Abstract
Purpose:
To report long-term follow-up of zonulo-hyaloido-vitrectomy (ZHV) via anterior approach for pseudophakic malignant glaucoma refractory to medical treatment.
Design:
Noncomparative case-series.
Materials and Methods:
Medical records of 9 patients who sought treatment for aqueous humor misdirection refractory to medical treatment were reviewed. All patients underwent anterior vitrectomy, hyaloido-zonulectomy, and peripheral iridectomy (PI) via an anterior approach. Main outcome measures were preoperative and postoperative visual acuity, intraocular pressure, medications, slit-lamp examination, and fundus findings.
Results:
10 eyes of 9 patients (7 female, 2 male) who underwent ZHV for refractory pseudophakic malignant glaucoma between 2003 and 2010 were included in this case-series. The mean age of patients was 77.4 ± 9.0 years, mean follow-up duration 50.2 ± 27.2 months. Recurrence of malignant glaucoma was noted in 40% (four cases) after a successful ZHV on long-term follow-up.
Conclusions:
An anterior segment surgeon can treat malignant glaucoma refractory to medical treatment successfully by vitrectomy, hyaloido-zonulectomy, and PI. This can be done via an anterior approach and patients require long follow-up to rule out a relapse despite a successful outcome in the short term.
Keywords: Malignant glaucoma, pseudophakic, surgical management, zonulo-hyaloido-vitrectomy
Malignant glaucoma is a rare secondary glaucoma diagnosed on the basis of a central and peripheral flat anterior chamber (AC), raised intraocular pressure (IOP), a patent peripheral iridectomy (PI) or laser peripheral iridotomy (LPI) and the absence of choroidal abnormalities.[1] It may occur in 2–4% of eyes with primary angle closure (PAC), typically after trabeculectomy or cataract surgery.[2] However, it can occur after almost any laser or surgical procedure in predisposed eyes. It has been reported after tube drainage surgery,[3] needling of trabeculectomy bleb,[4] vitrectomy[5,6] and laser procedures like Argon laser suture lysis of trabeculectomy flap,[7] LPI,[8] neodymium-doped: Yttrium aluminum garnet (Nd: YAG) laser posterior capsulotomy[9] and diode laser cyclophotocoagulation.[10] Malignant glaucoma is believed to be a type of cilio-lenticular block with aqueous diversion into the vitreous.[2]
In malignant glaucoma, the initial treatment is medical and is reported to be successful in 50% of cases in about 15 days.[11] It consists of cycloplegics, oral acetazolamide, and hyperosmotic agents. Topical aqueous suppressants and prostaglandin analogs have minimal effect on the IOP and pilocarpine may worsen the condition. Laser and surgical treatment is aimed at re-establishing a communication between the anterior and posterior segments of the eye. Nd: YAG laser hyaloidotomy[12] and more recently cyclodiode laser[13,14] have been used successfully treat the condition. In eyes not responding to medical or laser therapy, surgery has to be considered. Vitrectomy is probably the most effective surgical option and has to be performed by a vitreo-retinal (VR) surgeon.[15,16] Zonulo-hyaloido-vitrectomy (ZHV) has been described as an alternative surgical treatment for psuedophakic malignant glaucoma by anterior segment surgeons.[16,17]
We report the long-term follow-up of patients who underwent ZHV for malignant glaucoma unresponsive to medical or laser treatment.
Materials and Methods
Consecutive patients referred to the glaucoma clinic with pseudophakic malignant glaucoma who had ZHV between 2003 and 2010 were included in the study. Malignant glaucoma was diagnosed on the basis of a shallow or flat AC, raised IOP, presence of a patent PI or LPI, and the absence of a suprachoroidal effusion or hemorrhage. Patient information was retrospectively derived from case-notes and included history, surgical procedures, and medications. Snellen chart best-corrected visual acuity (BCVA), IOP, anterior segment, fundus findings and complications were noted.
Surgical procedure
Zonulo-hyaloido-vitrectomy was done via an anterior approach. A supero-temporal or nasal corneal incision parallel to the iris plane was made. A peripheral corneal paracentesis was made about 3 h away from the main incision. A PI was performed. The AC was then filled with a viscoelastic agent. The vitreous cutter was then introduced through the section, into the PI enlarging it whenever necessary. A zonulectomy was performed followed by a hyloidectomy and anterior vitrectomy. This was continued till the AC deepened, indicating the creation of a common passage between the vitreous cavity and the posterior chamber. Care was taken to introduce and maintain the cutter opened toward the center of the vitreous cavity and to direct it away from the ciliary processes and peripheral retina to prevent their damage. The main incision was sutured with a 10/0 nylon suture. Subconjunctival steroids and intracameral antibiotics were given on completion.
Results
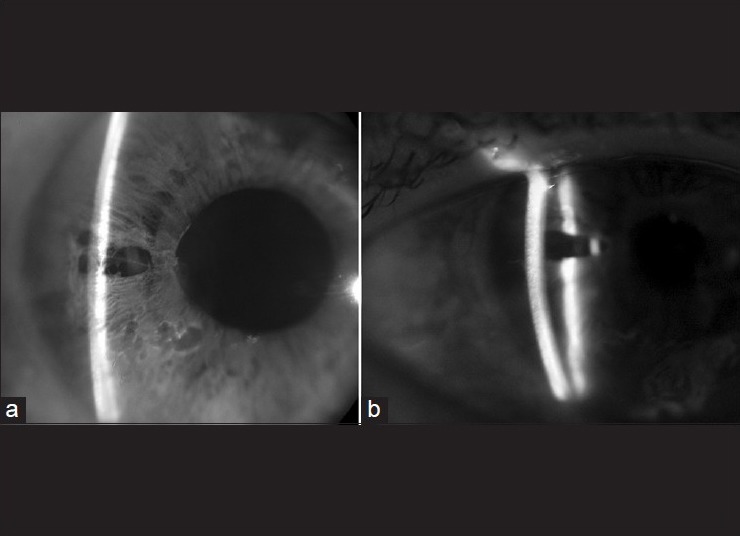
Ten eyes of 9 patients were included in the study. Mean follow-up was 50.2 ± 27.2 months. Mean age was 77.4 ± 9.0 years. There was a female preponderance with 7 females and 2 males. Mean ocular axial length was 21.32 ± 1.21 mmHg. Recurrence of malignant glaucoma after ZHV occurred in 4 eyes (40%). Patient details, procedures, and outcomes are listed in Table 1.
Table 1.
Details of patients undergoing Zonulo-hyaloido-vitrectomy
Case 1
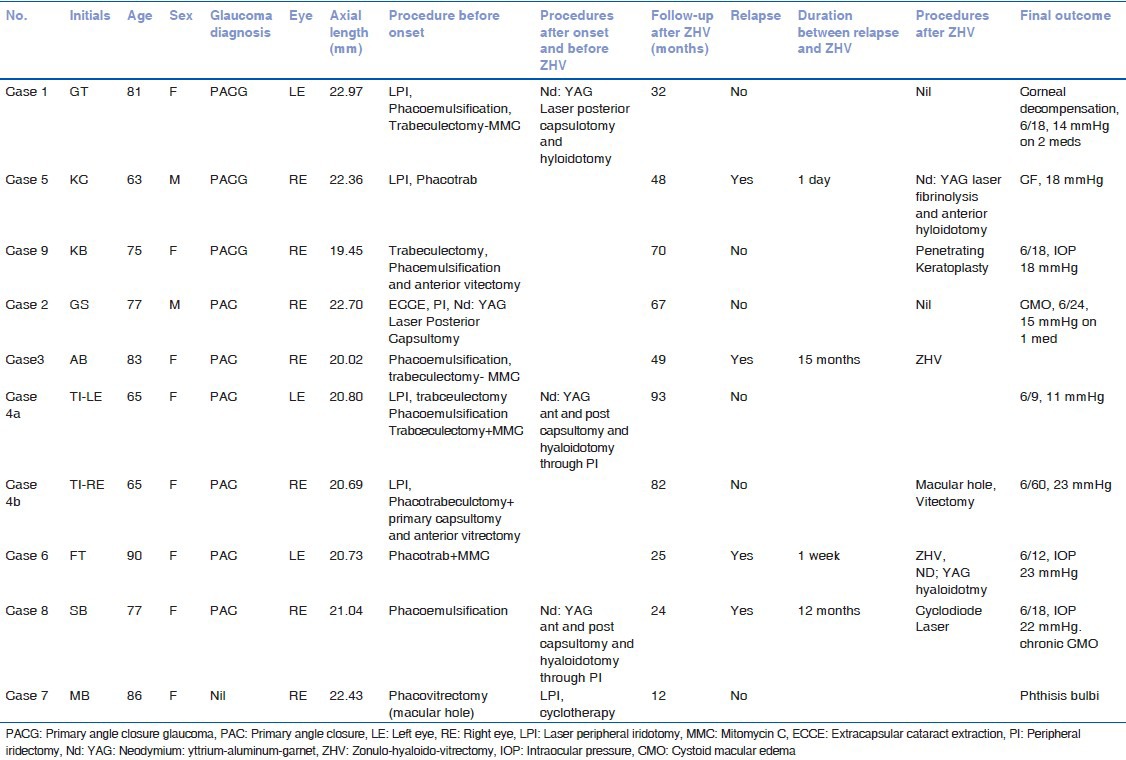
An 81-year-old Caucasian female was referred with an IOP of 48 mmHg on maximal medications and corneal edema after phacoemulsification. LPIs had been done in the past for PAC glaucoma (PACG). The AC was moderately shallow. An urgent trabeculectomy with intraoperative mitomycin C (MMC) application was done. The following morning, the IOP was 24 mmHg with a flat AC. Malignant glaucoma was suspected, and the patient started on atropine and topical steroids. Nd: YAG laser posterior capsulotomy and hyloidotomy were done, but the AC remained very shallow and the IOP increased to over 40 mmHg. The following week, a ZHV was performed, and the AC deepened intraoperatively [Fig. 1]. Postoperatively, while the AC was deep, the IOP remained high and on gonioscopy, the angle was almost completely closed. She was started on dorzolamide-timolol fixed combination eyes drops. On her last visit, 32 months after ZHV, VA was 20/60 and IOP 14 mmHg on medications. There was corneal edema, and the AC remained deep.
Figure 1.
(a) Case 1 with shallow anterior chamber (AC) and viscoelastic coming through paracentesis (arrow) due to high intraocular pressure (b) entry into AC with keratome. Keratome is withdrawn and directed posteriorly through iris and zonules (c) peripheral iridectomy performed with vitreous prolapsing through the section (d and e) zonulectomy, hyloidectomy, and anterior vitrectomy performed with vitreous cutter blood in AC from section as intraocular pressure has dropped significantly (f) viscoleastic injected into AC angle to break peripheral anterior synechiae (arrow)
Case 2
A 77-year-old Caucasian male who had a routine extracapsular cataract extraction with a surgical PI in his right eye 15 years ago, was seen with complaints of blurred vision. His BCVA was 20/30. Nd: YAG laser posterior capsulotomy was done twice. It was repeated after a year as he was still complaining of blurred vision, and the ophthalmologist thought that the central capsular clearance was inadequate. A month later, he had no improvement, and his VA was 20/60. The AC was deep, and some vitreous was herniating though the inferotemporal pupillary margin. He was managed conservatively. A further 6 months later his VA had decreased to 20/200 and IOP was 32 mmHg. He was started on topical beta-blockers, but the IOP remained high. He was referred to the glaucoma clinic where a shallow AC with peripheral iris-cornea touch and vitreous herniation through the inferotemporal pupillary margin was noted. Malignant glaucoma was diagnosed, and ZHV performed. By the 6th postoperative week, the IOP increased to 40 mmHg. It was controlled on topical travoprost and brinzolamide. Gonioscopy showed that the angle was >270° closed. He also developed nonresponsive cystoid macular edema (CMO). On the last visit, 67 months after ZHV, his IOP was 14 mmHg on the aforementioned medications and BCVA was 20/120.
Case 3
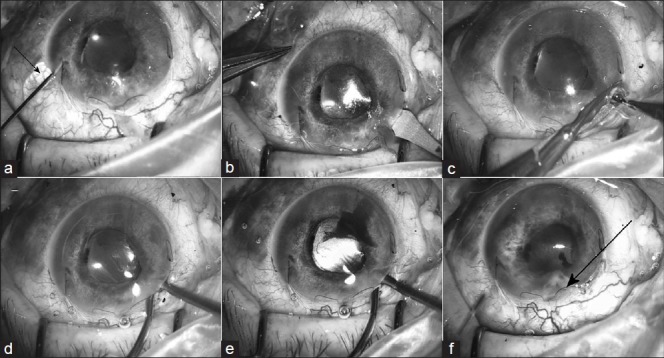
An 83-year-old lady of Indian origin with PAC, bilateral pseudophakia and IOP of 35 mmHg on maximal medical therapy underwent an augmented trabeculectomy with MMC in the right eye. Preoperatively, the AC was moderately shallow in the right eye, and gonioscopy showed a closed angle. The left eye AC was shallow with some peripheral anterior synechiae. A month later, the AC remained shallow, and IOP was 15–20 mmHg on 3 topical glaucoma medications. The patient was referred to the glaucoma clinic where malignant glaucoma was diagnosed, and ZHV preformed. The AC deepened; IOP settled at 15 mmHg and VA was 20/30. 6 months later, she presented with blurred vision for 3 months in the same eye. Her IOP was 23 in the left eye, and the AC was shallow with peripheral irido-corneal touch. Malignant glaucoma was suspected, and she was treated with Atropine 1% drops in that eye. The vision improved to 20/30, the AC deepened, and the IOP was 19 mmHg at 7 days follow-up. However, on a routine follow-up visit 15 months after ZHV, IOP was raised at 34 mmHg and peripheral AC was shallow once more with iridocorneal touch. A repeat ZHV was performed after which the AC deepened [Fig 2]. 2 years after the second ZHV, the IOP was stable at 17 mmHg without medication.
Figure 2.
Anterior segment photograph of case 3, before (a) and after (b) zonulo-hyaloidovitrectomy
Case 4a and b
A 65-year-old Caucasian lady with PAC, previous bilateral LPIs and trabeculectomy was re-referred for blurred vision. BCVA was 20/30 in the right eye and 20/40 in the left eye. IOPs were 16 mmHg in the right and 28 mmHg in the left eye. She underwent an uneventful cataract extraction in the left eye. The following day, IOP was 68 mmHg and AC shallow.
Gonioscopy showed a closed angle. She was referred to the glaucoma firm as the IOP did not settle with conservative management. An urgent trabeculectomy with MMC augmentation was performed. The next day, AC was flat, and IOP measured 42 mmHg. Malignant glaucoma was considered and a Nd: YAG posterior capsulotomy and hyaloidotomy was done. The AC deepened after the procedure. However 2 days later, the AC was shallow with an IOP of 22 mmHg. This time the eye did not respond to a repeat laser hyaloidotomy and surgical ZHV was performed. On final review, 93 months after, the VA was 20/30 and IOP 11 mmHg on no medications.
For her right eye, phacotrabeculectomy with intraoperative MMC augmentation was done. An intraocular lens (IOL) was placed in the ciliary sulcus after a central core vitrectomy was performed through a posterior capsulotomy. Two weeks after surgery, VA was 20/30 and IOP 24 mmHg, with a deep AC. Scleral flap suture removal and bleb needling with 5-florouracil was performed. The IOP dropped to 4 mmHg. 3 weeks postoperatively, she complained of photophobia and an ache around that eye. Her IOP was 60 mmHg, AC shallow and VA 20/200. Malignant glaucoma was diagnosed which did not respond to maximal glaucoma medications and topical atropine. ZHV was done in the right eye 4 weeks after the phacotrabeculectomy. After ZHV, the AC deepened, and IOP was 17 mmHg. A month after ZHV, the vision had deteriorated to 20/120. A stage 4 macular hole was noted, and she had a complete vitrectomy with internal limiting membrane peel and internal gas tamponade by the VR surgeon. The procedure failed to improve her vision. In her last visit, 82 months after ZHV, VA was 20/200 and IOP 23 mmHg on no medications.
Case 5
A 63-year-old Caucasian gentleman with schizophrenia was referred to the glaucoma clinic by his optician with bilateral pale optic discs, IOPs over 60 mmHg and vision of counting fingers in both eyes. In both eyes, AC was shallow; the angle completely closed, and the optic discs cupped and pale. A diagnosis of chronic angle closure was made, and bilateral LPIs done. The patient was started on oral acetazolamide and 3 topical glaucoma medications. A month later, the IOP had reduced to 21 mmHg in the right eye. Right eye phacotrabeculectomy under general anesthesia was done with prior explanation of the poor prognosis for visual recovery to the relatives. Intraoperatively, a floppy iris was noted which responded to intracameral phenylephrine. Postoperatively, the AC was shallow and IOP 16 mmHg. A week later, the IOP crept to 23 mmHg, the AC remained shallow with a fibrinous deposit over the pupil. Malignant glaucoma was considered to be the cause and ZHV performed. The AC deepened on the table, but the next morning, the AC was shallow with fibrin covering the pupil and the PI. Nd: YAG laser lysis of the fibrin and anterior hyaloidotomy through the PI was done. The AC deepened immediately. The IOP has been stable over the next 4 years at 18 mmHg without glaucoma medications. However, VA was counting fingers.
Case 6
An 89-year-old lady with high hypermetropia was referred by her optician for raised IOPs of 49 and 40 mmHg in the right and left eye, respectively. She had bilateral cataracts reducing VAs to 20/60 right and 20/30 in left eye. The optic discs were healthy. She was commenced on topical prostaglandin analogs and subsequently had phacotrabeculectomy with MMC in the right eye. On the first postoperative visit, the AC was very shallow with iridocorneal touch and IOP 24 mmHg. Malignant glaucoma was suspected and topical atropine 1% was started. An air bubble was injected to reform the AC. The AC remained shallow. On the advice from one of us (NA), the surgeon performed a ZHV and noted that the AC had deepened intraoperatively. However, the AC was shallow and IOP 35 mmHg the following day. She was then referred to the glaucoma clinic, and a repeat ZHV was done. The emphasis was to remove the anterior vitreous. Following the procedure, her AC deepened, and IOP was 22 mmHg. A month later, her vision improved to 20/60 but her IOP was raised at 40 mmHg with a moderately shallow AC. It was felt that the PI was blocked by vitreous and Nd: YAG laser hyaloidotomy was done through the PI. The AC deepened immediately after the laser. The IOP was initially controlled on 3 topical medications. Two years later, VA was 20/40, the IOP 23 mmHg on a timolol-dorzolamide fixed combination and AC deep. In the interim, her left eye which had raised IOP and >180° of iridotrabecular contact underwent a routine phacoemulsification with no subsequent complications.
Case 7
An 86-year-old Caucasian female was referred to the VR specialist for deteriorating vision in her right eye (2/200) due to a macular hole. The diagnosis was confirmed on optical coherence tomography, and she underwent a phacovitrectomy with internal limiting membrane peel, posterior chamber IOL implantation and gas tamponade with C2F6. On the first postoperative day, her AC was shallow and IOP 66 mmHg. This was thought to be because of gas overfill as the lower edge of the gas bubble was not visualized. The gas was released on 2 separate occasions by the VR surgeon. Laser and surgical PIs were done, but IOP remained extremely high on maximal medication, oral and intravenous hyperosmotic agents. B-scan ultrasonography ruled out suprachoroidal hemorrhage. Malignant glaucoma was diagnosed and 2 weeks after the VR surgery a ZHV was done. The rationale was that the remaining anterior vitreous was probably blocking communication between the anterior and posterior segments. Postoperatively, the AC deepened, and IOP decreased to 4 mmHg. However, there was no visual recovery, and the eye became phthisical over the next few months.
Case 8
A 77-year-old lady with PAC and an IOP of 34 mmHg without medication underwent a phacoemulsification in her right eye. The procedure was difficult with positive pressure and iris prolapsed through the temporal corneal section. 2 weeks postoperatively, IOP rose to 44 mmHg and AC shallowed significantly [Fig. 2a]. Nd: YAG laser anterior and posterior capsulotomy and hyaloidotomy were done through an inadvertent temporal PI. The AC deepened immediately after the procedure, and the IOP dropped to 34 mmHg. Over the next 2 weeks, the AC was deep, and IOP stabilized at 15 mmHg on topical latanoprost. In the meantime, she also underwent a routine phacoemulsification in the fellow eye. 4 months after her phacoemulsification, the right eye IOP had crept up to 32 mmHg on maximal tolerated medications and AC shallowed. ZHV was performed. Postoperatively, the AC deepened but the IOP control was inadequate, and CMO was noted. The CMO resolved on oral acetazolamide, topical prednisolone 1%, and ketorolac eye drops. However, gradually she developed intolerance to most topical medications. A year after ZHV, she noted blurred vision in the right eye. The IOP was over 30 mmHg, the AC moderately shallow and CMO had recurred. This time 270° cyclodiode laser was done, leading to resolution of the malignant glaucoma. The CMO partially resolved on oral acetazolamide. 2 years after the ZHV, her VA was 20/60 and IOP 22 mmHg without medication.
Case 9
An 81-year-old Caucasian lady with PACG was referred to the glaucoma clinic for raised IOP and blurred vision in the right eye. She had LPI and trabeculectomy 15 years ago and phacoemulsification with anterior vitrectomy 8 years ago. Her left eye had no vision due to complicated extracapsular cataract extraction, bullous keratopathy, and possible advanced glaucomatous optic atrophy. The IOP in the right eye was 22 mmHg on oral acetazolamide, topical pilocarpine 2%, latanoprost, and apraclonidine 1%. The VA was 20/40 with peripheral corneal edema and a shallow AC. Malignant glaucoma was thought to be the cause. Pilocarpine drops were stopped, and atropine started. However, the AC remained shallow. A ZHV was performed, and the AC deepened on the table. She subsequently underwent a penetrating keratoplasty for the preexisting pseudophakic bullous keratopathy. There has been no recurrence of malignant glaucoma for the last 7 years. On her last visit, the VA was 20/60 and IOP 18 mmHg without medications.
Discussion
Malignant glaucoma, first described by Von Graefe is a rare secondary glaucoma. It is common in eyes with PAC and can happen days, months or years after any intraocular surgery or laser in predisposed eyes. The term aqueous misdirection is used synonymously as experts believe that IOP rise is due to abnormal flow of the aqueous into the vitreous rather than the anterior segment.[2] Various anomalies of the ciliary body, choroid, lens, zonule, and vitreous which may lead to posterior diversion of aqueous humor into the vitreous cavity have been proposed.[2] Anterior rotation of the ciliary body processes can lead to cilio-lenticular touch and ciliary block.[18] Ultrasound biomicroscopy may aid in the diagnosis, but this was not available in our setting. Quigley proposed that choroidal exudation during a surgical intervention happens and the exudate is unable to pass through an abnormally impermeable vitreous. The vitreous body exerts forwards pressure on the lens and ciliary processes, leading to shallow AC and raised IOP, which does not respond to conventional treatment.[19]
Regardless of pathophysiology, malignant glaucoma is relieved when a direct communication is made between the AC and vitreous cavity. This implies that the lens, anterior vitreous face, and ciliary processes are intimately involved.[1]
The recommended initial management is medical. Topical cycloplegics may need to be continued indefinitely in some eyes to prevent a recurrence. In pseudophakic eyes, Nd: YAG laser hyaloidotomy is best done peripherally, as near the ciliary processes as possible.[20] It may be done through a preexisting PI or after maximal dilation of the pupil where there is no PI. An anterior and posterior capsulotomy is done prior to the hyaloidotomy. Transscleral cyclodiode laser ciliary body ablation has been reported to be effective in treating eyes not responding to medical treatment.[13,14]
Surgical means create a communication between the vitreous cavity and the AC. In phakic eyes, this involves lens removal and vitrectomy, more importantly an anterior rather than a core vitrectomy. Malignant glaucoma has been reported after vitrectomy which failed to remove the anterior hyaloid as in Case 7.[6] Tsai et al. investigated the surgical results in 25 patients with malignant glaucoma. Laser hyaloidotomy alone was successful in 16% and core vitrectomy in 4 of 6 pseudophakic (67%) and 1 of 4 phakic patients (25%). Combined cataract extraction and vitrectomy had a higher success rate in patients undergoing posterior capsulectomy at the time of surgery (5 of 6 patients; 83%) compared with those patients left with an intact posterior capsular bag (1 of 4 patients; 25%). Intracapsular cataract extraction was successful in 1 of 2 patients (50%). They recommended combined lens extraction, primary posterior capsulectomy and surgical vitrectomy for the surgical management of phakic malignant glaucoma.[21] Another approach recently described is vitrectomy-phacoemulsification-vitrectomy for malignant glaucoma in phakic eyes. After a core vitrectomy creates space, phacoemulsification is performed. Then residual vitrectomy, zonulohyaloidectomy, and PI (if not already present) is done by the VR surgeon.[22]
Zonulo-hyaloido-vitrectomy is a modification of this approach in pseudophakic eyes. A Medline search showed two case-series of ZHV for malignant glaucoma (one via the pars plana and the other through the anterior segment) with a 100% success rate at <1-year follow-up.[16,17]
All cases in the current series were performed via an anterior approach under local anesthesia with a mean follow-up of 4 years. Malignant glaucoma recurred in four cases (40%). The reasons are blockage of the channel by fibrin (Case 5) or vitreous (Cases 3, 6, 8).[5] In Case 6 it is also likely that the first ZHV was incomplete. In Case 3, malignant glaucoma recurred after 15 months and in Case 8 after 1-year. A case series from Belgium reported outcomes of multiple interventions for malignant glaucoma in 24 eyes of 21 patients. The relapse rates were 100% for medical management, 75% for Nd: YAG laser capsulotomy and hyaloidotomy, 75% for conventional vitrectomy and 66% after anterior vitrectomy with iridectomy-zonulectomy ZHV. There was no relapse after a complete vitrectomy with iridectomy-zonulectomy. The relapse rates were high with ZHV (66% vs. 40% in this series) despite a limited mean follow-up of 50 days (range 1–300) compared to 4 years in our patients.[23] It is difficult to explain this difference, as success rates with ZHV were <90% in the two aforementioned case-series.[16,17] Our success rates were lower, but this may be due to the longer follow-up period. Long-term failure after ZHV may be due to anterior movement of vitreous and blockage of the channel through the zonulectomy-iridectomy. However, all 4 relapses were successfully treated by modalities other than complete vitrectomy with iridectomy-zonulectomy [Table 1].
Case 4 is an example of malignant glaucoma in a vitrectomized eye. Probably the anterior hyaloid phase remained intact after core vitrectomy for macular hole. The lady lost her vision due to uncontrolled IOP for a prolonged period. As she had already undergone a vitrectomy, malignant glaucoma was not suspected initially causing a delay in surgical management with ZHV. ZHV disrupted the anterior hyaloid creating a communication between the two chambers thus normalizing the IOP. It is evident that malignant glaucoma may occur after a complete vitrectomy unless the vitreous base is also removed.[5,23,24]
There were serious sight-threatening complications associated with ZHV. Macular hole (Case 4b) and CMO (CASE 8) could be attributed to ZHV. The cornea decompensated in 2 eyes (Cases 1 and 9). In one of these, there was preexisting corneal edema. In Case 7, the eye became phthisical due to prolonged raised IOP rather than ZHV. The ophthalmologist may not always recognize malignant glaucoma. In Cases 1 and 4 malignant glaucoma was probably not recognized, and the patient underwent an incorrect procedure, trabeculectomy. Case 9 was diagnosed as chronic angle closure glaucoma despite being pseudophakic and placed on pilocarpine, which may aggravate the condition.
Conclusion
In summary, this case-series shows that ZHV can be performed by the anterior segment surgeon to reverse malignant glaucoma in pseudophakic eyes. There is, however, a long-term risk of relapse, and this should be explained to the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Ruben S, Tsai J, Hitchings RA. Malignant glaucoma and its management. Br J Ophthalmol. 1997;81:163–7. doi: 10.1136/bjo.81.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luntz MH, Rosenblatt M. Malignant glaucoma. Surv Ophthalmol. 1987;32:73–93. doi: 10.1016/0039-6257(87)90101-9. [DOI] [PubMed] [Google Scholar]
- 3.Greenfield DS, Tello C, Budenz DL, Liebmann JM, Ritch R. Aqueous misdirection after glaucoma drainage device implantation. Ophthalmology. 1999;106:1035–40. doi: 10.1016/S0161-6420(99)00530-8. [DOI] [PubMed] [Google Scholar]
- 4.Ramanathan US, Kumar V, O’Neill E, Shah P. Aqueous misdirection following needling of trabeculectomy bleb. Eye (Lond) 2003;17:441–2. doi: 10.1038/sj.eye.6700270. [DOI] [PubMed] [Google Scholar]
- 5.Massicotte EC, Schuman JS. A malignant glaucoma-like syndrome following pars plana vitrectomy. Ophthalmology. 1999;106:1375–9. doi: 10.1016/S0161-6420(99)00727-7. [DOI] [PubMed] [Google Scholar]
- 6.Zacharia PT, Abboud EB. Recalcitrant malignant glaucoma following pars plana vitrectomy, scleral buckle, and extracapsular cataract extraction with posterior chamber intraocular lens implantation. Ophthalmic Surg Lasers. 1998;29:323–7. [PubMed] [Google Scholar]
- 7.Macken P, Buys Y, Trope GE. Glaucoma laser suture lysis. Br J Ophthalmol. 1996;80:398–401. doi: 10.1136/bjo.80.5.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Small KM, Maslin KF. Malignant glaucoma following laser iridotomy. Aust N Z J Ophthalmol. 1995;23:339–41. doi: 10.1111/j.1442-9071.1995.tb00188.x. [DOI] [PubMed] [Google Scholar]
- 9.Malukiewicz G, Stafiej J. Malignant glaucoma and central retinal vein occlusion after Nd: YAG laser posterior capsulotomy. Klin Oczna. 2011;113:254–7. [PubMed] [Google Scholar]
- 10.Azuara-Blanco A, Dua HS. Malignant glaucoma after diode laser cyclophotocoagulation. Am J Ophthalmol. 1999;127:467–9. doi: 10.1016/s0002-9394(98)00359-6. [DOI] [PubMed] [Google Scholar]
- 11.Simmons RJ. Malignant glaucoma. Br J Ophthalmol. 1972;56:263–72. doi: 10.1136/bjo.56.3.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melamed S, Ashkenazi I, Blumenthal M. Nd-YAG laser hyaloidotomy for malignant glaucoma following one-piece 7 mm intraocular lens implantation. Br J Ophthalmol. 1991;75:501–3. doi: 10.1136/bjo.75.8.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stumpf TH, Austin M, Bloom PA, McNaught A, Morgan JE. Transscleral cyclodiode laser photocoagulation in the treatment of aqueous misdirection syndrome. Ophthalmology. 2008;115:2058–61. doi: 10.1016/j.ophtha.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 14.Muqit MM, Menage MJ. Malignant glaucoma after phacoemulsification: Treatment with diode laser cyclophotocoagulation. J Cataract Refract Surg. 2007;33:130–2. doi: 10.1016/j.jcrs.2006.07.041. [DOI] [PubMed] [Google Scholar]
- 15.Harbour JW, Rubsamen PE, Palmberg P. Pars plana vitrectomy in the management of phakic and pseudophakic malignant glaucoma. Arch Ophthalmol. 1996;114:1073–8. doi: 10.1001/archopht.1996.01100140275003. [DOI] [PubMed] [Google Scholar]
- 16.Bitrian E, Caprioli J. Pars plana anterior vitrectomy, hyaloido-zonulectomy, and iridectomy for aqueous humor misdirection. Am J Ophthalmol. 2010;150:82–7.e1. doi: 10.1016/j.ajo.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Lois N, Wong D, Groenewald C. New surgical approach in the management of pseudophakic malignant glaucoma. Ophthalmology. 2001;108:780–3. doi: 10.1016/s0161-6420(00)00642-4. [DOI] [PubMed] [Google Scholar]
- 18.Tello C, Chi T, Shepps G, Liebmann J, Ritch R. Ultrasound biomicroscopy in pseudophakic malignant glaucoma. Ophthalmology. 1993;100:1330–4. doi: 10.1016/s0161-6420(93)31479-x. [DOI] [PubMed] [Google Scholar]
- 19.Quigley HA. Angle-closure glaucoma-simpler answers to complex mechanisms: LXVI Edward Jackson Memorial Lecture. Am J Ophthalmol. 2009;148:657–69. doi: 10.1016/j.ajo.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Simmons RJ, Thomas JV, Yaqub F, Ritch R, Shields MB, Krupin T, editors. St Louis: CV Mosby; 1995. The Glaucomas; pp. 1251–63. [Google Scholar]
- 21.Tsai JC, Barton KA, Miller MH, Khaw PT, Hitchings RA. Surgical results in malignant glaucoma refractory to medical or laser therapy. Eye (Lond) 1997;11:677–81. doi: 10.1038/eye.1997.176. [DOI] [PubMed] [Google Scholar]
- 22.Arya SK, Sonika, Kochhar S, Kumar S, Kang M, Sood S. Malignant glaucoma as a complication of Nd: YAG laser posterior capsulotomy. Ophthalmic Surg Lasers Imaging. 2004;35:248–50. [PubMed] [Google Scholar]
- 23.Debrouwere V, Stalmans P, Van Calster J, Spileers W, Zeyen T, Stalmans I. Outcomes of different management options for malignant glaucoma: A retrospective study. Graefes Arch Clin Exp Ophthalmol. 2012;250:131–41. doi: 10.1007/s00417-011-1763-0. [DOI] [PubMed] [Google Scholar]
- 24.Chen SD, Salmon JF, Patel CK. Videoendoscope-guided fluorescein-assisted vitrectomy for phakic malignant glaucoma. Arch Ophthalmol. 2005;123:1419–21. doi: 10.1001/archopht.123.10.1419. [DOI] [PubMed] [Google Scholar]


