Abstract
Objective:
The epidemiology of major depressive disorder (MDD) was first described in the Canadian national population in 2002. Updated information is now available from a 2012 survey: the Canadian Community Health Study—Mental Health (CCHS-MH).
Method:
The CCHS-MH employed an adaptation of the World Health Organization World Mental Health Composite International Diagnostic Interview and had a sample of n = 25 113. Demographic variables, treatment, comorbidities, suicidal ideation, and perceived stigma were assessed. The analysis estimated adjusted and unadjusted frequencies and prevalence ratios. All estimates incorporated analysis methods to account for complex survey design effects.
Results:
The past-year prevalence of MDD was 3.9% (95% CI 3.5% to 4.2%). Prevalence was higher in women and in younger age groups. Among respondents with past-year MDD, 63.1% had sought treatment and 33.1% were taking an antidepressant (AD); 4.8% had past-year alcohol abuse and 4.5% had alcohol dependence. Among respondents with past-year MDD, the prevalence of cannabis abuse was 2.5% and that of dependence was 2.9%. For drugs other than cannabis, the prevalence of abuse was 2.3% and dependence was 2.9%. Generalized anxiety disorder was present in 24.9%. Suicide attempts were reported by 6.6% of respondents with past-year MDD. Among respondents accessing treatment, 37.5% perceived that others held negative opinions about them or treated them unfairly because of their disorder.
Conclusions:
MDD is a common, burdensome, and stigmatized condition in Canada. Seeking help from professionals was reported at a higher frequency than in prior Canadian studies, but there has been no increase in AD use among Canadians with MDD.
Keywords: major depressive disorder, major depressive episodes, depression, population studies, cross-sectional studies, health care use, epidemiology
Abstract
Objectif :
L’épidémiologie du trouble dépressif majeur (TDM) a été décrite pour la première fois dans la population canadienne nationale en 2002. L’information mise à jour est maintenant offerte par une enquête de 2012 : l’Enquête sur la santé dans les collectivités canadiennes - Santé mentale (ESCC-SM).
Méthode :
L’ESCC-SM a utilisé une adaptation de l’Entrevue composite diagnostique internationale de santé mentale mondial de l’Organisation mondiale de la santé et disposait d’un échantillon de n = 25 113. Les variables démographiques, le traitement, les comorbidités, l’idéation suicidaire, et les stigmates perçus ont été évalués. L’analyse a estimé les fréquences et les rapports de prévalence corrigés et non corrigés. Toutes les estimations incorporaient les méthodes d’analyse pour rendre compte des effets complexes de la méthodologie de l’enquête.
Résultats :
La prévalence du TDM sur un an était de 3,9 % (IC à 95 % 3,5 % à 4,2 %). La prévalence était plus élevée chez les femmes et dans les groupes plus jeunes. Chez les répondants ayant souffert du TDM l’an dernier, 63,1 % avaient demandé un traitement et 33,1 % prenaient un antidépresseur (AD); 4,8 % avaient abusé de l’alcool l’an dernier et 4,5 % étaient dépendants de l’alcool. Toujours chez les répondants ayant souffert du TDM l’an dernier, la prévalence de l’utilisation de cannabis était de 2,5 % et celle de la dépendance au cannabis était de 2,9 %. En ce qui concerne les drogues autres que le cannabis, la prévalence d’abus était de 2,3 % et celle de la dépendance, de 2,9 %. Des tentatives de suicide ont été déclarées par 6,6 % des répondants ayant souffert du TDM l’an dernier. Parmi les répondants ayant accès au traitement, 37,5 % percevaient que les autres avaient une opinion négative à leur égard ou qu’ils les traitaient injustement en raison de leur trouble.
Conclusions :
Le TDM est une affection commune, coûteuse, et stigmatisée au Canada. La recherche de l’aide de professionnels était rapportée à une fréquence plus élevée que dans les études canadiennes précédentes, mais l’utilisation d’AD n’a pas augmenté chez les Canadiens souffrant de TDM.
Until recently, a 2002 survey, called the CCHS 1.2, was the only national source of descriptive epidemiologic data for MDD in Canada.1 In 2012, Statistics Canada conducted a second national mental health survey, called the CCHS-MH. The repeat survey provides updated information about the epidemiology of this disorder. Consistent with the goals of descriptive epidemiology, the objective of our paper is to provide a broad characterization of the distribution of this condition within the population.2 Such information is useful for quantifying burden, for priority-setting, as foundational information for policy development, and for generating hypotheses about etiology. Descriptive estimates also provide a benchmark against which subsequent estimates can be referenced. Thus far, only preliminary estimates from the 2012 survey have been reported, including an estimated lifetime prevalence of MDE of 11.3% and an estimated past-year MDE prevalence of 4.7%.3
As this was a descriptive analysis, demographic variables were assessed. An additional goal was to examine 5 aspects of the epidemiology that had not previously been reported or were subject to change over time:
the frequency of treatment;
SUD comorbidity (in the CCHS 1.2, these disorders were assessed using only an abbreviated instrument);
comorbidity with GAD (not assessed by the prior study);
suicidal ideation (as the 2012 survey included a more detailed assessment of suicidal thoughts and behaviours than was previously available); and
perceived stigma associated with MDD.
The CCHS-MH assessment of perceived stigma was the first such assessment in a national mental health survey.
Clinical Implications
Clinical management of MDD may need to address adverse social correlates of this condition, for example, a strong negative association with income.
Changing patterns of pharmacological management include increased use of atypical APs, suggesting a need for anthropometric and metabolic monitoring.
Stigmatization was frequently reported by people with MDD. This may be a barrier to successful treatment.
Limitations
The CCHS-MH sample was restricted to household residents, excluding homeless people, full-time members of the Canadian Armed Forces, and people living on reserves or in institutions.
The diagnostic interview used in the CCHS-MH is not equivalent to clinical assessment by a professional. The instrument relies on lay interviewers working from a fully structured script.
Comparison of MDD epidemiology in 2012 to that of 2002 is complicated by a different method of assessment of BD.
Methods
Detailed methodological information on the CCHS-MH is available from Statistics Canada archives.4 In brief, the survey targeted Canadian household residents 15 years of age and over living in any of the 10 provinces. Excluded were people living on reserves and other Aboriginal settlements, full-time members of the Canadian Armed Forces, and residents of institutions. These exclusions amount to about 3% of the national population. A complex multi-stage sampling procedure was used. This was based initially on selection of geographical clusters, followed by selection of households from within those clusters, and finally by selection of one respondent per household. Data collection occurred between January 2, 2012, and December 31, 2012. A total of 25 113 interviews were conducted using computer assisted personal interviewing. Most interviews (87%) were conducted in person.
Statistics Canada calculates sampling weights that help to ensure valid inference to the target (household) population. The sampling weights account for design characteristics such as unequal selection probabilities, exclusion of out-of-scope units, nonresponse at the household and personal level, and extreme values.4 A set of 500 replicate bootstrap weights allow accurate confidence intervals to be calculated by accounting for clustering in the multi-stage sampling procedure.
From an initial sample of 43 030 households, 36 443 were found to be eligible for the survey. Among these, 29 088 households agreed to participate (79.8%). From those households, 25 113 individual respondents agreed to participate (86.3%), leading to a combined (household and person) response rate of 68.9%. The response rate is comparable to those achieved internationally in similar studies. For example, the WMH Surveys had an average response rate of 71.7%.5
Lifetime prevalence of MDE was estimated as the proportion of the population reporting one or more MDE during their lifetime according to the WMH-CIDI instrument.6 The prevalence of MDD was calculated in the same way, except that those with CIDI-defined BD I or II were excluded, in keeping with DSM-IV criteria. The version of the WMHCIDI used in the CCHS-MH covered MDD, BDs, GAD, alcohol abuse, alcohol dependence, drug abuse, and drug dependence. For our analysis, cannabis abuse and dependence was estimated, and estimates were also made for the prevalence of abuse and dependence on drugs other than cannabis.
Demographic items, such as age, sex, and marital and employment status, were assessed using standard interview items. Income was assessed in the survey using deciles based on total household income adjusted for family size and place of residence. Three aspects of treatment for MDD were assessed: perceived need for care, accessing services, and medication use. Accessing services was assessed using items from a module developed and field tested for this survey by Statistics Canada. Medication use was assessed by collecting the DINs during the interviews. DINs for past 2-day medication use were recorded after asking respondents to collect medication bottles and containers for any psychiatric medications taken in the 2 days preceding the interview.
SUD comorbidities and GAD prevalence were both assessed using WMH-CIDI modules and associated algorithms. The suicide module was designed and field tested by Statistics Canada. The module assessed both ideation and attempts. The CCHS-MH also assessed perceived stigma using a module developed by Statistics Canada in consultation with the Mental Health Commission of Canada.7 The module was administered only to respondents who reported receiving treatment during the past year. An initial item asked, “During the past 12 months, did you feel that anyone held negative opinions about you or treated you unfairly because of your past or current emotional or mental health problem?” This was followed by a series of questions asking “how did this affect you?” in the domains of family life, romantic life, school or work life, financial situation, housing situation, or care received for physical health problems. Each impact was assessed on a number analogue scale of 0 to 10 (0 meaning not affected and 10 meaning severely affected). We calculated the proportion reporting perceived stigma and mean impact across the 5 dimensions.
Data analysis was conducted at the Prairie Regional Data Centre in Calgary using the statistical software Stata version 12.8 As the data were cross-sectional, descriptive techniques were used, including estimation of frequencies, PRs, and associated 95% confidence intervals. Binomial regression was used to produce age- and sex-adjusted PRs and associated 95% confidence intervals. Age was included in these models as a continuous variable. Owing to widespread serious concerns about the validity of lifetime MDD prevalence estimates,9–11 the analysis focused on past-year MDD prevalence.
Results
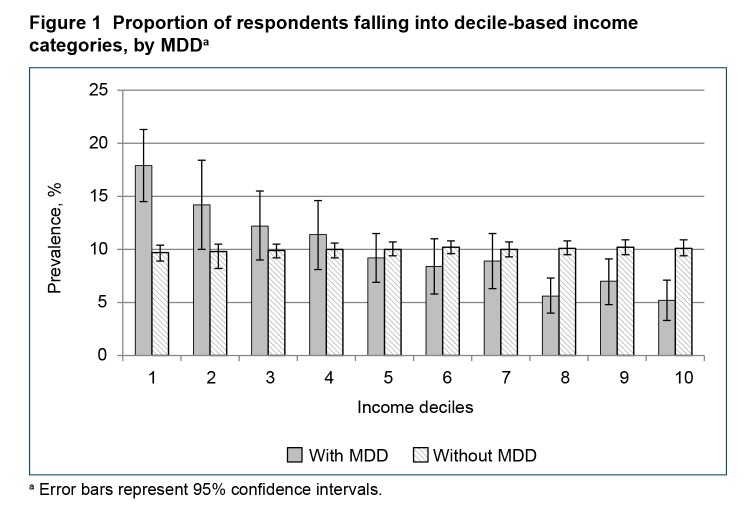
Demographic characteristics of the CCHS-MH sample (weighted) are presented in Table 1. Among respondents, 0.7% did not provide sufficient information on the WMHCIDI to classify their MDD status. With exclusion of these respondents, the analysis was restricted to n = 24 951. The lifetime prevalence of MDE was 11.3% (95% CI 10.6% to 11.9%) and the past-year prevalence of MDE was 4.7% (95% CI 4.3% to 5.1%). With exclusion of subjects with BD according to the WMH-CIDI, the lifetime prevalence of MDD was 9.9% (95% CI 9.3% to 10.5%) and the annual prevalence was 3.9% (95% CI 3.5% to 4.2%). Among men, 2.8% (95% CI 2.3% to 3.2%) reported past-year MDD, compared with 4.9% (95% CI 4.3% to 5.5%) of women. A likelihood ratio test for province of residence found no evidence of heterogeneity across provinces (χ2 = 13.45, df = 9, P = 0.14). Subjects with high school education (or less) had a prevalence (3.9%, 95% CI 3.1% to 4.6%), nearly identical to those with higher levels of education (3.8%, 95% CI 3.4% to 4.3%). The prevalence of MDD in the immigrant population was somewhat lower at 2.7% (95% CI 0.3% to 7.7%). Figure 1 shows deciles of total household income by MDD status. People with past-year MDD were almost twice as likely to be in the lowest decile category and were about one-half as likely to be in the highest decile group.
Table 1.
Demographic features of the study sample
| Demographic | Estimate (95% CI) |
|---|---|
| Sex, female, % | 50.7 (50.7 to 50.7) |
| Age, mean, years | 45.7 (45.5 to 45.8) |
| Marital status, % | |
| Married or common law | 60.1 (59.2 to 61.0) |
| Never married | 27.0 (26.3 to 27.7) |
| Widowed, separated, or divorced | 12.9 (12.3 to 13.6) |
| Level of education, % | |
| <High school graduation | 17.8 (17.0 to 18.6) |
| Some post-secondary | 82.2 (81.4 to 83.0) |
| Employment,a % | |
| Full timeb | 56.4 (55.3 to 57.4) |
| Part timec | 11.9 (11.3 to 12.5) |
| Unemployedd | 31.7 (30.8 to 32.7) |
| Difficulty making ends meet, % | 11.8 (11.0 to 12.5) |
| Immigrant status,e % | 25.2 (23.9 to 26.4) |
All employement estimates are restricted to those <75 years old
>30 hours/week
<30 hours/week
Did not work the previous week
Not born in Canada
Figure 1.
Proportion of respondents falling into decile-based income categories, by MDDa
aError bars represent 95% confidence intervals.
Binomial regression was used to examine the association of each of the variables in Table 1 with past-year MDD prevalence. Education was not associated with MDD in any analyses and did not affect the strength of association between other variables and MDD. Therefore, this variable was initially removed from the models. In a model simultaneously adjusting for each of the remaining variables, the PR for female sex was 1.7 (95% CI 0.14 to 2.0, P < 0.001). The PR for age was 0.98 (P < 0.001), suggesting a 2% decline in prevalence per year of age. Comparing single with married status, the PR was 1.3 (95% CI 1.0 to 1.7, P = 0.05) and that for divorced, separated, or widowed status was 2.1 (95% CI 1.5 to 3.0, P < 0.001). Not being employed had a PR of 1.2 (95% CI 1.1 to 1.3, P = 0.003), relative to those having full-or part-time employment. A protective effect of immigrant status persisted after adjustment, PR = 0.7 (95% CI 0.5 to 0.9, P < 0.001).
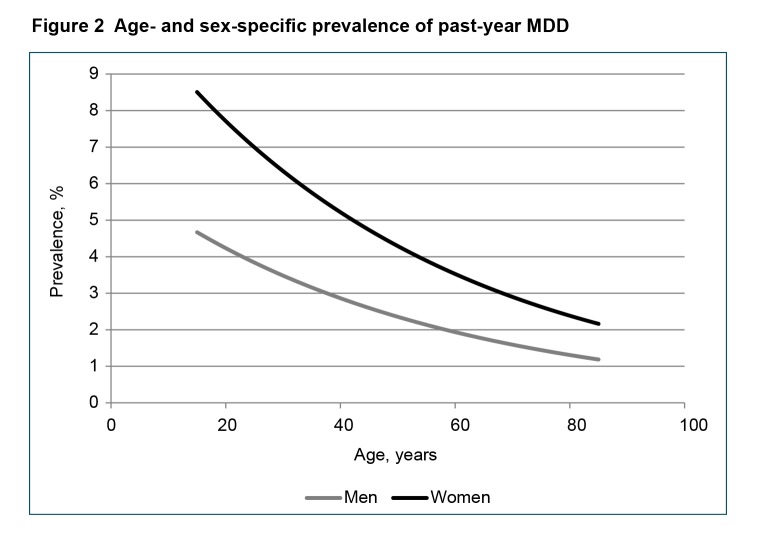
Age by sex interactions were not significant, and an age-squared term did not improve the fit of the model. Consistent with expectation, the prevalence was higher in women across the age range. Although, in the absence of interaction, the PR for sex was constant across the age range, the absolute difference became smaller in the older age groups (Figure 2).
Figure 2.
Age- and sex-specific prevalence of past-year MDD
Among subjects with past-year MDD, 85.1% reported that they considered themselves to have mental health care needs (compared with 22.2% of those without past-year MDD) and 63.1% (95% CI 58.5% to 67.7%) reported that they had seen a health professional about their mental health in the past year. Among these, slightly more than one-half (57.6%) reported that their mental health care needs were completely met, 31.4% reported that they were partially met, and 11.0% indicated that their needs were not met at all. Among respondents with past-year MDD, 33.1% (95% CI 28.1% to 38.0%) reported taking an AD in the 2 days preceding the survey. The proportion taking a sedative-hypnotic medication (benzodiazepine or Z-drug) was 7.9% (95% CI 5.5% to 10.4%), and the proportion taking an atypical AP was 6.4% (95% CI 4.6% to 8.3%).
The pattern of comorbidity with SUDs and GAD is presented in Table 2. The prevalence of alcohol and drug abuse and dependence was consistently higher in subjects with past-year MDD. As expected, GAD commonly coexisted with MDD.
Table 2.
Patterns of comorbidity with MDD, among conditions assessed in the Canadian Community Health Survey—Mental Health
| Prevalence in subjects | ||||
|---|---|---|---|---|
|
|
||||
| Variable | With MDD, %a | 95% CI | Without MDD, % | 95% CI |
| Alcohol dependence | ||||
| Lifetime | 8.6 | 6.4 to 10.9 | 2.8 | 2.5 to 3.1 |
| Past 12 months | 4.5 | 2.6 to 6.4 | 0.8 | 0.6 to 1.0 |
| Alcohol abuse | ||||
| Lifetime | 19.5 | 15.9 to 23.1 | 14.9 | 14.1 to 15.6 |
| Past 12 months | 4.8 | 2.9 to 6.7 | 2.1 | 1.8 to 2.4 |
| Drug dependence | ||||
| Lifetime, excluding cannabis | 6.1 | 4.4 to 7.8 | 1.7 | 1.4 to 2.0 |
| Lifetime cannabis dependence | 5.1 | 2.9 to 7.4 | 1.4 | 1.2 to 1.7 |
| Past 12 months, excluding cannabis | 2.5 | 1.4 to 3.5 | 0.3 | 0.2 to 0.4 |
| Past 12 months cannabis dependence | 2.9 | 0.9 to 5.0 | 0.4 | 0.3 to 0.5 |
| Drug abuse | ||||
| Lifetime, excluding cannabis | 5.9 | 3.8 to 8.1 | 1.9 | 1.7 to 2.2 |
| Lifetime cannabis abuse | 12.4 | 9.3 to 15.5 | 5.0 | 4.5 to 5.4 |
| Past 12 months, excluding cannabis | 2.3 | 0.7 to 3.9 | 0.2 | 0.1 to 0.3 |
| Past 12 months cannabis abuse | 2.5 | 1.1 to 3.8 | 0.7 | 0.6 to 0.9 |
| Generalized anxiety disorder | ||||
| Lifetime | 39.2 | 34.5 to 43.9 | 7.4 | 6.9 to 7.9 |
| Past 12 months | 24.9 | 21.0 to 28.8 | 1.7 | 1.4 to 1.9 |
Past-year MDD
Table 3 presents the frequency of suicidal ideation and perceived stigma in MDD. The prevalence of suicide attempts in the past year was elevated more than 20-fold in subjects with past-year MDD. Compared with subjects receiving treatment for mental health issues in the preceding year, those with MDD reported experiencing perceived stigma twice as often as those accessing mental health care for other reasons. In addition, they reported greater impact of the perceived stigmatization.
Table 3.
Association of MDD with suicidal ideation, attempts, and perceived stigma
| Variable | With MDD estimate, % | 95% CI | Without MDD estimate, % | 95% CI |
|---|---|---|---|---|
| Suicidal thought | ||||
| Lifetime | 47.7 | 43.1 to 52.4 | 10.4 | 9.8 to 11.0 |
| Past 12 months | 26.9 | 22.3 to 31.5 | 2.4 | 2.1 to 2.7 |
| Suicidal plan | ||||
| Lifetime | 22.6 | 18.1 to 27.0 | 3.4 | 3.0 to 3.7 |
| Past 12 months | 12.0 | 7.9 to 16.0 | 0.7 | 0.5 to 0.9 |
| Suicide attempt | ||||
| Lifetime | 16.6 | 12.3 to 20.9 | 2.5 | 2.2 to 2.8 |
| Past 12 months | 6.6 | 2.7 to 10.5 | 0.3 | 0.2 to 0.4 |
| Perceived others held negative opinions or was treated unfairlya | 37.8 | 30.5 to 45.0 | 20.0 | 16.9 to 23.0 |
| Mean stigma impacta | 7.5 | 5.5 to 9.4 | 3.4 | 2.8 to 4.1 |
The stigma module was administered to respondents reporting that they received treatment for an emotional or mental health problem in the preceding year. The Without MDD column consists of people seeking mental health treatment for other reasons.
Discussion
Our analysis cannot discern whether the prevalence of MDD has changed since the last national mental health survey in 2002. The prevalence of MDE was almost identical in the 2 surveys (4.7% in 2012 and 4.8% in 20021). The prevalence of MDD depends on the exclusion of cases of BD, which was done differently in the 2 surveys, such that the estimates are not directly comparable. The past-year prevalence of MDD was lower than several other recent surveys, such as the US National Comorbidity Survey Replication (6.6%)12 and the New Zealand Te Rau Hinengaro (5.7%).13 In high-income countries, past-year prevalence estimates in the WMH Surveys Initiative included some lower estimates as well; for example, 2.2% in Japan and 3.0% in Germany.5 Systematic reviews for the Global Burden of Disease Studies placed the point prevalence of MDD at 3.7% (95% uncertainty interval 3.1% to 4.3%),14 similar to the 12-month prevalence reported here.
Prevalence was higher in women and tended to decline with age, consistent with reports from most developed countries.5 Internationally, the pattern of declining age-specific prevalence has been less consistent than the sex difference (female > male). For example, in India and the Ukraine, young age is associated with low risk of MDE.5 Absolute difference between the prevalence in men and women became smaller at higher ages, similar to what was reported in 20021 and in a UK study.15 However, a statistical interaction on the multiplicative scale (as assessed by our binomial regression model) was not observed in this study (as it was in 20021). The prevalence was higher in subjects who were not working and in those who were unmarried. While the association of previously married status with MDD is consistently reported in international studies (especially for divorced or separated status), the association of never-married status is more characteristic of high-income countries such as Canada.5 The prevalence was lower in immigrants than in those who were Canadian-born, consistent with prior reports.16 The lack of association of MDD with education contrasts with US data17 and with estimates from Israel, Mexico, and the Ukraine,5 but is consistent with results from the 2002 Canadian survey,1 the European Study of the Epidemiology of Mental Disorders,18 and most other countries included in the World Mental Health Surveys program.5
After numerous prior Canadian reports of increasing AD use,19,20 these results do not suggest a continued increase in the frequency of AD use. Among subjects with past-year MDE, an analysis of the 2002 survey identified a 40% prevalence of AD use,21 whereas the frequency found in this analysis was 33%. However, a sizable proportion of atypical AP use was also found. The frequency of use of these medications among subjects with MDD has doubled since 2002.22 Overall, the proportion of people with a past-year MDD consulting with a health care professional appears to have increased, although caution is required owing to the differences between the 2 surveys, as noted above. Earlier studies have focused on MDE rather than MDD, but have generally reported frequencies of consultation in the 40% to 50% range23–25 among subjects with past-year MDE, whereas the frequency in 2012 was over 60%, similar to estimates from the most recent Australian survey.26 Also, nearly 60% reported that their mental health care–related needs were fully met, an encouraging percentage, but one that also suggests considerable room for improvement.
GAD is known to be strongly associated with MDD. The prevalence of this comorbidity in people with MDD (24.9% past-year and 39.2% lifetime) seems consistent with international estimates. In the Dunedin birth cohort, the rate of comorbidity was 30% by age 32.27 The New Zealand Survey (Te Rau Hinengaro) reported an odds ratio of 8.3 for the MDD–GAD comorbidity.28 The proportions reported in our Table 2 lead to an odds ratio of 8.1. Association of alcohol- and drug-related disorders with MDD have been reported previously. In DSM-5,29 the classification of SUDs has changed such that abuse and dependence are no longer distinguished. Te Rau Hinengaro reported odds ratios for these comorbidities that ranged from 2.7 to 8.0,28 consistent with the estimates reported in Table 2. One difference from the New Zealand study was the lack of association between MDD and alcohol abuse, whereas an association was evident in the Canadian data (Table 2).
Our study has several limitations. The estimates reported here are cross-sectional and do not imply causal effects. Further, the diagnostic interview employed in the CCHS-MH is administered by nonclinicians and is not as accurate as a detailed clinical assessment. Several of the instruments and items employed in the CCHS are abbreviated survey instruments, which may also be subject to inaccuracy. In many instances, more elaborate instruments (such as the use of semi-structured clinical interviews rather than a fully structured lay-administered instrument such as the Composite International Diagnostic Interview) would have been preferable. However, this approach is generally not feasible in large population surveys. Another limitation of the CCHS-MH is its limited coverage of anxiety disorders. GAD was the only anxiety disorder included in the survey. The process of choosing content for the CCHS survey involves consideration of respondent burden and feedback from consultation with advisory committees. GAD was included primarily because its prevalence had not previously been estimated in Canada.
Conclusion
People with MDD in Canada appear to be accessing mental health care more often than in the past, and the pattern of pharmacotherapy has changed, especially with increased use of atypical APs. The disorder is strongly associated with suicidal ideation, SUDs, and GAD. MDD remains a common, burdensome, and stigmatized condition within the Canadian population.
Acknowledgments
Dr Patten is a Senior Health Scholar with Alberta Innovates, Health Solutions. Keltie McDonald is a recipient of a Canadian Institutes of Health Research (CIHR)–Queen Elizabeth II Graduate Scholarship. This work was supported by a CIHR operating grant (MOP-130415). The study also received support from a Hotchkiss Brain Institute Grant “Depression in the Community.” The analysis was conducted at Prairie Regional Data Centre, which is part of the Canadian Research Data Centre Network (CRDCN). The services and activities provided by the CRDCN are made possible by the financial or in-kind support of the Social Sciences and Humanities Research Council, the CIHR, the Canadian Foundation for Innovation, Statistics Canada, and participating universities whose support is gratefully acknowledged. The views expressed in this paper do not necessarily represent the CRDCN’s or that of its partners. Data collection for the CCHS was carried out by Statistics Canada, but the analyses and interpretations presented here are those of the authors, not Statistics Canada.
Abbreviations
- AD
antidepressant
- AP
antipsychotic
- BD
bipolar disorder
- CCHS
Canadian Community Health Survey
- CCHS 1.2
CCHS: Mental Health and Well-being (2002)
- CCHS-MH
CCHS—Mental Health (2012)
- DIN
drug information number
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- GAD
generalized anxiety disorder
- MDD
major depressive disorder
- MDE
major depressive episode
- PR
prevalence ratio (a ratio of 2 prevalence estimates)
- SUD
substance use disorder
- WMH-CIDI
World Mental Health Composite International Diagnostic Interview
References
- 1.Patten SB, Wang JL, Williams JV, et al. Descriptive epidemiology major depression in Canada. Can J Psychiatry. 2006;51(2):84–90. doi: 10.1177/070674370605100204. [DOI] [PubMed] [Google Scholar]
- 2.Center for Disease Control and Prevention (CDC) An introduction to epidemiology [Internet] Atlanta (GA): CDC; 2012. [updated 2012 May 18; cited 2014 Nov 10]. Available from: http://www.cdc.gov/ophss/csels/dsepd/ss1978/lesson1/section6.html. [Google Scholar]
- 3.Pearson C, Janz T, Ali J. Mental and substance use disorders in Canada [Internet] Ottawa (ON): Statistics Canada; 2013. [updated 2013 Sep 18; cited 2014 Sep 6]. Available from: http://www.statcan.gc.ca/pub/82-624-x/2013001/article/11855-eng.htm. [Google Scholar]
- 4.Statistics Canada. Canadian Community Health Survey—mental health and well-being [Internet] Ottawa (ON): Statistics Canada; 2011. [updated 2013 Sep 10; cited 2014 Sep 6]. Available from: http://www23.statcan.gc.ca:81/imdb/p2SV.pl?Function=getSurvey&SDDS=5015&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 5.Bromet E, Andrade LH, Hwang I, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:83–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Statistics Canada. Canadian Community Health Survey—mental health stigma and discrimination content module—test (CCHS) Ottawa (ON): Statistics Canada; 2008. [updated 2008 May 5; cited 2014 Aug 19]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5152&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 8.StataCorp Stata, version 121 [software] College Station (TX): StataCorp; 2012. [Google Scholar]
- 9.Streiner DL, Patten SB, Anthony JC, et al. Has lifetime prevalence reached the end of its life? A review of the concept. Int J Methods Psychiatr Res. 2010;18:221–228. doi: 10.1002/mpr.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takayanagi Y, Spira AP, Roth KB, et al. Accuracy of reports of lifetime mental and physical disorders: results from the Baltimore Epidemiological Catchment Area study. JAMA Psychiatry. 2014;71(3):273–280. doi: 10.1001/jamapsychiatry.2013.3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moffitt TE, Caspi A, Taylor A, et al. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychol Med. 2010;40(6):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 13.Wells JE, Browne MA, Scott KM, et al. Prevalence, interference with life and severity of 12 month DSM-IV disorders in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):845–854. doi: 10.1080/j.1440-1614.2006.01903.x. [DOI] [PubMed] [Google Scholar]
- 14.Ferrari AJ, Somerville AJ, Baxter AJ, et al. Global variation in the prevalence and incidence of major depressive disorder: a systematic review of the epidemiological literature. Psychol Med. 2013;43(3):471–481. doi: 10.1017/S0033291712001511. [DOI] [PubMed] [Google Scholar]
- 15.Bebbington PE, Dunn G, Jenkins R, et al. The influence of age and sex on the prevalence of depressive conditions: report from the National Survey of Psychiatric Morbidity. Psychol Med. 1998;28:9–19. doi: 10.1017/s0033291797006077. [DOI] [PubMed] [Google Scholar]
- 16.Ali JS, McDermott S, Gravel RG. Recent research on immigrant health from statistics Canada’s population surveys. Can J Public Health. 2004;95(3):I9–I13. doi: 10.1007/BF03403659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 18.Alonso J, Angermeyer MC, Bernert S, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004;(420):21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 19.Patten SB. Progress against major depression in Canada. Can J Psychiatry. 2002;47:775–780. doi: 10.1177/070674370204700810. [DOI] [PubMed] [Google Scholar]
- 20.Simpson KR, Meadows GN, Frances AJ, et al. Is mental health in the Canadian population changing over time? Can J Psychiatry. 2012;57(5):324–331. doi: 10.1177/070674371205700508. [DOI] [PubMed] [Google Scholar]
- 21.Beck CA, Patten SB, Williams JVA, et al. Antidepressant utilization in Canada. Soc Psychiatry Psychiatr Epidemiol. 2005;40:799–807. doi: 10.1007/s00127-005-0968-0. [DOI] [PubMed] [Google Scholar]
- 22.Beck CA, Williams JVA, Wang JL, et al. Psychotropic medication use in Canada. Can J Psychiatry. 2005;50:605–613. doi: 10.1177/070674370505001006. [DOI] [PubMed] [Google Scholar]
- 23.Patten SB, Beck C. Major depression and mental health care utilization in Canada: 1994 to 2000. Can J Psychiatry. 2004;49:303–309. doi: 10.1177/070674370404900505. [DOI] [PubMed] [Google Scholar]
- 24.Bland RC, Newman SC, Orn H. Help-seeking for psychiatric disorders. Can J Psychiatry. 1997;42:935–942. doi: 10.1177/070674379704200904. [DOI] [PubMed] [Google Scholar]
- 25.Lin E, Parikh SV. Sociodemographic, clinical, and attitudinal characteristics of the untreated depressed in Ontario. J Affect Disord. 1999;53:153–162. doi: 10.1016/s0165-0327(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 26.Slade T, Johnson A, Teesson M, et al. The mental health of Australians 2. Report on the 2007 National Survey of Mental Health and Wellbeing. Canberra (AU): Department of Health and Aging; 2009. [Google Scholar]
- 27.Moffitt TE, Harrington H, Caspi A, et al. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 28.Scott KM, McGee MA, Oakley Browne MA, et al. New Zealand Mental Health Survey Research Team Mental disorder comorbidity in Te Rau Hinengaro: the New Zealand Mental Health Survey. Aust N Z J Psychiatry. 2006;40(10):875–881. doi: 10.1080/j.1440-1614.2006.01906.x. [DOI] [PubMed] [Google Scholar]
- 29.American Psychiatric Association (APA) Diagnostic and statistical manual of mental disorders. 5th ed. Arlington (VA): APA; 2013. [Google Scholar]