Abstract
Background & objectives
Six million US children have no health insurance, and substantial racial/ethnic disparities exist. The design, methods, and baseline characteristics are described for Kids’ Health Insurance by Educating Lots of Parents (Kids’ HELP), the first randomized, clinical trial of the effectiveness of Parent Mentors (PMs) in insuring uninsured minority children.
Methods & research design
Latino and African-American children eligible for but not enrolled in Medicaid/CHIP were randomized to PMs, or a control group receiving traditional Medicaid/CHIP outreach. PMs are experienced parents with ≥ 1 Medicaid/CHIP-covered children. PMs received two days of training, and provide intervention families with information on Medicaid/CHIP eligibility, assistance with application submission, and help maintaining coverage. Primary outcomes include obtaining health insurance, time interval to obtain coverage, and parental satisfaction. A blinded assessor contacts subjects monthly for one year to monitor outcomes.
Results
Of 49,361 candidates screened, 329 fulfilled eligibility criteria and were randomized. The mean age is seven years for children and 32 years for caregivers; 2/3 are Latino, 1/3 are African-American, and the mean annual family income is $21,857. Half of caregivers were unaware that their uninsured child is Medicaid/CHIP eligible, and 95% of uninsured children had prior insurance. Fifteen PMs completed two-day training sessions. All PMs are female and minority, 60% are unemployed, and the mean annual family income is $20,913. Post-PM-training, overall knowledge/skills test scores significantly increased, and 100% reported being very satisfied/satisfied with the training.
Conclusions
Kids’ HELP successfully reached target populations, met participant enrollment goals, and recruited and trained PMs.
Keywords: Child, adolescent, medically uninsured, public health, Hispanic Americans, African Americans
1. Introduction
Since the inception of the Children’s Health Insurance Program (CHIP) in 1997, the combination of CHIP and Medicaid has been credited with reducing the proportion of uninsured children in the US by 47% [1]. Nevertheless, there are still 5.9 million uninsured children in America, equivalent to one in 13 children without health insurance [2]. Furthermore, millions of these children are eligible for Medicaid/CHIP, but remain uninsured. Between 62–72% of all uninsured US children—equivalent to up to 4.2—million are eligible for but not enrolled in Medicaid/CHIP [3,4,5,6]. Among low-income children, 84% of the uninsured are Medicaid/CHIP eligible, but not enrolled [7].
Research documents many reasons why Medicaid/CHIP-eligible children remain uninsured. One study revealed 52 barriers to enrollment comprising 11 domains, including lack of knowledge about Medicaid/CHIP, failure to apply, language barriers, immigration status, income, income verification, misinformation from insurance representatives, system problems, hassles, decisions that were still pending, and family mobility [8]. Multiple studies document that lack of knowledge about the Medicaid and CHIP programs is one of the most important barriers to enrolling eligible uninsured children [8,9,10,11,12,13]. A Kaiser Commission on Medicaid and the Uninsured study [9] found that only 26% of parents of eligible uninsured children said that they had ever talked to someone or received information about Medicaid enrollment, and another study [7] revealed that 27% of parents of uninsured eligible children had not heard of Medicaid or CHIP. Hassles (i.e., a burdensome enrollment process) also have been identified in several studies as an enrollment barrier [8–13,14]; other recurrent enrollment barriers include language barriers [7–9;13], income and income verification [8–10], and mobility [8,12].
Among uninsured children in America, there are dramatic racial/ethnic disparities. In contrast to an uninsured rate of only 5% among white children, Latino children, at 12%, and African-American children, at 8%, have a greater risk of being uninsured [2]. Indeed, Latino and African-American children account for 56% of all uninsured children in America, even though they comprise only 42% of the total population of US children, and the number of uninsured Latino children (2.5 million) is approximately the same as the number of uninsured white children, even though white children outnumber Latino children by more than 2:1 in the US [15]. Among the 2.1 million poor US children without health insurance, Latino and African-American children account for 70% of the uninsured, equivalent to 1.5 million children [16].
Parent Mentors (PMs) are a uniquely tailored type of community health worker for children, consisting of parents who already have children with a particular health condition or risk who leverage this relevant experience, together with additional training, to assist and counsel other parents of children with the same health condition/risk. Herein we describe the design, methods, and baseline participant characteristics of the Kids’ Health Insurance by Educating Lots of Parents (Kids’ HELP) trial, the first randomized, clinical trial (RCT) of the effectiveness of PMs in insuring uninsured minority children.
2. Methods
2.1. Study aims
The specific aims of the Kids’ HELP trial are to conduct an RCT to evaluate whether:
PMs are more effective than traditional Medicaid and CHIP outreach and enrollment methods in insuring eligible, uninsured Latino and African-American children
PMs are more cost-effective than traditional Medicaid and CHIP outreach and enrollment methods in insuring eligible, uninsured Latino and African-American children
Compared with all study children at baseline and children uninsured throughout the study, uninsured children who obtain health insurance experience improvements in access to healthcare, health status, quality of life, use of health services, the quality of pediatric care, parental satisfaction with care, and parental-reported financial burden, with reductions in unmet healthcare needs, missed school and parental work days, emergency department (ED) visits, and hospitalizations.
2.2. Conceptual framework
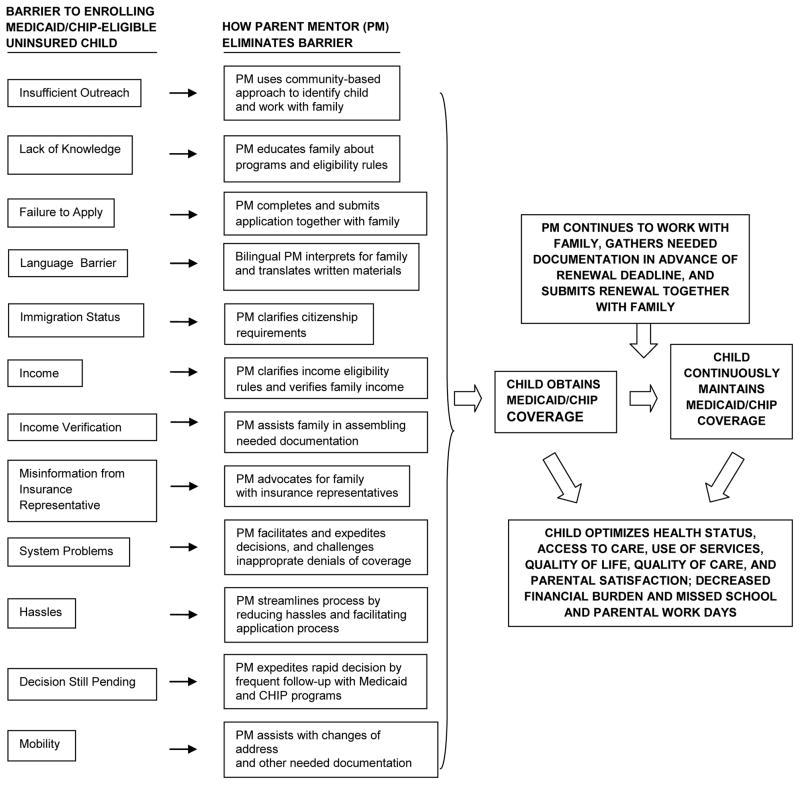
The Kids’ HELP trial builds upon a solid evidence base of relevant previous research. Prior qualitative research resulted in a taxonomy of 11 domains consisting of 52 barriers to enrollment of eligible uninsured children [8]. A subsequent RCT by our research team demonstrated that community case-management strategies targeting these barriers can lead to uninsured Latino children obtaining and maintaining health insurance coverage [17]. Another RCT by our team documented that PMs can be a highly efficacious and cost-effective mechanism for eliminating racial/ethnic disparities in asthma for minority children [18]. The conceptual framework for the Kids’HELP trial incorporates evidence from these three studies, highlighting the barriers targeted by the PM intervention, strategies used to eliminate the barriers and maintain insurance coverage, and the anticipated benefits that will be assessed for children’s health and healthcare (Fig. 1).
Fig. 1.
Conceptual framework for Kids’ HELP trial, highlighting the barriers targeted by the PM intervention, strategies used to eliminate the barriers and maintain insurance coverage, and the anticipated benefits that will be assessed for children’s health and healthcare.
2.3. Study population
The study population is uninsured Latino and African-American children residing in Dallas County who are eligible for Medicaid or CHIP but not enrolled in either program. Dallas County is an ideal setting for the proposed study, because the most recent available information at the time that the study was initiated revealed: 1) of the 184,196 uninsured children in the county, 166,013, or 90%, are Latino or African-American [19]; 2) 45.1% of Latino and 19.5% of African-American children in the county are uninsured, compared with 10.7% of white children [19]; and 3) in county regions with highest concentrations of Latinos and African-Americans (West Dallas and South Dallas), 69–71% of households have family incomes ≤ 200% of the federal poverty threshold [20], which was the income cut-off for CHIP eligibility in Texas.
2.4. Eligibility criteria
The eligibility criteria for enrollment in this study are:
The parent/guardian is a primary caretaker of at least one child 0–18 years old who currently has no health insurance
The parent/guardian self-identifies the uninsured child as Hispanic/Latino, African-American/black, or both
The uninsured child is eligible for either Medicaid or CHIP
The parent/guardian is willing to be contacted monthly by telephone, or in the form of a home visit (if no functioning telephone is present in the household).
Eligibility Criterion 1 was chosen to target the spectrum of uninsured children, from those who have been continuously uninsured for the prior year or longer, to the discontinuously/episodically uninsured who currently have no insurance, but were insured for part of the prior year. Research documents that children uninsured for part of the year have comparable outcomes to those uninsured for the full year, in terms of access to healthcare, unmet healthcare needs, and use of health services [21]. The research team queries appropriate state Medicaid and CHIP program representatives at the Texas Health and Human Services Commission to verify that the child does not currently have active Medicaid or CHIP coverage.
Eligibility Criterion 2 was chosen because self-identification of race/ethnicity by research participants has been shown to be feasible, efficient, accurate, and to result in lower rates of missing and unusable data than do standard questions [22].
For Eligibility Criterion 3, the research staff determines whether the uninsured child qualifies for Medicaid or CHIP in Texas. Eligibility criteria for both Medicaid and CHIP in Texas include that the child must be: 1) 18 years old or younger; 2) a Texas resident; and 3) a U.S citizen or legal permanent resident [23]. The citizenship or immigration status of the parents does not affect the child’s eligibility and are not reported on the application form. During the recruitment phase of the Kids’ HELP trial, to qualify for Medicaid in Texas, the family income thresholds varied by the child’s age [24]. Infants who had not yet reached their first birthday qualified for Medicaid if the family income was ≤ 185% of the federal poverty threshold; children 1–5 years old qualified for Medicaid if the family income was ≤ 133% of the federal poverty threshold; and children 6–18 years old qualified for Medicaid if the family income was ≤ 100% of the federal poverty threshold. Children receiving Medicaid coverage in Texas during most of the study enrollment period (through December 2013) were required to renew their Medicaid coverage every six months [25], except for those enrolled in the final study enrollment month (January 2014) or in the latter half of 2013 and due for renewal in 2014; for the latter two groups, Medicaid renewal was required annually [26], but with income verification after six months. For a child to qualify for Texas CHIP, the family income must be ≤ 200% of the federal poverty threshold, but above the income thresholds for Medicaid [24], and renewal is required every 12 months [26] (but with an income verification after six months).
Regarding Eligibility Criterion 4, prior work by the research team has established that phone or in-person follow-up with intervention families is crucial to the success of a community-based intervention to insure uninsured children [17,27].
2.5. Recruitment sites and process
Recruitment efforts focused on the three regions with the highest proportions of Latinos and the three regions with the highest proportions of African-Americans in Dallas County [20]. For Latinos, these included: 1) West Dallas, with 67% of the population Latino and 69% with a family income ≤ 200% of the federal poverty threshold [20]; 2) Northwest Oak Cliff, with 43% of the population Latino and 35% with a family income ≤ 200% of the poverty threshold [20]; and 3) East Dallas, with 41% of the population Latino and 39% with a family income ≤ 200% of the poverty threshold [20]. For African-Americans, these regions include: 1) South Dallas, with 77% of the population African-American and 71% with a family income ≤ 200% of the federal poverty threshold [20]; 2) South Oak Cliff, with 60% of the population African-American and 48% with a family income ≤ 200% of the poverty threshold [20]; and 3) West Dallas, with 30% of the population African-American and 69% with a family income ≤ 200% of the federal poverty threshold [20]. Thus, a total of five regions were the focus of recruitment efforts, given that West Dallas has high proportions of both Latinos and African-Americans.
In each of these five communities, study participants were recruited from sites confirmed by our team’s prior research [8,17] to yield many eligible uninsured children and their families willing to take part in research and programs on insuring uninsured children, as well as several new venues: supermarkets, department stores, dollar stores, Goodwill stores, restaurants, public libraries, community centers, food banks, health fairs, Boys and Girls clubs, YMCAs, churches, schools, community outpatient clinics, day-care establishments, Laundromats, apartment complexes, housing projects, homeless shelters, and WIC centers. A total of 198 sites were approached about potentially serving as recruitment venues for Kid’s HELP, of which 97 agreed to participate. After obtaining the permission of business owners, church pastors, homeless shelter staff, or other leaders, trained bilingual research staff who are experienced at working with these communities approached potential participants outside of these establishments, utilizing a protocol similar to that employed in our team’s prior community-based RCT of community-based case management [17]. Research staff explained to each parent/guardian that: 1) we are conducting a study of effective ways to get health insurance for uninsured children; 2) participants will receive a $50 honorarium at the start of the study and a $5 honorarium for each of 12 brief monthly follow-up contacts (increased to $10 for the longer six- and 12-month surveys), for a total of $120 by the end of the study; 3) depending on the randomization, some parents will get a PM free-of-charge whose job will be to help families get health insurance for their child, while other parents will get no PM and will just be contacted monthly; 4) all parents will be contacted monthly to find out whether their child has health insurance and to evaluate the child’s health and healthcare; 5) all information shared with us in this study is strictly confidential, and will not be available to any federal, state, or local official; and 6) participation is completely voluntary. The parents are then asked whether they are interested in participation. For more details on participant candidate screening, please see the following video clip: http://www.mediafire.com/watch/qach852og44amph/Recruiting_Article_2.mp4
2.6. Study protocol
Parents interested in participating in the study first signed a detailed written consent form that was approved by the University of Texas Southwestern Medical Center’s Institutional Review Board. Interested parents/guardians then completed a brief, orally administered screening questionnaire (in English or Spanish, according to parental preference) which had been used in the research team’s prior work [17] to confirm eligibility, determine baseline characteristics, and record contact information. Orally administering all study instruments avoided any literacy issues for the parents/guardians.
Data on baseline characteristics collected using the screening questionnaire included:
Age of parent and child(ren)
Race/ethnicity of parent and child(ren) (by self-identification)
Marital status of parent
Educational attainment of parent
Employment status of parent and significant other (if currently living in household)
Annual combined family income
Health-insurance coverage for the parent/guardian and significant other (when applicable)
Number of years parent has lived in US (for those not born in US)
Primary language spoken at home and English proficiency of parent (if primary language spoken at home not English)
Citizenship status of parent
Contact information collected for each family enrolled in the study included: the names of the parent and child(ren), whether there is a functioning telephone in the household, home and cellular telephone numbers, the preferred alternate telephone number of friends or family members (if there is no functioning telephone in the household), and the mailing address.
Research staff then opened the sealed, opaque randomization envelope (see Randomization section below), and informed the parent whether he or she and the child had been assigned to the PM or control group. Parents enrolled in the intervention group received the initial component of the PM intervention (see Intervention section below), including a needs assessment and completion of relevant applications. Parents assigned to the control group received no additional interventions. Parents enrolled in both groups were asked to inform the research staff of the most convenient time for the first monthly follow-up contact, and then were given the $50 honorarium by research staff. For parents who stated that they were not interested in the study at any point in the recruitment process, the numbers of refusals and the reasons for refusal were recorded.
2.7. Randomization
Subjects were allocated using a computer-generated, stratified randomization process. Stratified randomization ensures that compared maneuvers in an RCT are suitably distributed among pertinent subgroups [28]. The pertinent subgroups in this study were the two racial/ethnic groups: Latino and African-American.
The randomization schedule was prepared using computer-generated random numbers. SAS© software (SAS Institute, Cary, NC) was employed by the research team statistician to produce randomization schedules for each of the two strata, using the RANUNI function. Sequentially numbered, opaque, sealed envelopes were produced for each racial/ethnic group, to ensure adequate allocation concealment. Research staff, who did not partake in any aspect of preparation of randomization schedules, opened the envelopes in the presence of enrolled participants to inform them of their group assignment.
2.8. Intervention
PMs are experienced parents who have at least one child currently covered by Medicaid or CHIP. PMs were recruited from June 2011 through August 2013, primarily at the Resident Continuity Clinic at Children’s Medical Center Dallas. This Clinic experiences approximately 11,000 patient visits annually, 94% of whom are covered by Medicaid (86%) or CHIP (8%). One of the authors (ML), who has been an attending pediatrician in the Clinic for two decades, identified potential PM candidates at this clinic. One additional PM was recruited through RCT participant-recruitment activities at a charter school, and four others were recruited based on the recommendation of established PMs. For more details on PM candidate screening, please see the following video clip: https://vimeo.com/95286928. All PM candidates were interviewed by the Program Coordinator (CW) to identify the best candidates for carrying out the intervention. Each PM was hired as a temporary employee and is paid a monthly stipend for each family whom they assist as a PM. PMs and intervention participants are matched by race/ethnicity and zip code (whenever possible). For Latino families, only fluently bilingual Latino PMs are provided, to ensure that study families do not face linguistic barriers to obtaining health insurance for their children.
PMs perform the following functions for intervention-group children and their families: 1) providing information on the types of insurance programs available and the application process; 2) furnishing information and assistance on program eligibility requirements; 3) completing the child’s insurance application together with the parent, and submitting the application for the family; 4) expediting final coverage decisions by early and frequent contact with program representatives for Texas Medicaid and CHIP; 5) acting as a family advocate by being the liaison between the family and the Medicaid and CHIP programs; 6) rectification by contacting Medicaid/CHIP program representatives of situations where a child inappropriately was deemed ineligible for insurance or had coverage inappropriately discontinued; 7) assisting with completion and submission of applications for renewal of coverage; and 8) educating caregivers about how to successfully renew Medicaid/CHIP or reapply after losing benefits. These functions are almost identical to those of community-based case managers who were significantly more successful at insuring uninsured Latino children than traditional Medicaid/CHIP outreach and enrollment strategies in an RCT by our research team [17].
PMs participate in a two-day intensive training session led by the Program Coordinator. The training, which is based on training sessions provided to community case managers in the research team’s prior successful RCT [17], consists of nine sections on: 1) Why health insurance is such an important issue for US Children; 2) the Kids’ HELP trial; 3) how to be a successful PM; 4) PM responsibilities; 5) the Medicaid and CHIP programs; 6) the Medicaid and CHIP application process; 7) the next steps after obtaining Medicaid/CHIP coverage; 8) medical homes; 9) and study paperwork. Full details on the PM training sessions are available elsewhere [29].
The content of the PM training session is detailed in the PM’s Manual (available in both English and Spanish), which was prepared by the PI, Program Coordinator, and other research staff, and is carried by PMs at all times in the field. Additional details on its content are available elsewhere [29]. The sections of the Manual are structured to correspond to the conceptual framework described above (Fig. 1), based on prior research by the research team that resulted in the taxonomy of 11 domains consisting of 52 barriers to enrollment of eligible uninsured children [8], as well as the subsequent RCT by the PI demonstrating that community case-management strategies targeting these barriers can lead to uninsured children obtaining and maintaining health insurance coverage [17]. The obstacles to insuring eligible uninsured children and the corresponding strategies employed by PMs include:
Insufficient Outreach: the PM uses a community-based approach to identify uninsured children and work with the family
Lack of Knowledge: PMs educate families about the Medicaid and CHIP programs and eligibility rules
Failure to Apply: PMs complete and submit the application together with the family
Language Barriers: Bilingual PMs interpret for the family and translate written materials and forms
Immigration Status: PMs clarify Medicaid and CHIP citizenship requirements
Income: PMs clarify income eligibility rules and verify family income
Income Verification: PMs assist families in assembling needed paystubs and other documentation
Misinformation from Insurance Representatives: PMs advocate for families when speaking with the insurance representatives
System Problems: PMs facilitate and expedite decisions and challenge inappropriate denials of coverage
Hassles: PMs streamline the insurance-enrollment process by reducing hassles and facilitating the application process
Decision Still Pending: PMs expedite rapid coverage decisions by frequent follow-up with the Medicaid and CHIP programs
Mobility: PMs assist with changes of address and other needed documentation associated with a move
Renewals: PMs continue to work with the families, gathering needed documentation in advance of renewal deadlines, and complete and submit the renewal application together with the family
Each PM follows the protocol successfully established in the research team’s prior RCT on community case management [17]. The PM fills out the Medicaid or CHIP application together with the parent. The PM contacts the Medicaid or CHIP program one week later, to verify that the application is complete, and to determine whether a decision has been made to cover the child or not. If any forms are incomplete or missing, the PM contacts the parent, obtains the necessary information, and helps with re-submission of the paperwork. If the Medicaid or CHIP program has approved coverage of the child, the PM contacts the parent immediately, and provides any information requested about the new coverage. If the Medicaid or CHIP program has denied coverage for the child, the PM contacts a program official to determine the reason. If the PM considers the denial to be inappropriate, he or she advocates for the parent and child and attempts to resolve the situation. If the Medicaid or CHIP program appropriately rules the child ineligible, the PM contacts the parent to discuss other available insurance options for the child. If the Medicaid or CHIP program makes no coverage decision after one week, the PM contacts the Medicaid or CHIP program at least weekly until a decision is made.
In addition to the two-day training session, PMs received ongoing training from Kids’ HELP research staff on Medicaid, CHIP, outreach, and enrollment. Quarterly PM meetings with research staff also were held to provide PMs with new tools and information to use in assisting intervention-group children and families.
To evaluate whether the PM training program resulted in PMs acquiring the knowledge and skills to insure uninsured children, a 33-item pre-training test was administered to all PMs to assessed their knowledge and skills regarding Medicaid and CHIP, the application process, and medical homes. A 46-item post-test contained the same 33 pre-test items (ordered differently) and 13 Likert-scale questions on training satisfaction.
2.9 Control group
Control-group subjects receive no intervention, because they already have the opportunity to receive the “standard of care” outreach efforts by the Texas Medicaid and CHIP programs. The Texas Health and Human Services Commission (HHSC), which is responsible for the state Medicaid and CHIP programs, launched an outreach and education campaign in 2006–2007 “…to ensure that low-income families are aware of the coverage provided through the Children’s Health Insurance Program (CHIP) and Children’s Medicaid.” The goal of this campaign was to “…emphasize the importance of health insurance and regular preventive care, explain how to apply for coverage and encourage families to complete the renewal process on time to avoid gaps in coverage for their children.” [30] These efforts, as described by HHSC, feature media, back-to-school, and ongoing campaigns that include the use of 1) bilingual radio ads; 2) television ads on Spanish language stations in Dallas/Fort Worth, El Paso, San Antonio, and the Rio Grande Valley; 3) newspaper announcements; 4) messages on buses and bus benches in selected markets; 5) a new website with updated information, an application link, and order forms for materials for community-based organizations; and 6) special outreach to daycare centers that serve low-income children [30]. Thus, although control subjects in this study receive no intervention, HHSC would consider them to have ample opportunity to obtain insurance coverage through their outreach and education campaign. This contrasts with US Census data, which document that Texas continues to have the highest number of uninsured children of any state (approximately one million) [31], and has been either the worst or second worst state for decades in terms of the proportion of uninsured [32]. After study completion, all uninsured controls and their families will continue to have the opportunity to apply for Medicaid or CHIP coverage using state websites and by contacting insurance-program personnel.
2.10. Outcome Measures
The following four primary outcomes are assessed for all participants:
The proportion of children with health insurance is the main outcome. A study child is considered insured once official written notification of insurance is confirmed, either through an electronic or hard copy of the state coverage letter, or via verification from the Texas HHSC.
The number of days from study enrollment to obtaining coverage. Zero time (the point at which the maneuver is imposed) is the date and time of study enrollment. Occurrence of the main outcome event is the date and time of official notification that the child is insured.
The proportion of children with episodic coverage (obtained but then lost insurance coverage). Any child who obtained coverage during the study, but then lost it before study termination, is classified as having had episodic coverage.
Parental satisfaction with the process of obtaining coverage for the child. Parental satisfaction is measured separately for those whose children were successfully insured, and those whose children remained uninsured. Overall parental satisfaction (regardless of whether insurance coverage was obtained) is determined for each maneuver. Parental satisfaction is assessed both using a five-point Likert-scale and open-ended questions. First, parents are asked to select one of five responses to the statement, “I have been satisfied with the process of obtaining health insurance for my child.” The responses include: “strongly agree,” “agree,” “uncertain,” “disagree”, and “strongly disagree.” We also are collecting descriptive information from two open-ended questions: 1) What have you liked most about the process of obtaining health insurance for your child? And 2) What have you liked least about the process of obtaining health insurance for your child?
These outcomes are identical to those assessed in the research team’s prior RCT of community case management [17], and the same instrument is used. Outcomes are monitored for 12 months. Outcomes (1), (2), and (3) are monitored on a monthly basis, beginning one month after enrollment. Outcome (4) is determined in the last monthly contact. Outcomes are assessed by telephone contact or a brief home visit (when a household has no functioning telephone).
Outcomes are monitored by a member of the research staff who is blinded to the subject group assignment and does not participate in the intervention in any way. This RCT thus is single-blinded. Double blinding is not feasible, because by definition, subjects are conspicuously aware of whether they have a PM or not.
A cost-effectiveness analysis (CEA) is being conducted to assess the cost effectiveness and potential cost savings of the intervention, in accordance with methodological principles for conducting economic evaluations detailed by the US Public Health Services Panel on Cost-Effectiveness in Health and Medicine [33,34]. This CEA compares the costs and effectiveness of the PM intervention in obtaining health insurance for the target population with those of the control group that did not receive the PM intervention. The following CEA cost items are monitored and assessed:
Direct healthcare costs are calculated using two sources. First, parents are asked to estimate the total out-of-pocket healthcare costs in the past month. This information include any co-pays or other out-of-pocket costs associated with any ED visits, hospitalizations, intensive care unit stays, and healthcare provider visits by the child. Second, data are collected on use of health services (by parental report, since access to medical records from multiple facilities is not feasible). The costs of each health service received are determined by applying the mean Texas Medicaid or CHIP reimbursement for the specific service.
Health-insurance enrollment fees. Parents are asked monthly whether they obtained any health insurance coverage for their child. For children obtaining coverage, information is collected about the type of health insurance obtained and the associated enrollment fee (if any).
Intervention costs are estimated by summing all program costs for the intervention. These costs include payments to PMs, supply costs, honoraria, and travel expenses associated with PM case-management activities. PMs keep detailed activity and time logs for all program-related activities. This permits calculation of both total time spent per family and a breakdown of time spent per activity. Costs of travel are assessed using standard mileage rates, actual parking costs, or costs of public transit. The cost of PM training will be added to the fixed costs (i.e., time and wage costs) of the intervention.
Indirect costs include missed parental work days and time costs incurred by parents while seeking health insurance for their uninsured children. Parents are asked to estimate the time spent in seeking health-insurance information, completing paperwork, and calling or visiting state offices or private insurers. Time costs are converted to dollars using wage rates. For participants in the labor force, actual wage rates are used, based on self-reported income.
The incremental cost-effectiveness ratio (ICER) will be calculated by subtracting the total costs for the control group from those for the intervention group, and then dividing by the mean difference in the proportion of insured children.
This calculation produces an estimate of the mean cost for increasing health-insurance coverage for the study population by 1%. Given that costs and effectiveness are defined over one year, no discounting will be performed.
The following secondary outcomes are assessed:
Health status is evaluated using two measures: (1) the following validated question from the National Survey of Children’s Health [35]: “In general, how would you describe [CHILD]’s health? Would you say [his/her] health is excellent, very good, good, fair, or poor?” and (2) the following two validated, reliable questions about parental worry about their child’s health, derived from National Institute of Child Health and Human Development Study of Early Child Care and Youth Development: “I worry about my child’s health more than other people worry about their children’s health,” and “During the past 4 weeks, how much emotional worry or concern did your child’s physical health cause you?” [36]
Quality of life for the child, using the Pediatric Quality of Life Inventory Version 4.0 Generic Core Scales (PedsQL). This 23-item instrument measures parent-reported health-related quality of life in children 2–18 years old [37]. It employs a five-point response scale, and addresses four domains of functioning: physical, emotional, social, and school. It has been shown to be valid and reliable, and correlates with measures of morbidity and illness burden [37].
Access to healthcare is assessed using validated questions from longstanding national surveys and state surveys [35,38,39,40,41,42]. The following domains are addressed: usual source of sick care, usual source of preventive care, (including specialty care), usual source of sick care is same as usual source of preventive care, child has a regular (personal) doctor or nurse, having 24-hour telephone coverage for sick care, usually receives an appointment for the child the same or next day after the parent calls, difficulty getting an appointment, difficulty getting a medical person on the phone, the travel time to the usual source of care, access to interpreter services (when applicable), ease of getting all healthcare needed, and ease of seeing a healthcare provider for routine, acute, and subspecialty care.
Unmet healthcare needs are evaluated using previously published domains and questions [35,40] regarding unmet needs for any health service; specialty care; mental healthcare; acute care; preventive care; dental care; prescription medications; vision care; physical, occupational, or speech therapy; ED care; and other care (substance abuse treatment/counseling, home healthcare, eyeglasses/vision care, hearing aids/hearing care, or medical equipment/supplies).
Use of health services is assessed using validated questions from longstanding national surveys and state surveys [43,44]. Outcomes assessed include primary-care visits, preventive-care visits, sick visits, chronic illness visits, specialty-care visits, ED visits, and hospitalizations in the prior month and prior year (at the final 12-month follow-up assessment).
The quality of pediatric care is appraised by parental report, using validated questions from the Consumer Assessment of Healthcare Providers and Systems [45]. Parents are asked to rate the overall quality of their children’s care using a Likert scale, as well as the quality of primary care, preventive care, specialty care, and acute care; the waiting time to see the provider at the usual source of care also is examined.
Parental satisfaction with care is measured using validated questions derived from the National Survey of Early Childhood Health [44]. We assess overall satisfaction with care, as well as satisfaction with primary care, preventive care, specialty care, acute care, and hospital care (when applicable).
Parental-reported financial burden is evaluated using validated questions from national, state, and regional surveys [39,42,46]. Questions from the National Survey of Children with Special Healthcare asked (in slightly modified form) include: (1) Has (CHILD)’s health conditions or healthcare caused financial problems for your family?; (2) Have you or other family members cut down on the hours you work to provide healthcare for (CHILD)? (3) Have you needed additional income to cover (CHILD)’s medical expenses? and (4) Have you or other family members stopped working because of (CHILD)’s health conditions or healthcare? In addition, we inquire about how much the parent paid out-of-pocket for the child’s healthcare and for prescriptions in the last month and last year (at the final 12-month follow-up). Parents also are asked to rate the financial burden related to their child’s health and healthcare over the past month and year (at the final 12-month follow-up).
Missed school days due to illness or injury are assessed by parental report using a question from the National Health Interview Survey [47] which also was used in the research team’s prior parent mentor RCT for minority children with asthma [18].
Missed parental work days due to child’s illness or injury are assessed by parental report using a modified question from the National Health Interview Survey [47] which also was used in the research team’s prior parent mentor RCT for minority children with asthma [18].
All 10 of these secondary outcomes are monitored at baseline, the six-month follow-up visit, and the 12-month follow-up visit. Table 1 summarizes the study outcomes and details on the frequency and timing of assessment by the blinded outcomes assessor.
Table 1.
Kids’ HELP trial outcomes, with details on the frequency and timing of assessment by the blinded outcomes assessor
| Outcome | Follow-Up Month (After Enrollment) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
| 1.1: Child obtained health insurance | |||||||||||||
| 1.2: # of days from study enrollment to obtaining insurance | |||||||||||||
| 1.3: Episodic coverage (obtained but then lost insurance) | |||||||||||||
| 1.4: Parental satisfaction with coverage process | |||||||||||||
| 2.1: Direct healthcare costs | |||||||||||||
| 2.2: Health insurance enrollment fees | |||||||||||||
| 2.3: Intervention costs | |||||||||||||
| 2.4: Indirect costs (missed parental work days and time costs) | |||||||||||||
| 3.1: Health status of child | |||||||||||||
| 3.2: Quality of life for child | |||||||||||||
| 3.3: Access to healthcare | |||||||||||||
| 3.4: Unmet healthcare needs | |||||||||||||
| 3.5: Use of health services | |||||||||||||
| 3.6: Quality of pediatric care | |||||||||||||
| 3.7: Parental satisfaction with care | |||||||||||||
| 3.8: Parental-reported financial burden | |||||||||||||
| 3.9: Missed school days due to illness or injury | |||||||||||||
| 3.10: Missed parental work days due to child’s illness or injury | |||||||||||||
2.11. Analyses
2.11.1. Power and sample size calculations
We aimed to recruit an initial sample size of 150 children in each study group, based on sample size calculations using a power of 80%, an alpha = .05, and the hypothesis that approximately 15% of the control group and a minimum of 35% of the intervention group will be insured at study’s end (i.e., a delta = 20%). A sensitivity analysis was performed to determine the impact on the sample size of varying the insured rate in the control group from as little as 10% to as high as 55%. This sensitivity analysis reveals that a sample size of 150 for each group would be more than sufficient (holding fixed a power = 80%, α = .05, and δ = 20%) across the full range for this 45% margin of error for the insurance rate, and could compensate for an attrition rate of from 29% to 52%.
Using a power = 80%, α = .05, and δ = 20%, a sample size of 150 in each group allows detection of differences between the intervention and control groups in other primary outcomes as small as 28.3 days for time to obtain insurance, as little as 16.2% for the difference in the proportion continuously insured rate, and 0.4 points on the Likert-scale score for parental satisfaction for the process of obtaining child’s insurance. These minimum differences were calculated in standard power analyses using reference means and standard deviations from the research team’s prior work on the effects of community-based case managers on insuring uninsured children [17].
2.11.2. Analytical Methods, Potential Confounding, Attrition, and Quality Control
The following analytic methods are being used to evaluate the main study questions and address potential confounding, attrition, missing data, and quality control issues:
Step I: The statistician and research technicians perform data entry, coding, and cleaning. Data are double-entered independently by two research staff, to ensure data-entry quality and accuracy. Univariate analyses are performed to identify missing values, attrition, and outliers. Missing values are handled using relative imputing methods, such as listwise and pairwise deletion, mean substitution, raw maximum likelihood, and multiple imputation (depending on the missing value pattern).
Step II: Baseline sociodemographic characteristics for the two study groups are compared to ensure equivalency. Percentages are used for categorical data, and means (with standard deviations) and medians (with ranges) for continuous data. The t-test and Wilcoxon rank-sum test are used to examine differences between the control and intervention groups in the continuous characteristics. The Pearson’s χ2 test is used to test the difference in categorical outcomes. Two-tailed P values are reported, and a P < .05 considered to be statistically significant. If significant differences are found in baseline characteristics, analyses will be suitably adjusted using both stratification and multivariable methods.
Step III: Bivariate and correlation analyses will be used to identify potential independent variables for use in multivariable analyses. Known and potential prognostic factors of a child’s insurance status (race/ethnicity, family income, parents’ marital status, employment status, English proficiency, highest level of education, and parental immigration status) will be examined in relation to group assignment (intervention vs. control) and the outcome measures. Bivariate analyses will also be conducted to evaluate the associations between group assignment and the outcome measures. The Pearson’s χ2 test, t-test, ANOVA, and the nonparametric Wilcoxon rank-sum test will be performed for bivariate analyses. Parental satisfaction with the process of obtaining insurance will be analyzed by coding the five-point Likert scale results both as a categorical variable (using theχ2 test) and as a continuous variable (using the t test).
Step IV: Multivariable analyses (multiple linear and logistic regression modeling) will be performed for each of the outcomes to adjust for differences in any baseline sociodemographic characteristics or potential prognostic factors. Generalized estimating equations for binary data with logit link functions will be performed to examine time trends. A generalized estimated equation (GEE) approach will be employed to adjust for multiple measurements and clustering by family. Stepwise model selection will be done using SAS. Analysis of the number of days from study enrollment to obtaining coverage will be performed using the Kaplan-Meier method. Potential bias caused by systematic censoring will be examined when comparing the number of censored observations in the intervention and control groups. For those who do not obtain insurance and drop out or withdraw early from the study, the dropout and withdrawal reasons will be evaluated. Analyses of the number of days from study enrollment to obtaining coverage will then be calculated with and without early dropouts and withdrawals to determine whether or not bias exists, and if so, to what extent. An adjusted cumulative incidence curve for the time to obtaining insurance also will be plotted.
Step V: A cost-effectiveness evaluation will be conducted to assess the incremental cost associated with improving access to health insurance in the target population. The incremental cost-effectiveness ratio (ICER) will be computed by subtracting the total costs for the control group from those for the intervention group, and then dividing by the mean difference in the proportion of uninsured children. The main categories for the costs of intervention group includes personnel, payments to PMs, the cost of purchased supplies, honoraria payments to participants enrolled in the study, training costs, and healthcare costs. The indirect costs include the changes in time costs incurred by parents seeking health insurance, and missed parental work days. Time cost will be converted to dollars using wage rates. Total costs for the control group only include the healthcare costs and the indirect time costs, obtained in the same manner as for the intervention group.
3. Results
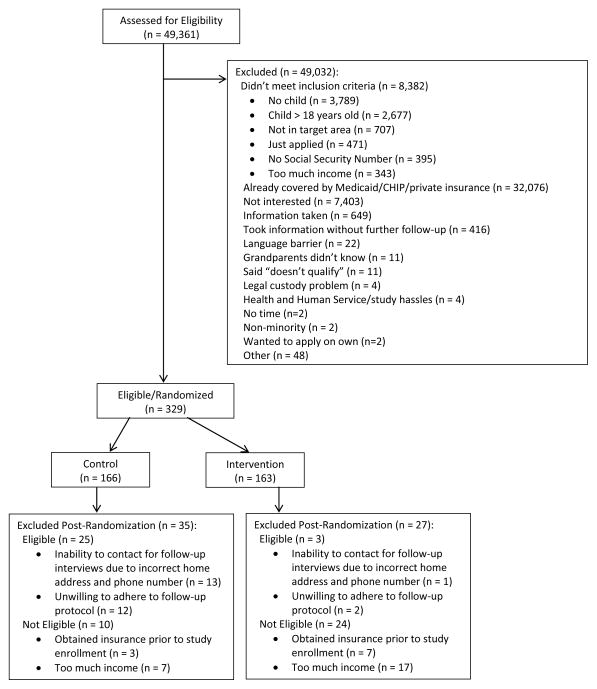
Recruitment occurred from May 2, 2011, until January 30, 2014. A total of 49,361 potential caregivers were screened for study eligibility (Fig. 2). Exclusions occurred for 49,032 candidates, because of failure to meet inclusion criteria, the caregiver’s child already had Medicaid or CHIP coverage, the caregiver was not interested in participating, and several other less frequent reasons, including no time for the study, and legal custody issues. The final number of subjects who fulfilled eligibility criteria and were randomized was 329, with allocation of 166 to the control group and 163 to the PM intervention. Post-randomization, 35 subjects from the control group and 27 from the intervention group were excluded, due to inability of the staff to contact the family because of incorrect addresses and phone numbers, parental unwillingness to adhere to the follow-up protocol, the child obtaining health insurance prior to study enrollment, or having an annual family income which exceed the maximum to qualify for Medicaid or CHIP. The baseline characteristics of these 62 excluded subjects will be compared to those who continued in the trial to determine whether there are any significant intergroup differences. Because a mean attrition rate of 40% was built into the power and sample-size calculations, and the current attrition rate is only 11%, the post-randomization-exclusion sample sizes of 131 in the control group and 136 in the intervention groups are more than adequate to power the study, even with ongoing attrition, as a minimum of 90 subjects is needed in each group to meet sample-size requirements.
Fig. 2.
Summary of participant recruitment flow for the Kids’ HELP trial.
The mean age of the sample of 267 children currently enrolled in the Kids’ HELP trial is seven years old, ranging from 1–18 years old (Table 2). There are equal proportions of male and female children; approximately two-thirds are Latino and one-third African-American, and 95% of children were born in the US. The mean age of the children’s primary caregiver is 32 years old, ranging from 17–75 years old, and 96% are female. Among the Latino caregivers, almost three-quarters are Mexican-American, and among the African-American caregivers, most did not know their African-American subgroup origin, but the highest proportion (14%) was of South African ethnicity. Approximately 40% of the caregivers were born in the US, English was the primary language spoken at home for almost half of households, and about one-third of caregivers have limited English proficiency. Almost 40% of the caregivers are married and living with the spouse, with the remainder single, separated, in a common-law marriage, divorced, living with a partner, or widowed. Almost half of caregivers are not high-school graduates, and over half are unemployed. The mean annual combined family income is $21,857, ranging from $1,440 to $64,000, and the mean number of children and adults in the household was 2.3 and 2.1, respectively.
Table 2.
Selected sociodemographic characteristics of uninsured minority children and their caregivers (N = 267) in the Kids’ HELP trial.
| Characteristic | Mean or % |
|---|---|
|
| |
| Age of child (years), mean (range) | 7.3 (1, 18) |
|
| |
| Gender of child | |
| Male | 50% |
| Female | 50% |
|
| |
| Race/ethnicity of child | |
| Latino | 65% |
| African-American | 35% |
|
| |
| Child born in US | 95% |
|
| |
| Age of caregiver (years), mean (range) | 32.2 (17, 75) |
|
| |
| Gender of primary caregiver | |
| Female | 96% |
| Male | 4% |
|
| |
| Race/ethnicity of caregiver | |
| Latino | 64% |
| Argentine | 1% |
| Costa Rican | 0.5% |
| Honduran | 2% |
| Mexican | 73% |
| Puerto Rican | 0.5% |
| Salvadoran | 2% |
| Spanish | 0.5% |
| Venezuelan | 0.5% |
| Latino subgroup unknown | 20% |
| African-American | 34% |
| Comoros | 2% |
| Egypt | 1% |
| Ethiopia | 1% |
| Kenya | 1% |
| Mali | 1% |
| Nigeria | 2% |
| South Africa | 14% |
| Jamaica | 1% |
| Brazil | 1% |
| Cuba | 1% |
| African-American subgroup unknown | 75% |
| White/Caucasiana | 2% |
|
| |
| Caregiver born in US | 40% |
|
| |
| Primary language spoken at home is English | 45% |
|
| |
| Primary caregiver has limited English proficiency | 32% |
|
| |
| Marital status of primary caregiver | |
| Married, living with spouse | 39% |
| Single | 30% |
| Married, separated from spouse | 13% |
| Common-law marriage | 7% |
| Divorced | 6% |
| Living with partner | 4% |
| Widowed | 1% |
|
| |
| Primary caregiver not high-school graduate | 43% |
|
| |
| Primary caregiver unemployed | 53% |
|
| |
| Mean combined annual family income (range) | $21,857 ($1,440, $64,000) |
|
| |
| Mean number of children in household (range) | 2.3 (1, 13) |
|
| |
| Mean number of adults in household (range) | 2.1 (1, 6) |
Child is multiracial, and parent identifies child as Latino or African-American.
Approximately 40% of children are not in excellent or very good health (Table 3). About half of the children’s caregivers were not aware that their uninsured child is eligible for Medicaid or CHIP, and 95% of these uninsured children had been insured before. Among children who previously had been insured, Medicaid comprised about three-quarters of the coverage, followed by CHIP (14%) and private insurance (13%). The mean number of months that the child had been uninsured was 14, ranging from 1–144, and the median was six months. About two-thirds of caregivers report that their health is not excellent or very good. Only about one-quarter of the caregivers have health insurance, with over half having public insurance, and almost half covered by private insurance, of which 69% was employer-sponsored. Detailed baseline findings on health, special healthcare needs, parental reasons for the child being uninsured, access to healthcare, unmet needs, financial burden, the quality of care, satisfaction with care, and quality of life will be reported in a separate manuscript.
Table 3.
Selected characteristics of the health status and insurance coverage of uninsured minority children and their caregivers (N = 267) in the Kids’ HELP trial.
| Characteristic | Mean or % |
|---|---|
|
| |
| Child’s health statusa | |
| Excellent | 31.6% |
| Very Good | 29.3% |
| Good | 29.0% |
| Fair | 8.7% |
| Poor | 1.5% |
|
| |
| Primary caregiver aware that child is eligible for Medicaid or CHIP | 49% |
|
| |
| Child ever had health insurance before | 95% |
|
| |
| Insurance that uninsured child had in past | |
| Medicaid | 72% |
| CHIP | 14% |
| Privateb | 13% |
| Instituto Mexicano del Seguro Socialc | 1% |
|
| |
| Mean months without insurance (range) | 14.2 (1–144) |
|
| |
| Median months without insurance (inner 95th percentile range) | 6 (1, 84) |
|
| |
| Primary caregiver’s health statusd | |
| Excellent | 14.9% |
| Very Good | 23.1% |
| Good | 39.3% |
| Fair | 18.8% |
| Poor | 3.9% |
|
| |
| Primary caregiver has health insurance | 26% |
|
| |
| Type of insurance coverage for insured caregiver | |
| Public | 52% |
| Privatee | 45% |
| Other | 3% |
By parental report.
Of which 27% was through the caregiver’s employer-sponsored insurance.
Public health insurance in Mexico.
By self-report.
Of which 69% was employer-sponsored insurance.
Fifteen PMs completed the two-day training session. All PMs are female and non-white, 60% are unemployed, and the mean annual combined family income is $20,913. Post-training, overall test scores (on a 0–100 scale, with 100 equal to a perfect score) significantly increased, from a mean score = 62 (range: 39–82) to 88 (67–100) (P<.01), and the number of wrong answers decreased (mean reduction = 8; P<.01). Significant improvements occurred in six of nine topics, and 100% of PMs reported being very satisfied (86%) or satisfied (14%) with the training. PMs had an average caseload of three to eight participants and their families, with a maximum of 18 at any one point in time. Full details on the PM training sessions and the evaluations results are available elsewhere [48].
4. Discussion
The Kids’ HELP trial is the first RCT comparing the effectiveness of PMs to traditional Medicaid/CHIP outreach and enrollment in insuring eligible, uninsured Latino and African-American children. Our team conducted the only published RCT of an insurance intervention to date [17], but this community case-manager intervention differed from the proposed RCT in that it 1) did not evaluate parent mentors; 2) was limited solely to Latino children, 3) did not examine costs or health outcomes; and 4) was conducted in a state where undocumented immigrant children are eligible for limited insurance coverage. A few other published studies have examined interventions for insuring uninsured children, but none was an RCT, nor did any examine health outcomes [49,50,51,52]. Three were prospective observational studies conducted in EDs which examined the efficacy of a hospital case worker or handing out CHIP applications to uninsured patients’ families [49–51]. The fourth was a quasi-experimental, nonequivalent control group study (of an intervention consisting of information sheets, automated phone messages, presentations, and a personal phone call) conducted in three elementary schools and targeting uninsured Korean children [52].
The Kids’ HELP trial results to date document that the study design and methods have been successful in reaching the target population, meeting participant enrollment goals, and recruiting and training PMs. The substantial number (N=97) and variety of community recruitment sites proved crucial in being able to screen over 49,000 candidate participants and families, and ultimately, to enroll and randomize more than the target sample size of 300 participants. Selecting the five Dallas communities with the highest proportions of minority and low-income families permitted efficient screening and enrollment processes, the rapid formation of community partnerships, and effective community engagement with families, businesses, and community-based organizations. Recruiting PM candidates from a hospital-based outpatient clinic serving predominantly Medicaid- and CHIP-covered minority children and using a careful screening process resulted in dedicated PMs who significantly improved their knowledge and skills after training, and with high PM satisfaction with the training.
In February 2009, President Obama signed into law (Public Law 111-3) the Children’s Health Insurance Program Reauthorization Act of 2009, or CHIPRA [53]. The national allotment for CHIPRA was $68.9 million. Two of the most important CHIPRA objectives [54] were to 1) increase outreach and enrollment to more eligible uninsured children, and 2) insure at least four million more uninsured children eligible for Medicaid and CHIP. But rigorous evidence is severely lacking on effective outreach and enrollment mechanisms for insuring uninsured children, given that there has been only one published RCT [17] evaluating insurance interventions for children. For CHIPRA to meet these objectives of reaching and enrolling millions of eligible uninsured children, there is an urgent need for efficacious, innovative, cost-effective insurance interventions that have been rigorously evaluated. A particularly high priority is effective insurance interventions for minority children that eliminate racial/ethnic disparities, given that 56% of all uninsured children in America are Latino or African-American.
Certain study limitations should be noted. Approximately 65% of the target population (32,076 of 49,032 screened potential study candidates) was already enrolled in Medicaid/CHIP when approached for participation in the study. Although this is consistent with approximately 32% of Latino and African-American children in Dallas County being uninsured (the mean of the combined uninsurance rates of 45.1% for Latino and 19.5% for African-American children [19]), it is likely that enrollment of children in Medicaid/CHIP among the target population was actually lower than 65%, as our team has noted in the ongoing RCT that a number of parents believe that their children have obtained Medicaid/CHIP, but their children are actually uninsured, based on verification of uninsurance status by Texas HHSC. After eliminating potential subjects who did not meet inclusion criteria or already had Medicaid/CHIP coverage for their children, there were 8,574 subjects who chose not to participate in the study. The vast majority (7,403 = 85%), however, simply stated that they were not interested, and it is unclear what proportion of this group would have met inclusion criteria and actually had uninsured, Medicaid/CHIP-eligible children, as these individuals declined to provide additional information on their characteristics. Analogous data from other studies are not available. One possibility for the seemingly large refusal rate may be the well-documented distrust of medical research and hesitancy to enroll in studies among minority communities [55].
Achievement of the aims of the proposed study has the potential to be a significant contribution to reducing racial/ethnic disparities, empowering minority communities, providing economic revitalization through employment of minority parents, and advancing knowledge, practice, and child health policy. If, as anticipated, the proposed PM intervention is more efficacious and cost-effective than traditional Medicaid/CHIP outreach and enrollment, this intervention could serve as a national model for insuring uninsured children and reducing racial/ethnic disparities in childhood insurance coverage.
Acknowledgments
Supported in part by Award Number R01HD066219 (Principal Investigator: Flores) from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The content is solely the responsibility of the authors, and does not necessarily represent the official views of NICHD or the National Institutes of Health (NIH). Neither NICHD nor NIH had any role in the study design; collection, analysis, or interpretation of data; writing of the report; or the decision to submit the article for publication We are very grateful to all of the Kids’ HELP children, parents, Parent Mentors, and collaborating community partners, for their enthusiasm, commitment, and dedication to improving the health and healthcare of uninsured children.
Footnotes
Clinical Trials.gov NCT01264718
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lesley B. [Access verified 19 August 2014];Protecting child health by embracing its success. Available from: http://www.huffingtonpost.com/bruce-lesley/protecting-child-health-b_b_2902841.html.
- 2.Smith JC, Medalia C US Census Bureau. Health Insurance Coverage in the United States: 2013. Washington, DC: U.S. Government Printing Office; 2014. [Access verified 19 September 2014]. (Current Population Reports, P60-250). Available from: http://www.census.gov/content/dam/Census/library/publications/2014/demo/p60-250.pdf. [Google Scholar]
- 3.Hudson JL, Selden TM. Children’s eligibility and coverage: recent trends and a look ahead. Health Aff (Millwood) 2007;26:w618–29. doi: 10.1377/hlthaff.26.5.w618. [DOI] [PubMed] [Google Scholar]; American Academy of Pediatrics. Fact Sheet. Children’s Health Insurance; [Access verified 20 August 2014]. Available at: http://www.aap.org/research/factsheet.pdf. [Google Scholar]
- 4.Horner D, Guyer J, Mann C, Alker J. The Children’s Health Insurance Program Reauthorization Act of 2009. Washington, DC: Center for Children and Families, Georgetown University Health Policy Institute; 2009. [Google Scholar]
- 5.American Academy of Pediatrics. Fact Sheet. [Access verified 20 August 2014];Children’s Health Insurance. Available from: http://www.aap.org/research/factsheet.pdf.
- 6.Kenney GM, Lynch V, Haley JM, Huntress M, Resnick D, Coyer C. Gains for children: Increased participation in Medicaid and CHIP in 2009. Washington, DC: Urban Institute; 2011. [Access verified 20 August 2014]. Available from: http://www.urban.org/UploadedPDF/412379-Gains-for-Children.pdf. [Google Scholar]
- 7.Holahan J, Dubay L, Kenney GM. Which children are still uninsured and why. Future Child. 2003;13:55–79. [PubMed] [Google Scholar]
- 8.Flores G, Abreu M, Brown V, Tomany-Korman SC. How Medicaid and the State Children’s Health Insurance Program can do a better job of insuring uninsured children: The perspectives of parents of uninsured Latino children. Ambul Pediatr. 2005;5:332–340. doi: 10.1367/A04-067R2.1. [DOI] [PubMed] [Google Scholar]
- 9.The Kaiser Commission on Medicaid and the Uninsured. Medicaid and Children. Overcoming Barriers to Enrollment. Findings from a National Survey. Washington, DC: The Henry J. Kaiser Family Foundation; 2000. [Google Scholar]
- 10.Kempe A, Renfrew BL, Barrow J, Cherry D, Jones JS, Steiner JF. Barriers to enrollment in a state child health insurance program. Ambul Pediatr. 2001;1:169–177. doi: 10.1367/1539-4409(2001)001<0169:bteias>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 11.Salsberry PJ. Why are some children still uninsured? J Pediatr Health Care. 2003;17:32–38. doi: 10.1067/mph.2003.23. [DOI] [PubMed] [Google Scholar]
- 12.Haley J, Kenney G. Low-income uninsured children with special health care needs: why aren’t they enrolled in public health insurance programs? Pediatrics. 2007;119:60–68. doi: 10.1542/peds.2006-1726. [DOI] [PubMed] [Google Scholar]
- 13.Perry M, Paradise J The Kaiser Commission on Medicaid and the Uninsured. Enrolling Children in Medicaid and SCHIP: Insights from Focus Groups with Low-Income Parents. Washington, DC: The Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- 14.Manos MM, Leyden WA, Resendez CI, Klein EG, Wilson TL, Bauer HM. A community-based collaboration to assess and improve medical insurance status and access to health care of Latino children. Public Health Rep. 2001;116:575–584. doi: 10.1093/phr/116.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau. Current Population Survey. Table HI08. [Access verified August 28, 2014];Health insurance coverage status and type of coverage by selected characteristics for children under 18. 2012 Available at: https://www.census.gov/hhes/www/cpstables/032013/health/toc.htm.
- 16.U.S. Census Bureau. Current Population Survey. Table HI03. [Access verified August 28, 2014];Health insurance coverage status and type of coverage by selected characteristics for poor people in the poverty universe: 2012 (income-to-poverty ratio is below 100 percent) Available at: https://www.census.gov/hhes/www/cpstables/032013/health/toc.htm.
- 17.Flores G, Abreu M, Chaisson CE, Meyers A, Sachdeva RC, Fernandez H, et al. A randomized trial of the effectiveness of community-based case management in insuring uninsured Latino children. Pediatrics. 2005;116:1433–1441. doi: 10.1542/peds.2005-0786. [DOI] [PubMed] [Google Scholar]
- 18.Flores G, Snowden-Bridon C, Torres S, Perez R, Walter T, Brotanek J, et al. Improving asthma outcomes in minority children: A randomized, controlled trial of parent mentors. Pediatrics. 2009;124:1522–1532. doi: 10.1542/peds.2009-0230. [DOI] [PubMed] [Google Scholar]
- 19.Texas State Data Center and Office of the State Demographer. [Access verified September 3, 2014];Estimates of the Number and Percent Uninsured by Age and Race/Ethnicity for Texas Health Regions. 2005 Available at: http://txsdc.utsa.edu/reports/2006/CountyEstimatesUninsured/uninsured_estimates_all_2005.pdf.
- 20.The J. McDonald Williams Institute Research Arm of the Foundation for Community Empowerment. The Cost of Not Addressing Concentrated Poverty: How Much Can Dallas Afford to Pay? Dallas, TX: Foundation for Community Empowerment; Jul, 2006. [Google Scholar]
- 21.Olson LM, Tang SF, Newacheck PW. Children in the United States with discontinuous health insurance coverage. N Engl J Med. 2005;353:382–391. doi: 10.1056/NEJMsa043878. [DOI] [PubMed] [Google Scholar]
- 22.Baker DW, Cameron KA, Feinglass J, Thompson JA, Georgas P, Foster S, et al. A system for rapidly and accurately collecting patients’ race and ethnicity. Am J Public Health. 2006;96:532–537. doi: 10.2105/AJPH.2005.062620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Texas Health and Human Services Commission. CHIP/Children’s Medicaid. [Access verified September 3, 2014];Can I Get It? Available at: http://chipmedicaid.org/en/Can-I-Get-It.
- 24.The Henry J. Kaiser Family Foundation State Health Facts. [Access verified September 3, 2014];Income Eligibility Limits for Children’s Regular Medicaid and Children’s CHIP-funded Medicaid Expansions as a Percent of Federal Poverty Level (FPL) 2013 Jan; Available at: http://kff.org/medicaid/state-indicator/income-eligibility-fpl-medicaid/
- 25.Ross DC, Marks C Kaiser Commission on Medicaid and the Uninsured. Challenges of Providing Health Coverage for Children and Parents in a Recession: A 50 State Update on Eligibility Rules, Enrollment and Renewal Procedures, and Cost-Sharing Practices in Medicaid and SCHIP in 2009. Washington, DC: The Henry J. Kaiser Family Foundation; 2009. [Access verified September 3, 2014]. Available at: http://www.kff.org/medicaid/upload/7855.pdf. [Google Scholar]
- 26.Texas Health and Human Services Commission. CHIP/Children’s Medicaid. [Access verified September 3, 2014];How to Renew. Available at: http://chipmedicaid.org/CommunityOutreach/How-to-Renew.
- 27.Flores G. Devising, implementing, and evaluating successful interventions to eliminate racial/ethnic disparities in children’s health and healthcare: tips, pitfalls, and a research agenda. Pediatrics. 2009;124:S214–S223. doi: 10.1542/peds.2009-1100J. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feinstein AR. The Architecture of Clinical Research. Philadelphia, PA: W.B. Saunders Co; 1985. Clinical Epidemiology. [Google Scholar]
- 29.Flores G, Walker C, Lin H, Lee M, Fierro M, Henry M, et al. A successful program for training parent mentors to provide assistance with obtaining health insurance for uninsured children. Academic Pediatr. 2015 doi: 10.1016/j.acap.2014.09.011. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Texas Health and Human Services Commission. Children’s health insurance outreach and education campaign. Austin, TX: Texas Health and Human Services Commission; Apr 11, 2006. news release. [Google Scholar]
- 31.State Health Access Data Assistance Center. A State-by-State Analysis. Princeton, NJ: Robert Wood Johnson Foundation; 2014. [Access verified September 5, 2014]. For Kids’ Sake: State-Level Trends in Children’s Health Insurance. Available at: http://www.rwjf.org/content/dam/farm/reports/reports/2014/rwjf412274. [Google Scholar]
- 32.U.S. Census Bureau. Table HIB-5. [Access verified September 5, 2014];Health Insurance Coverage Status and Type of Coverage by State--Children Under 18: 1999 to 2012. Available at: https://www.census.gov/hhes/www/cpstables/032013/health/toc.htm.
- 33.Gold M. Panel on cost-effectiveness in health and medicine. Med Care. 1996;34(12 Suppl):DS197–199. [PubMed] [Google Scholar]
- 34.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 35.Health Resources and Services Administration, Maternal and Child Health Bureau, Centers for Disease Control and Prevention, National Center for Health Statistics, State and Local Area Integrated Telephone Survey. Interview Sections 1–11. Atlanta, GA: Centers for Disease Control and Prevention; 2003. [Access verified September 5, 2014]. National Survey of Children’s Health. Available at: http://www.cdc.gov/nchs/data/slaits/NSCH_Questionnaire.pdf. [Google Scholar]
- 36.Magee JC, Ritterband LM, Thorndike FP, Cox DJ, Borowitz SM. Exploring the relationship between parental worry about their children’s health and usage of an internet intervention for pediatric encopresis. J Pediatr Psychol. 2009;34:530–8. doi: 10.1093/jpepsy/jsn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4. 0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Szilagyi PG, Zwanziger J, Rodewald LE, Holl JL, Mukamel DB, Trafton S, et al. Evaluation of a state health insurance program for low-income children: implications for state child health insurance programs. Pediatrics. 2000;105:363–371. doi: 10.1542/peds.105.2.363. [DOI] [PubMed] [Google Scholar]
- 39.Moreno L, Hoag SD. Covering the uninsured through TennCare: does it make a difference? Health Aff (Millwood) 2001;20:231–239. doi: 10.1377/hlthaff.20.1.231. [DOI] [PubMed] [Google Scholar]
- 40.Szilagyi PG, Dick AW, Klein JD, Shone LP, Zwanziger J, McInerny T. Improved access and quality of care after enrollment in the New York State Children’s Health Insurance Program (SCHIP) Pediatrics. 2004;113:e395–404. doi: 10.1542/peds.113.5.e395. [DOI] [PubMed] [Google Scholar]
- 41.Kempe A, Beaty BL, Crane LA, Stokstad J, Barrow J, Belman S, et al. Changes in access, utilization, and quality of care after enrollment into a state child health insurance plan. Pediatrics. 2005;115:364–371. doi: 10.1542/peds.2004-0475. [DOI] [PubMed] [Google Scholar]
- 42.Centers for Disease Control and Prevention. SLAITS National Survey of Children with Special Health Care Needs. Atlanta, GA: Centers for Disease Control and Prevention; [Access verified September 5, 2014]. Available at: http://www.cdc.gov/nchs/data/slaits/NS-CSHCN%20Questionnaire%20(website)1.pdf. [Google Scholar]
- 43.Holl JL, Szilagyi PG, Rodewald LE, Shone LP, Zwanziger J, Mukamel DB, et al. Evaluation of New York State’s Child Health Plus: access, utilization, quality of health care, and health status. Pediatrics. 2000;105(3 Suppl E):711–718. [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. National Survey of Early Childhood Health. Appendix III. Atlanta, GA: Centers for Disease Control and Prevention; [Access verified September 5, 2014]. SLAITS: The State and Local Area Integrated Telephone Survey. Available at: http://www.cdc.gov/nchs/data/slaits/survey_sech00.pdf. [Google Scholar]
- 45.Agency for Healthcare Research and Quality. CAHPS Health Plan Survey 4.0. Version: Child Medicaid Questionnaire. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 46.Lave JR, Keane CR, Lin CJ, Ricci EM, Amersbach G, LaVallee CP. Impact of a children’s health insurance program on newly enrolled children. JAMA. 1998;279:1820–1825. doi: 10.1001/jama.279.22.1820. [DOI] [PubMed] [Google Scholar]
- 47.Centers for Disease Control and Prevention. Draft 2009 NHIS Questionnaire - Sample Child. Atlanta, GA: Centers for Disease Control and Prevention; 2009. [Access verified September 5, 2014]. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2009/english/qchild.pdf. [Google Scholar]
- 48.Flores G, Walker C, Lin H, Lee M, Fierro M, Henry M, et al. A successful program for training parent mentors to provide assistance with obtaining health insurance for uninsured children. Academic Pediatrics. 2015 doi: 10.1016/j.acap.2014.09.011. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gordon JA, Dupuie TA. Child health insurance outreach through the emergency department: a pilot study. Acad Emerg Med. 2001;8:1088–1090. doi: 10.1111/j.1553-2712.2001.tb01120.x. [DOI] [PubMed] [Google Scholar]
- 50.Gordon JA, Emond JA, Camargo CA., Jr The State Children’s Health Insurance Program: a multicenter trial of outreach through the emergency department. Am J Public Health. 2005;95:250–253. doi: 10.2105/AJPH.2003.037242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mahajan P, Stanley R, Ross KW, Clark L, Sandberg K, Lichtenstein R. Evaluation of an emergency department-based enrollment program for uninsured children. Ann Emerg Med. 2005;45:245–250. doi: 10.1016/j.annemergmed.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 52.Chen JY, Swonger S, Kominski G, Liu H, Lee JE, Diamant A. Cost-effectiveness of insuring the uninsured: the case of Korean American children. Med Decis Making. 2009;29:51–60. doi: 10.1177/0272989X08322011. [DOI] [PubMed] [Google Scholar]
- 53. [Access verified September 19, 2014];Public Law 111–3—Feb. 4, 2009. Available at: http://frwebgate.access.gpo.gov/cgi-bin/getdoc.cgi?dbname=111_cong_public_laws&docid=f:publ003.111.pdf.
- 54.Horner D, Guyer J, Mann C, Alker J. The Children’s Health Insurance Program Reauthorization Act of 2009. Washington, DC: Center for Children and Families, Georgetown University Health Policy Institute; 2009. [Google Scholar]
- 55.Heller C, Balls-Berry JE, Nery JD, Erwin PJ, Littleton D, Kim M, Kuo WP. Strategies addressing barriers to clinical trial enrollment of underrepresented populations: A systematic review. Contemp Clin Trials. 2014;39(2):169–182. doi: 10.1016/j.cct.2014.08.004. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]