Abstract
Objective:
To evaluate trends in the prevalence of major depressive episodes (MDEs) in Canada during the past 2 decades using data collected in a series of national surveys.
Method:
MDE prevalence has been assessed in national surveys that either used a short form version of the Composite International Diagnostic Interview Short Form for Major Depression (CIDI-SFMD) or an adaptation of the World Health Organization’s (full-length) version, World Mental Health (WMH) CIDI. We applied meta-regression methods to adjust for instrument type while also addressing design effects in the individual data sets. Interprovincial differences that might have confounded estimation of national trends were also explored.
Results:
Interprovincial differences were not found to be significant, nor were time by province interactions. Estimates based on the WMH-CIDI were about 1% lower than those using the CIDI-SFMD. There was no evidence of changing prevalence over time, with slope for time, adjusted for assessment instrument, being nearly zero (β = 0.0007, P = 0.24).
Conclusion:
An extensive collection of surveys conducted in Canada between 1994 and 2012 provide an opportunity to examine long-term trends in the prevalence of major depression. MDE prevalence has not changed during this period of time.
Keywords: major depressive episode, major depression, epidemiologic studies, time trends, cross-sectional studies, meta-regression
Abstract
Objectif :
Évaluer les tendances de la prévalence des épisodes de dépression majeure (EDM) au Canada durant les 2 dernières décennies à l’aide des données recueillies dans une série d’enquêtes nationales.
Méthode :
La prévalence des EDM a été évaluée dans les enquêtes nationales qui utilisaient soit une version abrégée de l’entrevue composite diagnostique internationale pour la dépression majeure (CIDI-SFMD), soit une adaptation de la version (intégrale) de l’Organisation mondiale de la santé, World Mental Health (WMH) CIDI. Nous avons appliqué des méthodes de méta-régression pour nous adapter au type d’instrument tout en abordant les effets de la méthodologie sur les ensembles de données individuelles. Les différences interprovinciales qui auraient pu confondre l’estimation des tendances nationales ont aussi été explorées.
Résultats :
Les différences interprovinciales ne se sont pas avérées significatives, pas plus que les interactions de temps par province. Les estimations basées sur la WMH-CIDI étaient d’environ 1 % plus faibles que celles utilisant la version CIDI-SFMD. Aucune donnée probante n’indiquait un changement de la prévalence avec le temps, la courbe du temps, corrigée pour l’instrument d’évaluation, étant près de zéro (β = 0,0007, P = 0,24).
Conclusion :
Un ensemble imposant d’enquêtes menées au Canada entre 1994 et 2012 offrent la possibilité d’examiner les tendances à long terme de la prévalence de la dépression majeure. La prévalence des EDM n’a pas changé durant cette période.s
Temporal trends in mental disorder prevalence have been difficult to discern in epidemiologic studies. Small changes made to the fully structured diagnostic interviews used in these studies can have a large impact on prevalence estimates,1 such that repeated surveys are generally not directly comparable. Also, structured diagnostic interviews have undergone revisions over the years, as have the algorithms used to interpret them. As a consequence, despite repeated surveys occurring in several countries, there has been little agreement about whether prevalence is changing. In Canada, a simulation study2 designed as a support tool for policy decisions related to the national mental health strategy adopted an assumption of stable prevalence, using evidence available at the time.3 Since then, additional data sources have become available, in particular a second national mental health survey.4
During the past 2 decades in Canada, the prevalence of MDE has been repeatedly assessed by national studies incorporating 1 of 2 instruments. A short form version of the CIDI major depression module (that is, the CIDI-SFMD5) has been repeatedly incorporated, without modification, into a series of general health surveys starting in 1994. Also, 2 national mental health surveys (the CCHS 1.2 and the CCHS-MH), conducted in 2002 and 2012, used a Canadian adaptation of the WMH-CIDI. While some WMH-CIDI modules were modified for the second survey, the MDE module was not. The objective of this study was to evaluate temporal trends in MDE prevalence while incorporating all of these data sources and using meta-regression to account for the use of the 2 different instruments. We sought to address the question of whether the prevalence of MDE is changing over time.
Methods
Our study used data from 3 sources; the NPHS,6 the general health cycles of the CCHS,7 and 2 mental health–focused iterations of the CCHS (CCHS 1.2 and CCHS-MH).4,8 The NPHS and CCHS are national general health surveys targeting the Canadian household population. The NPHS was a longitudinal study that nevertheless produced cross-sectional data files in 1994, 1996, and 1998.6 This was possible because of a sampling strategy that resulted in the cohort being refreshed with a child and adolescent sample from another survey, so-called buy-in samples from some provinces and the recalculation of sampling weights for use in making cross-sectional estimates. The CCHS consists of a series of general health surveys7 as well as topically specialized ones. The general health CCHS surveys often included the CIDI-SFMD.5 The instrument was usually included as optional content, meaning that it was included in the survey interview in some, but not all, provinces. The mental health–focused CCHS surveys, which included a Canadian adaptation of the WMH-CIDI,9 occurred in 2002 and 2012.
Clinical Implications
Perceptions of an epidemic of depression are probably due to increasing awareness of this condition and are not supported by available data.
Several studies have shown that treatment provision for depression, particularly antidepressant use, has increased. This has not been associated with diminishing prevalence of MDEs.
Limitations
All of the diagnostic instruments employed in these studies are vulnerable to inaccuracy because of their inability to incorporate clinical judgment into the diagnostic assessment.
In some surveys, the assessment of MDEs was optional content. Differing trends in various provinces or regions may not have been detected as a result.
Despite design similarities, considerable heterogeneity (beyond that accounted for by instrument type) was observed.
The decision to combine data from these various sources at the survey-estimate level (rather than at the individual level as in a pooled analysis) was motivated by the need to incorporate sampling weights and bootstrap variance estimation to account for design effects, helping to ensure valid estimates of prevalence and of the precision associated with those estimates. The available survey weights were not designed for use in pooled analyses.
Estimates were initially examined graphically using forest plots of the prevalence estimates and associated 95% confidence intervals by province, survey, and year. We examined heterogeneity (I2) and since high levels of heterogeneity (>90%) were observed, meta-analytic estimates were subsequently generated using random effects models. Random effects meta-regression was used to examine changes over time, with adjustment for the measurement strategy employed in the individual surveys. Time was represented in these analyses as years since the initial assessment of MDE prevalence in 1994. This meant that the intercept term in the meta-regression’s linear equation represented a baseline estimate (1994), and the slope term represented change per year. As recommended by Higgins and Thompson,10 permutation tests (with n = 1000 Monte Carlo trials) were used to confirm P values from the meta-regression models. The analyses used Stata’s metan command (StataCorp, release 13; College Station, TX, 2013) and were conducted in the Prairie Regional Data Centre in Calgary.
Results
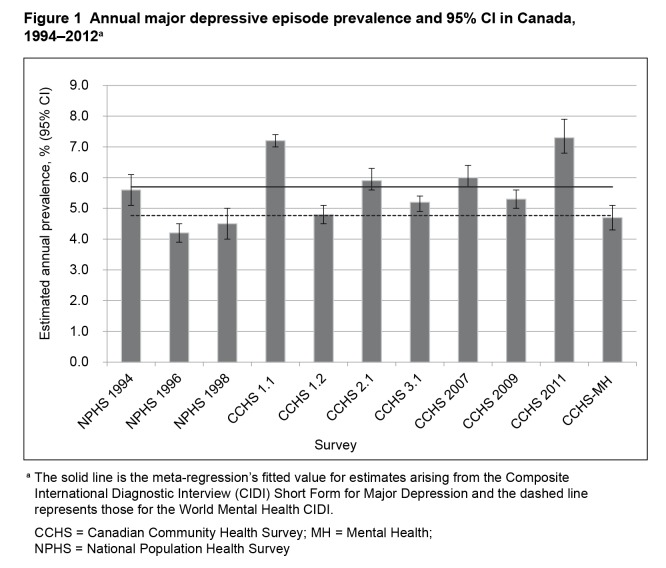
Table 1 summarizes the number of available observations for each of the outcome variables in each survey cycle. Figure 1 presents the annual prevalence estimates and associated 95% confidence interval from each survey. Although considerable heterogeneity is present, there is no visual evidence of increasing prevalence over time.
Table 1.
Sample size availability from NPHS and CCHS cycles
| Survey | CIDI-SFMD | WMH-CIDI |
|---|---|---|
| NPHS 1994 | 16 719 | |
| NPHS 1996 | 70 538 | |
| NPHS 1998 | 14 781 | |
| CCHS 2000 | 128 182 | |
| CCHS 1.2 | 36 789 | |
| CCHS 2003 | 50 751 | |
| CCHS 2005 | 68 389 | |
| CCHS 2007/08 | 46 739 | |
| CCSH 2009/10 | 58 128 | |
| CCHS 2011/12 | 21 636 | |
| CCHS-MH | 24 954 |
CCHS = Canadian Community Health Survey;
CCHS 1.2 = CCHS: Mental Health and Well-being (conducted in 2002);
CCHS-MH = CCHS—Mental Health (conducted in 2012);
CIDI-SFMD = Composite International Diagnostic Interview Short Form for Major Depression;
NPHS = National Population Health Survey;
WMH-CIDI = World Mental Health Composite International Diagnostic Interview
Figure 1.
Annual major depressive episode prevalence and 95% CI in Canada, 1994–2012a
aThe solid line is the meta-regression’s fitted value for estimates arising from the Composite International Diagnostic Interview (CIDI) Short Form for Major Depression and the dashed line represents those for the World Mental Health CIDI.
CCHS = Canadian Community Health Survey; MH = Mental Health; NPHS = National Population Health Survey
Prevalence estimates sometimes appeared to be lower in Newfoundland and Labrador, Prince Edward Island, and Quebec, compared with other provinces, but these effects were neither consistent over time nor statistically significant when evaluated in meta-regression models. Also, there was a tendency for the estimates based on the WMH-CIDI to be slightly lower than many of those based on the CIDI-SFMD (Figure 1), an effect that did not, however, achieve statistical significance (random effects meta-regression, β = −0.009, t = 1.19, df = 1, P = 0.26). Lower prevalence with the WMH-CIDI was expected owing to its application of more detailed probes for symptom severity and persistence when compared with the CIDI-SFMD.
The overall pooled annual prevalence was 5.5% (95% CI 4.8% to 6.2%), with an associated tau2 value from the random effects model of 0.0001 and an I2 of 97.8%. The addition of time to this model led to an estimated coefficient that was near zero at 0.0004 (95% CI −0.0009 to 0.001) and which was not significantly different from the null value of zero (t = 0.82, df = 1, P = 0.43). Inclusion of time did not decrease the I2 value, which was 98.0% in this model. In a model containing the time variable, an indicator representing use of the WMH-CIDI instrument again suggested lower prevalence by about 1% with this instrument (β = 0.012), but remained nonsignificant (t = 1.54, df = 1, P = 0.16). With adjustment for measurement instrument, the time coefficient (β = 0.0007) remained very close to zero and remained nonsignificant (t = 1.28, df = 1, P = 0.24). Because lower estimates with the WMH-CIDI were expected, the meta-regression depicted in Figure 1 includes the relevant indictor term despite its lack of statistical significance. Results using the permutation test confirmed these results, with neither time (P = 0.43) nor measurement instrument (P = 0.31) being statistically significant. The 95% confidence interval for time, adjusted for measurement strategy, was −0.0006 to 0.0021. In this model, the I2 value was much the same as that for the overall prevalence estimate at 98.0%.
Discussion
A perception has emerged that the prevalence of this MDE may be increasing over time. This perception may be attributable to an increase in antidepressant use and an increased frequency of self-reported diagnoses of depression,3 as well as to a greater awareness of depression within the general public. However, examination of prevalence during a long period of time in a set of nationally representative samples in our study did not identify an increase in prevalence.
A limitation of the analysis concerns the precision of the estimated time effect. The slope coefficient for time, adjusted for measurement instrument, was 0.0007, indicating a nonsignificant increase of slightly less than one-tenth of 1% per year. The upper bound of the confidence interval indicated that the data are consistent with an increase as large as 0.2% per year, which could be of public health significance as it could lead to substantial changes over time. However, the effect was not statistically significant in this analysis. The null hypothesis of a zero slope was not rejected at the P < 0.05 level of confidence.
The meta-analytical methods employed weight the pooled estimates according to the inverse of their variance. However, they do not give more weight to the presumably superior measurement instrument, the WMH-CIDI. Therefore, it is important to note that the point estimate in 2012 was 4.7%, very similar to the 4.8% estimate of the 2002 survey, which also used the WMH-CIDI. This observation provides additional support for the conclusion that the annual prevalence of this condition is stable.
Considerable heterogeneity was observed across these studies. This suggests that some factors other than chance had an impact on the prevalence estimates. These factors are unknown but may relate to societal conditions, regional differences, or to measurement artifacts, such as the relative placement of the MDE assessment modules in the survey interviews. However, temporal trends do not seem to be contributing to this heterogeneity.
Acknowledgments
Dr Patten is a Senior Health Scholar with Alberta Innovates, Health Solutions (AIHS). At the time of this analysis, Kirsten Fiest is supported by a PhD Studentship from AIHS. The estimates reported in this paper derive used data collected by Statistics Canada, but the analysis and results are the sole responsibility of the authors and do not reflect the views of Statistics Canada. This work was supported by an operating grant from the Canadian Institutes of Health Research (MOP-130415) and by the Hotchkiss Brain Institute.
Abbreviations
- CCHS
Canadian Community Health Survey
- CCHS 1.2
CCHS Mental Health and Well-being (2002)
- CCHS-MH
CCHS—Mental Health (2012)
- CIDI-SFMD
Composite International Diagnostic Interview Short Form for Major Depression
- MDE
major depressive episode
- NPHS
National Population Health Survey
- WMH-CIDI
World Mental Health Composite International Diagnostic Interview
References
- 1.Narrow WE, Rae DS, Robins LN, et al. Revised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimates. Arch Gen Psychiatry. 2002;59:115–123. doi: 10.1001/archpsyc.59.2.115. [DOI] [PubMed] [Google Scholar]
- 2.Patten SB, Lin E, Martens PJ, et al. Synthesis through simulation: insights on the epidemiology of mood and anxiety disorders in Canada. Can J Psychiatry. 2012;57(12):765–771. doi: 10.1177/070674371205701209. [DOI] [PubMed] [Google Scholar]
- 3.Simpson KR, Meadows GN, Frances AJ, et al. Is mental health in the Canadian population changing over time? Can J Psychiatry. 2012;57(5):324–331. doi: 10.1177/070674371205700508. [DOI] [PubMed] [Google Scholar]
- 4.Statistics Canada . Canadian Community Health Survey—mental health and well-being [Internet] Ottawa (ON): Statistics Canada; 2013. [cited 2014 Jun 24]. Available from: http://www23.statcan.gc.ca:81/imdb/p2SV.pl?Function=getSurvey&SDDS=5015&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 5.Kessler RC, Andrews G, Mroczek D, et al. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF) Int J Methods Psychiatr Res. 1998;7:171–185. [Google Scholar]
- 6.Statistics Canada . National Population Health Survey—household component—cross-sectional (NPHS) [Internet] Ottawa (ON): Statistics Canada; 2013. [cited 2014 Jun 24]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3236&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 7.Statistics Canada . Canadian Community Health Survey—annual component [Internet] Ottawa (ON): Statistics Canada; 2013. [cited 2014 Jun 24]. Available from: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&lang=en&db=imdb&adm=8&dis=2. [Google Scholar]
- 8.Gravel R, Béland Y. The Canadian Community Health Survey: mental health and well-being. Can J Psychiatry. 2005;50:573–579. doi: 10.1177/070674370505001002. [DOI] [PubMed] [Google Scholar]
- 9.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13:83–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins JP, Thompson SG. Controlling the risk of spurious findings from meta-regression. Stat Med. 200415;23(11):1663–1682. doi: 10.1002/sim.1752. [DOI] [PubMed] [Google Scholar]