ABSTRACT
Until recently, Ebola virus (EBOV) was a rarely encountered human pathogen that caused disease among small populations with extraordinarily high lethality. At the end of 2013, EBOV initiated an unprecedented disease outbreak in West Africa that is still ongoing and has already caused thousands of deaths. Recent studies revealed the genomic changes this particular EBOV variant undergoes over time during human-to-human transmission. Here we highlight the genomic changes that might negatively impact the efficacy of currently available EBOV sequence-based candidate therapeutics, such as small interfering RNAs (siRNAs), phosphorodiamidate morpholino oligomers (PMOs), and antibodies. Ten of the observed mutations modify the sequence of the binding sites of monoclonal antibody (MAb) 13F6, MAb 1H3, MAb 6D8, MAb 13C6, and siRNA EK-1, VP24, and VP35 targets and might influence the binding efficacy of the sequence-based therapeutics, suggesting that their efficacy should be reevaluated against the currently circulating strain.
Observation
As the Ebola virus disease (EVD) outbreak in West Africa of 2013 continues (1), public health and emerging infectious disease officers have declared a state of emergency (2). As of 8 January 2015, the mean lethality in this outbreak, caused by Ebola virus (EBOV), reached 39.4% (http://www.who.int/csr/don/archive/disease/ebola/en/). Another study, utilizing different methods, calculated the real case fatality rate at 70% (3). The uncontrolled situation in the outbreak area, now spread over six West African countries, and the risk of further EBOV exportation beyond the African continent prompted the World Health Organization to adopt emergency containment measures. Among them is the testing of as-yet-unapproved medical countermeasures in the affected human population (4–7).
At the moment, there are three treatment modalities directly based on the EBOV genomic sequence that have been explored for postexposure treatment of EVD with encouraging results in nonhuman-primate models: small interfering RNAs (siRNAs) (8) and phosphorodiamidate morpholino oligomers (PMOs) (9) targeting EBOV genome L, VP24, and/or VP35 gene transcripts and passive immunotherapy based on antibodies or antibody cocktails targeting EBOV epitopes (10–14). Briefly, they inhibit viral replication by either targeting viral transcripts for degradation (siRNA), by blocking translation (PMO), or by acutely neutralizing the virus to allow the host to mount an effective immune response against the pathogen (passive immunotherapy). The binding sites for antisense therapeutics based on siRNAs and PMOs are described in references 8 and 15, respectively. All of them were designed specifically against sequences derived from the EBOV variant causing an EVD outbreak around Yambuku, Zaire (present-day Democratic Republic of the Congo), in 1976 (Ebola virus/H.sapiens-tc/COD/1976/Yambuku-Mayinga; short name, EBOV/Yam-May; RefSeq no. nc_002549 [16]). All monoclonal antibodies used for passive immunotherapy were generated against the glycoprotein of the EBOV variant causing an EVD outbreak in Kikwit, Zaire, in 1995 (Ebola virus/H.sapiens-tc/COD/1995/Kikwit-9510621; short name, EBOV/Kik-9510621; GenBank no. ay354458 [17]). Traditional peptide-based epitope mapping allowed the differentiation of conformational and linear epitopes. Coimmunoprecipitation assays were performed against broad domains of the glycoprotein to identify binding targets of conformational antibodies (18, 19). Table 1 summarizes publicly available information (8–12, 15, 18, 19) for the three treatment types, including therapeutic targeting and efficacy in postinoculation treatment of experimental EBOV infection in animals. All postexposure studies evaluating these therapeutics were completed using EBOV/Kik-9510621 as the challenge virus.
TABLE 1 .
Summary of binding and postexposure efficacy data available for EBOV therapeuticsa
| Candidate therapeutic component | Treatment modality | Therapeutic(s) | Nucleotide position based on GenBank/RefSeq entryb | Amino acid residues of target protein | Target gene | Treatment time p.i. | Treatment success (% survival range) | Reference(s) |
|---|---|---|---|---|---|---|---|---|
| EK-1-mod | siRNA | Tekmira | 17,396–17,418 | NA | L | 30 min to 6 days | 66.7–100c | 8 |
| VP24-1160-mod | siRNA | Tekmira | 11,043–11,065 | NA | VP24 | 30 min to 6 days | 66.7–100c | 8 |
| VP35-855-mod | siRNA | Tekmira | 3884–3906 | NA | VP35 | 30 min to 6 days | 66.7–100c | 8 |
| 1H3 Mab | Passive immunization | ZMAB | 6039–6508 | 1–157 | GP | 3–9 days | 50–100d | 10, 18 |
| 2G4 Mab | Passive immunization | ZMAPP, ZMAB | 7540–8039 | 501–676 | GP | 3–9 days | 50–100d,e | 10, 12, 18 |
| 4G7 Mab | Passive immunization | ZMAPP, ZMAB | 7414–7542 | 459–501 | GP | 3–9 days, 5 days | 50–100d,e | 10, 12, 18 |
| 13C6 Mab | Passive immunization | MB-003, ZMAPP | 6039–7542 | 1–501 | GPf | 1–2 days, 5 days | 66.7–100e | 11, 12, 18, 19 |
| 6D8 Mab | Passive immunization | MB-003 | 7204–7254 | 389–405 | GP | 1–2 days | 66.7 | 11, 19 |
| 13F6 Mab | Passive immunization | MB-003 | 7240–7290 | 401–417 | GP | 1–2 days | 66.7 | 11, 19 |
| AVI-7537 | PMO | AVI-6002 | 10,331–10,349 | NA | VP24 | 30–60 min | 60 | 9, 15 |
| AVI-7539 | PMO | AVI-6002 | 3133–3152 | NA | VP35 | 30–60 min | 60 | 9, 15 |
MAb, monoclonal antibody; NA, not applicable; p.i., postinoculation; PMO, phosphorodiamidate morpholino oligomers; siRNA, small interfering RNA. Recognition sequences for PMO and siRNA are listed in the supplemental methods.
siRNA positions include both sense and antisense oligonucleotide positions. Mutations specific to each are designated in Fig. 1.
Survival range is dependent on dosing.
Survival range is dependent on addition of Ad-IFN (interferon co-treatment) to treatment 1 day p.i.
Survival range is dependent on formulation.
Cross-reacts with TAFV (Tai Forest virus) and SUDV (Sudan virus) GP.
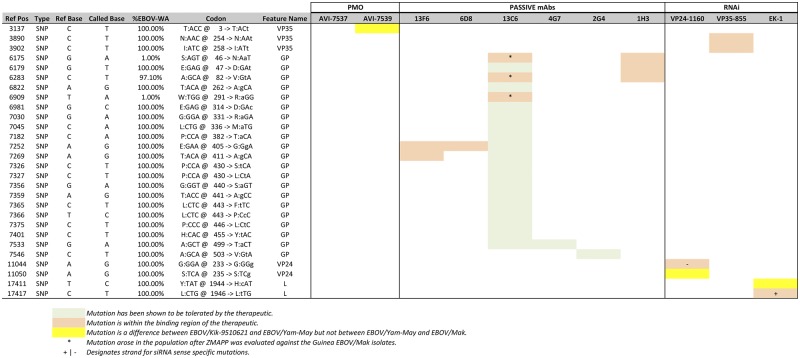
For this study, we reviewed all publicly available genomic information for the Ebola virus Makona variant (EBOV/Mak) causing the 2013–2014 West African outbreak (102 genomic sequences) (1, 20, 21) and assessed the potential of the observed EBOV/Mak genetic drift relative to EBOV/Yam-May and EBOV/Kik-9510621 to affect each therapeutic. When EBOV/Mak was compared against EBOV/Kik-9510621, a total of 640 (3.38% of the genome) single-nucleotide polymorphisms (SNPs) were identified (327 synonymous, 76 nonsynonymous, and 237 noncoding), whereas when it was compared against EBOV/Yam-May, a total of 603 (3.18% of the genome) SNPs were identified (297 synonymous, 80 nonsynonymous and 226 noncoding). Four mutations are located in the published binding region of the siRNA- or PMO-based therapeutics, and 21 induce nonsynonymous changes to epitopes recognized by monoclonal antibodies in passive immunotherapy cocktails. Figure 1 combines an SNP table with a heat map that outlines the potential of each SNP to affect the efficacy of available therapeutics. The column designated “%EBOV-WA” stratifies changes by the number of West African sequences that support each mutation. Changes that are present in all sequences obtained from West Africa are considered “interoutbreak”; changes that are observed in only some sequences from the West African outbreak are considered “intraoutbreak” (i.e., EBOV-WA represents <100% of the population at the specified position). Of the 28 sites observed within binding regions, 3 SNPs (21.4%) evolved during the 2013–2014 EVD outbreak (intraoutbreak), whereas 22 SNPs (78.6%) evolved prior to the outbreak (interoutbreak). None of the specific SNPs presented here have been previously associated with EBOV resistance to any therapeutic; however, there is a general lack of information surrounding the appearance of viral resistance to EBOV therapeutics compared to viral systems like influenza virus and HIV due to the limitations of gain-of-function experiments. Eighteen of the changes have been demonstrated to be tolerated by the ZMAPP cocktail (13C6, 4G7, and 2G4), which demonstrated an increased binding affinity to the EBOV/Mak glycoprotein sequence (12), thus minimizing the potential impact of the mutations. Nevertheless, some of the intraoutbreak changes observed in this region still need to be evaluated. The changes observed in the West African sequences that are already represented in EBOV/Yam-May are also listed as tolerated (yellow), as the therapeutics discussed here have had testing completed with both viruses or mouse/guinea pig-adapted version of the virus and are not different between EBOV/Yam-May and EBOV/Mak (19, 22–24). The other ten mutations, affecting the binding sites of MAb 13F6, MAb 6D8 (part of MB-003), MAb 13C6 (part of MB-003 and ZMAPP), MAb 1H3 (part of ZMAB), and siRNA EK-1, VP24, and VP35 targets, might influence the binding efficacy of the sequence-based therapeutics; their efficacy should be tested against the currently circulating strain (Fig. 2).
FIG 1 .
Mutation analysis of candidate therapeutic binding sites. An SNP table is combined with a heat map based on three categories: (i) mutation shown to be tolerated by the therapeutic (10), (ii) mutations that are within the binding region of the therapeutic but have not been tested (8–12, 15, 18, 19), and (iii) tolerated diversity between development strains. %EBOV-WA, percentage of genomes containing a change in the West African (WA) sequences of 2014 from EBOV/Kik-9510621.
FIG 2 .
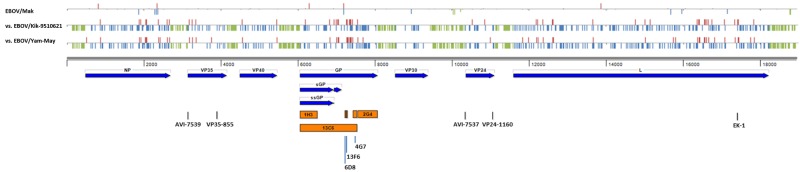
EBOV therapeutic map. Each of the therapeutics was mapped onto the genome of EBOV/Kik-9510621 according to published binding information. Blue arrows represent the nine open reading frames conserved among all Ebola viruses. A graphic representation of the SNPs is above the genomic position scale. Red vertical bars denote nonsynonymous mutations, blue vertical bars represent synonymous mutations, and green vertical bars represent noncoding mutations.
Closing this gap might be critical to ongoing efforts to control the outbreak. A robust genomics screening, pre- and post-treatment, would allow clinicians to make informed choices in treatment regimen as well as clarify what signs of viral resistant development should be tracked.
Our risk assessment is not without caveats. (i) This analysis is limited to the binding regions of candidate therapeutics, yet deleterious changes may not be limited to these regions. (ii) Changes in the binding regions may be well tolerated and not influence therapeutic efficacy. (iii) As EBOV/Mak genomes from humans treated with these therapeutics have not yet been determined, conclusions about intrahost selection pressure cannot be made at this stage. It is also important to note that some of the therapeutics have been deliberately designed to be tolerant to possible target mutation: for instance, siRNAs and PMOs were targeted to areas of higher conservation where mutation was thought to be unlikely (based mainly on conservation on all available EBOV sequences at the time of design), and monoclonal antibody cocktails were designed to include several antibodies that bind to distinct regions of the EBOV glycoprotein (18, 19). This multitarget development may ensure that multiple genetic bottlenecks are present to minimize the impact of individual mutations of an evolving EBOV variant.
In summary, the information presented here offers a concise evaluation of the potential impact of the evolutionary drift of Ebola virus Makona in the development of sequence-based therapeutics based on sequence information available in September 2014. Given the ongoing continued person-to-person transmission, it is imperative that more current isolates be sequenced and evaluated in a similar manner.
SUPPLEMENTAL MATERIAL
Supplemental materials and methods. Download
ACKNOWLEDGMENTS
This work was supported by Defense Threat Reduction Agency. J.H.K. performed this work as an employee of Tunnell Government Services, Inc., a subcontractor to Battelle Memorial Institute under its prime contract with NIAID, under contract no. HHSN272200700016I. This material is based upon work supported by the National Science Foundation Graduate research fellowship under grant no. DGE 1144152.
The content of this publication does not necessarily reflect the views or policies of the U.S. Department of the Army, the U.S. Department of Defense, or the U.S. Department of Health and Human Services or of the institutions and companies with which the authors are affiliated.
Footnotes
Citation Kugelman JR, Sanchez-Lockhart M, Andersen KG, Gire S, Park DJ, Sealfon R, Lin AE, Wohl S, Sabeti PC, Kuhn JH, Palacios GF. 2015. Evaluation of the potential impact of Ebola virus genomic drift on the efficacy of sequence-based candidate therapeutics. mBio 6(1):e02227-14. doi:10.1128/mBio.02227-14.
REFERENCES
- 1.Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keita S, De Clerck H, Tiffany A, Dominguez G, Loua M, Traore A, Kolie M, Malano ER, Heleze E, Bocquin A, Mely S, Raoul H, Caro V, Cadar D, Gabriel M, Pahlmann M, Tappe D, Schmidt-Chanasit J, Impouma B, Diallo AK, Formenty P, Van Herp M, Gunther S. 2014. Emergence of Zaire Ebola virus disease in Guinea—preliminary report. N Engl J Med 371:1418–1425. doi: 10.1056/NEJMoa1404505. [DOI] [PubMed] [Google Scholar]
- 2.Hawkes N. 2014. Ebola outbreak is a public health emergency of international concern, WHO warns. BMJ 349:g5089. doi: 10.1136/bmj.g5089. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Ebola Response Team 2014. Ebola virus disease in West Africa—the first 9 months of the epidemic and forward projections. N Engl J Med 371:1481–1495 doi: 10.1056/NEJMoa1411100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anonymous. 2014. Ethical considerations for use of unregistered interventions for Ebola virus disease (EVD). World Health Organization, Geneva, Switzerland. [Google Scholar]
- 5.Gulland A. 2014. First Ebola treatment is approved by WHO. BMJ 349:g5539. doi: 10.1136/bmj.g5539. [DOI] [PubMed] [Google Scholar]
- 6.Shuchman M. 2014. WHO enters new terrain in Ebola research. CMAJ 186:E527–E528 doi: 10.1503/cmaj.109-4893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayburn A. 2014. WHO gives go ahead for experimental treatments to be used in Ebola outbreak. BMJ 349:g5161. doi: 10.1136/bmj.g5161. [DOI] [PubMed] [Google Scholar]
- 8.Geisbert TW, Lee AC, Robbins M, Geisbert JB, Honko AN, Sood V, Johnson JC, de Jong S, Tavakoli I, Judge A, Hensley LE, Maclachlan I. 2010. Postexposure protection of non-human primates against a lethal Ebola virus challenge with RNA interference: a proof-of-concept study. Lancet 375:1896–1905. doi: 10.1016/S0140-6736(10)60357-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Warren TK, Warfield KL, Wells J, Swenson DL, Donner KS, Van Tongeren SA, Garza NL, Dong L, Mourich DV, Crumley S, Nichols DK, Iversen PL, Bavari S. 2010. Advanced antisense therapies for postexposure protection against lethal filovirus infections. Nat Med 16:991–994. doi: 10.1038/nm.2202. [DOI] [PubMed] [Google Scholar]
- 10.Qiu X, Audet J, Wong G, Fernando L, Bello A, Pillet S, Alimonti JB, Kobinger GP. 2013. Sustained protection against Ebola virus infection following treatment of infected nonhuman primates with ZMAb. Sci Rep 3:3365. doi: 10.1038/srep03365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pettitt J, Zeitlin L, Kim DH, Working C, Johnson JC, Bohorov O, Bratcher B, Hiatt E, Hume SD, Johnson AK, Morton J, Pauly MH, Whaley KJ, Ingram MF, Zovanyi A, Heinrich M, Piper A, Zelko J, Olinger GG. 2013. Therapeutic intervention of Ebola virus infection in rhesus macaques with the MB-003 monoclonal antibody cocktail. Sci Transl Med 5:199ra113. doi: 10.1126/scitranslmed.3006608. [DOI] [PubMed] [Google Scholar]
- 12.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, Johnson A, Morton J, Swope K, Bohorov O, Bohorova N, Goodman C, Kim D, Pauly MH, Velasco J, Pettitt J, Olinger GG, Whaley K, Xu B, Strong JE, Zeitlin L, Kobinger GP. 2014. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514:47–53 doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olinger GG Jr, Pettitt J, Kim D, Working C, Bohorov O, Bratcher B, Hiatt E, Hume SD, Johnson AK, Morton J, Pauly M, Whaley KJ, Lear CM, Biggins JE, Scully C, Hensley L, Zeitlin L. 2012. Delayed treatment of Ebola virus infection with plant-derived monoclonal antibodies provides protection in rhesus macaques. Proc Natl Acad Sci U S A 109:18030–18035. doi: 10.1073/pnas.1213709109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dye JM, Herbert AS, Kuehne AI, Barth JF, Muhammad MA, Zak SE, Ortiz RA, Prugar LI, Pratt WD. 2012. Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. Proc Natl Acad Sci U S A 109:5034–5039. doi: 10.1073/pnas.1200409109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heald AE, Iversen PL, Saoud JB, Sazani P, Charleston JS, Axtelle T, Wong M, Smith WB, Vutikullird A, Kaye E. 2014. Safety and pharmacokinetic profiles of Phosphorodiamidate morpholino oligomers with activity against Ebola virus and Marburg virus: results of two single-ascending dose studies. Antimicrob Agents Chemother 58:6639–6647. doi: 10.1128/AAC.03442-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuhn JH, Andersen KG, Bào Y, Bavari S, Becker S, Bennett RS, Bergman NH, Blinkova O, Bradfute S, Brister JR, Bukreyev A, Chandran K, Chepurnov AA, Davey RA, Dietzgen RG, Doggett NA, Dolnik O, Dye JM, Enterlein S, Fenimore PW, Formenty P, Freiberg AN, Garry RF, Garza NL, Gire SK, Gonzalez JP, Griffiths A, Happi CT, Hensley LE, Herbert AS, Hevey MC, Hoenen T, Honko AN, Ignatyev GM, Jahrling PB, Johnson JC, Johnson KM, Kindrachuk J, Klenk HD, Kobinger G, Kochel TJ, Lackemeyer MG, Leroy EM, Lever MS, Mühlberger E, Netesov SV, Olinger GG, Omilabu SA, Palacios G, Panchal RG. 2014. Filovirus RefSeq entries: evaluation and selection of filovirus type variants, type sequences, and names. Viruses 6:3663–3682. doi: 10.3390/v6093663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuhn JH, Bao Y, Bavari S, Becker S, Bradfute S, Brister JR, Bukreyev AA, Chandran K, Davey RA, Dolnik O, Dye JM, Enterlein S, Hensley LE, Honko AN, Jahrling PB, Johnson KM, Kobinger G, Leroy EM, Lever MS, Mühlberger E, Netesov SV, Olinger GG, Palacios G, Patterson JL, Paweska JT, Pitt L, Radoshitzky SR, Saphire EO, Smither SJ, Swanepoel R, Towner JS, van der Groen G, Volchkov VE, Wahl-Jensen V, Warren TK, Weidmann M, Nichol ST. 2013. Virus nomenclature below the species level: a standardized nomenclature for natural variants of viruses assigned to the family Filoviridae. Arch Virol 158:301–311. doi: 10.1007/s00705-012-1454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiu X, Alimonti JB, Melito PL, Fernando L, Ströher U, Jones SM. 2011. Characterization of Zaire ebolavirus glycoprotein-specific monoclonal antibodies. Clin Immunol 141:218–227. doi: 10.1016/j.clim.2011.08.008. [DOI] [PubMed] [Google Scholar]
- 19.Wilson JA, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn AL, Hart MK. 2000. Epitopes involved in antibody-mediated protection from Ebola virus. Science 287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 20.Stephen K, Gire AG, Andersen KG, Sealfon RSG, Park DJ, Kanneh L, Jalloh S, Momoh M, Fullah M, Dudas G, Wohl S, Moses LM, Yozwiak NL, Winnicki S, Matranga CB, Malboeuf CM, Qu J, Gladden AD, Schaffner SF, Yang X, Jiang P.-P, Nekoui M, Colubri A, Coomber RM, Fonnie M, Moigboi A, Gbakie M, Kamara FK, Tucker V, Konuwa E, Saffa S, Sellu J, Azziz Jalloh A, Kovoma A, Koninga J, Mustapha I, Kargbo K, Foday M, Yillah M, Kanneh F, Robert W, Massally JLB, Chapman SB, Bochicchio J, Murphy C, Nusbaum C, Young S, Birren BW, Grant DS, Scheiffelin JS, Lander ES, Happi C, Sahr M, Gnirke A, Rambaut A, Garry RF, Humarr Khan S, Pardis C, Sabeti PC. 2014. Genomic surveillance elucidates Ebola virus origin and transmission during the 2014 outbreak. Science 345:1369–1372. doi: 10.1126/science.1259657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kuhn JH, Andersen KG, Baize S, Bào Y, Bavari S, Berthet N, Blinkova O, Brister JR, Clawson AN, Fair J, Gabriel M, Garry RF, Gire SK, Goba A, Gonzalez JP, Günther S, Happi CT, Jahrling PB, Kapetshi J, Kobinger G, Kugelman JR, Leroy EM, Maganga GD, Mbala PK, Moses LM, Muyembe-Tamfum JJ, N’Faly M, Nichol ST, Omilabu SA, Palacios G, Park DJ, Paweska JT, Radoshitzky SR, Rossi CA, Sabeti PC, Schieffelin JS, Schoepp RJ, Sealfon R, Swanepoel R, Towner JS, Wada J, Wauquier N, Yozwiak NL, Formenty P. 2014. Nomenclature- and database-compatible names for the two Ebola virus variants that emerged in Guinea and the Democratic Republic of the Congo in 2014. Viruses 6:4760–4799. doi: 10.3390/v6114760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Towner JS, Paragas J, Dover JE, Gupta M, Goldsmith CS, Huggins JW, Nichol ST. 2005. Generation of eGFP expressing recombinant Zaire ebolavirus for analysis of early pathogenesis events and high-throughput antiviral drug screening. Virology 332:20–27. doi: 10.1016/j.virol.2004.10.048. [DOI] [PubMed] [Google Scholar]
- 23.Swenson DL, Warfield KL, Warren TK, Lovejoy C, Hassinger JN, Ruthel G, Blouch RE, Moulton HM, Weller DD, Iversen PL, Bavari S. 2009. Chemical modifications of antisense morpholino oligomers enhance their efficacy against Ebola virus infection. Antimicrob Agents Chemother 53:2089–2099. doi: 10.1128/AAC.00936-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Geisbert TW, Hensley LE, Kagan E, Yu EZ, Geisbert JB, Daddario-DiCaprio K, Fritz EA, Jahrling PB, McClintock K, Phelps JR, Lee AC, Judge A, Jeffs LB, MacLachlan I. 2006. Postexposure protection of guinea pigs against a lethal Ebola virus challenge is conferred by RNA interference. J Infect Dis 193:1650–1657. doi: 10.1086/504267. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental materials and methods. Download