Abstract
Introduction: Community‐based participatory research (CBPR) adds community perspectives to research and aids translational research aims. There is a need for increased capacity in CBPR but few models exist for how to support the development of community/university partnerships.
Objective: Evaluate an approach to promote nascent CBPR partnerships.
Methods: Design was a mixed–methods evaluation using interviews, process notes, and open‐ and close‐ended survey questions. We trained 10 community scholars, matched them with prepared researchers to form seven partnerships, and supported their developing partnerships. Sequential mixed–methods analysis assessed research and partnership processes and identified integrated themes.
Results: Four of seven partnerships were funded within 15 months; all self‐reported their partnerships as successful. Themes were: (1) motivators contributed to partnership development and resiliency; (2) partners took on responsibilities that used individuals’ strengths; (3) partners grappled with communication, decision making, and power dynamics; and (4) community–university infrastructure was essential to partnership development.
Conclusions: This program for developing nascent partnerships between academicians and community members may guide others in increasing capacity for CBPR. Clin Trans Sci 2011; Volume 4: 428–433
Keywords: community‐based participatory research, translational research
Introduction
Community‐based participatory research (CBPR) adds community perspectives to research that can increase the validity, usability, and likelihood for sustainability of research products. 1 , 2 , 3 , 4 Investigators have looked to CBPR as a means to address challenges to the translational research process including limited external validity, poor community trust in research, and lack of sustainability of programming in community settings. 5 , 6 Furthermore, community‐engaged research has been identified as a key component of efforts to eliminate health disparities. 7
Despite arguments for CBPR, community‐engaged research represents a small portion of all research, 8 so capacity must be increased. Therefore, approaches are needed that identify effective means for training, developing, and supporting CBPR partnerships between academicians and community members.
Components of CBPR partnerships have been identified in the literature, 9 , 10 , 11 and a model describing CBPR as part of translational research has recently been proposed, 5 but no published report evaluates a capacity building project to promote nascent CBPR research collaborations between university researchers and community members. Our study addresses this gap in the literature.
Methods
Partners in Research (PIR): Improving the Health and Wellness of Immigrants and Refugees in St Paul, Minnesota was an NIH‐funded study that took place in 2009 and 2010. The research team was composed of two university researchers (Schools of Medicine and Public Health), and two collaborators from the cosponsoring community clinic (physician and community organizer). The study design was a mixed–methods evaluation of a capacity building program to support CBPR partnerships. The program focused on training and matching of partners, and facilitation of partnership development. We defined a model to guide our work ( Figure 1 ) including four components identified through a review of the literature and our experiences that lead to partnership success: (1) activated community members who represent their communities in research; (2) prepared researchers who adhere to principles of CBPR; (3) trusted community‐based institutions that facilitate research partnership process; and (4) a flexible and dynamic infrastructure that supports the educational, financial, and logistical needs of CBPR endeavors. 9 , 10 , 11 , 12 , 13 Successful partnerships are funded collaborations that implement research and collaborative processes in a manner consistent with CBPR principles. This project was determined exempt by the University of Minnesota institutional review board (IRB).
Figure 1.
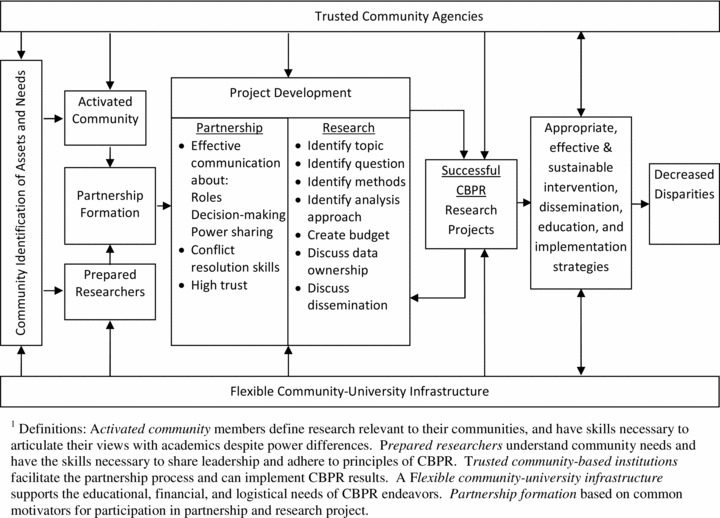
Model for community/university collaborative partnerships to address health disparities. 1
Intervention
We recruited participants from Hmong, Latino, and Somali communities served by the community–clinic partner. Through an interview process, we chose 10 community members to become paid community scholars on the basis of their interest in CBPR, leadership experience, ability to describe a health topic of importance, and bilingual language skills; one participant had prior research experience. We recruited academic faculty (only one had extensive CBPR experience) working in topic areas defined by community scholars with the goal of developing prepared researchers. We created and implemented parallel community and faculty curricula based on a review of the literature; interviews with community leaders and key informant university faculty; 14 and our own experiences with CBPR. Curricula which included didactic, role‐playing, and experiential activities emphasizing communication strategies to address common partnership challenges (trust, decision making, and power sharing), are described elsewhere. 15 Community member trainings additionally focused on developing research capacity. Community scholars received 18 hours of training (six sessions) and faculty received 6 hours of training (two sessions).
The flexible community–university infrastructure consisted of: (1) community–campus liaisons who assisted the research team with matching community scholars with prepared researchers based on community scholars’ research priorities, (2) research team that supported partnership development through meetings with community scholars, partnership facilitation, and consultations as requested, and (3) a competitive university seed‐funding mechanism.
Data analysis
To evaluate the program, we collected qualitative and quantitative data about research processes (i.e., methods, design, and grant writing) and partnership processes (i.e., trust, communication, and decision making). Qualitative data included individual interviews with community and academic participants at the end of the project using an open‐ended questionnaire with prompts adapted from partnership evaluation tools; 16 community scholar group discussion notes; facilitation meetings with funded partnerships; and written comments on a survey at two points in time. Quantitative data provided a more anonymous and standardized assessment of partnership experiences through an online survey that paralleled the interview questions about research and partnership processes. 16 The survey, delivered approximately 3 and 12 months posttrainings, contained 37 Likert‐scaled questions. Nine community scholars and six researchers completed both surveys, although three community scholars completed only the initial survey.
The program was evaluated using a sequential mixed–methods design that prioritized qualitative data. 17 We analyzed the qualitative and quantitative results separately, and then combined them. We analyzed qualitative interviews in a stepwise fashion to identify codes for responses to each question. Three investigators worked together to identify codes and categories by research and partnership processes, using an editing mode of analysis. 18
We analyzed the quantitative survey data using Stata V10 (StataCorp LP, College Station, TX, USA), contrasting responses for community and academic scholars. Given the small sample size, analytical tests of significance were not conducted. Instead, we compared mean responses per item across groups to identify trends within responses.
To connect the qualitative and quantitative data, the four investigators worked together to identify the major themes, incorporating the categories from the qualitative interviews with quantitative trends. Finally, the interviewers returned to the transcripts to identify key quotes to illustrate the themes.
Results
Ten community scholars (four Hmong, three Latino, and three Somalis) were matched with seven researchers to form seven partnerships. Community scholars were diverse in terms of ethnicity, education level, and gender; faculty partners were largely tenured, US‐born, and European‐Americans (Table 1). Six partnerships submitted grant proposals addressing a spectrum of health issues (Table 2) to a competitive university funding mechanism, and three were funded in year one; subsequently two projects were submitted and one was funded at the end of year two. Four community scholars left the project, mostly for life events (i.e., childbirth), and one faculty left the project before solidifying a partnership.
Table 1.
Demographic characteristics of community scholars and collaborating faculty.
| Community scholars (n = 10) | Faculty (n = 7) | |
|---|---|---|
| Gender | 7 women, 3 men | 5 women, 2 men |
| Ethnicity | 4 Hmong, 3 Latino, 3 Somali | 7 White |
| First generation in US | 8 | 0 |
| Education | 3 High school | 1 Medical doctor |
| 4 Bachelor degree | 6 Ph.D. | |
| 3 Master degree | ||
| Academic Rank | Not applicable | 2 Assistant professor |
| 5 Associate or full professor |
Table 2.
Project and partnership descriptions.
| Research topic/community | Community scholars (no.)* | Faculty partners/training | Community agencies | Research phase† |
|---|---|---|---|---|
| Intimate partner violence/Hmong | 2 | 1 Family therapy | Hmong agency | Implementation |
| Childhood obesity/Latino | 2 | 1 Public health | Latino agency | Implementation |
| HIV among women/Somali | 1 | 1 Psychology | Somali agency | Implementation |
| Exercise for elders/Hmong | 2 | 1 Nursing | Hmong agency | Preparation |
| Youth resiliency/Latino | 1 | 1 Family medicine | Latino agency | Preparation |
| Cancer screening among women/Somali | 1 | 1 Public health | Somali agency | Preparation |
| Youth mental health/Somali | 1 | 1 Sociology | None | Prepreparation |
*Four community scholars left the program, 1 early, 1 midway, and 2 at the end of the project evaluation period.
†Implementation, acquired grant support and initiated research; preparation, forming partnership, developing a research project, and competing for funding; pre preparation, partnership did not develop.
We identified four themes assessing the capacity building approach (Table 3).
Table 3.
Illustrative quotes supporting each major theme.
| Major themes | Illustrative quotes* |
|---|---|
| Personal and interpersonal motivators contributed to partnership development and resiliency | “She said HIV is her mission and I knew we’d hit it off.” (Community 3) |
| “I was looking for a new project that sparked me and this came along, and this just seemed like a really important area. I got really excited …” (Faculty 1) | |
| “The community leaders and members think the research topic is relevant and worth discovering. With both researchers and community leaders and members coming together to do the research, the hope is to create services that will benefit the community someday down the road.” (Community 3) | |
| “We both sort of had a passion for this topic, so it was something that we could really both commit to fully… And it’s an area that fits with my research area.” (Faculty 4) | |
| Partners took on responsibilities that used their strengths | “We all value our expertise, the researcher’s experience in research and our expertise in our own community…. I trust her experience and I like her willingness to work with us, who have little research experience. Our research partner recognizes the importance of our community expertise and involvement.” (Community 8) |
| “It was pretty clear early on that he [my community partner] would be in charge of bringing together the community side of it…. [T]hose roles were clear from the beginning, and that he was going to be able to take care of creating any connections we needed.” (Faculty 4) | |
| “In writing the proposal, [faculty partner] did most of the work. I would like to gain experience in writing research proposals, but there was miscommunication about our role in terms of writing the proposal. I hope next time we will share the responsibility.” (Community 1) | |
| “What is the best way to do that? That deferring is a natural part of a project when we have distinct areas of expertise. So I just worried that I was being domineering before, but she now feels comfortable saying what she thinks will work.” (Faculty 6) | |
| Partners grappled with communication, decision making, and power dynamics | “I felt comfortable with them in making decisions. At first, we spent time getting to know each other and our styles, but it progressed quickly into a good partnership. I did not have to compromise my values. I don’t think they did either.” (Faculty 5) |
| “Among the three of us, we talked about our roles, labeled our roles, and wrote how we envisioned this project…We agreed that we could change roles and also facilitate.” (Community 3) | |
| “(Decision making) was a challenge I faced. I was the referee [because] my partners had two mind frames… So I was dealing with Discovery Channel [academic partner] and Soap Opera [agency partner]. [But] the communication gap slowly came together.” (Community 2) | |
| “I would have liked to have more meetings in person instead of communicating via email.” (Community 9) | |
| “Initially, I think I was intimidated by the entire process, hence not voicing as much as I should have. … I am accustomed to being told what to do in these types of situations; not making the decisions so changing the mentality was difficult at first.” (Community 7) | |
| Community–university infrastructure was essential to partnership development and project progress | Funding: |
| “I definitely think creating opportunity by making funds available for community leaders/members to participate in any research area is worth the cost.” (Community 3) | |
| Training: | |
| “Having the CBPR training helped me know what kinds of things might be problematic … learning about typical areas that trip partnerships up.” (Faculty 5) | |
| “[Also, the importance of] understanding different cultures: academic and community. It’s important to make us more conscious (of both). It is not just them working with us, it’s us working with them. I have a part in making the partnership work, so it’s good for me to know about the University.” (Community 7) | |
| “I think that including more about how to write the initial research proposal could have been more useful. I had to rely on my partner’s expertise … because I lacked the experience.” (Community 9) | |
| Community Scholar support: | |
| “Everybody sharing their experiences made me feel I was not the only one going through that. And we could struggle together and learn from each other.” (Community 1) | |
| Partnership Facilitation: | |
| “That … facilitation session was helpful because I think it was at a time when we were a little bit stuck, and so just having an outside set of ears to help us process a little bit was really useful.” (Faculty 4) | |
| “I thought the program was run nicely by the leadership. It wasn’t top‐down. They allowed us to express our opinions and take ownership in the group as well. It gave us an example about how our partnership with the researcher should look like.” (Community 7) | |
| “Having an initial meeting with everyone involved‐ agency, university, PIR and myself would have been helpful.” (Community 5) |
*Community indicates community scholar and identification number. Faculty indicates faculty partner and identification number.
(1) Personal and interpersonal motivators contributed to partnership development and resiliency:“Motivators” brought partners together initially and helped partnerships be resilient through challenges.
Initially, faculty considered opportunity costs of engaging in new CBPR partnerships and agreed to participate when the project contributed to their larger professional development, whether in area of research, or interest in a specific community, or a desire to learn about CBPR (Table 3). Community scholars’ main drivers were their commitment to the research topic and desire for long‐term health benefits for their communities. For some scholars, participation in research supported their professional goals of obtaining advanced education or using past training.
The primary motivators for ongoing involvement for both faculty and community were commitments to partners, the health topic, communities, and the funder. For community scholars, an additional motivator was the sense of accountability to each other, which was reinforced during monthly meetings.
(2) Partners took on responsibilities that used their strengths: Qualitative data identified variation in partner division of responsibility for research tasks (Table 3). Partners described an often unspoken process of dividing tasks under the pressure of deadlines. Faculty struggled with when to take responsibility for aspects of the project in their area of expertise and when to divide the labor. Many community scholars described a lack of confidence in their abilities to contribute to tasks such as proposal writing and submission of IRB applications. Nonetheless, some of them, particularly those with professional aspirations in health promotion, desired a more active role and mentorship to develop their skills in these areas.
Quantitative results indicated that partners were in agreement regarding level of involvement in four research process tasks (identification of: topic area, question, dissemination plan, and determining data ownership). In other areas (budget and proposal writing) community scholars felt they were sharing research tasks equally, although most faculty perceived they were carrying a larger responsibility.
Overall, community scholars and faculty ranked the results of negotiations around the research processes as successful, with choice of research topic viewed most positively (Table 4, 2nd panel). Academics consistently rated success across quantitative domains higher at both time periods, though perceptions of success were somewhat less positive for both partners over time as the challenges of implementing research projects emerged.
Table 4.
Partner contribution to research and partnership processes and partner ratings of success.
| Time since completion of trainings | Predominant contribution (faculty, community, or equal)* | Mean ratings of success (poor to excellent)† | ||||||
|---|---|---|---|---|---|---|---|---|
| Community scholars | Faculty scholars | Community scholars | Faculty scholars | |||||
| 3 months (n = 9) | 12 months (n = 7) | 3 months (n = 6) | 12 months (n = 6) | 3 months (n = 9) | 12 months (n = 7) | 3 months (n = 6) | 12 months (n = 6) | |
| Research processes | ||||||||
| Identify research area | CS | CS | CS | CS | 4.2 | 3.6 | 4.3 | 4.5 |
| Identify research question | EQ | EQ | EQ | EQ | 3.7 | 3.3 | 4.3 | 4.0 |
| Identify methods | EQ | FAC | FAC | FAC | 3.7 | 3.4 | 4.5 | 4.2 |
| Identify analysis approach | EQ | FAC | FAC | FAC | 3.8 | 3.0 | 4.4 | 3.8 |
| Identify dissemination plan | EQ | EQ | EQ | EQ | 3.3 | 3.0 | 3.6 | 3.4 |
| Determine data ownership | EQ | EQ | EQ | EQ | 3.9 | 3.2 | 4.0 | 3.0 |
| Determine initial budget | EQ | EQ | FAC | FAC | 3.9 | 3.4 | 4.0 | 3.5 |
| Proposal writing | EQ | EQ | FAC | FAC | 3.7 | 3.0 | 4.0 | 3.8 |
| Partnership processes | ||||||||
| Decision making approach | EQ | EQ | EQ | EQ | 3.4 | 3.4 | 4.0 | 3.2 |
| Communicating goals | EQ | EQ | EQ | EQ | 3.6 | 3.4 | 3.8 | 3.2 |
| Negotiating differences | EQ | EQ | EQ | EQ | 3.8 | 3.4 | 4.3 | 3.5 |
As indicated below, cut points for the 5‐point Likert scales divided into equal intervals can be interpreted as follows:
*”FAC” indicates faculty dominated (score 1.0–2.59), ‘‘EQ” indicates equal contribution (score 2.6–3.39), and “CS” indicates community scholar dominated (score 3.4–5.0).
†There are no responses in the fair or poor categories (1.0–2.59); mean responses between 2.6 and 3.39 are good; 3.4–4.19 are very good; and 4.2–5.0 are excellent.
(3) Partners grappled with communication, decision‐making, and power dynamics: Qualitative results suggested that partners used direct communication and were explicit about their priorities and decision‐making processes. Partners reported discussing decision‐making options, universally agreeing on a consensus style. Faculty and community scholars reported egalitarian processes in terms of decision making, communicating, and negotiating. Both groups rated these processes as successful (Table 4).
All partners reported they could speak directly with their partner and felt that their opinions were considered and respected (Table 5). Generally, academics were more positive about the quality of partnership processes than community scholars. On average, both partners agreed or strongly agreed with the seven statements about the quality of their partnerships.
Table 5.
Summary of quantitative assessment of relationship processes.
| Time since completion of trainings | Community scholars | Faculty scholars | ||
|---|---|---|---|---|
| 3 months (n = 9) | 12 months (n = 7) | 3 months (n = 6) | 12 months (n = 6) | |
| Talk openly honestly | 3.56 | 3.29 | 3.33 | 3.50 |
| Comfortable expressing point of view | 3.44 | 3.14 | 3.67 | 3.17 |
| Comfortable bringing up new ideas | 3.56 | 3.14 | 3.67 | 3.67 |
| Opinion listened to and considered | 3.33 | 3.14 | 4.00 | 3.83 |
| Feel ownership in partnership | 3.44 | 3.29 | 3.33 | 3.67 |
| Partnership can positively affect community | 3.33 | 3.29 | 3.50 | 3.50 |
| Partnership increased knowledge and understanding | 3.44 | 3.14 | 3.83 | 3.67 |
Cut points for the 4‐point Likert scales divided into equal intervals can be interpreted as follows: there are no responses in the disagree or strongly disagree categories (score 1.0–2.49); mean responses between 2.5 and 3.24 are agree; and mean response between 3.25and 4.0 are strongly agree (represented in bold).
Despite good communication, two challenges were described. First, several community scholars did not communicate about personal life circumstances, which ultimately affected the momentum of the projects. Second, some community scholars felt uncomfortable expressing their needs or priorities to their faculty partners.
In some cases power and communication challenges arose between community scholars collaborating on a single project, or between community scholars and their collaborating community agencies. Community scholars recommended that we develop CBPR training for community agencies as a means to address these issues.
(4) Community–university infrastructure was essential to partnership development and project progress: Four components of the infrastructure supporting these partnerships were essential for partnership development and success: (1) training, (2) community scholars’ stipends, (3) seed funding for research projects, and (4) support for partnership development (Table 3).
Faculty ranked the trainings as good and community scholars as very good in preparing them for their partnerships. Faculty reported using the communication training and the general introduction to CBPR. Community scholars identified preparation for partnering with faculty and learning about research processes as helpful. Reflecting their desire for skill building, a number of community scholars wanted more training on research methods such as focus group facilitation, grant writing, and IRB applications.
Funding was key. The small monthly stipend for community scholars supported their time, and fostered commitment to the project. The availability of seed funding for projects proved to be essential even before partners received grants, as having a firm deadline pushed partnership activity. Indeed, the three nonfunded partnerships did not move forward until a year later when subsequent funding proposals were due. Overall success ratings were higher for funded than nonfunded projects.
All partners reported positive experiences with the matching process, and identified partnership facilitation and the opportunity for troubleshooting with the research team as helpful. In addition, faculty and particularly community scholars identified the community organizer as an important bridging person who could answer questions, solve problems, and provide support.
Discussion
Given the potential of CBPR to contribute to improved translational science and reduction of health disparities, it is important to understand how best to increase capacity for successful partnerships between academic researchers and community members. Results of this PIR program indicate that CBPR partnerships may be supported from nascency through an approach that focuses on providing participatory research training, funding opportunities, and facilitation of partnership matching and development.
In only 15 months, six partnerships were developed between nine community scholars and six academicians; and four projects were funded. Two elements portray lack of complete success: one partnership was never formed between the 10th community scholar and a faculty member, and three community scholars left the program because of personal life events that interfered with their ability to fulfill their commitments to their partnerships.
Both community and university partners reported high levels of trust, strong communication, and positive reactions to participation in CBPR. In general, the mixed–method analysis revealed that partners were appropriately matched so that priorities and needs were met on both sides of the partnerships; training was essential, particularly around communication to deal with inevitable conflicts or differences of opinion; division of tasks between partners required proactive discussion; and infrastructure such as training, support, and funding contributed to project success.
CBPR theory stresses an egalitarian process of colearning, which assumes that most tasks should be divided equally. In this project, partners describe equal responsibility in many research domains, but not in all; in several areas, one partner dominated as their strengths dictated. Although partners generally found this division of labor acceptable, improved commitment to capacity building and attention to communication, and power dynamics might have alleviated uncertainty about tasks and responsibilities as well as disappointment from a few community scholars at not being mentored more in research processes.
Unlike other CBPR training programs, we chose to train community and researchers separately for several reasons. First, the community scholars needed basic research training. Second, community members benefited from forming a social support group that helped them cope with challenges. The strength of this attachment is reflected in the fact that the community scholars created an ongoing CBPR project under the auspices of the community clinic partner. 19
An unanswered question is whether the amount of training was adequate to prepare partners for CBPR collaboration. Several community scholars reported anxiety regarding their knowledge of research and ability to contribute; however, given that this was the first research experience for most of them it is unlikely that more training would have relieved their concern. Faculty did not identify a need for additional training; however it is possible that community partners’ slightly lower ratings of partnership success and research processes compared to those of faculty members signify that faculty were not egalitarian partners and thus that the 6 hours of training was inadequate to prepare faculty for partnership.
Trainings for both community scholars and faculty stressed the importance of sound and explicit communication. Results suggest that future training should address how early communication about personal life events may improve planning and lessen the impact of partner changes on the project. Nonetheless, funded partnerships moved forward with involvement from another community scholar or the community organization representative.
Study results reinforce observations in the literature that infrastructure and financial support are important to foster community involvement in research. 20 , 21 Without the grant funding that supported community involvement in training, and the availability of a university funding mechanism to seed the projects, it is unlikely that the partnerships would have solidified. Additional key infrastructure components included facilitation of partnership development, and a community‐based bridging person who was available for troubleshooting.
There are limitations to this study. First, as a small convenient sample, the results may not be generalizable to other communities or universities. Second, the research team both delivered the trainings and facilitation, and evaluated the program. The lack of anonymity in the evaluation process and relationship between the research team and participants could have contributed to participants providing socially desirable responses. This likelihood was decreased by our mixed–methods approach.
In sum, this educational and facilitation program to support partnership building may guide other programs to increase capacity for CBPR with communities and research institutions. Improved collaboration may in turn improve the translational research process and ultimately address health disparities.
Acknowledgment
This project was funded by the National Institutes of Health, NIDA, grant number: 1R03DA0266632–01.
References
- 1. Macaulay AC, Freeman WL, Gibson N, McCabe ML, Robbins CM, Twohig PL. Responsible Research with Communities: Participatory Reserach in Primary Care, 1998. http://www.napcrg.org/responsibleresearch.pdf. Accessed September 28, 2010.
- 2. Leung MW, Yen IH, Minkler M. Community based participatory research: a promising approach for increasing epidemiology’s relevance in the 21st century. Int J Epidemiol. 2004; 33(3): 499–506. [DOI] [PubMed] [Google Scholar]
- 3. Minkler M, Wallerstein N. Introduction to community based participatory research In: Minkler M, Wallerstein N, eds.Community Based Participatory Research for Health. 1st edn. San Francisco , CA : John Wiley & Sons; 2003: 1–27. [Google Scholar]
- 4. Horowitz CR, Robinson M, Seifer S. Community‐based participatory research from the margin to the mainstream: are researchers prepared? Circulation. 2009; 119(19): 2633–2642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wallerstein N, Duran B. Community‐based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health.2010; 100(Suppl. 1): S40–S46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Schmittdiel JA, Grumbach K, Selby JV. System‐based participatory research in health care: an approach for sustainable translational research and quality improvement. Ann Fam Med.2010; 8(3): 256–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dankwa‐Mullan I, Rhee KB, Williams K, Sanchez I, Sy FS, Stinson N Jr, Ruffin J. The science of eliminating health disparities: summary and analysis of the NIH summit recommendations. Am J Public Health.2010; 100(Suppl. 1): S12–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hood NE, Brewer T, Jackson R, Wewers ME. Survey of community engagement in NIH‐funded research. Clin Transl Sci. 2010; 3(1): 19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Israel B, Schulz A, Parker E, Becker AB, Allen A, Guzman JR. Critical issues in developing and following CBPR principles In: Minkler M, Wallerstein N, eds.Community‐Based Participatory Research for Health: From Process to Outcomes. 2nd edn. San Francisco , CA : Jossey‐Bass; 2008:47–66. [Google Scholar]
- 10. Jones L, Wells K. Strategies for academic and clinician engagement in community‐participatory partnered research. JAMA. 2007; 297(4): 407–410. [DOI] [PubMed] [Google Scholar]
- 11. Wallerstein N, Oetzel J, Duran B, Tafoya G, Belone L, Rae R. What predicts outcomes in CBPR?In: Minkler M, Wallerstein N, eds. Community‐Based Participatory Research for Health: From Process to Outcomes. 2nd edn. San Francisco , CA : Jossey‐Bass; 2008:371–388. [Google Scholar]
- 12. Seifer SD, Calleson DC. Health professional faculty perspectives on community‐based research: implications for policy and practice. J Interprof Care. 2004; 18(4): 416–427. [DOI] [PubMed] [Google Scholar]
- 13. Wallerstein N, Duran, B , Minkler, M Foley, K . Developing and maintaining partnerships with communities In: Israel BA, Eng E, Schulz A, Parker E, eds.Methods in Community‐Based Participatory Research for Health. 1st edn. San Francisco , CA : John Wiley & Sons; 2005: 31–51. [Google Scholar]
- 14. Allen ML, Culhane‐Pera KA, Pergament SL, Call KT. Facilitating research faculty participation in CBPR: development of a model based on key informant interviews. Clin Transl Sci. 2010; 3(5): 233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Allen ML, Culhane‐Pera KA, Call KT, Pergament SL. Partners in research: curricula to prepare community and faculty for CBPR partnerships, 2011. Available at http://ces4health.info/find‐products/view‐product.aspx?code=T63W5WBC. Accessed November 15, 2011.
- 16. Israel BA, Lantz PM, McGranaghan RJ, Kerr DL, Guzman JR. Documentation and evaluation of CBPR partnerships: in‐depth interview and closed‐ended questionnaires In: Israel BA, Eng E, Schulz A, Parker E, eds.Methods in Community‐Based Participatory Research for Health. 1st edn. San Francisco , CA : John Wiley & Sons; 2005: 255–278. [Google Scholar]
- 17. Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Method Approaches. 2nd edn Thousand Oaks , CA : Sage; 2003. [Google Scholar]
- 18. Crabtree BF, Miller WL. Clinical research: a multimethod typology and qualitative roadmap In: Crabtree BF, Miller WL, eds.Doing Qualitative Research (Research Methods for Primary Care). 2nd edn. Thousand Oaks , CA : Sage; 1999: 3–32. [Google Scholar]
- 19. Culhane‐Pera KA, Allen M, Pergament SL, Call K, Adawe A, de la Torre R, Hang M, Jama F, Navas M, Ortega L, et al. Improving health through community‐based participatory action research. Giving immigrants and refugees a voice. Minn Med. 2010; 93(4): 54–57. [PMC free article] [PubMed] [Google Scholar]
- 20. Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community‐based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998; 19: 173–202. [DOI] [PubMed] [Google Scholar]
- 21. Ahmed SM, Beck B, Maurana CA, Newton G. Overcoming barriers to effective community‐based participatory research in US medical schools. Educ Health (Abingdon). 2004; 17(2): 141–151. [DOI] [PubMed] [Google Scholar]


