Abstract
Background: Effective leadership is of prime importance in any organization and it goes through changes based on accepted health promotion and behavior change theory. Although there are many leadership styles, transformational leadership, which emphasizes supportive leadership behaviors, seems to be an appropriate style in many settings particularly in the health care and educational sectors which are pressured by high turnover and safety demands. Iran has been moving rapidly forward and its authorities have understood and recognized the importance of matching leadership styles with effective and competent care for success in health care organizations. This study aimed to develop the Supportive Leadership Behaviors Scale based on accepted health and educational theories and to psychometrically test it in the Iranian context.
Methods: The instrument was based on items from established questionnaires. A pilot study validated the instrument which was also cross-validated via re-translation. After validation, 731 participants answered the questionnaire.
Results: The instrument was finalized and resulted in a 20-item questionnaire using the exploratory factor analysis, which yielded four factors of support for development, integrity, sincerity and recognition and explaining the supportive leadership behaviors (all above 0.6). Mapping these four measures of leadership behaviors can be beneficial to determine whether effective leadership could support innovation and improvements in medical education and health care organizations on the national level. The reliability measured as Cronbach’s alpha was 0.84.
Conclusion: This new instrument yielded four factors of support for development, integrity, sincerity and recognition and explaining the supportive leadership behaviors which are applicable in health and educational settings and are helpful in improving self –efficacy among health and academic staff.
Keywords: Contextualization, Socio- cognitive Theory, Standardization, Supportive Leadership Behavior Questionnaire
Introduction
There are many leadership styles used by effective leaders, but two of the most common approaches are transactional and transformational styles. These styles are seen in a wide range of domains such as politics, business, education, sport, law (1), health system, nursing and police work (2). Transactional leadership is identified by a sense of duty based on reward and punishment to reach goals (3). In this style, emphasis is put on the interaction between leaders and their subordinates, asserting a sense of self-worth in the followers. Transformational leadership focuses on shaping change by emphasizing supportive leadership behavior (SLB) (4, 5) for which people feel inspired and committed. Leaders who make use of SLB show concern for followers’ needs, consideration and understanding, trust and respect, friendship and encouragement, and they help followers develop their abilities and careers. The transformational leadership approach leans toward a search of subordinates’ happiness (6). Based on the findings of some research in the healthcare sector and nursing, it is noteworthy to mention that transformational leadership styles can reduce work-life conflict (7), increase staff job satisfaction (7,8) and psychological wellbeing (7) and result in effectiveness and better leadership outcomes (9).
There is no one “right” way to lead in a way that fits all situations, but the implementation of transformational leadership and of SLB can be appropriate in many circumstances. This may become apparent in the current health care sector, which is pressured by a global shortage of health care workers, demanding patients and fiscal constraints. Employees are being asked to do more than ever before: making suggestions for continuous improvement, handling complex problems quickly, and taking greater responsibilities on the front line while the resources and support are being decreased. Due to the standardization of competences and globalization, in general employees do not tend to remain at the same job for their entire working career. Employees' loyalty has therefore shifted dramatically since the 60’s and 70’s (6). Employees bring value to the customer, especially in the health care system where effective quality care is promised and offered to the patient (6).Therefore, to keep a competent staff, which thrives and delivers effective quality patient care, leaders of health system organizations ought to make use of SLB (10). In one study conducted in nursing homes, a large number of nurses left their job because of insufficient communication skills, weak teamwork and non-supportive leadership in their workplace. In that study, it was revealed that the annual average turnover rate of the nurses was between 70% and 100%. Furthermore, it was demonstrated that this problem reduced the quality of care (11). Therefore, it was suggested that a supportive work environment be developed to solve this dilemma (11); other researchers also found the same results (8, 12).
Transformational leadership consequences on health sector call for more attention, and training should be provided based on key leadership competencies (8, 13). Due to the significant effect of leadership on health professions with the increasing complexities of medical education, leadership styles and their development have become increasingly important in medical education (14). Multiple studies have developed or researched many courses, programs, curricula, etc., to promote leadership styles in medical education (15-19).
The current Iranian research on leadership style and its effects on subordinates reveals that task-oriented behavior is the dominant style among Iranian leaders in the health care and educational systems (11). This style focuses on accomplishment and increases the rate of subordinates’ burn out (20). Research shows that in the field of medical education and health care, Iranian leaders should apply cooperative learning to improve critical thinking among their staff. Leaders should be able to encourage new ideas to promote the organizational outcomes, improve learning abilities, lead change and spur innovation among themselves and their followers (20).
Assessing the effects of SLB on subordinates' satisfaction and performance has provided valuable data for the health care administration in recent years, and it has had a tremendous effect on the quality of health care services (21, 22). In Iran, as in many other developing countries, employees are suffering from lack of supportive leadership (un- published data). More research on supportive leadership is needed to promote supportive leadership styles especially in healthcare and educational organizations, which need a valid and reliable tool to assess leaders' performance. The available instruments in the world may not be appropriate to assess SLB and its' correlation with educational theory in the Iranian context, and therefore developing a new instrument in this field is a serious demand. The aim of this study was to develop a valid tool for assessing supportive behavior among leaders by standardizing and developing the Iranian version of a SLB instrument for nurses through a cross-sectional and correlation study using factor analysis.
Methods
Design
This cross-sectional, correlational study consisted of a pilot study followed by the first phase of a randomized control trial (RCT) to develop and validate a questionnaire, which on a national level determines whether effective supportive leadership could maintain innovation and improvements in medical education institutions and health care organizations. The study was conducted between June 2009 and November 2010. The pilot study was conducted in June 2009 while the data for the first phase of the study were collected in September 2009 after the pilot study. Both phases of the study had been approved by The Ethical Committee of Tehran University of Medical Sciences, Tehran, Iran. All participants were informed about the study and its aims, and they participated in the project voluntarily.
Development of the Questionnaire
The first step in the development of the questionnaire items was reviewing the related literature on the concept of SLB. To the best of our knowledge, no similar questionnaire had been developed in Iran. Therefore, from the field of behavioral leadership, relevant SLB questions were extracted from the three different questionnaires of Developmental Leadership (DL), Hersey and Blanchard's Situational theory (HBS) and Ohio State (OSQ) (23-25); and then they were translated to Persian. A group of experts, consisting of two medical education specialists (MS, SJM), one management specialist in education (AE), one epidemiologist (SMA), and one researcher in the field of medical education (SJMM) assessed the first draft of the translated questionnaires. Questions were extracted from three original questionnaires (DL), (HBS) and (OSQ), which were not directly relevant to the supportive leadership behavior, but they had some questions pertaining to supportive leadership. The expert panel developed and added some new SLB related questions to make the questionnaire more complete and comprehensible. Finally, the first draft of the Iranian questionnaire consisting of a 50-item Likert-scale questionnaire was developed. The face and content validity of the instrument was ensured through the two rounds Delphi methods, and finally the results of Delphi was discussed in the expert panel and was approved by the consensus of the panel. The expert panel consisted of ten faculty members of TUMS from different fields (medical education, management, epidemiology and psychology), who were selected based on their specialty and availability. The responses were based on a five-point scale: “completely agree”, “agree”, “Do not know“, “disagree” and “completely disagree”. Scoring of each item was between one for “completely agree “to 5 for “completely disagree”. The instrument could yield an overall ranging from 40 to 200.
Pilot Study
The number of the participants in the pilot study was 20 nurses with different qualifications, who were excluded from the main sample population.
The reliability of the questionnaire was assessed via a test-retest approach. The questionnaire was answered twice by the participants of the pilot study and in a 10- day interval. We used Kappa as a measure of agreement between the two measurements. All the items with Kappa less than 0.7 were excluded because the agreement was low in those cases. The results of the assessment were discussed within the group of experts, and the required modifications were made accordingly. The remained number of the items in the questionnaire was 40, and the mean Kappa for all questions was 0.86.
To ensure external validity, the questionnaire was cross-validated by retranslating it to English and sending it to an authority in the field, Gerry Larsson, to seek his advice. The content validity of the questionnaire was assessed through the experts’ consensus. Finally, 40 items were determined. The instrument could yield an overall score ranging from 40 to 200.
The First Phase of the Study
The first phase of the study was conducted at all 16 hospitals of Tehran University of Medical Sciences (TUMS, the largest University located in the capital of Iran, Tehran) to determine the validity and reliability of the developed questionnaire. We assessed the leadership performance of 110 head nurses, including 6 subordinates for each head nurse, making a total of 660 subordinate nurses with different levels of nursing education such as registered nurses and nurse aids (N = 621); some of the nurses (N = 39), however, did not agree to participate in the study (Fig. 1). The total number of the participants was 731 and in order to increase the response rate, the researchers visited the participants and talked with them about the project, and this resulted in a response rate of 94%. We also provided credit points toward Continuing Nursing Education (CNE) to all those who answered the questionnaire.
Fig.1 .
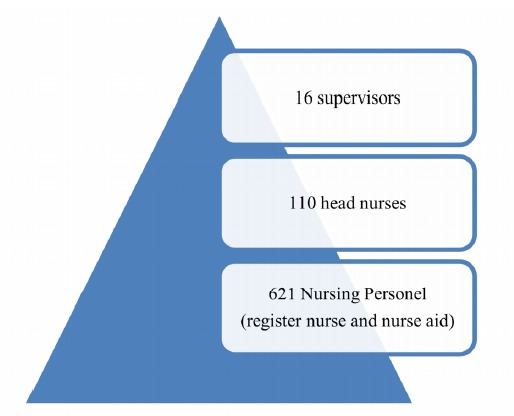
Hierarchy of nursing samples in the study
Statistical Analysis
To better understand the dimensions underlying the questionnaire, an exploratory factor analysis was conducted based on principle axis factoring and varimax rotation. This analysis was used for data reduction to identify a small number of factors that could explain most of the variance observed in a much larger number of manifest variables. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy in factor analysis was used. Cronbach’s Alphas were calculated to evaluate the internal reliability and item homogeneity of the scales. SPSS version 16 was used to analyze the data.
Nominating the Factors
The expert panel, consisting of one psychologist, two nursing management specialists, and two medical educationalists nominated the factors based on the content of the questions in each domain.
Results
KMO showed that 95% of the variance was caused by 5 underlying factors with an Eigen value larger than one: 15.31, 3.99, 2.69, 1.48, 1.38, respectively (Tables 1 and 2). Thus, in the first step of the study, we selected a five-factor solution for further analysis from the scale which consisted of 40 mixed items of positive and negative oriented leadership behaviors. Gradually, the questionnaire was streamlined and re-tested for validity. We decided to remove items with loading of less than 0.6 (1, 2, 3, 4, 5, 10, 11, 12, 13, 1518, 19, 24, 25, 26, 27, 28, 29, 33, 35.), and this resulted in the removal of one factor and a final version of 20-item questionnaire with a four- factors solution. Considering the varimax rotation analysis, factor 1 accounted for 20.07 % of the explained variance and was related to support for development; factor 2 explained 11.84% of the variance regarding integrity; factor 3 represented 11.77% of the explained variance and was related to sincerity; and finally, factor 4 accounted for 6.35% of the explained variance and was related to recognition. Table 1 demonstrates the load of each item on the four factors.
Table1 . Load of each item in the four factors (loading below 0.6 are not presented in the table). Variance, eigen values, and Cronbach’s alphas are also shown .
| Questions | Factors | |||
| 1 (20.07% of total variance) | 2 (11.84% of total variance) | 3 (11.77% of total variance) | 4 (6.35% of total variance) | |
| 1. He "needles" foremen under him for greater effort . | 0.79 | |||
| 2. He backs up the members in their actions. | 0.65 | |||
| 3. He is friendly and approachable. | 0.65 | |||
| 4. He makes group members feel at ease when talking with them. | 0.90 | |||
| 5. He tries to keep the foremen him in good standing with those in higher authority | 0.75 | |||
| 6. Expresses values that have an humanistic basis. | 0.85 | |||
| 7. Accepts responsibility for the operations–even in hard times. | 0.68 | |||
| 8. Encourages to develop my abilities | .64 | |||
| 9. Inspiration to think creativity | 0.61 | |||
| 10. Inspires me to try new working methods | 0.74 | |||
| 11. Looks for the mistakes. | 0.92 | |||
| 12. He encourages his junior officials immediately after they have accomplished their tasks successfully. | 0.66 | |||
| 13. He encourages his junior officials regularly after they have accomplished their tasks successfully. | 0.70 | |||
| 14. He formally encourages his junior officials in group meetings because of their proper performance | 0.60 | |||
| 15. Creates enthusiasm for a task. | 0.72 | |||
| 16. He emphasizes high morale among his underhand authorities. | 0.60 | |||
| 17. He gives appropriate feedback to subordinate regarding their individual and group performance | 0.67 | |||
| 18. Creates chummy, flexible and dynamic environment | 0.60 | |||
| 19. Mentioned his ideas and strategies for his followers | 0.68 | |||
| 20. He makes possibility for growing up and learning new skill among subordinates for achieving the organizational goals | 0.66 | |||
Table 2 . Factor Matrix for all questions of SLB questionnaire .
| Factor | |||||
| 1 | 2 | 3 | 4 | 5 | |
| SO1.1* ** | -.476 | .310 | -.417 | -.073 | -.178 |
| SO1.2 | -.012 | .514 | -0.95 | --.019 | -.329 |
| SO1.3 | -.573 | -.298 | .302 | .039 | -.025 |
| SO1.4 | .249 | -.147 | .539 | .095 | -.044 |
| SO1.5 | .106 | .320 | .370 | .195 | -.043 |
| SO1.6 | .206 | .789 | .207 | .157 | .013 |
| SO1.7 | .650 | .265 | .181 | .196 | .144 |
| SO1.8 | .380 | .295 | .648 | .126 | .219 |
| SO1.9 | .148 | .889 | -.032 | .009 | .008 |
| SO1.10 | .667 | .223 | .511 | .017 | .021 |
| SO1.11 | -.223 | -.117 | .299 | .184 | .253 |
| SO1.12 | .586 | -.319 | .320 | .028 | .052 |
| SO1.13 | -.379 | -.538 | .185 | .184 | .290 |
| SO1.14 | .260 | .752 | -.189 | .145 | .165 |
| SO1.15 | .510 | -.143 | .028 | -.123 | .049 |
| SO1.16 | .100 | .849 | -.062 | .006 | .086 |
| SO1.17 | .677 | -.281 | -.143 | -.085 | .099 |
| SO1.18 | .535 | .009 | .142 | -.151 | .076 |
| SO1.19 | .395 | .280 | .066 | -.013 | .031 |
| SO1.20 | .637 | -.152 | .023 | -.020 | .058 |
| SO1.21 | .791 | -.223 | .177 | -.074 | .103 |
| SO1.22 | .249 | .740 | .189 | .132 | .131 |
| SO1.23 | .267 | -.162 | .919 | -.004 | -.067 |
| SO1.24 | .140 | .280 | .455 | -.114 | -.441 |
| SO1.25 | .187 | -.044 | -.455 | -.114 | .441 |
| SO1.26 | .474 | .177 | -.238 | .104 | -.053 |
| SO1.27 | .382 | -.257 | .488 | -.325 | -.160 |
| SO1.28 | .310 | .111 | .224 | .159 | -.042 |
| SO1.29 | .526 | .013 | .206 | .286 | -.143 |
| SO1.30 | .478 | -.009 | -.226 | .658 | -.233 |
| SO1.31 | .369 | -.266 | -.131 | .685 | -.098 |
| SO1.32 | .528 | -.415 | -.156 | .559 | -.162 |
| SO1.33 | .526 | -.374 | -.145 | .542 | -.154 |
| SO1.34 | .723 | -.232 | -.324 | .004 | .100 |
| SO1.35 | -.312 | .103 | .189 | .288 | -.531 |
| SO1.36 | .599 | -.183 | -.299 | -.002 | -.060 |
| SO1.37 | .663 | -.205 | -.331 | -.053 | .113 |
| SO1.38 | .595 | -.137 | -.030 | -.128 | -.029 |
| SO1.39 | .677 | -.107 | -.269 | -.133 | .151 |
| SO1.40 | .662 | -.211 | -.082 | -.055 | .103 |
The reliability estimate measured as Cronbach’s alpha of the20-item questionnaire was 0.84. The Cronbach’s alpha for all factors were all above 0.6 except for Factor 3 which was 0.37.
Discussion
SLB style was in line with the fundamental socio- cognitive theory in learning; for instance, Bandura emphasized context, individual and personal behavior as the three important elements of this theory. The SL B is based on two out of the three issues of Bandura theory (individual and personal behavior). The psychometric findings of the instrument endorsed the usefulness of the scale.
The first factor analysis of the 40 SLB items was carried out and streamlined to a 20-item questionnaire. The items explained the leadership behaviors in four correlated factors as below:
1)Support for development
2)Integrity
3)Sincerity
4)Recognition
High-quality leadership relies on attitudinal qualities of a leader (22). Examples of highly significant leadership qualities are integrity, honesty, humility, courage, commitment, sincerity, passion, confidence, positivity, wisdom, determination, compassion and sensitivity which are in line with andrological learning theories in the socio- cognitive domain. Bandura (26) emphasized the importance of context (interpersonal and culture), behavior (developmental behavior) and individual (sincerity) effects on the learning process which is well adapted to the supportive leadership behavior model (27). Leaders with these types of behavioral qualities tend to attract followers (28). The four factors of SLB in our study could be considered in academic leadership as well as healthcare system. Moreover, the results of the application of this model could improve the performance of the followers and increase their loyalty to the system.
One of the strengths of this study was its appropriate theoretical frame work, selected based on social cognitive and ecological theories, which could be applied in managing health care organizations as well as educational institutions. Secondly, the large sample size in this study provided the necessary element for the standardization of the instrument. Moreover, the advanced construct validity of the instrument was underpinned by exploratory factor analysis.
Support for Development
The first factor solution is related to the notion of support for staff development by supervisors. Those qualities which contributed to the support of development in the followers' behavior are included staff changing, adapting and moving forward. The essential issues embedded in the factors of emotion, intrinsic elements of teamwork development, mutual support, innovative thinking and responsibility are in line with cognitive capability items (27).
Bass and colleagues emphasized the characteristics of rational leaders who want to develop subordinates’ capability to develop creativity and innovation (4, 5). Macgilton believes that supportive supervisors listen to their staff carefully in order to understand their views; they also seek the expressed needs of the staff and try to find their capabilities, and help them develop individual and social values (29). However, researchers argue that nursing supervisors do not believe in supportive leadership because of the rigidity defined by the professional status and the intrinsic differences among them and their followers (2, 30). Nursing leadership styles ought to be considered by health care organizations when establishing a positive organizational culture. Since their effect on subordinate personal development is still a subject of discussion, close attention to contextual factors is also a necessity for a successful staff development and self- efficacy.
Integrity
The second factor, integrity, supports interpersonal context, and it develops from trustworthiness, encouragement and good interpersonal communication skills, which could help the followers to achieve their goals and be more committed. Our findings are compatible with those reported in a qualitative study assessing the impact of supportive leadership in an Australian police work environment (2). SLB demonstrates the usefulness of integrity as a first step towards a climate change-process in an organization. These behaviors can increase consciousness and strengthen management practices based on the identification of individual and workplace issues. Involving subordinates in decision making, arranging counseling meetings, open-door policy and providing feedback are important workplace strategies that are emphasized in SLB practices. In other studies, integrity also underpins a "build up the good communication skill with staff" where supervisors play a role of coaching and mentoring. In a meta-analysis, the role of supervisors was studied with respect to organizational commitment and burnout (5, 31). Therefore, when intending to improve the quality of a healthcare or educational organization, it seems crucial to consider the integrity behaviors within a coaching role that a supervisor can play in decreasing burnout among staff (32).
Sincerity
The third factor is related to sincerity. Items in this factor show high loadings on demonstrating friendly and approachable behavior. In this case, supervisors do not actively look for followers’ mistakes but collaborate with them on a more personal level, fixing positive behavior which can lead to organizational change. Consistent to our findings, a qualitative study confirms our findings in which a supervisor stated: “You earn the person’s respect by giving them respect, and that goes a long way,” and “It doesn’t take any more time to treat staff with respect (33) if you want to achieve greater goals”. A friendly and sincere relationship between a leader and a subordinate is an important issue for achieving success in health care and academic organizations (34).
Recognition
The last factor which had the lowest variance was the supervisors’ recognition of the subordinates’ performance. In a study by Horn (35) on development of leadership, culture was considered to be an important factor. Culture provides a supportive environment in which everyone is recognized and appreciated. The leader may even play the role of “a parent” in the organization and try to meet the demands of the members and this leads to the feeling of comfort and security in the members. However, it is debatable whether or not this approach is beneficial for the development of organizations. On the other hand, in agreement with the concept of this factor “contingent reward”, a behavior emphasized by Boss and Atonakis, illustrates the transformational power which is achievable when the supervisors recognize and praise the followers’ good work (5, 32).
This is also in agreement with cultural and contextual issues which directly affect the followers’ performance; and in an academic leadership, it will affect the learners’ situation and improve their self-efficacy and will also help them to promote their capability (31, 36).
Conclusion
The use of supportive leadership behaviors grows in importance when successful improvement of health organizations and academic leadership is desired. Mapping the SLB can prove beneficial for sustainment when organizational changes are initiated. The significant factors of supportive leadership behavior are support for followers’ development, integrity, sincerity and recognition. SLB builds up a dynamic supportive model, consisting of “integrity" and "recognition" which affect contextual level, "sincerity" which works on the personal level and "support for development" which affects behavior. Our results seem promising with respect to the development of an instrument as a valid and reliable measure of SLB capacity based on socio- cognitive theories and with respect to its application in the Iranian context and perhaps other contexts.
Acknowledgements
The authors wish to thank Christer Sandhal for his help in designing the study.
Conflict of interest
No conflict of interest has been declared by the authors.
Cite this article as: Shirazi M, Emami A.H, Mirmoosavi S.J, Alavinia S.M, Zamanian H, Fathollahbeigi F, Masiello I. Contextualization and standardization of the supportive leader-ship behavior questionnaire based on socio- cognitive theory in Iran. Med J Islam Repub Iran 2014 (8 November). Vol. 28:125.
References
- 1. Bass BM, Riggo RE. Transformational Leadership. 2nd Ed. New Jersey: Lawrence Erlbaum Associates; 2006.
- 2.Muller J, Maclean R, Biggs H. The impact of a supportive leadership program in a policing organisation from the participants' perspective. Work. 2009;32(1):69–79. doi: 10.3233/WOR-2009-0817. [DOI] [PubMed] [Google Scholar]
- 3.Jolson MA, Alan J, Dubinsky FJ, Yammarino Yammarino, Lucette B, Comer Comer. Transforming the Sales Force with Leadership. Sloan Management Review. 1993;spring:95–106. [Google Scholar]
- 4.Bass BM, Avolio BJ. Transformational Leadership and Organizational Culture. Public Administration Quarterly. 1993;17(1):112–21. [Google Scholar]
- 5. Bass B M, Bass R R. The Bass handbook of leadership: theory, research, and managerial applications. New York: Free Press; 2008.
- 6. The Loyalty Research Center, In Leatherman RW. Quality Leadership Skills: Standards of Leadership Behavior. Massachusetts: HRD Press; 1990.
- 7.Munir F, Nielsen K, Garde AH, Albertsen K, Carneiro IG. Mediating the effects of work-life conflict between transformational leadership and health-care workers' job satisfaction and psychological wellbeing. J Nurs Manag. 2012;20(4):512–21. doi: 10.1111/j.1365-2834.2011.01308.x. [DOI] [PubMed] [Google Scholar]
- 8.Abualrub RF, Alghamdi MG. The impact of leadership styles on nurses' satisfaction and intention to stay among Saudi nurses. J Nurs Manag. 2012;20(5):668–78. doi: 10.1111/j.1365-2834.2011.01320.x. [DOI] [PubMed] [Google Scholar]
- 9.Casida J, Parker J. Staff nurse perceptions of nurse manager leadership styles and outcomes. J Nurs Manag. 2011;19(4):478–86. doi: 10.1111/j.1365-2834.2011.01252.x. [DOI] [PubMed] [Google Scholar]
- 10.Leatherman RW. Quality Leadership Skills: Standards of Leadership Behavior Massachusetts: HRD Press. 2008 [Google Scholar]
- 11.Anderson RA, Corazzini KN, McDaniel RR. Complexity Science and the Dynamics of Climate and Communication: Reducing Nursing Home Turnover. Gerontologist. 2004;44(3):378–88. doi: 10.1093/geront/44.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thyer GL. Dare to be different: transformational leadership may hold the key to reducing the nursing shortage. J Nurs Manag . 2003 Mar;11(2):73–9. doi: 10.1046/j.1365-2834.2002.00370.x. [DOI] [PubMed] [Google Scholar]
- 13.Murphy L. Transformational leadership: a cascading chain reaction. J Nurs Manag. 2005;13(2):128–36. doi: 10.1111/j.1365-2934.2005.00458.x. [DOI] [PubMed] [Google Scholar]
- 14.Steinert Y, Naismith L, Mann K. Faculty development initiatives designed to promote leadership in medical educationA BEME systematic review: BEME Guide No19. Med Teach. 2012;34(6):483–503. doi: 10.3109/0142159X.2012.680937. [DOI] [PubMed] [Google Scholar]
- 15.Haan CK, Zenni EA, West DT, Genuardi FJ. Graduate medical education leadership development curriculum for program directors. J Grad Med Educ. 2011;3(2):232–5. doi: 10.4300/JGME-D-10-00180.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Edler A, Adamshick M, Fanning R, Piro N. Leadership lessons from military education for postgraduate medical curricular improvement. Clin Teach. 2010;7(1):26–31. doi: 10.1111/j.1743-498X.2009.00336.x. [DOI] [PubMed] [Google Scholar]
- 17.Frugé E, Mahoney DH, Poplack DG, Horowitz ME. Leadership: "They never taught me this in medical school". J PediatrHematolOncol. 2010;32(4):304–8. doi: 10.1097/MPH.0b013e3181cf4594. [DOI] [PubMed] [Google Scholar]
- 18.Malling B, Mortensen L, Bonderup T, Scherpbier A, Ringsted C. Combining a leadership course and multi-source feedback has no effect on leadership skills of leaders in postgraduate medical educationAn intervention study with a control group. BMC Med Educ. 2009;10(9):72. doi: 10.1186/1472-6920-9-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Varkey P, Peloquin J, Reed D, Lindor K, Harris I. Leadership curriculum in undergraduate medical education: a study of student and faculty perspectives. Med Teach. 2009;31(3):244–50. doi: 10.1080/01421590802144278. [DOI] [PubMed] [Google Scholar]
- 20.Hassanian M. Leadership Style of the Heads of the Departments in Hamadan. IJME. 2004;12(4):108–12. [Google Scholar]
- 21.Yang C, Wang Y, Chang S, Guo S, Huang M. A Study on the Leadership Behavior, Safety Culture, and Safety Performance of the Healthcare Industry. World Academy of Science, Engineering and Technology. 2009;53:1148–55. [Google Scholar]
- 22.Ferile E, Shortell S. Improving the Quality of Health Care in the United Kingdom and the United StatesA Framework for Change. Milbank Quarterly. 2001;79(2):281–315. doi: 10.1111/1468-0009.00206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larsson G. The Developmental Leadership Questionnaire (DLQ): Some psychometric properties. Scandinavian Journal of Psychology. 2006;47:253–62. doi: 10.1111/j.1467-9450.2006.00515.x. [DOI] [PubMed] [Google Scholar]
- 24.Hersey p, Blanchard KH. Situational Leadership, Perception, and the Impact of Power. Group Organization Management. 1979;vol. 4(4):418–28. [Google Scholar]
- 25. Halpin AW. LEADER BEHAVIOR DESCRIPTION QUESTIONNAIRE. Columbus, OH The Ohio State University. 1962.
- 26. Bandura, A., Self‐efficacy1994: Wiley Online Library.
- 27. Rimer, B.K. and K. Glanz, Theory at a glance: A guide for health promotion practice2005: US Department of Health and Human Services, National Institutes of Health, And National Cancer Institute.
- 28. Hersey P, Blanchard KH, Johnson DE. Management of Organizational Behavior: Leading Human Resources. Ninth Ed. New Jersey: Prentice Hall; 2008.
- 29.McGilton KS, Hall LM, Wodchis WP, Petroz U. Supervisory support, job stress, and job satisfaction among long-term care nursing staff. J Nurs Adm. 2007;37(7-8):366–72. doi: 10.1097/01.nna.0000285115.60689.4b. [DOI] [PubMed] [Google Scholar]
- 30. Foner N. The caregiving dilemma: Work in an American nursing home. Berkeley: University of California Press; 1994.
- 31.Leiter M, Maslach CH. The impact of Interpersonal environment on burnout and organizational commitment. Journal of Organizational Behavior. 1988;9:297–308. [Google Scholar]
- 32.Antonakis J. The validity of the transformational, transactional, and laissez-faire leadership model as measured by the Multifactor Leadership Questionnaire (MLQ5X) Dissertation Abstracts International. 2001;62(01):233–91. [Google Scholar]
- 33.Smith RG. Leadership Development. Journal of Trauma Nursing. 2006;13(3):122–5. doi: 10.1097/00043860-200607000-00010. [DOI] [PubMed] [Google Scholar]
- 34. Scott, G., H. Coates, and M. Anderson, Academic Leadership Capabilities for Australian Higher Education. 2008.
- 35.Horn SD. RN staffing and long-term care. American Journal of Nursing. 2006;106(3):15–6. doi: 10.1097/00000446-200603000-00005. [DOI] [PubMed] [Google Scholar]
- 36. Glanz, K. and B.K. Rimer, Theory at a glance: A guide for health promotion practice, 1997, US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute.


