Abstract
Multiple idiopathic external apical root resorption (MIEARR) is a relatively rare condition affecting multiple teeth in a dentition. As the condition is nonsymptomatic, a case is usually detected as an incidental radiographic finding. However, it may cause pain and mobility in severe cases. It is sometimes self-limiting or sometimes may progress to tooth loss. This paper presents a case of external apical root resorption involving multiple teeth in which etiology was not identified, so idiopathic root resorption was considered as a diagnosis of exclusion.
Keywords: Apical, idiopathic, root resorption
INTRODUCTION
Deciduous teeth are exfoliated as a result of root resorption. This is a physiological process and thought to arise from the pressure of erupting teeth. In contrast, root resorption in permanent teeth is infrequent and pathological. Pathological root resorption is related to several local and systemic factors.
By definition, if an etiological factor cannot be identified for root resorption, the term “idiopathic” is applied. Two types of idiopathic root resorption have been observed; namely, apical and cervical. Cervical root resorption starts in the cervical area of the teeth and progresses toward the pulp. In the apical type, the resorption starts apically and progresses coronally causing a gradual shortening and rounding of the remaining root. Patients with idiopathic root resorption are commonly asymptomatic[1] clinically with an occasional complaint of tooth mobility, so the condition is usually found in routine radiographic examination.
CASE REPORT
A 22-year-old male patient came to the department of conservative dentistry and endodontics with the chief complains of decayed teeth. On clinical examination, the patient had multiple minimally carious dentition except mandibular left first molar which was grossly carious and pulpally involved. A panoramic radiograph revealed evidence of generalized root resorption [Figure 1]:
Figure 1.

OPG revealing apical root resorption involving multiple teeth in maxillary and mandibular arch, OPG = Orthopantomogram
Moderate to severe apical root resorption affecting all maxillary and mandibular posterior teeth was present [Figure 2a and b].
The severity of the resorption was more in posterior teeth.
Maxillary second molar teeth (17, 27) appeared to be the most severely affected, with almost complete loss of the distobuccal root.
Roots of maxillary first molars were considerably resorbed.
There was also evidence of apical root resorption of the mandibular molars bilaterally and blunting of all the mandibular premolar roots [Figure 2c and d].
Resorption pattern was bilaterally symmetrical.
Figure 2.
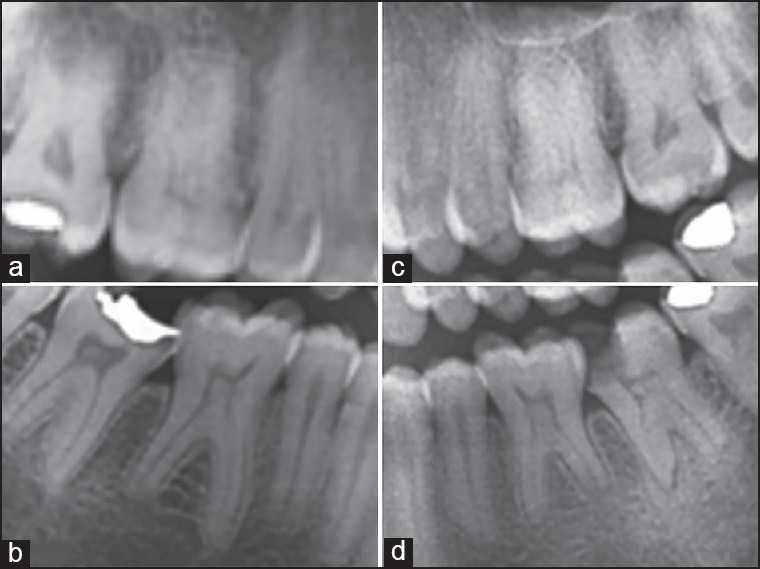
(a) Radiograph revealing resorption of 16 and 17. (b) Radiograph revealing resorption of 46 and 47. (c) Radiograph revealing resorption of 26 and 27. (d) Radiograph revealing resorption of 36 and 37
Electric pulp testing indicated that all teeth with resorbed roots except mandibular left first molar were vital. There was no history of trauma. His past medical and family histories were unremarkable. Hematological and biochemical screening was within the normal range. A diagnosis of multiple idiopathic external apical root resorption (MIEARR) was made radiographically. Root canal therapy was done for mandibular left first molar. Patient was kept on follow-up for future outcome of resorbed teeth.
DISCUSSION
External root resorption of the permanent dentition is a condition which is sometimes diagnosed from routine dental examinations. There are multiple causes mentioned in the literature for root resorption including trauma, periapical inflammation, reimplantation of avulsed teeth, tumors, cysts, and tooth impactions.[2] Factors contributing multiple external root resorption may include endocrine imbalances such as hypophosphatasia, hyperparathyroidism, and hypothyroidism; although some of these have come under question.[3] Orthodontic movement is also a causative factor and perhaps accounts for the greatest number of cases.[4] External root resorption which develops in the absence of a plausible cause is termed idiopathic.
Literature search for MIEARR identified few published case reports describing only numerated case;[5,6,7,8,9] to which we have added one more case, presented in this article. These cases indicate that MIEARR affects a wide age range of patients, from 14 to 39 years. In contrast to multiple idiopathic external cervical root resorption (MIECRR), males appear to be more frequently affected by MIEARR than females, with a male: female ratio of 11:4. In addition, MIEARR appears to have a predilection for premolar and molar regions.
Common features of the MIEARR cases are:[5]
Normal clinically appearing teeth and periodontal tissues.
Root resorption may be associated with vital teeth or endodontically treated teeth.
No periodontal and periradicular inflammation present.
Alveolar bone levels may be within normal limits.
Absence of any local etiological factors.
Patients are asymptomatic until very late in the pathological process where increased tooth mobility has occurred.
Generally found as an incidental finding on radiographs.
Bilaterally symmetrical pattern of root resorption.
Histological examination of any soft tissue or bone removed reveals chronic nonspecific inflammation and other laboratory test results indicate no significant abnormalities.[10]
In an attempt to explain the etiology, Stafne and Slocumb[11] in a study of root resorption cases failed to find any definite associations with systemic disease. In contrast, Gunraj[12] has suggested that changes in the host cellular immune system may be implicated. Activation of interlukin (IL)-IB plays an important role in resorption of tooth and the bone. Al-Qawasmi et al.,[13] suggested that polymorphisms in IL-1 gene are involved in root resorption pathogenesis. Urban et al.,[14] demonstrated that IL-1 gene polymorphism presents a significantly higher risk for development of pathological root resorptions. Linares et al.,[15] also suggested that variations in not only the IL-IB gene, but also the IL-1 receptor antagonist gene (rs419598) are determinants of a predisposition to external apical root resorption.
Pinska and Jarzynka[16] first suggested genetic susceptibility in their report of a family with generalized root resorption. Newman[3] then followed this study and a tentative genetic association was found. Six families displayed an autosomal dominant inheritance pattern, three families an autosomal recessive pattern, while three individuals displayed a spontaneous phenotype. Newman failed to find a distinct mode of inheritance, stating that autosomal dominant, autosomal recessive, and polygenic modes of inheritance were all possible in external root resorption. The most compelling evidence for a genetic association with MIEARR came from Saravia and Meyer.[17] The authors described 14-year-old monozygotic twins, presented with identical clinical and radiographic patterns of MIEARR. In the present case, patient recalled no history of early tooth loss in parents, grandparents, or siblings.
With no absolute etiological factors identified, treatment of MIEARR depends largely on the presenting symptoms and the extent and severity of root resorption. The usual treatment is the extraction of teeth of poor prognosis and long-term monitoring of the remaining dentition using serial radiographs, periodontal measures, sensibility tests, or patient symptoms. Edentulous saddles may be restored using adhesive or conventional fixed bridges, removable partial dentures, or osseointegrated implants. Abutment teeth must be carefully assessed for root resorption. The success of long-term osseointegration in sites where root resorption has been active is unknown. In severe cases, the only option available may be extraction of all teeth and construction of a complete denture.
According to Fuss et al.,[18] to ‘render proper treatment’, root resorption invariably relies on ‘removing the etiological factor’; consequently, given that the etiology was unclear in all cases, appropriate management involved stabilization of the condition and avoidance of factors likely to compound the problem. If adverse occlusal loading or occlusal trauma is suspected, then adjustment of occlusal interferences or provision of an occlusal appliance to remove the influence of such interferences may be indicated. In the present case; patient's occlusion was examined, but no wear facets or premature contacts were found and the patient gave no history of bruxism or clenching. He had no history of orthodontic treatment, trauma, or any unusual dental, medical, or dietary factors.
A more invasive approach involves endodontic treatment of the affected teeth. This has been well-documented for inflammatory root resorption, where calcium hydroxide is the current intraradicular medicament of choice. However, a common finding in MIEARR is that teeth remain vital even after extensive root resorption. It has been suggested that Ledermix (triamcinolone acetonide and demeclocycline calcium, Lederle Laboratories, UK) inhibits the proliferation of dentinoclasts[19] and it may prove effective when mixed with calcium hydroxide. An experimental approach may be calcitonin[20] as an intracanal medicament. Calcitonin inhibits osteoclast motility and retraction and could be potentially useful in modifying the resorptive process. Postlethwaite and Hamilton[21] unfortunately could not find a positive outcome with endodontic therapy and calcium hydroxide as an intracanal medicament. Rivera and Walton[22] stated that MIEARR does not seem to be mediated by or have its source from the dental pulp. Therefore, in the absence of pulpal symptoms, endodontic therapy cannot be indicated for MIEARR. In the future, bioactive molecules capable of modifying the process of root resorption may become available which target the periradicular resorptive process.[23]
CONCLUSIONS
The current mainstay of management for affected individuals remains long-term monitoring, but occlusal therapy and restorative dental treatment have a role in appropriate circumstances. However, endodontic therapy is not indicated at the present time. The etiology of MIEARR remains unknown, but it is hoped that in future the discovery of the molecular and cellular mechanism of root resorption will yield new methods of treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kerr DA, Courtney RM, Burkes EJ. Multiple idiopathic root resorption. Oral Surg Oral Med Oral Pathol. 1970;29:552–65. doi: 10.1016/0030-4220(70)90467-6. [DOI] [PubMed] [Google Scholar]
- 2.Bakland LK. Root resorption. Dent Clin North Am. 1992;36:491–507. [PubMed] [Google Scholar]
- 3.Newman WG. Possible etiologic factors in external root resorption. Am J Orthod. 1975;67:522–39. doi: 10.1016/0002-9416(75)90298-5. [DOI] [PubMed] [Google Scholar]
- 4.Topkara A, Karaman AI, Kau CH. Apical root resorption caused by orthodontic forces: A brief review and a long-term observation. Eur J Dent. 2012;6:445–53. [PMC free article] [PubMed] [Google Scholar]
- 5.Cholia SS, Wilson PH, Makdissi J. Multiple idiopathic exernal apical root reorption: Report of four cases. Dentomaxillfac Radiol. 2005;34:240–6. doi: 10.1259/dmfr/74146718. [DOI] [PubMed] [Google Scholar]
- 6.Khojastepour L, Bronoosh P, Azar M. Multiple idiopathic apical root resorption: A Case report. J Dent (Tehran) 2010;7:165–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Kanungo M, Khandelwal V, Nayak UA, Nayak PA. Multiple idiopathic apical root resorption. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2013-009696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moazami F, Karami F. Multiple idiopathic apical root resorption: A case report. Int Endod J. 2007;40:573–8. doi: 10.1111/j.1365-2591.2007.01267.x. [DOI] [PubMed] [Google Scholar]
- 9.Hegde S, Shubha AB, Kakti A, Rao BD. Extensive idiopathic external apical root resorption on a 13 year old child. J Clin Pediatr Dent. 2012;36:289–92. doi: 10.17796/jcpd.36.3.a3m31828227kq6h8. [DOI] [PubMed] [Google Scholar]
- 10.Di Domizio P, Orsini G, Scarano A, Piattelli A. Idiopathic root resorption: Report of a case. J Endod. 2000;26:299–300. doi: 10.1097/00004770-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Stafne EC, Slocumb CH. Idiopathic resorption of teeth. Am J Orthod Oral Surg. 1944;30:41–9. [Google Scholar]
- 12.Gunraj MN. Dental root resorption. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:647–53. doi: 10.1016/s1079-2104(99)70002-8. [DOI] [PubMed] [Google Scholar]
- 13.Al-Qawasmi RA, Hartsfield JK, Jr, Everett ET, Flury L, Liu L, Foroud TM, et al. Genetic predisposition to external apical root resorption in orthodontic patients: Linkage of chromosome-18 marker. J Dent Res. 2003;82:356–60. doi: 10.1177/154405910308200506. [DOI] [PubMed] [Google Scholar]
- 14.Urban D, Mincik J. Monozygotic twins with idiopathic internal root resorption: A case report. Aust Endod J. 2010 Aug;36:79–82. doi: 10.1111/j.1747-4477.2010.00223.x. [DOI] [PubMed] [Google Scholar]
- 15.Iglesias-Linares A, Yañez-Vico R, Ballesta-Mudarra S, Ortiz-Ariza E, Ortega-Rivera H, Mendoza-Mendoza A, et al. Postorthodontic external root resorption is associated with IL1 receptor antagonist gene variations. Oral Diseases. 2012;18:198–205. doi: 10.1111/j.1601-0825.2011.01865.x. [DOI] [PubMed] [Google Scholar]
- 16.Pinska E, Jarzynka W. Spontaneous resorption of the roots of all permanent teeth as a familial disease. Czas Stomatol. 1966;19:161–5. [PubMed] [Google Scholar]
- 17.Saravia ME, Meyer ML. Multiple idiopathic root resorption in monozygotic twins: Case report. Pediatr Dent. 1989;11:76–8. [PubMed] [Google Scholar]
- 18.Fuss Z, Tsesis I, Lin S. Root resorption: Diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19:175–82. doi: 10.1034/j.1600-9657.2003.00192.x. [DOI] [PubMed] [Google Scholar]
- 19.Pierce An, Heithersay G, Lindskog S. Evidence for direct inhibition of dentinoclasts by a corticosteroid/antibiotic endodontic paste. Endod Dent Traumatol. 1988;4:44–5. doi: 10.1111/j.1600-9657.1988.tb00292.x. [DOI] [PubMed] [Google Scholar]
- 20.Pierce A, Berg JO, Lindskog S. Calcitonin as an alternative therapy in the treatment of root resorption. J Endod. 1988;14:459–64. doi: 10.1016/S0099-2399(88)80136-5. [DOI] [PubMed] [Google Scholar]
- 21.Postlethwaite KR, Hamilton M. Multiple idiopathic external root resorption. Oral Surg Oral Med Oral Pathol. 1989;68:640–3. doi: 10.1016/0030-4220(89)90253-3. [DOI] [PubMed] [Google Scholar]
- 22.Rivera EM, Walton RE. Extensive idiopathic apical root resorption: A case report. Oral Surg Oral Med Oral Pathol. 1994;78:673–7. doi: 10.1016/0030-4220(94)90184-8. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg M, Six N, Decup F, Lasfargues JJ, Salih E, Tompkins K, et al. Bioactive molecules and the future of pulp therapy. Am J Dent. 2003;16:66–76. [PubMed] [Google Scholar]


