectories. Objective benchmarks occurred relatively consistently across patient groups with clinically significant change occurring between 2–4 weeks post-admission.
Conclusion
The nonlinear trajectory of recovery observed in these data provides insight regarding the dynamics of inpatient recovery. Across all patient groups, symptom reduction was most dramatic in the initial week of hospitalization. However, notable improvement continued for several weeks post-admission. Results suggest timelines for adequate inpatient care are largely contingent on program-specific goals.
Keywords: inpatient treatment, psychiatric hospitalization, depression, symptom trajectory, latent growth curve modeling
Parameters of inpatient psychiatric care have changed significantly over the past several decades, in large part due to deinstitutionalization of mental health services and decreasing rates of payer reimbursement.1–3 Organizational shifts have contributed to overall reductions in the typical length of psychiatric hospitalization,4–5 inspiring a sizable literature exploring the impact of abbreviated hospitalization and factors contributing to extended care. To date, research comparing outcome across varying lengths of hospitalization is equivocal. Whereas symptom reduction from admission to discharge is noted consistently, shorter hospitalization has been associated with less,6 greater,7 and comparable 8–9 improvement across individual studies. Research examining correlates of admission length is more consistent. Prior hospitalization, initial symptom severity, and diagnoses of depressive, bipolar, and psychotic disorder typically are associated with more prolonged care.10–21 Substance use and adjustment-related pathology, by contrast, are related to shorter hospitalization.10,21 Associations with sociodemographic characteristics are noted in this literature but have been largely inconsistent.10,22
Extant research provides descriptive parameters for inpatient care, but the ability of these data to inform psychiatric practice is limited by a number of issues. First, duration of hospitalization is of limited use as an outcome for most clinical applications. Psychiatric hospitalization is a locus of treatment, serving as only an imperfect proxy for the frequency and intensity of specific interventions administered in that setting. Correlates of admission length inform hypotheses regarding factors influencing recovery, but treatment-focused outcomes including symptom severity, psychiatric distress, and adaptive functioning serve as the primary determinants for adequacy of care. Research targeting treatment-focused outcomes is arguably of greater use for guiding intervention and policy.
Second, research targeting treatment-focused outcomes generally is limited to the assessment of pre- to post-treatment change. Symptom reduction from admission to discharge provides only limited information regarding the nature or trajectory of change. Analysis of individual patterns of recovery could help determine (a) an expected trajectory of symptom change; (b) patients who may benefit from increased or specialized services; and (c) empirically-derived targets for timing of intervention.
Finally, data frequently are evaluated without considering the specific goals of intervention. Facilities seeking to optimize post-discharge functioning may benefit from a more extended timeline of care while brief admissions may be sufficient for programs targeting acute psychiatric stabilization. Although frequently overlooked, program-specific objectives become central in evaluating the clinical implications of existing research and in establishing benchmarks for the adequacy of intervention.
Given these considerations, the current research had three primary aims. The first was to determine the trajectory of depressive symptoms over the course of hospitalization in a large sample of psychiatric inpatients. Depressive symptoms were selected as a clinical outcome given their relevance among inpatient populations and close relationship with general distress.23 Symptom trajectories were estimated using latent growth curve (LGC) methods. Analyses provide a model of expected recovery based on individual patterns of change observed within the sample. The second aim was to identify factors impacting the trajectory of change over time. Existent research indicates a number of variables associated with intake severity, duration of admission, and rates of re-hospitalization, but the degree to which these factors influence the course of recovery is unknown. Age, sex, probable trauma history, prior psychiatric hospitalization, and presenting diagnosis were examined as potential moderators of recovery. The final aim was to evaluate the magnitude of expected recovery based on normative data and standards for clinically significant change.24 Analyses were intended to evaluate the adequacy of intervention in this sample and to inform expectations for psychiatric care more broadly.
Methods
Participants
Data were collected from psychiatric inpatients (N = 1084) hospitalized at a private, not-for-profit facility in the southwestern United States. Treatment objectives of this facility include clarifying diagnoses, addressing clinical symptoms, enhancing functional capacity, and facilitating adherence to a sustainable plan for post-discharge care. Patients were admitted between April 2008 and December 2010. Data from the most recent admission was used for patients with multiple hospitalizations during this period. Treatment programming was diverse and included medication management, psychoeducational groups, individual and group psychotherapy, addictions services, and structured interpersonal and recreational activities. Inclusion criteria for the final sample are detailed below (see Table 1).
Table 1.
Sample characteristics (N = 1084)
| Age | mean = 36.7 | SD = 14.9 |
|---|---|---|
| Sex (Female) | 539 | 49.7% |
| White/Caucasian | 980 | 90.4% |
| Hispanic | 38 | 3.5% |
| Relationship | ||
| Single | 568 | 52.4% |
| Cohabitating | 15 | 1.4% |
| Married | 320 | 29.5% |
| Separated | 63 | 5.8% |
| Divorced | 95 | 8.8% |
| Widowed | 13 | 1.2% |
| Employment | ||
| Full-Time | 283 | 26.1% |
| Part-Time | 179 | 16.5% |
| Unemployed | 521 | 57.3% |
| Retired | 100 | 9.2% |
| Disability | 92 | 8.5% |
| Trauma Exposure | 670 | 61.8% |
| Primary Dx | ||
| Depressive | 564 | 52.0% |
| Bi-polar | 178 | 16.4% |
| Psychotic | 79 | 7.3% |
| ETOH/Sub | 31 | 2.9% |
| Secondary Dx a | ||
| Depressive | 161 | 10.6% |
| Bi-polar | 18 | 1.2% |
| Psychotic | 18 | 1.2% |
| ETOH/Sub | 566 | 37.3% |
| Previous | ||
| Hospitalization | 664 | 61.3% |
| Length of Stay (days) | mean = 33.8 | SD = 16.9 |
Secondary diagnoses include any additional diagnoses contained within the medical record
Procedure
Data were collected as part of a larger treatment outcome study monitoring longitudinal response to inpatient care.25 A standardized assessment battery was completed on admission with follow-up measures administered at 2-week intervals for the duration of hospitalization. Diagnoses were established by clinical treatment teams and attending psychiatrist, consistent with DSM-IV criteria. All data collection procedures were approved through the facility’s institutional review board and were incorporated as a component of routine clinical care. See Allen and colleagues for full details.25
Measures
Background information
Background information was collected at admission. History of probable trauma exposure and previous psychiatric hospitalization were of particular interest for this study. Probable trauma history was assessed using a 14-item screening measure developed for use within inpatient settings.26 Trauma history was coded as a dichotomous variable (0 = absent, 1 = present) based on endorsement of at least one item on this measure. Previous psychiatric hospitalization – not limited to this facility – also was coded as a dichotomous indicator (0 = absent, 1 = present).
Beck Depression Inventory-II (BDI-II)
The BDI-II 27 was used to assess depressive symptomatology at admission and bi-weekly for the duration of hospitalization. Prior research provides evidence for the internal consistency (α = .91–.93), test-retest reliability (r = .93), and convergent/discriminant validity of this measure.27–29 Interpretive guidelines for the BDI-II are as follows: ≤ 13 minimal; 14 – 19 mild; 20 – 28 moderate; 29 – 63 severe. Admission scores at this facility were characteristic of those observed in other inpatient samples.7,30–32 Scores at each assessment were univariate normal with excellent internal consistency (α = .93–.94).33
Analytic Approach
Analysis
Latent growth curve (LGC) analysis was used to model expected trajectory of recovery. LGC methods assume that patterns of observed change emerge as a consequence of underlying processes estimated as a series of growth parameters. Parameters associated with different types of change (e.g., linear, quadratic) are specified to best approximate patterns observed in the data. With this approach, patient-specific trajectories initially are aggregated to form a model of baseline change; however, predictors of patient-specific change may be included in cases where individual trajectories vary meaningfully from the aggregate baseline model.
Analyses were conducted using a stepped approach consistent with Bollen and Curran.34 First, a baseline model was estimated, providing an overall trajectory of expected recovery. Models specifying both linear and quadratic change were explored. Next, variance estimates for the baseline model were examined to determine whether patient-specific trajectories deviated meaningfully from parameters in the baseline model. Significant estimates suggest the presence of unique trajectories that may be related to patient-specific factors (e.g., change in females differs from change in males). Finally, predictors were incorporated to form a final model of patient-specific change. Predictors in the final model were grand-mean centered. Effects indicate unique associations between patient factors and expected change, controlling for other variables in the model.
Data structure
Analyses were conducted using MPlus 6.1 software with maximum likelihood (ML) estimation.35 A notable feature of ML is the ability to accommodate cases with partially missing values. Model parameters are estimated using all available information and remain unbiased when missingness is either (a) unrelated to any variable in the model, or (b) associated with variables in the model but independent when accounting for these factors.36 For the current sample, missingness was primarily a product of differences in length of admission (i.e., cases with longer admission recorded a greater number of assessments than those with shorter admissions). Given that (a) missing data at later assessments was a direct function of admission length and (b) admission length was explicitly accounted for in the model, data were considered appropriate for ML estimation.
Model Fit
The comparative fit index (CFI), Tucker-Lewis index (TLI), root-mean-square of approximation (RMSEA), and standardized root-mean-square residual (SRMR) were used to evaluate model fit. Based on previous recommendations, CFI and TLI > .90, RMSEA < .08, and SRMR < .10 were considered evidence of adequate fit.37–39 CFI and TLI > .95, RMSEA < .06, and SRMR < .08 were indicative of close fit.40
Results
Data screening and preparation
Diagnostic information and symptom data were available for 1197 individuals. Of these, 5 cases were excluded due to record errors, and 13 were removed given incomplete background information. Patients hospitalized beyond the 8-week assessment period (n = 95) also were excluded given concerns regarding model convergence and parameter stability. Relative to the final sample (N = 1084), patients with more extended hospitalization were younger (mean = 31.3, SD = 13.0; p < .001), more likely to be female (66.3%; p = .002), more likely to report prior psychiatric hospitalization (71.6%; p = .047), less likely to have a primary diagnosis of a psychotic disorder (1.1%; p = .020), and evidenced higher BDI-II scores at admission (mean = 29.7, SD = 11.7; p = .001). Extended hospitalization was unrelated to probable trauma history or primary diagnoses of depressive, bipolar, or substance use disorders. Demographic information for the final sample is provided in Table 1.
Baseline Model: What is the expected trajectory of symptoms?
Baseline linear and quadratic models were examined to determine the overall shape of recovery. Models were specified according to Muthén and Muthén with loadings for growth parameters weighted to reflect time - in weeks - since admission (i.e., 0, 2, 4, 6, 8).35 Latent growth factors were regressed onto length of admission (mean centered) to account for missingness and to control for variability in duration of hospitalization. Bootstrapped standard errors and bias-corrected confidence intervals were estimated using 2000 redraws from the original sample. Means, standard deviations, and correlations are presented in Table 2.
Table 2.
Correlations, variances, means, and standard deviations
| LOA | BDI-II0 (N = 1080) | BDI-II2 (N = 870) | BDI-II4 (N = 649) | BDI-II6 (N = 483) | BDI-II8 (N = 191) | Sex | Age | Trma | Inpt | Dep | BP | Psyc | Sub | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LOA | 286.09 | |||||||||||||
| BDI-II0 | .20** | 173.01 | ||||||||||||
| BDI-II2 | .24** | .60** | 137.79 | |||||||||||
| BDI-II4 | .20** | .44** | .71** | 114.22 | ||||||||||
| BDI-II6 | .19** | .36** | .62** | .75** | 98.51 | |||||||||
| BDI-II8 | .07 | .28** | .46** | .62** | .80** | 81.97 | ||||||||
| Sex | −.06 | −.21** | −.11** | −.08* | −.07 | −.10 | .25 | |||||||
| Age | −.08** | .01 | −.04 | −.02 | −.04 | −.00 | .01 | 221.29 | ||||||
| Trma | .01 | .10** | .04 | .01 | −.05 | −.02 | −.10** | −.07* | .24 | |||||
| Inpt | .06* | .15** | .17** | .14** | .13** | .12 | −.10** | −.02 | .10** | .24 | ||||
| Dep | .09** | .19** | .07* | .06 | .02 | .00 | −.08** | .14** | .01 | −.06 | .25 | |||
| BP | −.02 | .02 | −.01 | −.02 | .03 | .07 | −.06* | .01 | .04 | .14** | −.46** | .14 | ||
| Psyc | −.07* | −.13** | −.05 | −.01 | −.03 | −.09 | .14** | −.15** | −.04 | .06* | −.29** | −.12** | .07 | |
| Sub | −.09** | −.14** | −.07 | −.06 | −.06 | − | .07* | .02 | −.00 | −.01 | −.18** | −.08* | −.05 | .03 |
| mean | 33.78 | 25.11 | 14.66 | 11.38 | 9.20 | 7.57 | .50 | 36.73 | .62 | .61 | .52 | .16 | .07 | .03 |
| SD | 16.91 | 13.15 | 11.74 | 10.69 | 9.23 | 9.05 | .50 | 14.88 | .49 | .49 | .50 | .37 | .26 | .17 |
Note: Variances provided along the diagonal; LOA = length of admission; BDI-II = Beck Depression Inventory II [subscripts indicate scores from admission to week 8]; Trma = probable trauma history; Inpt = previous psychiatric hospitalization; Dep = primary depressive diagnosis; BP = primary bipolar diagnosis; Psyc = primary psychotic disorder diagnosis; Sub = primary alcohol/substance use diagnosis.
p ≤ .05
p ≤ .01
Fit of the baseline linear model was poor (χ2(13) = 304.11; p < .001) with CFI (.80), TLI (.77), RMSEA (.14; CI90 = .13, .16) and SRMR (.23) all below standards for acceptable fit. The baseline quadratic model evidenced substantially better fit (χ2(8) = 58.28; p < .001). CFI (.97), TLI (.93), and RMSEA (.08; CI90 = .06, .10) values were adequate although SRMR (.17) remained elevated. Growth parameters for this model (intercept = 24.70; slope = −5.68; quadratic = .45) indicated a trajectory of decreasing gains over time, controlling for length of admission. The baseline quadratic model was selected for further examination given evidence of superior fit. Variance estimates for intercept, slope, and quadratic parameters all were significant (p < .001), indicating the presence of meaningful patient-specific trajectories.
Final Model: What factors impact symptom trajectory?
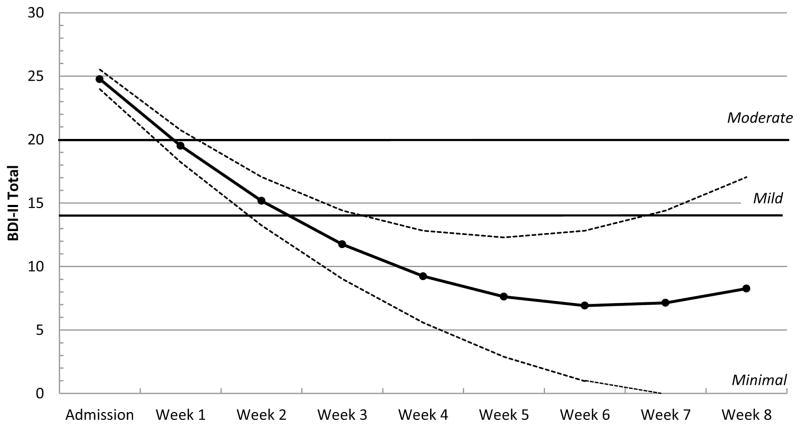
Age, sex, probable trauma history, previous psychiatric hospitalization, and presenting diagnosis (i.e., depressive, bipolar, psychotic, alcohol/substance disorder) were introduced in the final model, resulting in improved fit (χ224 = 74.80, p < .001; CFI = .97; TLI = .93; RMSEA = .04; CI90 = .03, .06; SRMR = .08). Expected trajectory of recovery for the final model (with 95% confidence bands) is presented in Figure 1.
Figure 1.
Expected symptom trajectory with 95% confidence bands a
a BDI-II = Beck Depression Inventory II; Bold horizontal lines denote cut points for mild (BDI-II = 14), and moderate (BDI-II = 20) depressive symptoms.
Intercept (expected BDI-II score at admission) for the final model was 24.77. Males (p <.001) and patients presenting with alcohol/substance disorders (p = .004) evidenced lower admission scores than other groups. By contrast, probable trauma exposure (p = .024), previous psychiatric hospitalization (p < .001), and primary depressive diagnosis (p < .001) were associated with higher scores at admission (see Table 3).
Table 3.
Parameter estimates for the final quadratic growth model
| M (SE) | β | b | SE | 95% CI | p | |
|---|---|---|---|---|---|---|
| Intercept | 24.77 (0.39) | [23.98 to 25.52] | ||||
| LOA | 0.16 | 0.11 | 0.02 | [0.06 to 0.15] | < .001 | |
| Sex | −0.18 | −3.94 | 0.73 | [−5.39 to −2.41] | < .001 | |
| Age | < 0.01 | < 0.01 | 0.03 | [−0.05 to 0.05] | .986 | |
| Inpatient | 0.15 | 3.47 | 0.80 | [1.81 to 4.98] | < .001 | |
| Trauma | 0.07 | 1.70 | 0.75 | [0.14 to 3.10] | .024 | |
| Depressive | 0.19 | 4.20 | 0.96 | [2.31 to 6.18] | < .001 | |
| Bipolar | 0.06 | 1.82 | 1.26 | [−0.55 to 4.41] | .148 | |
| Psychotic | −0.06 | −2.40 | 1.74 | [−5.60 to 1.26] | .166 | |
| Substance | −0.09 | −5.99 | 2.07 | [−10.08 to −1.98] | .004 | |
| Slope | −5.70 (0.21) | [7.79 to 16.69] | ||||
| LOA | 0.29 | 0.07 | 0.01 | [0.04 to 0.09] | < .001 | |
| Sex | 0.11 | 0.81 | 0.36 | [0.12 to 1.53] | .026 | |
| Age | −0.06 | −0.02 | 0.01 | [−0.04 to 0.01] | .182 | |
| Inpatient | < 0.01 | 0.03 | 0.37 | [−0.68 to 0.77] | .932 | |
| Trauma | −0.10 | −0.80 | 0.36 | [−1.53 to −0.10] | .027 | |
| Depressive | −0.19 | −1.42 | 0.46 | [−2.36 to −0.58] | .002 | |
| Bipolar | −0.09 | −0.92 | 0.61 | [−2.10 to 0.29] | .128 | |
| Psychotic | 0.08 | 1.12 | 0.87 | [−0.69 to 2.80] | .198 | |
| Substance | 0.09 | 1.94 | 1.04 | [−0.01 to 4.15] | .063 | |
| Quadratic | 0.46 (0.04) | [0.05 to 0.20] | ||||
| LOA | −0.42 | −0.01 | < 0.01 | [−0.01 to −0.01] | < .001 | |
| Sex | −0.05 | −0.05 | 0.05 | [−0.14 to 0.04] | .311 | |
| Age | 0.05 | < 0.01 | < 0.01 | [−0.01 to 0.01] | .372 | |
| Inpatient | −0.04 | −0.03 | 0.05 | [−0.12 to 0.05] | .494 | |
| Trauma | 0.08 | 0.07 | 0.05 | [−0.02 to 0.16] | .123 | |
| Depressive | 0.15 | 0.12 | 0.06 | [0.02 to 0.23] | .027 | |
| Bipolar | 0.09 | 0.11 | 0.07 | [−0.04 to 0.25] | .145 | |
| Psychotic | −0.10 | −0.15 | 0.12 | [−0.38 to 0.08] | .187 | |
| Substance | −0.10 | −0.25 | 0.16 | [−0.61 to 0.01] | .104 |
Note: M = fixed effect [i.e, mean parameter] for the conditional model; SE = standard error; LOA = length of admission; Inpatient = previous psychiatric hospitalization; Trauma = probable trauma history; Depressive = primary depressive diagnosis; Bipolar = primary bipolar diagnosis; Psychotic = primary psychotic disorder diagnosis; Substance = primary alcohol/substance use diagnosis.
Slope (initial symptom reduction at admission) was −4.95 points/week controlling for length of admission and other variables. Initial reductions were greatest among females (p = .026), individuals endorsing previous trauma (p = .027), and patients presenting with a primary depressive disorder (p = .002). Correlation between slope and intercept parameters (r = −.388; p = .001) indicate more immediate symptom reduction among patients with higher intake scores.
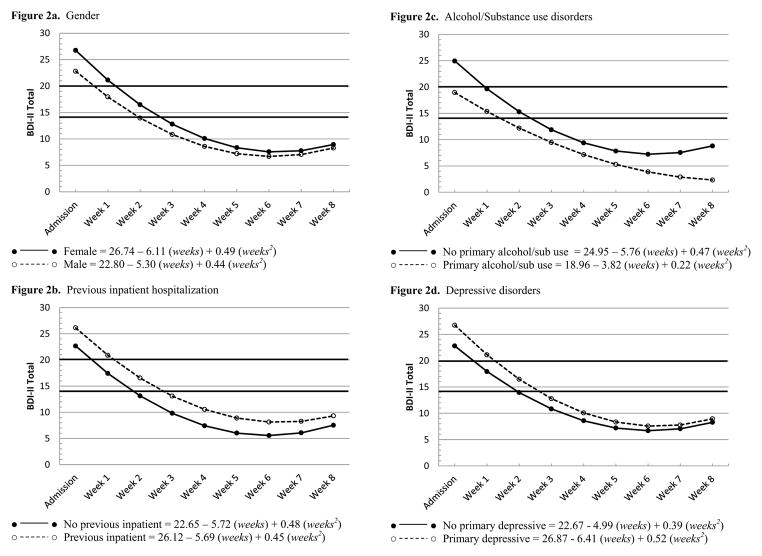
The quadratic parameter in this model (β2= .34) estimates the tapering of recovery over time. For these data, only primary depressive disorder was associated with quadratic change (p = .027). Specifically, more rapid flattening of recovery was expected among depressive patients relative to other diagnostic groups. Correlation between quadratic and slope parameters (r = −.923; p < .001) indicate increased deceleration of improvement in patients with more immediate gains. Trajectories associated with the most notable deviations from baseline are presented in Figure 2.
Figure 2.
Differential symptom trajectories across patient subgroupsa
a BDI-II = Beck Depression Inventory II; Bold horizontal lines denote cut points for mild (BDI-II = 14), and moderate (BDI-II = 20) depressive symptoms.
Clinical significance of expected change
Magnitude of expected recovery was evaluated using interpretive guidelines for the BDI-II and standards for clinically significant change.24,27 As illustrated in Figure 1, depressive symptoms were projected to remain in the moderate range through the initial week of hospitalization. Mild symptoms were expected to persist through week 2 before falling into the minimal range. Symptom reductions of at least 1 point/week were projected to continue through week 5. Model-implied change equaled 0 (i.e., no further reduction in symptoms) at around 6-weeks post-admission.
Standards for clinically significant change provide an alternative approach to evaluating outcome. Although definitions of clinically significant change vary given the availability of normative data, conservative estimates may be operationalized as the point at which a patient’s level of functioning becomes closer to the mean of a normative population than to the mean of the original dysfunctional sample.24 Based on a normative sample of adults,41 threshold for clinically significant change in this research was 12.19. Results suggest the average inpatient should achieve criteria for clinically significant change between 2- to 4-weeks post-admission given 95% confidence bands projected for these data.
Conclusions
Aims of the current study were to (a) determine the trajectory of symptom reduction over the course of psychiatric hospitalization, (b) identify patient characteristics associated with recovery, and (c) quantify the magnitude of expected change using accepted clinical benchmarks. LGC analysis provided a model of nonlinear recovery, with symptom reductions greatest at admission and slowing gradually over time. Unique trajectories were noted across several patient groups. Initial BDI-II scores were lower among patients with primary alcohol/substance use and higher among those reporting prior hospitalization. Women also evidenced higher scores at admission and more immediate symptom reduction than did men. Patients reporting probable trauma exposure evidenced a similar trajectory. Finally, patients with a primary depressive diagnosis demonstrated higher admission scores, greater immediate symptom reduction, but more rapid deceleration of recovery compared to other groups. Mild depressive symptoms were expected to persist through 2 weeks post-admission (excluding patients with primary alcohol/substance use) with clinically significant change occurring between weeks 2 and 4.
Results extend the existing inpatient literature by providing context for pre- to post-treatment changes noted in previous studies. Trajectories indicated recovery was most rapid in the first week of admission, consistent with previous research demonstrating statistically significant symptom reduction following even brief intervention.6–8,17,19 Factors contributing to immediate gains likely are multifaceted within this heterogeneous inpatient sample. Counter to delayed antidepressant response hypotheses,42–44 meta-analyses of double-blind, placebo-controlled antidepressant trials provide evidence for medication effects as early as 1–2 weeks among depressed samples.45 Further reviews note evidence for therapeutic effects of antipsychotic agents within 1–2 weeks among patients with serious mental illness.46 Symptom trajectories in the current study are strikingly similar to those noted in pharmacological trials, suggesting that medication effects could contribute to early treatment gains. Other factors influencing immediate response likely include the provision of basic needs (e.g., food, shelter, medical attention), removal of external stressors, detoxification from alcohol and substances, general supportive contact, sudden therapeutic gains,47–48 and/or regression to the mean.
Whereas symptom reduction was most rapid in the initial week of intervention, 70% of total expected gains occurred between weeks 1 and 6. The gradual deceleration of recovery during this period is reminiscent of trajectories documented across both medication and outpatient psychotherapy trials.45–46,49 Although speculative, this curvilinear trajectory – as well observed correlations between slope-intercept and quadratic-slope parameters – could be conceptualized as following principles similar to the law of initial value.50 Specifically, patients presenting to treatment in extreme distress could possess greater potential for immediate gains relative to those with more moderate symptoms, resulting in a steeper slope of initial recovery. Evidence of increased antidepressant response among patients with more severe depression is consistent with this hypothesis.51 However, the potential for continued improvement would decrease as patients approach a threshold of maximum expected gains. Continued incremental change may require increased time and therapeutic effort, resulting in an overall deceleration of recovery. Mechanisms underlying this pattern require further investigation, but evidence of common trajectories in response to both medication and psychotherapy trials would appear to favor more global processes over intervention-specific factors.
Finally, characteristics associated with prolonged intervention in previous research – gender, trauma exposure, previous psychiatric hospitalization, depressive diagnoses – evidenced symptom trajectories reflective of more severe psychopathology.10–21 The converse was true with respect to more moderate trajectories observed for primary alcohol/substance use.7,21 However, timelines for clinical benchmarks occurred with relative consistency and offer an empirical basis from which to inform program-specific objectives. Consistent with dose-response models of therapeutic change,52–53 results suggest that brief intervention (e.g., 1 week) is likely adequate for facilities targeting crisis management and acute safety. Programs targeting clinically significant change and enhanced functional capacity, by contrast, could benefit from more extended care (e.g., 2 – 4 weeks).
Interpretations should be made within the context of the study’s strengths and limitations. The sample was racially homogenous, and the prevalence of psychotic disorders was low relative to estimates for general community hospitals.23 Comparable symptom severity and relationships consistent with those noted in previous studies offer evidence of generalizability; however, replication within more diverse samples and settings is needed. Outcome also was limited to a single indicator of depressive symptomatology. Advantages of the BDI-II include established psychometric properties, interpretive norms, and the prevalence of depressive pathology among psychiatric inpatients. Regardless, future research would be strengthened by inclusion of alternative indicators of recovery. Continued research also would be strengthened through consideration of factors falling on other clinical axes. Personality dysfunction and health-related conditions have been shown to impact response to treatment, indicating the potential for unique trajectories of recovery within these groups.54–56 Finally, patients with prolonged admissions (> 8-weeks) were excluded given concern that estimating trajectories beyond 8-weeks in this limited subset of individuals (less that 10% of the total sample) would (a) produce instability in model parameters and (b) negatively impact the overall generalizability of results. However, individuals experiencing complicated and otherwise prolonged hospitalization represent an important subset of the inpatient population. Further research exploring symptom trajectories specifically within this difficult patient subset will be beneficial.
Results provide a model of expected recovery in response to multisystemic inpatient psychiatric intervention. Although the availability and parameters of psychiatric care often are determined by institutional factors (e.g., cost, space), these data demonstrate the viability of inpatient care for achieving acute stabilization as well as symptom remission across patients with a diverse range of psychiatric needs.
Clinical Points.
Reduction of depressive symptoms follows a curvilinear trajectory among psychiatric inpatients.
Symptom reduction is most rapid immediately following admission with improvement slowing gradually over time.
Despite evidence for unique trajectories of recovery, clinical benchmarks are relatively consistent across patient groups.
Acknowledgments
Funding/Support: This research was supported in part by funding from the Menninger Foundation, the McNair Medical Institute, and the National Institute of Mental Health. Dr. Frueh is a McNair Scholar. Dr. Clapp was a NIMH-sponsored intern at the Medical University of South Carolina (T32 MH18869) during the development of this project.
We are grateful for the assistance of all the research assistants at The Menninger Clinic.
Footnotes
Previous Presentation: None
Disclaimer: All authors fulfill the criteria for authorship. JGA, JM, JMO, TE, and BCF participated in the conception and design of this study; JDC, ALG, and JDE completed the data analyses; all authors participated in the interpretation of data, manuscript preparation, and all approve of the final version. JDC, JGA, and BCF together had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. There is no else who fulfills the criteria for authorship who has not been included as an author.
Potential conflicts of interest: Dr. Grubaugh serves as a research consultant for the Menninger Clinic. Dr. Clapp, Dr. Allen, Dr. Mahoney, Dr. Oldham, Dr. Fowler, Dr. Ellis, Dr. Elhai, and Dr. Frueh have no financial interests to disclose.
References
- 1.Geller J. History of hospital psychiatry and lessons learned. In: Sharfstein SS, Dickerson FB, Oldham JM, editors. Textbook of hospital psychiatry. Arlington, VA: American Psychiatric Publishing; 2009. pp. 1–20. [Google Scholar]
- 2.Mark T, Levit K, Coffey R, et al. National Expenditures for Mental Health Services and Substance Abuse Treatment, 1993–2003. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. SAMHSA Publication SMA 07-4227. [Google Scholar]
- 3.Oldham JM, Russakoff LM. The medical therapeutic community. J Psychiatr Treat & Eval. 1982;4(4):337–343. [Google Scholar]
- 4.Mechanic D, McAlpine D, Olfson M. Changing patterns of psychiatric inpatient care in the United States, 1988–1994. Arch Gen Psychiatry. 1998;55(9):785–791. doi: 10.1001/archpsyc.55.9.785. [DOI] [PubMed] [Google Scholar]
- 5.Hareen O, Dixon L, Gavirneni S, et al. The association between decreasing length of stay and readmission rate on a psychogeriatric unit. Psychiatr Serv. 2002;53(1):76–79. doi: 10.1176/appi.ps.53.1.76. [DOI] [PubMed] [Google Scholar]
- 6.Lieberman P, Wiitala S, Elliott B, et al. Decreasing length of stay: Are there effects on outcomes of psychiatric hospitalization? Am J Psychiatry. 1998;155(7):905–909. doi: 10.1176/ajp.155.7.905. [DOI] [PubMed] [Google Scholar]
- 7.Pettit J, Averill P, Wassef A, et al. Ratings of Early Major Depressive Disorder Symptom Change During a Brief Psychiatric Hospitalization. Psychiatr Q. 2005;76(1):33–48. doi: 10.1007/s11089-005-5579-x. [DOI] [PubMed] [Google Scholar]
- 8.Hirsch SR, Platt S, Knights A, et al. Shortening hospital stay for psychiatric care: Effect on patients and their families. Br Med J. 1979;1(16161):442–446. doi: 10.1136/bmj.1.6161.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Platt S, Hirsch S, Knights A. Effects of brief hospitalization on psychiatric patients’ behaviour and social functioning. Acta Psychiatr Scand. 1981;63(2):117–128. doi: 10.1111/j.1600-0447.1981.tb00658.x. [DOI] [PubMed] [Google Scholar]
- 10.Stevens A, Hammer K, Buchkremer G. A statistical model for length of psychiatric in-patient treatment and an analysis of contributing factors. Acta Psychiatr Scand. 2001;103(3):203–211. doi: 10.1034/j.1600-0447.2001.00043.x. [DOI] [PubMed] [Google Scholar]
- 11.Blader J. Acute inpatient care for psychiatric disorders in the United States, 1996 through 2007. Arch Gen Psychiatry. 2011;68(12):1276–1283. doi: 10.1001/archgenpsychiatry.2011.84. [DOI] [PubMed] [Google Scholar]
- 12.Choy L, Dunn E. Determinants of length of stay in a general hospital psychiatric unit in Hong Kong. Hong Kong Journal Of Psychiatry. 2007;17(4):131–138. [Google Scholar]
- 13.Cohen C, Casimir G. Factors associated with increased hospital stay by elderly psychiatric patients. Hosp Community Psychiatry. 1989;40(7):741–743. doi: 10.1176/ps.40.7.741. [DOI] [PubMed] [Google Scholar]
- 14.Draper B, Luscombe G. Quantification of factors contributing to length of stay in an acute psychogeriatric ward. Int J Geriatr Psychiatry. 1998;13(1):1–7. doi: 10.1002/(sici)1099-1166(199801)13:1<1::aid-gps716>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 15.Hallak J, Crippa J, Vansan G, et al. Diagnostic profile of inpatients as a determinant of length of stay in a general hospital psychiatric unit. Braz J Med Biol Res. 2003;36(9):1233–1240. doi: 10.1590/s0100-879x2003000900014. [DOI] [PubMed] [Google Scholar]
- 16.Herr B, Abraham H, Anderson W. Length of stay in a general hospital psychiatric unit. Gen Hosp Psychiatry. 1991;13(1):68–70. doi: 10.1016/0163-8343(91)90011-k. [DOI] [PubMed] [Google Scholar]
- 17.Hopko D, Lachar D, Bailley S, et al. Assessing predictive factors for extended hospitalization at acute psychiatric admission. Psychiatr Serv. 2001;52(10):1367–1373. doi: 10.1176/appi.ps.52.10.1367. [DOI] [PubMed] [Google Scholar]
- 18.Kirshner L, Johnston L. Length of stay on a short-term unit. Gen Hosp Psychiatry. 1985;7(2):149–155. doi: 10.1016/0163-8343(85)90028-3. [DOI] [PubMed] [Google Scholar]
- 19.Rocca P, Mingrone C, Bogetto F, et al. Outcome and length of stay in psychiatric hospitalization, the experience of the University Clinic of Turin. Soc Psychiatry Psychiatr Epidemiol. 2010;45(6):603–610. doi: 10.1007/s00127-009-0091-8. [DOI] [PubMed] [Google Scholar]
- 20.Shergill S, Ebrahim I, Greenberg M. Predictors of length of stay in day hospital patients. Psychiatric Bulletin. 1997;21(12):760–763. [Google Scholar]
- 21.Warnke I, Rössler W. Length of stay by ICD-based diagnostic groups as basis for the remuneration of psychiatric inpatient care in Switzerland? Swiss Med Wkly. 2008;138(35–36):520–527. doi: 10.4414/smw.2008.12108. [DOI] [PubMed] [Google Scholar]
- 22.Sajatovic M, Donenwirth K, Sultana D, et al. Admissions, length of stay and medication use among women in an acute care state psychiatric facility. Psychiatr Serv. 2000;51(10):1278–1281. doi: 10.1176/appi.ps.51.10.1278. [DOI] [PubMed] [Google Scholar]
- 23.Saba DK, Levit KR, Elixhauser A. [Accessed December 9, 2011];Statistical Brief #62: Hospital stays related to mental health 2006. 2008 Oct; http://www.hcup-us.ahrq.gov/reports/statbriefs/sb62.pdf. [PubMed]
- 24.Jacobson N, Truax P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J Consult Clin Psychol. 1991;59(1):12–19. doi: 10.1037//0022-006x.59.1.12. [DOI] [PubMed] [Google Scholar]
- 25.Allen JG, Frueh BC, Ellis TE, et al. Integrating outcomes assessment and research into clinical care in inpatient adult psychiatric treatment. Bull Menninger Clin. 2009;73(4):259–295. doi: 10.1521/bumc.2009.73.4.259. [DOI] [PubMed] [Google Scholar]
- 26.Allen JG, Coyne L, Huntoon J. Complex posttraumatic stress disorder in women from a psychometric perspective. J Pers Assess. 1998;70(2):277–298. doi: 10.1207/s15327752jpa7002_7. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 28.Beck AT, Steer RA, Ball R, et al. Comparison of Beck Depression Inventories-IA and -II in psychiatric outpatients. J Pers Assess. 1996;67(3):588–597. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- 29.Dozois DJA, Dobson KS, Ahnberg JL. A psychometric evaluation of the Beck Depression Inventory-II. Psychol Assess. 1998;10(2):83–89. [Google Scholar]
- 30.Krefetz D, Steer R, Gulab N, et al. Convergent validity of the Beck Depression Inventory-II with the Reynolds Adolescent Depression Scale in psychiatric inpatients. J Pers Assess. 2002;78(3):451–460. doi: 10.1207/S15327752JPA7803_05. [DOI] [PubMed] [Google Scholar]
- 31.Osman A, Kopper B, Barrios F, et al. Reliability and validity of the Beck Depression Inventory--II with adolescent psychiatric inpatients. Psychol Assess. 2004;16(2):120–132. doi: 10.1037/1040-3590.16.2.120. [DOI] [PubMed] [Google Scholar]
- 32.Steer R, Rissmiller D, Beck A. Use of Beck Depression Inventory-II with depressed geriatric inpatients. Behav Res Ther. 2000;38(3):311–318. doi: 10.1016/s0005-7967(99)00068-6. [DOI] [PubMed] [Google Scholar]
- 33.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4. Boston, MA: Allyn & Bacon; 2001. pp. 73–77. [Google Scholar]
- 34.Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- 35.Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- 36.Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 243–277. [Google Scholar]
- 37.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 38.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage Publications; 1993. pp. 136–162. [Google Scholar]
- 39.Kline RB. Principals and practice of structural equation modeling. 2. New York: Guilford Press; 2005. [Google Scholar]
- 40.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 41.Trahan DE, Ross CE, Trahan SL. Relationships among postconcussional-type symptoms, depression, and anxiety in neurologically normal young adults and victims of mild brain injury. Arch Clin Neuropsychol. 2001;16(5):435–445. [PubMed] [Google Scholar]
- 42.Hordern A. The antidepressant drugs. N Engl J Med. 1965;272(22):1159–1169. doi: 10.1056/NEJM196506032722206. [DOI] [PubMed] [Google Scholar]
- 43.Klerman GL, Hirschfeld RMA. The use of antidepressant drugs in clinical practice. JAMA. 1978;240(13):1403–1406. [PubMed] [Google Scholar]
- 44.Quitkin FM, Rabkin JG, Ross D, McGrath PJ. Duration of antidepressant drug treatment: What is an adequate trial? Arch Gen Psychiatry. 1984;41(3):238–245. doi: 10.1001/archpsyc.1984.01790140028003. [DOI] [PubMed] [Google Scholar]
- 45.Posternak MA, Zimmerman M. Is there a delay in the antidepressant effect? A meta-analysis. J Clin Psychiatry. 2005;66(2):148–158. doi: 10.4088/jcp.v66n0201. [DOI] [PubMed] [Google Scholar]
- 46.Agid O, Kapur S, Arenovich T, Zipursky RB. Delayed-onset hypothesis of antipsychotic action: A hypothesis tested and rejected. Arch Gen Psychiatry. 2003;60(12):1228–1235. doi: 10.1001/archpsyc.60.12.1228. [DOI] [PubMed] [Google Scholar]
- 47.Stiles W, Leach C, Hardy G, et al. Early sudden gains in psychotherapy under routine clinic conditions: Practice-based evidence. J Consult Clin Psychol. 2003;71(1):14–21. [PubMed] [Google Scholar]
- 48.Tang T, DeRubeis R. Reconsidering rapid early response in cognitive behavioral therapy for depression. Clin Psychol Sci Prac. 1999;6(3):283–288. [Google Scholar]
- 49.Lutz W, Stulz N, Köck K. Patterns of early change and their relationship to outcome and follow-up among patients with major depressive disorders. J Affect Disord. 2009;118(1–3):60–68. doi: 10.1016/j.jad.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 50.Wilder J. Modern psychophysiology and the law of initial value. Am J Psychother. 1958;12(2):199–221. doi: 10.1176/appi.psychotherapy.1958.12.2.199. [DOI] [PubMed] [Google Scholar]
- 51.Khan A, Brodhead A, Kolts R, Brown W. Severity of depressive symptoms and response to antidepressants and placebo in antidepressant trials. J Psychiatr Res. 2005;39(2):145–150. doi: 10.1016/j.jpsychires.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 52.Howard K, Lueger R, Maling M, Martinovich Z. A phase model of psychotherapy outcome: Causal mediation of change. J Consult Clin Psychol. 1993;61(4):678–685. doi: 10.1037//0022-006x.61.4.678. [DOI] [PubMed] [Google Scholar]
- 53.Haase M, Frommer J, Schmitz N, et al. From symptom relief to interpersonal change: Treatment outcome and effectiveness in inpatient psychotherapy. Psychother Res. 2008;18(5):615–624. doi: 10.1080/10503300802192158. [DOI] [PubMed] [Google Scholar]
- 54.Ilardi S, Craighead W, Evans D. Modeling relapse in unipolar depression: The effects of dysfunctional cognitions and personality disorders. J Consult Clin Psychol. 1997;65(3):381–391. doi: 10.1037//0022-006x.65.3.381. [DOI] [PubMed] [Google Scholar]
- 55.Lyketsos C, Dunn G, Kaminsky M, Breakey W. Medical comorbidity in psychiatric inpatients: Relation to clinical outcomes and hospital length of stay. Psychosomatics. 2002;43(1):24–30. doi: 10.1176/appi.psy.43.1.24. [DOI] [PubMed] [Google Scholar]
- 56.Sloan D, Yokley J, Gottesman H, Schubert D. A five-year study on the interactive effects of depression and physical illness on psychiatric unit length of stay. Psychosom Med. 1999;61(1):21–25. doi: 10.1097/00006842-199901000-00005. [DOI] [PubMed] [Google Scholar]