Abstract
Intracranial extraaxial ependymomas (IEAEs) are very rare, and extra-axial petroclival ependymoma (EAPE) has not been reported in the reviewed English-language literature by now. We present a male patient with EAPE misdiagnosed as a petroclival meningioma preoperatively, and involved recurrence at 4th months after operation though totally resection. Thereafter, we report this case and discuss the clinical characteristics of the disease by briefly review.
Keywords: Ependymomas, extraaxial, petroclival region, intracranial
Introduction
Ependymomas represent 2% to 9% of all intracranial tumors, which are more common in children and majority are located in posterior fossa [1]. Of course, intracranial ependymomas can arise from the ventricular system or extraventricular tissue [2]. However, intracranial extra-axial ependymomas (IEAEs) are extremely rare. There is no literatures involvement IEAEs occuring in petroclival region. Here, we firstly report a male patient case with extra-axial petroclival ependymoma (EAPE), which was diagnosed as a meningioma preoperatively.
Case report
A 35-year-old male patient was admitted with complaint of a 3-month history of right upper extremity strength decreased with fingers numbness, as well as slight declined right lower extremity strength, without headache and vomiting. No abnormal physical and laboratory examination was detected except for slight left facial and oculomotor nerve palsy after admission. The patient had a no-detailed history of craniocerebral trauma nine years ago. Magnetic resonance imaging (MRI) showed that the lesion was 4.2 × 3.5 × 3.8 cm in size in the petroclival region with long-T1 signal, iso- to long-T2 signal and heterogeneous contrast enhancement on gadolinium-enhanced T1-weighted images. The boundary of the lesion was relatively clear from surrounding brainstem (Figure 1A-D). The lesion was diagnosed as a meningioma preoperatively.
Figure 1.
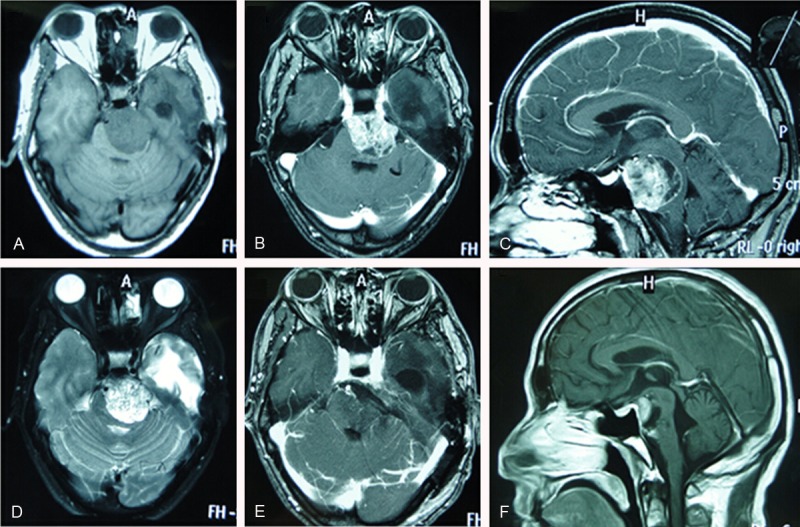
Radiologic characterization of extra-axial petroclival ependymoma. A, D. Preoperative cranial MRI showing the tumor is hypointensesity on T1-weighted imaging (T1W) and iso- to hyperintensity on T2-weighted imaging (T2W). B, C. Axial and sagittal contrast enhanced T1-weighted MR imaging showing heterogenous enhancement. E. Postoperative axial contrast enhanced T1-weighted MR image revealing the tumor was totally resection. F. Postoperative cranial MRI at 4-month follow-up showing tumor recurrence.
The mass was completely removed via left retrosigmoid sinus craniotomy (Figure 1E). During the operation, the left cranial nerves (V, VII, VIII) passed through the surface of the tumor. The adhesion between lesion and brainstem showed poor though the brainstem was compressed severely. The main blood supply of the mass came from the petroclival duramater.
The histological diagnosis revealed a typical ependymoma (WHO II). On hematoxylin and eosin staining, tumor cells formed perivascular pseudorosettes (Figure 2A), the tumor showed a positive immunoreactivity for glial fibriallary acid protein (GFAP) (Figure 2B). The PCK and Calretinin immunoreactivity were negative. The Ki67-MIB1 index was 5-10%.
Figure 2.
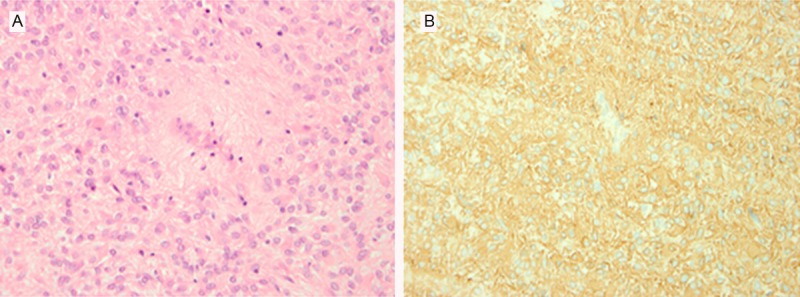
Histopathologic characterization of extra-axial petroclival ependymoma. A. Photomicrograph from primary resection demonstrating tumor cell forming perivascular pseudorosettes. (H & E, 400 ×). B. GFAP immunohistochemistry staining revealing a strong cytoplasmic immunoreactivity. (immunostaining, 400 ×).
The patient recovered well after operations, especially for the limb muscle strength. There was no new neurological defect and complications except the left abducens nerve palsy after surgery. The patient did not accept radiotherapy or chemotherapy because of totally resection through the review of postoperative MRI. Unfortunately, MRI showed the tumor recurrence during the 4 months of follow-up (Figure 1F). Radiotherapy (gamma knife) was applied for the recurrence mass.
Discussion
Ependymomas most frequently occur in intraventricular or intraspinal locations, and other soft tissue locations involvement ependymomas have also been reported, such as lung, mediastinum and ovary tissues [3]. About 60 to 70% of intracranial ependymomas arise in the posterior fossa, especially in the fourth ventricle [4]. Although many masses extend into the cisterna magna or cerebellopontine cistern, it is extremely rare for the intracranial ependymomas completely originating from extra-axial locations. To date, only 14 cases of IEAEs have been reported in the English literature [1-14]. However, IEAEs occuring in petroclival region have not been reported by now. Our case is the first reported case of extra-axial petroclival ependymoma (EAPE).
The details of all the 15 cases of IEAEs, including our case with EAPE, have been summarized in Table 1. Of course, it may be impossible to distinguish whether a tumor is entirely extra-axial due to the poor microscopic technique and the undeveloped MRI scanning at earlier stage. Though, Winer et al [12] reported an ependymoma involving the pituitary fossa, they cannot exclude the possibility that the tumour arose in the third ventricle and extended downwards into the sella. Therefore, it is likely that the number of IEAEs have been overestimated in the related literature. Nevertheless, the limitation literature can not hinder us from getting understanding of the clinical characteristics of the disease.
Table 1.
Summary of intracranial extra-axial ependymomas
| Author (references) | Sex/age | Clinical manifestation | Tumor location | MRI (T1WI/T2WI/enhance-ment) | Adjuvant therapy | Follow-up |
|---|---|---|---|---|---|---|
| Hanche [7] | M/29 | Headache | Interhemispheric | NA | Radiotherapy, Chemotherapy | NA |
| Cosgrove [4] | M/78 | Headache, nausea | CPA | NA | No | NA |
| Winer [12] | M/81 | Visual fields failure, diplopia | pituitary fossa | NA | NA | NA |
| Hayashi [8] | M/13 | Headache, nausea, vomiting | Occipital convexity CPA | Iso/iso/heterogenous | No | NA |
| Fukui [5] | M/66 | Facial pain | CPA and cavernous sinus | Low/slightly high/heterogenous | Radiotherapy | 2.5 years/tumor-free |
| Donich [3] | F/22 | Headache, facial paralysis | Interhemispheric | NA/high/heterogenous | Radiotherapy | 18 months/tumor-free |
| Youkilis [11] | M/20 | Seizure | Frontal convexity | Iso/iso/heterogenous | No | 1 year/tumor-free |
| Goto [6] | M/29 | Seizure, Hemiparesis | CPA and Meckel’s cave | Iso/iso/heterogenous | No | 9 months/tumor-free |
| Torun [10] | M/31 | Headache, nausea, dizziness, facial paresis | CPA | Iso/NA/heterogenous | Radiotherapy | NA |
| Kasliwal [9] | F/50 | Headache, vomiting | Frontotemporal convexity | Iso/iso/NA | Radiotherapy | NA |
| L Ma [2] | M/10 | Headache, vomiting | parietooccipital region | Iso/iso/heterogenous | No | 2 years/tumor free |
| Salunke [1] | F/43 | Visual-loss headaches | CPA | Iso/iso/homogenous | Radiotherapy | 6 months/tumor free |
| Gill [14] | M/48 | Headache, vomiting, ataxia, mild hearing loss | the ambient cistern | Hypo/hyper/ heterogenous | NA | NA |
| GY Seo [13] | M/25 | Headache | Petroclival region | Iso-to-hyper/iso-to-hypo/heterogenous | Radiotherapy, Chemotherapy | NA |
| Present case | M/35 | hemiparesis | Hypo/hyper/ heterogenous | No | 4-mon/tumor recurrence |
CPA, cerebellopontine angle; NA, not available; T1WI, T1-weighted image; T2WI, T2-weighted image.
To our knowledge, the location of CPA is a relatively high incidence area for IEAEs (n = 6, Table 1). In spite of IEAEs have affected other regions sporadically, no more evidence show petroclival region involvement of these diseases. IEAEs have a predilection for male patients (n = 12, including our case), the onset age (35 years) of our case is close to the mean age of 38.8 years (ranging from 10 to 81 years). Unlike headache or vomiting in most of the IEAEs, the patient in our report presented hemiparesis with mainly performance of right upper extremity strength decreased, which was caused by the fatal tumor compression of the brainstem. This reveals that there may be without any typical symptoms belong to IEAEs.
The reason why we made misdiagnosis preoperatively is that the rarity of IEAEs and the tumor mimicking petroclival meningioma. Actually, we cannot exclude the possibility of atypical heterogenous enhanced meningioma even if most of meningiomas showed homogenous enhancement [15]. Considering unspecific injury of the cranial nerves, the possibility of schwannoma was excluded. However, intraoperative frozen section was inconclusive and the pathological diagnosis after surgery overthrew our preoperative diagnosis. The key histological features with perivascular pseudorosettes indicated a typical ependymoma in our case. The positive reactive for GFAP consolidated the diagnosis of EAPE and denied meningioma or schwannoma [2]. The Ki67-MIB1 index (5-10%) was corresponding to the WHO grade II ependymoma.
Interestingly, how tumor originated from the petroclival region. Despite some hypothesized mechanisms can be obtained for the development of IEAEs from the limitation literatures [2], the viewpoint that the origin of IEAEs is associated with the presence of heterotopic ependymal cell rests during the fetal development is favored by most of the learners [2,4,8,12]. Our case was a pure IEAE without any attachment to the brainstem as observed intraoperatively, though the brainstem was compressed severely, and probably originated from the heterotopic ependymal cell residue in the subarachnoid space (namely prepontine cistern). Other possibilities included an ependymal cell rest or multiple ependymal cell rests in the petroclival region. Whether existing so-called ependymal cell precursors in the petroclival region triggering ependymoma subsequently during fetal development deserves to deeply research in the future.
Whereas the rarity, the optimal treatment of IEAEs is undefined. Surgical management was completed in all cases except not available in Hanchey’s report [7]. Although totally resection was performed in our case under the observation of intraoperative microscope and postoperative MRI, the tumor still recurred at 4th month after surgery. Two mainly reasons can interpret the recurrence mass. There must be some residual tumor cells attaching to the petroclival duramater, which could not be seen by the naked eye and was the source of recurrence. Besides, the patient in our case rejected postoperative radiotherapy; this may be another key factor determining whether the tumor recurred in a short time. Here, we suggest that postoperative adjuvant radiotherapy should be applied to IEAEs individually especially for the patient with close relationship between the tumor and surrounding tissues. The patient received radiotherapy (gamma knife) for the recurrence tumor, and he was stable at present.
In conclusion, this case presents the unusual occurrence of an entirely IEAE and is the first reported case of an ependymoma involving the petroclival location, which can foster us better understanding of these diseases.
Disclosure of conflict of interest
None.
References
- 1.Salunke P, Kovai P, Sura S, Gupta K. Extra-axial ependymoma mimicking a parasagittal meningioma. J Clin Neurosci. 2011;18:418–420. doi: 10.1016/j.jocn.2010.04.042. [DOI] [PubMed] [Google Scholar]
- 2.Ma L, Xiao SY, Liu XS, You C, Zhang YK. Intracranial extraaxial ependymoma in children: a rare case report and review of the literature. Neurol Sci. 2012;33:151–154. doi: 10.1007/s10072-011-0664-7. [DOI] [PubMed] [Google Scholar]
- 3.Donich D, Lee JH, Prayson R. Giant extra-axial cerebellopontine angle/cavernous sinus ependymoma: case report. Neurosurg. 1999;44:195–198. doi: 10.1097/00006123-199901000-00116. [DOI] [PubMed] [Google Scholar]
- 4.Cosgrove GR, Villemure JG, Robitaille Y, Melanson D. Extraaxial ependymoma of the posterior fossa. Surg Neurol. 1985;24:433–436. doi: 10.1016/0090-3019(85)90304-0. [DOI] [PubMed] [Google Scholar]
- 5.Fukui MB, Hogg JP, Martinez AJ. Extraaxial ependymoma of the posterior fossa. Am J Neuroradiol. 1997;18:1179–1181. [PMC free article] [PubMed] [Google Scholar]
- 6.Goto T, Ohata K, Tsuyuguchi N, Takami T, Hara M. Extra-axial subarachnoid ependymoma of the cerebral convexity. Acta Neurochir. 2003;145:913–917. doi: 10.1007/s00701-003-0103-5. [DOI] [PubMed] [Google Scholar]
- 7.Hanchey RE, Stears JC, Lehman RA, Norenberg MD. Interhemispheric ependymoma mimicking falx meningioma: case report. J Neurosurg. 1976;45:108–112. doi: 10.3171/jns.1976.45.1.0108. [DOI] [PubMed] [Google Scholar]
- 8.Hayashi K, Tamura M, Shimozuru T, Kasamo S, Hirahara K, Kadota K, Asakura T. Extra-axial ependymoma-case report. Neurol Med Chir. 1994;34:295–299. doi: 10.2176/nmc.34.295. [DOI] [PubMed] [Google Scholar]
- 9.Kasliwal MK, Chandra PS, Sharma BS. Images in neuro-oncology: primary extraaxial cerebellopontine angle ependymoma. J Neurooncol. 2007;83:31–32. doi: 10.1007/s11060-007-9330-6. [DOI] [PubMed] [Google Scholar]
- 10.Torun F, Tuna H, Bozkurt M, Deda H. Extra-axial ependymoma of posterior fossa extending to the Meckel’s cave. Clin Neurol Neurosurg. 2005;107:334–336. doi: 10.1016/j.clineuro.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 11.Youkilis AS, Park P, McKeever PE, Chandler WF. Parasagittal ependymoma resembling falcine meningioma. Am J Neuroradiol. 2001;22:1105–1108. [PMC free article] [PubMed] [Google Scholar]
- 12.Winer JB, Lidov H, Scaravilli F. An ependymoma involving the pituitary fossa. J Neurol Neurosurg Psychiatry. 1989;52:1443. doi: 10.1136/jnnp.52.12.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Seo GY, Byun JS, Kim JK, Kwon JT, Park ES, Jung YY. Intracranial Extra-Axial Ependymoma in the Ambient Cistern That Initially Presented as Calcification: A Report of Case. J Korean Soc Radiol. 2013;68:5–8. [Google Scholar]
- 14.Gill AS, Taheri MR, Hamilton J, Monfared A. Extra-Axial Ependymoma Presenting as a Cerebellopontine Angle Mass. Otol Neurotol. 2014 doi: 10.1097/MAO.0000000000000479. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 15.Buetow MP, Buetow PC, Smirniotopoulos JG. Typical, atypical, and misleading features in meningioma. Radiographics. 1991;11:1087–1106. doi: 10.1148/radiographics.11.6.1749851. [DOI] [PubMed] [Google Scholar]


