Abstract
Background: Pigmented villonodular synovitis (PVNS) is characterized by the presence of inflammation and hemosiderin deposition in the synovium. Two forms of PVNS distinguished in the literature are diffused and localized involvements. There are controversies in the literature about the surgical management of PVNS. We report our experience in the management of knee PVNS at a mean follow-up of 4 years. We also introduce our preferred method of treatment for these patients.
Methods: A number of 26 patients (26 knees) with histologically proven PVNS of the knee in the pathology department at Shafa Yahyaeyan hospital were identified between January 1996 and February 2012. Annual clinical follow-up was conducted in all patients and a follow-up MRI scans was ordered for symptomatic cases. All patients were examined according to the Knee Society Score (KSS) in which the knees were graded from excellent to poor.
Results: Mean age of the patients was 28.08±12.5. A number of 15 patients (58%) had diffused involvement of the knee joint and 11 (42%) had a localized form of involvement. Mean follow up was 4 years. The mean duration of symptoms prior to presentation was 44.40±38.69 months. In five cases (23%) subtotal synovectomy and in 21 cases (77%) total synovectomy was performed. Two cases (7.7%) had recurrence. In a comparison between new methods vs. routine methods, after adjusting the pre-operation KSS scores, there was a significant difference between both methods in their post-op results. There were no complications in the form of knee instability, infection or neurovascular injury.
Conclusion: The PVNS of knee joint; especially the diffused form should be carefully observed and managed using appropriate investigations. Staged open total synovectomy with a posterior and then an anterior approach seems to be a superior method for surgical treatment of diffused forms.
Keywords: Knee joint, Pigmented Villonodular Synovitis, Synovectomy, Recurrence
Introduction
Pigmented villonodular synovitis (PVNS) is a condition of the synovial membrane that is characterized by the presence of inflammation and hemosiderin deposition in the synovium. The PVNS was introduced in1852 as a neoplastic process (1) because of its unrelenting growth pattern, capacity to erode surrounding bone and joint tissue, and high recurrence rate after resection. In 1941, however, Jaffe et al (2) presented the pathologic entity as a synovitis, thereby shifting the focus from a neoplastic process to an inflammatory one. The incidence of PVNS is 1.8 patients per million, equally affecting both genders in third and fourth decades of life.
Two forms of PVNS that are distinguished in the literature are diffuse (DPVNS) and localized (LPVNS) types (3,4). The localized form principally affects those between 30 and 50 years of age with a female predominance. The diffused type is a rare, usually benign proliferative lesion that develops in the synovium with an incidence of two per million people annually, in patients < 40 years, with an equal distribution. The knee is the most commonly occurring site (5).Although considered to be a benign lesion; the diffuse form is more aggressive, with a high recurrence rate after surgery (25% intra articular and 25% to 50% extra articular disease) (6).
There are controversies in the literature on surgical management of the PVNS between arthroscopic (7,8) and traditional open synovectomy (9,10). Management options for PVNS include radiation induced, arthroscopic, and open synovectomy. There is no method of choice in treatment of diffused forms
We report our experience in the management of knee PVNS at a mean follow up of 4 years in ShafaYahyaeyan Hospital. We also introduce our preferred method (staged method) in the treatment of diffused forms.
Methods
Between January1996 and February 2012, 26 patients (26 knees) with histologically proven PVNS of the knee were enrolled from the Shafa Yahyaeyan Hospital. Informed consent was obtained from all included patients.
Both localized and diffused forms were included in this series. The follow-up was calculated from the date of surgery to the last follow-up entry in the records. Postoperative complications, recurrence and treatment details were recorded. Anteroposterior and lateral radiographs of the knee were performed to exclude other pathologies and for evidence of osteoarthritis. Aspiration cytology was carried out in patients who presented with a true haemarthrosis.
In all cases, a MRI scan was ordered for better evaluation (Fig. 1). Biopsy was carried out in 15patients. For other 11 patients whom their MRI evaluation was completely diagnostic, biopsy was sent in the same operation. Synovial specimen was sent for histological examination. Annual clinical follow-up was continued in all patients at least for 2 years. A follow-up MRI scans was ordered for symptomatic cases. All knees were examined according to the KSS score before and after surgery, graded from excellent to poor.
Fig. 1 .
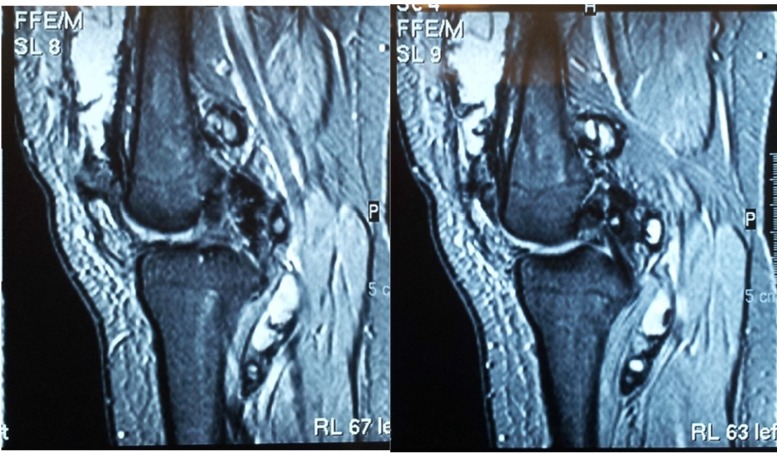
Diffused form of PVNS
Our surgical method of choice: In this method we first approached posteriorly in prone position with lazy- S skin incision. After isolation of neurovascular bundle two heads of gastrochenemious were detached and posterior transverse capsulotomy was performed (Fig. 2). After complete excision of the tumor body, capsule was repaired and both heads of the gastrochenemious were reattached to their remnants. Then patients underwent aggressive physiotherapy for regaining range of motion using a continuous passive motion (CPM) machine. After achieving the complete range of motion, the second staged anterior approach was performed with standard anteromedial knee arthrotomy. This method seems to be effective because all patients regained complete range of motion in a few days and no patient needed further knee manipulation. Also, KSS score was increased significantly in these patients. It seems that for open approach in diffused type at first posterior approach then anterior approach is a superior method. In posterior approach the surgeons must consider that this is the first and last operation of the patient and all tumor body have to be resected.
Fig. 2 .

Posterior transverse capsulotomy
Data were reported as mean SD and frequency and relative frequency. The paired test were used to compare before and after differences. ANCOVA test also used for multivariate analysis. A p value of less than 0.05 was considered statistically significant. SPSS version 13 was used for statistical analysis.
Results
A total of 26 patients were enrolled with histologically proven PVNS in this study. About 69% (18 cases) were female and 31% (8 cases) male. The presence of locking or pseudo locking was the predominant mode of manifestation in the localized disease, whereas recurrent joint effusion and spontaneous onset mild pain of chronic duration was the common presenting symptom in all diffused varieties.
Mean (±SD) age was 28.2±12.37 (range, 13-67 years). About 58% (15 cases) had diffused involvement of the knee joint and 42% (11 cases) had a localized form of involvement. In the localized form one patient had posterior involvement and 10 patients had anterior involvement. Mean (±SD) follow-up was 4.6±3.24 years (range 2-17 years). The mean (±SD) duration of symptoms prior to presentation was 30.3±25.19 months (range 6–96 months). Sixteen cases (61.5%) were left-sided and 10 cases (38.5%) were right-sided. Anteroposterior and lateral radiographs of the knee revealed normal findings in 24 patients (92.3%) and 2 (7%) with features of osteoarthritis in the knee. Obtained MRI scan revealed the extent of involvement with classic low intensity signals in both T1- and T2-weighted images Aspiration cytology was performed in four patients and all showed hemosiderin containing macrophages. Biopsy (arthroscopically, incisional, excisional) was carried out for histological confirmation in 15 patients (57.7%). In the rest 11 patients (42.3%) biopsy was not performed before surgery due to the diagnostic findings in the MRI and arthroscopy.
Histological appearance was largely similar in both localized and diffused forms. Proliferating polyhedral, mononuclear, synovial cells are the most important, predominant lesion-defining cells in PVNS. Presence of both intracellular and extracellular hemosiderin deposits is quite characteristic of PVNS. Foamy histiocytes, mononuclear cells, giant cells and chronic inflammatory infiltrate (CINF) were the remaining cellular population.
From 5 cases (23%) with diffused involvement, due to the intact posterior capsule and also largely upon the surgeon's preference, 4 cases underwent subtotal synovectomy with anterior arthrotomy and synovectomy, and arthroscopic subtotal anterior synovectomy was performed in one case. These patients were non-symptomatic and there was no need for another operation in their follow-up. In 21 cases (77%) total synovectomy was performed. Two cases had full arthroscopic anterior and posterior synovectomy, 2 cases had anterior arthroscopic surgery, 1 case had posterior arthroscopic surgery, 6 cases had staged posterior then anterior open synovectomy, 8 cases anterior open synovectomy, 1 case had full arthroscopic anterior and then posterior open synovectomy and 1 case had first anterior then posterior open synovectomy.
Recurrence was identified clinically by pain and swelling and confirmed histologically.
Two patients (7.7%) had recurrence of PVNS. One case had full anterior arthroscopic and then posterior open synovectomy in her follow-up; recurrence was identified and she underwent total synovectomy. Another case had full arthroscopic anterior and posterior synovectomy and again in her follow-up had a recurrence of the tumor and underwent open total synovectomy. Four patients with a history of arthrofibrosis following anterior open synovectomy required manipulation under anesthesia with subsequent improvement of range of motion in two of them.
There were no complications in the form of knee instability, infection or neurovascular injury. Two patients showed moderate to severe osteoarthritis before and in their follow-up radiographs, one of which underwent total knee arthroplasty, while the other patient was adequately coping with her symptoms on her last follow-up. All data are shown in Table 1 and 2.
Table 1 . Descriptive statistics of the studied variables .
| Variable | Mean | SD | Min | Max |
| Age (years) | 28.2 | 12.37 | 13 | 67 |
| Duration of symptom per month | 30.3 | 25.19 | 6 | 96 |
| Pre-operation KSS | 63.1 | 6.68 | 47 | 73 |
| Post operation KSS | 77.8 | 9.29 | 54 | 91 |
| Follow up duration per year | 4.6 | 3.24 | 2 | 17 |
Table 2 . Frequency distribution of the studied variables .
| Variable | n | % | |
| Sex | Male | 8 | 30.8 |
| Female | 18 | 69.2 | |
| Biopsy status | Positive | 15 | 57.7 |
| Negative | 11 | 42.3 | |
| Tumor Type | Diffused | 15 | 57.7 |
| Localized | 11 | 42.3 | |
| Complication/ Second Surgery | Positive | 8 | 30.8 |
| Negative | 18 | 69.2 |
The mean (±SD) of pre- and post-operative KSS were 63.1± 6.68 and 77.8± 9.29, respectively. This difference was significant (p<0.009). The KSS scores before and after surgery in patients who underwent staged posterior and then anterior approaches were 62/66±4/45 and 83/33±6/34: in which the difference was significant. In a comparison between new vs. routine methods, the adjusted pre operation KSS score (ANCOVA) showed a significant difference (Fig. 3).
Fig. 3 .
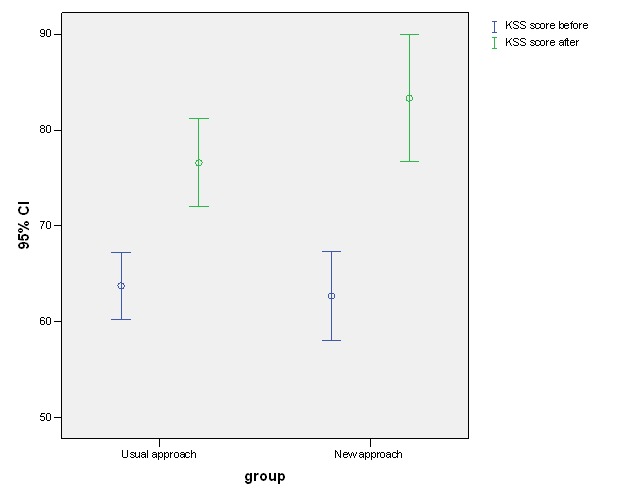
KSS score difference between usual approach and our new technique
Discussion
Diagnostic dilemma can occur in PVNS, not only at the clinical and radiological levels, but also while choosing the best treatment. Our experience with treatment of knee PVNS with a mean follow up of 4 years supports the proponents of an aggressive surgical treatment.
Our cases had a mean age of 27 years and a female preponderance (18F: 8M). This was non comparable to the literature which described PVNS as most commonly affecting adult patients in their third or fourth decades of life, and occurring with equal sex distribution (1,3-5,11).There is no documented study in Iran showing predominant sex in PVNS, but in our study females are predominant, which may be due to genetic bases of Iranian population (Table 1).
Although there are several hypotheses for the PVNS, but the etiopathogenesis still remains unclear. Some more important ones are, for example, inflammatory synovial hyperplasia, benign neoplasm of unknown etiology, abnormality of local lipid metabolism, repetitive trauma and hemorrhage. The main etiology of PVNS has been proposed to be precipitated by trauma, proposing a hyper vascular cellular phase subsequent to trauma produced by hyalinization and fibrosis (1-5)
Previous history of trauma to the affected region can be found in approximately 50% of patients. In our study 15 cases (58%) recalled trauma which is comparable to other studies. We believe that these patients probably thought of the trauma as a possible reason for the disease or their deterioration. Recurrent joint effusion, spontaneous onset mild pain and synovial swelling were the common presenting symptoms in all diffused varieties in our series.
This entity has been classified into three categories on the basis of clinical presentation: (a) isolated, discrete lesion occurring within a tendon sheath, most often seen in the hand, (b) localized pigmented villonodular synovitis (LPVS), occurring most commonly in the knee and presenting most commonly with mechanical symptoms, and (c) generalized pigmented villonodular synovitis (DPVS), presenting with chronic pain and edema, most commonly in the knee, hip and ankle (12).
In our study, 11 patients (42%) were diagnosed with localized forms (3 patients were treated arthroscopically and 8 patients had open synovectomy). In the remaining 15 cases (58%), the diffused form of the disease was noted and 5 cases had subtotal synovectomy. In these cases only anterior open subtotal synovectomy was performed in 4 cases and one underwent arthroscopic subtotal synovectomy (Table 1, case 20). In these cases, because the intact posterior capsule and surgeon’s preference, posterior part of the synovium remained intact. In their follow-ups no symptoms were found and no one underwent any more surgery. For the other 10 cases, total synovectomy (2 arthroscopy cases, 7 open staged arthrotomy cases and one case had full anterior arthroscopic and then posterior open synovectomy) was performed.
Surgical treatment of knee PVNS is controversial. Total synovectomy, open or arthroscopic, for the diffused form (recurrence common), local excision for the nodular form (recurrence rare) and radiotherapy in the management of recurrent and residual lesions have been described with varying success in the literature (1,3-5,7).
In this study for the 3 localized forms of PVNS (two in anterior part, one in posterior part) arthroscopic total synovectomy was performed and no recurrence was found after operation in their follow-ups (Table 1,case 12,13,14). These patients had full knee range of motion and their KSS score increased significantly.
In contrast, four patients with a localized form of the disease, experienced significant decrease in range of motion when anterior open synovectomy was performed and they had undergone knee manipulation during their follow-up and unfortunately only two of them improved afterwards. There is a significant incidence of loss of range of motion with pain after an open synovectomy operation, primarily associated with a para patellar incision (7). In a clinical outcome of the patients reported by Chiari, C. et.al, (1), 8 cases required manipulation under anesthesia due to loss of motion after open synovectomy, and in our study, only 4 patients with the localized form of the disease who underwent anterior medial para patellar approach had significant loss of range of motion, but unfortunately only two of them had improvement in range of motion with manipulation under anesthesia (Table 1,case 9,11).
In the diffused form (a total of 15 patients), 10 patients underwent total synovectomy in which 6 of them had staged posterior and then anterior total synovectomy (Table 1,case 12-14,23-25).
In these 6 patients the KSS score increased significantly and since there was no damage to the extensor mechanism, patients’ range of motion was fully intact in the final assessment. After first stage posterior approach, physical therapy was given and after regaining full range of motion the second stage anterior approach was performed. As it is shown in Figure 3, the post-op score between this group and those who received a routine approach had a significant difference, implying that this approach has better results.
Only in two patients with diffused form an arthroscopic total synovectomy with anterolateral, anteromedial and posteromedial portal was performed (Table 1,case 4,18). One patient had an improvement of signs and no recurrence was found after one year follow-up (Table 1, case 18). But in another patient’s follow-up, the tumor had recurred and she underwent open total synovectomy (Table 1 case 4). It seems that arthroscopic surgery for diffused forms should be used cautiously.
In majority of cases, plain radiographs were normal, although, bone erosions were present in 33% to 56% of diffused PVNS (9,11,13). Our study had two patients with the diffused PVNS, with moderate to severe osteoarthritis and finally one of them underwent total knee arthroplasty during her follow-up (Table 1,case 16).
The appearance of PVNS in MRI imaging consists of multiple synovial lesions with low or intermediate signal intensity on T1-weighted images, low signal intensity on T2-weighted images and gradient-echo images (4,14). Also all patients in our study had this diagnostic finding in their MRI. Because of the diagnostic findings in the MRI and arthroscopy, biopsy was not performed in 11 patients (out of 26) before surgery. All patients had histological confirmation after operation.
Classic microscopic findings included: all-important lesion-defining proliferating polyhedral, mononuclear synovial cells, hemosiderin deposits both intracellular and extracellular, foamy histiocytes or mononuclear cells and giant cells (3,4,11).
The recurrence rates for diffused forms of PVNS vary greatly from 5% to 35% in literature (1,6). Arthroscopic treatment most likely results in recurrence of the lesions and a high recurrence rate is associated with diffused lesions (15).Two cases (7%) of this study had recurrence of PVNS (Table 1,case 1,4) which is comparable to other studies. These patients had a diffused form of PVNS and one of them underwent arthroscopic resection in the anterior part and open resection in the posterior part. Another one of the patients had full arthroscopic resection of the tumor.
Radiation therapy was not used in our patients as we had concerns regarding radiation-induced sarcomas in young patients; nevertheless, some research studies have found it useful for residual, recurrent and large primary lesions (7,16,17).
Conclusion
This study showed that PVNS of the knee joint especially the diffused form should be carefully observed and managed by appropriate investigations and satisfactory treatment planning to obtain optimal outcome. Staged open total synovectomy with initial posterior approach and then, after regaining full range of motion, the anterior approach, is our treatment of choice for diffused forms due to its good results. The anterior localized form can be dealt with arthroscopic total synovectomy with good results.
Conflicts of interest
Iran University of Medical Sciences supported this study and researchers have no conflict of interest.
Cite this article as: Jabalameli M, Jamshidi Kh, Radi M, Hadi H, Bagherifard A. Surgical outcomes of 26 patients with pigmented villonodular synovitis (PVNS) of the knee at a mean follow-up of 4 years: introducing a novel technique. Med J Islam Repub Iran 2014 (29 October). Vol. 28:123.
References
- 1.Chiari C, Pirich C, Brannath W, Kotz R, Trieb K. What affects the recurrence and clinical outcome of pigmented villonodular synovitis? Clin Orthop Relat Res. 2006;450:172–178. doi: 10.1097/01.blo.0000224051.01873.fb. [DOI] [PubMed] [Google Scholar]
- 2.Dines JS, DeBerardino TM, Wells JL. et al. Long-term follow-up of surgically treated localized pigmented villonodular synovitis of the knee. Arthroscopy. 2007;23:930–937. doi: 10.1016/j.arthro.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 3.Sharma H, Rana B, Mahendra A, Jane MJ, Reid R. Outcome of 17 pigmented villonodular synovitis (PVNS) of the knee at 6 years mean follow-up. Knee. 2007;14:390–394. doi: 10.1016/j.knee.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 4.Sharma V, Cheng E. Outcomes after excision of pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 2009;467:2852–2858. doi: 10.1007/s11999-009-0922-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akinci O, Akalin Y, Incesu M, Eren A. Long-term results of surgical treatment of pigmented villonodular synovitis of the knee. Acta Orthop Traumatol Turc. 2011;45:149–155. doi: 10.3944/AOTT.2011.2442. [DOI] [PubMed] [Google Scholar]
- 6.Rauh PB, Bernard J, Craig DM. Pigmented villonodular synovitis of the knee: Average five-year follow-up of arthroscopic treatment. J South Orthop Assoc. 2002;11:88–92. [PubMed] [Google Scholar]
- 7.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2003;19:602–607. doi: 10.1016/s0749-8063(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 8.Blanco CE, Leon HO, Guthrie TB. Combined partial arthroscopic synovectomy and radiation therapy for diffuse pigmented villonodular synovitis of the knee. Arthroscopy. 2001;17(5):527–31. doi: 10.1053/jars.2001.24068. [DOI] [PubMed] [Google Scholar]
- 9.Martin RC, Osborne DL, Edwards MJ, Wrightson W, McMasters KM. Giant cell tumor of tendon sheath, tenosynovial giant cell tumor, and pigmented villonodular synovitis: Defining the presentation, surgical therapy and recurrence. Oncol Rep. 2000;7:413–419. [PubMed] [Google Scholar]
- 10.Shabat S, Kollender Y, Merimsky O, Isakov J, Flusser G, Nyska M. et al. The use of surgery and yttrium 90 in the management of extensive and diffuse pigmented villonodular synovitis of large joints. Rheumatology (Oxford) 2002;41(10):1113–8. doi: 10.1093/rheumatology/41.10.1113. [DOI] [PubMed] [Google Scholar]
- 11.Ottaviani S, Ayral X, Dougados M, Gossec L. Pigmented villonodular synovitis: A retrospective single-center study of 122 cases and review of the literature. Semin Arthritis Rheum. 2011;40:539–546. doi: 10.1016/j.semarthrit.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 12.Rhee PC, Sassoon AA, Sayeed SA, Stuart MS, Dahm DL. Arthroscopic treatment of localized pigmented villonodular synovitis: Long-term functional results. Am J Orthop. 2010;39:E90–E94. [PubMed] [Google Scholar]
- 13.Muscolo DL, Makino A, Costa-Paz M, Ayerza M. Magnetic resonance imaging evaluation and arthroscopic resection of localized pigmented villonodular synovitis of the knee. Orthopedics. 2000;23:367–369. doi: 10.3928/0147-7447-20000401-18. [DOI] [PubMed] [Google Scholar]
- 14.Cheng XG, You YH, Liu W, Zhao T, Qu H. MRI features of pigmented villonodular synovitis (PVNS) Clin Rheumatol. 2004;23(1):31–4. doi: 10.1007/s10067-003-0827-x. [DOI] [PubMed] [Google Scholar]
- 15.Akinci O, Akalin Y, Kayali C. Results of total knee arthroplasty in patients with gonarthrosis resulting from the delayed diagnosis of PVNS: A case series. Eur J Orthop Surg Traumatol. 2012;22:51–56. [Google Scholar]
- 16.Ward WGSr, Boles CA, Ball JD, Cline MT. Diffuse pigmented villonodular synovitis. Clin Orthop Relat Res. 2007;454:186–191. doi: 10.1097/01.blo.0000229345.57092.a2. [DOI] [PubMed] [Google Scholar]
- 17.Berger B, Ganswindt U, Bamberg M, Hehr T. External beam radiotherapy as postoperative treatment of diffuse pigmented villonodular synovitis. Int J Radiat Oncol Biol Phys. 2007;67:1130–1134. doi: 10.1016/j.ijrobp.2006.10.016. [DOI] [PubMed] [Google Scholar]


