Abstract
Aims: To evaluate the feasibility and effectiveness of a telemedicine system based on internet in the follow-up of patients with type 2 diabetes mellitus (T2DM). Methods: A prospective randomized telemedicine study with two parallel groups was designed. 114 patients diagnosed T2DM were randomly divided into telemedicine group and traditional face-to-face visit group as control. 57 cases were included for each group. 108 patients completed the trial, in which 53 cases in telemedicine group and 55 cases in control group. Patients in telemedicine group were taught to use telemedicine software to upload their blood glucose and other metabolic information at home at least every 2 weeks, and the researchers gave proper advices according to patients’ key behaviors. The telemedicine interval is 3 months. Results: Compared to control group, telemedicine group exhibited better HbA1c and fasting blood glucose controlling (P < 0.05). Moreover, telemedicine intervention decreased hypoglycemia risk (P = 0.044), and contributed to levels of HbA1c less than 7% which is the target of our study (P = 0.049). Conclusions: Telemedicine system can provide a tighter glycemic control for the treatment of T2DM patients, especially in cases with difficulties to access to the medical centre.
Keywords: Type 2 diabetes mellitus, telemedicine, management, HbA1c
Introduction
Diabetes mellitus (DM) is one of the most prevalent chronic diseases throughout the world and is considered among the most common illness in 21st century [1]. It is a leading cause of morbidity and mortality and a major contributor to health care cost [2,3]. Increases in HbA1c levels above the normal range in patients with diabetes are associated with progressive increases in morbidity and mortality due to micro- and macrovascular disease [4]. Intensive glycemic control can reduce microvascular complications in both type 1 and type 2 diabetes [5,6]. And treatment of patients with type 2 diabetes mellitus (T2DM) targeted HbA1c < 7.0% [7-9].
In the situation of T2DM in China, the morbidity is increasing rapidly. The epidemic investigation from Chinese Medical Association revealed that the morbidity of male adults over 20 years old reached 10.6%, and 8.8% for females [10]. The total morbidity is 9.7% or 92.4 million people suffered from diabetes mellitus and its complications. China becomes a super country of diabetes and bears big burden of society. However, management of diabetes has not been parallel to the huge population of diabetes. In China, people visit doctors randomly, and their glucose or other risk factors control cannot be known before they next time visit the doctors. Diabetes management requires frequent fingerstick glucose measurements, multiple intakes of oral hypoglycemic agents, daily injections of insulin, and frequent insulin dose adjustments. Appropriate and prompt management of episodes of hypoglycemia, hyperglycemia, and ketonuria may prevent emergency department visits, and hospitalizations. Thus, the traditional face-to-face visits have shortcomings. Telemedicine may be an effective method to facilitate the management of these patients and to provide diabetes education and training for patient’s them-selves and their family.
Telemedicine studies of diabetes till now are mainly focused on glucose monitoring and the communicating function of professionals and patients [11-16]. However, at the same time of intensive glycemic control, iatrogenic hypoglycemia (blood glucose ≤ 3.9 mmol/L, or 70 mg/dl) causes recurrent morbidity in many people with T2DM [17]. Hypoglycemia and fear of hypoglycemia remain major barriers of T2DM patients to achieve HbA1c targets. Reduction of risk factors and individualized treatment are key solutions for preventing incidence of extreme events. Besides the glucose, we suppose that some key behaviors including smoking, drinking, diet controlling and body excising may be essential for glycemic controlling, incidence of hypoglycemia and patients’ outcome. And in our randomized control trial, we did demonstrate that these key behaviors changes benefit HbA1c, fasting blood glucose, and more importantly reduce the risk of hypoglycemia. These results will highlight the necessary of behavior monitoring in diabetes management. The main objective of these systems is to provide a way to improve the quality of illness care through a closer communication between the patients and the professionals.
Materials and methods
Patients
A prospective randomized interventional study with two parallel groups was designed. All patients diagnosed as type 2 Diabetes according to WHO criteria in 1999 and referred to the First Affiliated Hospital of Jinan University from July 2012 to February 2013 were invited to participate in this study. Patients aged 18 to 75 years old who can manage glycemic meter at home and voluntarily participate in this trial were invited. Patients were excluded if they did not have an internet device as required for the home telemedicine system used. In this study, 114 participants signed written informed consent and 108 completed the study. The reasons patients did not complete the study are those they did not upload their glucose data or did not go back to outpatient at the end of the study after 3-month intervention. The study was approved by the Ethical Committee of our institution.
Sample size estimation
HbA1c is the main target of our observation. It is reported that 3 months intervention resulted in 1.7% decrease of HbA1c in telemedicine group and 0.7% decrease in control group [18]. In preliminary study, we treated 10 diabetes patients with telemedicine and the standard deviation is 1.72. Thus, according to formula: N = 2[(U+U)/] 2 + 1/4U2, = 1-2 = 1.7-0.7 = 1.0, = 1.72, we get N equals to 49. If the drop-out rate is 15%, cases for each group is 57, therefore, totally 114 cases should be investigated.
Telemedicine system
Diabetes Telemedicine System is a media between patients and professional staffs based on internet. It is developed by endocrine department and computer center of our hospital, targeting to meet the need of general diabetes management. In this system, patients enter their data of capillary glucose, blood pressures, body weight, etc. Staffs read and analyze the data, and then give guidance to the patients through internet, short messages, or telephone. In this study, staffs do not suggest a medication change but the key behaviors including cigarette smoking, drinking, dietary control, exciting, and glucose monitoring. As the supplementary communication means, professional staffs contact to participants through online communication, short message platform, mobile short message, and telephone when necessary.
Interventions
All participants enrolled their basic health and diabetes related information, including the height, body weight, blood pressure (BP), fasting blood glucose (FBG), HbA1c and plasma lipids. Participants in both groups attended a 30-60 min educational session for diabetes self-management and nutrition. Everyone received a pamphlet of diabetes management and a schedule of diabetes courses.
According to time sequence patients enrolled, participants were randomly divided into 2 groups by using random numbering method. In telemedicine group, patients were taught to use the telemedicine system and upload their data at home. Meanwhile, they were told the telephone number of outpatient department and they can contact to staff if they need a help. Or they may log on internet at home to view the indicated homepage for self-education. All the patients in telemedicine group were asked to upload their blood glucose and key behaviors (smoking, drinking, diet controlling and body exercise) at least once every 2 weeks. If they didn’t do so, researchers will find the reason through telephone or short messages. Researchers help participants to monitor blood glucose and solve diabetes-related problems in daily life through this system. Then the researchers analyze the data and provide proper guidance to their key behaviors, or ask the patient to attend outpatient for further treatment if necessary. In control group, without specific intervention, patients freely went to outpatient as usual when researchers collect the clinical information, including blood glucose, HbA1c, blood pressure, etc. All the participants of these two groups were asked a face-to-face visit in outpatient after 3 months (±1 month).
Statistical analysis
All data were analyzed by SPSS 13.0 software (SPSS, Chicago, IL). Representation of data was as follows: x̅ ± s, for normal distributed data; median (quartile range), for abnormal distribution data. Test was used for categorical data. Student t test and Mann-Whitney test were used to analyze quantitative data. A difference was considered statistically significant if the P value was < 0.05.
Results
Baseline patient characteristics
Baseline characteristics including body weight index (BMI), BP, FBG, HbA1c, and plasma lipids were similar in both groups (Table 1).
Table 1.
Basic metabolic information of all participants
| Control (n=55) | Telemedicine (n=53) | t | P | |
|---|---|---|---|---|
| BMI (kg/m2) | 23.64±3.01 | 24.72±3.38 | 1.76 | 0.082 |
| SBP (mmHg) | 131.93±12.29 | 128.55±14.34 | 1.32 | 0.191 |
| DBP (mmHg) | 76.89±8.09 | 79.38±9.53 | 1.46 | 0.146 |
| FBG (mmol/L) | 8.73±2.60 | 8.73±2.61 | 0 | 0.500 |
| HbA1c (%) | 8.22±1.58 | 8.44±1.58 | 0.73 | 0.468 |
| TC (mmol/L) | 5.23±1.31 | 4.99±1.21 | 1.01 | 0.316 |
| TG (mmol/L)# | 0.26±0.35 | 0.28±0.27 | 0.25 | 0.804 |
| LDL-C (mmol/L) | 2.89±1.13 | 2.75±0.93 | 0.74 | 0.460 |
| HDL-C (mmol/L) | 1.23±0.35 | 1.18±0.34 | 0.74 | 0.459 |
Abnormal distribution, data were logarithm linearized.
According to 2010 guidance, HbA1c less than 7% are defined as standard. We examined the basic HbA1c values of all 108 participants enrolled, in which only 21 patients (19.4%) reach the standard. In those who didn’t reach the standard, HbA1c of 15.7% patients is more than 10% (Figure 1). However, there is no significant difference of HbA1c between these two groups (Table 2).
Figure 1.
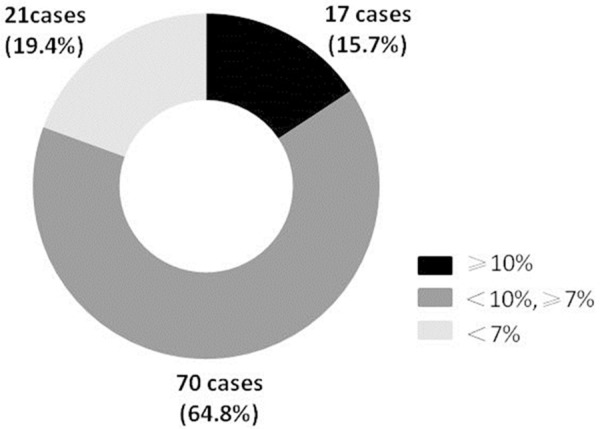
HbA1c values of all 108 participants.
Table 2.
Basic HbA1c levels
| HbA1c (%) | Control (n=55) | Telemedicine (n=53) | X2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| n (%) | n (%) | |||||
| <7 | 11 | 20 | 10 | 18.9 | 0.77 | 0.681 |
| ≥7 | 44 | 80 | 43 | 81.1 | ||
Metabolic parameter changes after telemedicine intervention
Three months later, we compared metabolic parameters within each group by paired t test as shown by Table 3. BP, FBG, HbA1c, TG and HDL-C of telemedicine group changed markedly as indicated in the Table. BMI, TC and LDL-C had no change. Because of the medication, in control group, patients also have attenuation in parameters except BMI, LDL-C and HDL-C. However, larger extents of BP, FBG, HbA1c and HDL-C changes are detected in telemedicine group than in control group, in which FBG and HbA1c had statistical significance (Table 4). The attenuation of TC and LDL-C was not better in telemedicine group than control (Figure 2).
Table 3.
Metabolic parameter changes within each group
| Control (n=55) | t | P | Telemedicine (n=53) | t | P | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before | After | Before | After | |||||
| BMI (kg/m2) | 23.64±3.01 | 23.75±2.93 | 1.02 | 0.314 | 24.72±3.38 | 24.72±3.36 | 0.02 | 0.987 |
| SBP (mmHg) | 131.9±12.29 | 128.95±12.08 | 2.19 | 0.033* | 128.55±14.34 | 124.53±12.32 | 3.01 | 0.004* |
| DBP (mmHg) | 76.89±8.09 | 75.05±7.18 | 2.17 | 0.034* | 79.38±9.53 | 77.13±8.46 | 2.97 | 0.005* |
| FBG (mmol/L) | 8.73±2.60 | 8.02±2.38 | 2.80 | 0.007* | 8.73±2.61 | 7.06±1.49 | 4.90 | <0.001* |
| HbA1c (%) | 8.22±1.58 | 7.60±1.57 | 3.58 | 0.001* | 8.44±1.58 | 6.84±1.20 | 7.88 | <0.001* |
| TC (mmol/L) | 5.23±1.31 | 4.70±0.84 | 3.34 | 0.002* | 4.99±1.21 | 4.91±1.00 | 0.42 | 0.674 |
| TG (mmol/L)# | 0.26±0.35 | 0.19±0.25 | 2.11 | 0.039* | 0.28±0.27 | 0.17±0.29 | 3.55 | 0.001* |
| LDL (mmol/L) | 2.89±1.13 | 2.63±0.82 | 1.76 | 0.085 | 2.75±0.93 | 2.77±0.99 | 0.20 | 0.845 |
| HDL (mmol/L)# | 0.08±0.10 | 0.08±0.11 | 0.14 | 0.890 | 0.05±0.12 | 0.09±0.09 | 2.36 | 0.022* |
Abnormal distribution, data were logarithm linearized.
Difference with significance.
Table 4.
Cases of HbA1c achievement after intervention within each group
| HbA1c | Control (n=55) | X2 | P | Telemedicine (n=53) | X2 | P | ||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before | After | Before | After | |||||
| <7% | 11 | 26 | 4.57 | 0.033* | 10 | 35 | 14.67 | <0.001* |
| ≥7% | 44 | 29 | 43 | 18 | ||||
Difference with significance.
Figure 2.
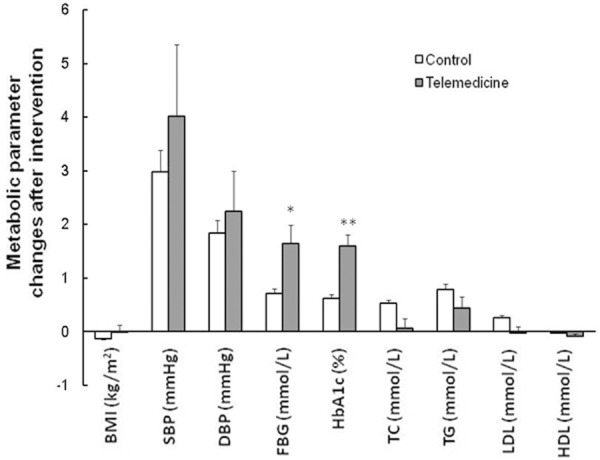
Metabolic parameter changes after intervention. *P < 0.05, **P < 0.01. Error bars, SE.
Note that key behavior improvement by telemedicine showed advantages in achievement of HbA1c target. Target achievement percentage of HbA1c in telemedicine group is 66.04%, which is significantly higher than 47.27% in control group (Table 5).
Table 5.
Cases of HbA1c achievement after intervention within each group
| HbA1c | Control (n=55) | X2 | P | Telemedicine (n=53) | X2 | P | ||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Before | After | Before | After | |||||
| <7% | 11 | 26 | 4.57 | 0.033* | 10 | 35 | 14.67 | <0.001* |
| ≥7% | 44 | 29 | 43 | 18 | ||||
Difference with significance.
Incidence of hypoglycemia is a horrible threat to life of diabetes patients. In the 3-month intervention, 23 participants of 108 patients underwent 47 times hypoglycemia, ranging from 2.1 to 3.9 mmol/L without severe outcomes. There are 7 cases of hypoglycemia (13.21%) in telemedicine group and 16 cases (29.09%) in control group (P = 0.044) as shown by Table 6.
Table 6.
Incidence of hypoglycemia
| Hypoglycemia | Control (n=55) | Telemedicine (n=53) | X2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| n (%) | n (%) | |||||
| Yes | 16 | 29.1 | 7 | 13.2 | 4.06 | 0.044* |
| No | 39 | 70.9 | 46 | 86.8 | ||
Difference with significance.
Discussion
The present study shows that the telemedicine system based on the internet applied to monitoring key behaviors rather than solely blood glucose is feasible and meaningful in clinical practice. There is a scientific consensus that the risk of diabetic complications rises steadily when HbA1c values are in excess of 6.5% (48 mmol/mol) [19,20]. Therefore, from 2010/2011 onward, this value has been incorporated as a diagnostic criterion in the recommendations of the World Health Organization (WHO) [21]. However, the diabetes controlling status in China is far behind the target of the guideline. Furthermore, only hypoglycemic therapy always results in frequent incidences of hypoglycemia which is more dangerous than diabetes itself. We aimed to help patients effectively manage themselves at home and achieve better glucose level, body weight, blood pressure and lipids. Our study improved the situation of glucose and HbA1c, more importantly, reduced hypoglycemia incidence.
In recent two decades, more and more diabetes patients use Trace blood glucose meter to monitor change of glucose and regulate their intake of oral medicine or injection volume of insulin. However, as a matter of fact, patients usually do not realize the abnormal glucose level. Sometimes they don’t know how to regulate or falsely regulate the medication according to the glucose. In some special situations, such as acute attack of disease, patients usually don’t know how to control their diet, body exercising and medication, resulting in a bad glucose management. On the other hand, as the professional staff, they cannot get the information like glucose or BP until next time when the patients visit. Thus they are not able to give advice or medical treatment in time when the patients encounter extreme events. Traditional face-to-face visit between diabetes patients and professionals need a supplementary management system to become more flexible and effective. Our system provides a better fashion to achieve self-management of patients at home.
Type 2 diabetes mellitus (T2DM) is a multiple metabolic disease, which is usually accompanied by obese, hypertension, dyslipidemia, etc. These co-morbidities elevate the risk of T2DM complications remarkably. Therefore, successful treatment of diabetes should base on well controlling of metabolic balance. By design, our study focused on BMI, BP, FBG, HbA1c and plasma lipids of patients with suboptimal glucose control and observed the effects of telemedicine intervention on diabetes through managing these metabolic indexes. The telemedicine group had better performance in the FBG, HbA1c, BP and lipids, in which FBG and HbA1c have significant improvement. The differences of BP and lipids between intervention group and control group may need a longer interval of investigation to be demonstrated.
HbA1c is the golden standard of long term glucose controlling. United Kingdom Prospective Diabetes Study (UKPDS) proved that any reduction in HbA1c is likely to reduce the risk of complications, with the lowest risk being in those with HbA1c values in the normal range (< 6.0%) [4]. A 10-year follow-up trial from the UKPDS indicated that intensive glycemic control established earlier in the course of type 2 diabetes does reduce subsequent cardiovascular events, even though the differential in HbA1c among patients initially treated intensively dissipated within 1 year [22]. However, intensive glycemic control would have resulted in hypoglycemia, which is the baffle of diabetes treatment. Our results provide a novel view that better key behaviors may contribute to reducing incidence of hypoglycemia.
A significant reduction in the number of face-to-face visits means a significant saving of time and community resources. This is another advantage of telemedicine treatment. Nevertheless, since it is a system based on internet, the application is restricted. T2DM patients are usually old and some of them are lack of education. Although the relatives can sometimes help them to manage the system, actually the data are always delayed or omitted. Especially when extremely high or low glycemia happened, the specialist cannot be aware of and provide proper guidance in time. In addition, the feedback of information between patients and the specialists on line is not proper because of a third person to convey. This may impact the effects of patients’ self-management. In the preliminary stage of the study, researchers made a survey on hospitalized T2DM patients. Only 20.8% patients agree with the telemedicine management after leaving hospital. Not familiar with internet or no internet device at home are the main reasons. Due to the results from the survey, this study extend the terms that the patients who can log on internet at home by themselves or with the help from relatives or friends to log on internet are encouraged to participate in this investigation.
Our study achieved effective short-term goals to control glycemia and reduce incidence of hypoglycemia although this system did not combine active medication management. However, the use of the telemedicine system as an alternative to unscheduled face-to-face visits did not determine differences in the BMI, BP nor some lipids in outcomes. A long-term of investigation is necessary to further assess the diabetes associated metabolic items and outcomes.
Acknowledgements
This project was supported by Research Fund of the First Clinical Medical College of Jinan University; Medical Science Foundation of Guangdong Province, 20120345.
Disclosure of conflict of interest
None.
References
- 1.Guariguata L, Whiting D, Weil C, Unwin N. The International Diabetes Federation diabetes atlas methodology for estimating global and national prevalence of diabetes in adults. Diabetes Res Clin Pract. 2011;94:322–332. doi: 10.1016/j.diabres.2011.10.040. [DOI] [PubMed] [Google Scholar]
- 2.Maciejewski ML, Maynard C. Diabetes-related utilization and costs for inpatient and outpatient services in the Veterans Administration. Diabetes Care. 2004;27(Suppl 2):B69–73. doi: 10.2337/diacare.27.suppl_2.b69. [DOI] [PubMed] [Google Scholar]
- 3.Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- 4.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, Hadden D, Turner RC, Holman RR. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352:854–865. [PubMed] [Google Scholar]
- 6.The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. The Diabetes Control and Complications Trial Research Group. New Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 7.Colagiuri S, Dickinson S, Girgis S, Colagiuri R, editors. National evidence based guideline for blood glucose control in type 2 diabetes. Diabetes Australia and the NHMRC. 2009. Available from URL: http://www.nhmrc.gov.au/guidelines/publications/di19 (Accessed 15 August 2011)
- 8.American Diabetes Association. Standards of medical care in diabetes-2011. Diabetes Care. 2011;34:s19. doi: 10.2337/dc11-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Canadian Diabetes Association. Clinical practice guidelines for theprevention and management of diabetes in Canada. Can J Diabetes. 2008;32(Suppl 1):580–591. [Google Scholar]
- 10.Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, Shan Z, Liu J, Tian H, Ji Q, Zhu D, Ge J, Lin L, Chen L, Guo X, Zhao Z, Li Q, Zhou Z, Shan G, He J. Prevalence of diabetes among men and women in China. New Engl J Med. 2010;362:1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 11.Montori VM, Helgemoe PK, Guyatt GH, Dean DS, Leung TW, Smith SA, Kudva YC. Telecare for patients with type 1 diabetes and inadequate glycemic control: a randomized controlled trial and meta-analysis. Diabetes Care. 2004;27:1088–1094. doi: 10.2337/diacare.27.5.1088. [DOI] [PubMed] [Google Scholar]
- 12.Kwon HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM, Kim SR, Chang SA, Kim HS, Cha BY, Lee KW, Son HY, Lee JH, Lee WC, Yoon KH. Establishment of blood glucose monitoring system using the internet. Diabetes Care. 2004;27:478–83. doi: 10.2337/diacare.27.2.478. [DOI] [PubMed] [Google Scholar]
- 13.Kwon HS, Cho JH, Kim HS, Lee JH, Song BR, Oh JA, Han JH, Kim HS, Cha BY, Lee KW, Son HY, Kang SK, Lee WC, Yoon KH. Development of web-based diabetic patient management system using short message service (SMS) Diabetes Rres Clin Pract. 2004;66(Suppl 1):S133–137. doi: 10.1016/j.diabres.2003.10.028. [DOI] [PubMed] [Google Scholar]
- 14.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes. Diabetes Care. 2005;28:1624–9. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bellazzi R, Arcelloni M, Ferrari P, Decata P, Hernando ME, Garcia A, Gazzaruso C, Gómez EJ, Larizza C, Fratino P, Stefanelli M. Management of patients with diabetes through information technology: tools for monitoring and control of the patients’ metabolic behavior. Diabetes Technol Ther. 2004;6:567–578. doi: 10.1089/dia.2004.6.567. [DOI] [PubMed] [Google Scholar]
- 16.Kim C, Kim H, Nam J, Cho M, Park J, Kang E, Ahn C, Cha B, Lee E, Lim S, Kim K, Lee H. Internet diabetic patient management using a short messaging service automatically produced by a knowledge matrix system. Diabetes Care. 2007;30:2857–2858. doi: 10.2337/dc06-2464. [DOI] [PubMed] [Google Scholar]
- 17.Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in Type 2 diabetes. Diabetic Med. 2008;25:245–54. doi: 10.1111/j.1464-5491.2007.02341.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stone RA, Rao RH, Sevick MA, Cheng C, Hough LJ, Macpherson DS, Franko CM, Anglin RA, Obrosky DS, Derubertis FR. Active care management supported by home telemonitoring in veterans with type 2 diabetes: the DiaTel randomized controlled trial. Diabetes Care. 2010;33:478–484. doi: 10.2337/dc09-1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Selvin E, Steffes MW, Zhu H, Matsushita K, Wagenknecht L, Pankow J, Coresh J, Brancati FL. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. New Engl J Med. 2010;362:800–811. doi: 10.1056/NEJMoa0908359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, Kojima Y, Furuyoshi N, Shichiri M. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995;28:103–117. doi: 10.1016/0168-8227(95)01064-k. [DOI] [PubMed] [Google Scholar]
- 21.Summary of revisions for the 2010 Clinical Practice Recommendations. Diabetes Care. 2010;33(Suppl 1):S3. doi: 10.2337/dc10-S003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89. doi: 10.1056/NEJMoa0806470. [DOI] [PubMed] [Google Scholar]


