Abstract
Objective
To develop and test latent variables of the social determinants of health that influence diabetes self-care.
Methods
615 adults with type 2 diabetes were recruited from two adult primary care clinics in the southeastern United States. Confirmatory factor analyses (CFA) identified the latent factors underlying socioeconomic determinants, psychosocial determinants, and self-care (diet, exercise, foot care, glucose testing, and medication adherence). Structured equation modeling (SEM) investigated the relationship between determinants and self-care.
Results
Latent variables were created for diabetes self-care, psychological distress, self-efficacy, social support and social status. The initial model (chi2(254)=388.04, p<0.001, RMSEA=0.03, CFI=0.98) showed that lower psychological distress (r=-0.13, p=0.019), higher social support (r=0.15, p=0.008), and higher self-efficacy (r=0.47, p<0.001) were significantly related to diabetes self-care. Social status was not significantly related to self-care (r=0.003, p=0.952). In the trimmed model (chi2(189)=211.40, p=0.126, RMSEA=0.01, CFI=0.99) lower psychological distress (r=-0.13, p=0.016), higher social support (r=0.15, p=0.007), and higher self-efficacy (r=0.47, p<0.001) remained significantly related to diabetes self-care.
Conclusion
Based on theoretical relationships, three latent factors that measure social determinants of health (psychological distress, social support and self-efficacy) are strongly associated with diabetes self-care.
Practice Implications
This suggests that social determinants should be taken into account when developing patient self-care goals.
1. INTRODUCTION
Diabetes affects 382 million people worldwide, and is associated with long-term complications and decreased quality of life. [1] Self-care behaviors are an integral aspect of comprehensive care for patients with type 2 diabetes, including exercise, diet, blood sugar testing, foot care, and adherence to oral medications [2,3]. As diabetes self-management education (DSME) is a critical element for improving self-care, clinicians and researchers continue to investigate how to enhance current efforts. [2,4,5] Current standards note that there is no one ‘best’ approach, and recommend consideration of behavioral and psychosocial strategies and development of personal strategies. [4,6,7] One overarching framework to use in considering how to develop individualized strategies is consideration of how social determinants of health may influence whether patients engage in self-care behaviors. Social determinants of health are the circumstances in which people are born, live, work, and age. [8] This includes socioeconomic circumstances, neighborhood environments, psychosocial factors, and upstream political, economic and sociocultural drivers. [9] Current evidence suggests that social determinants of health influence diabetes prevalence and outcomes. [10-11] Consideration of social determinants known to influence DSME may assist in understanding how to personalize DSME efforts and improve self-care.
Structured equation modeling (SEM) is a set of strategies, combining regression, path analysis, and factor analysis, which allows complex modeling of closely related predictors. [12] Through the use of latent variables, or hypothetical constructs that reflect a concept not directly observable, SEM also incorporates measurement error into models. [12-14] As a result of the ability to explicitly take measurement error into account and determine the extent to which a theoretical model is supported by sample data, SEM can advance understanding of complex relationships and model multiple outcomes simultaneously. [12,14] Latent variables are appropriate for investigating the relationship between social determinants of health and diabetes self-care because of the number of underlying and unobserved variables involved. [15] For example, social determinants of health research shows the importance of education, income, and employment, all causal indicators of a larger social status latent variable. [16,17] Similarly, while extensive work has been done on depression, diabetes distress and serious psychological distress [18,19,20], an underlying construct of emotional distress has been suggested to explain the influence previously measured by individual factors. [21]
A conceptual framework developed by the World Health Organization (WHO) for investigation of social determinants of health found that material circumstances, behaviors, and psychosocial factors influence health status and well-being. [22] Since SEM provides a way to determine whether certain factors are more strongly related to overarching constructs, this study was designed to determine which social determinants most strongly influence diabetes self-care. A search of the literature showed that constructs hypothesized to influence diabetes self-care fit into WHO’s categories of material circumstances and psychosocial factors. Based on a literature review in 2005, more self-efficacy and less distress may be most important in influencing self-care in diabetes. [23] A systematic review of the barriers to self-management conducted in 2011 found more financial resources, less co-morbidities and more social support to be influential. [24] While individual studies have looked at the impact of these factors as observed variables on self-care [25,26-28], few studies have incorporated latent variables for various socioeconomic and psychosocial factors in order to address measurement error inherent in these concepts.
The aim of this study was to develop and test latent variables using SEM to provide a better understanding of the social determinants of health that influence diabetes self-care. Based on a review of the literature for constructs that are regularly shown to influence self-care, latent variables were hypothesized for social status and the psychological factors of self-efficacy, social support and psychological distress. Structured equation modeling was then used to test the associations between these social determinants of health and a latent variable for diabetes self-care. Our hypothesis was that low social status and psychological distress will be associated with poor self-care, while higher self-efficacy and social support will be associated with good self-care behaviors.
2. METHODS
2.1 Sample
615 patients were recruited from two adult primary care clinics in the southeastern United States, after institutional review board approval. Eligibility included ages 18 years or older, diagnosis of type 2 diabetes in their medical record, and ability to communicate in English. Patients were ineligible if through interaction or chart documentation patients were determined to be cognitively impaired as a result of significant dementia or active psychosis. Patients showing interest after receiving letters of invitation or being approached in the clinic waiting room were provided a detailed explanation of the study and consented. Participants completed validated questionnaires that captured social determinants of health factors along with demographic and self-care information. Validated questionnaires were included based on a modified version of the conceptual framework by Brown et al. relating socioeconomic factors to diabetes processes and outcomes [29].
2.2 Social Determinants of Health Variables
Socioeconomic Status
Previously validated items from the 2002 National Health
Interview Survey [30] were used to capture household income, years of education and employment status. Household income was categorized into 4 income units: <$20,000, $20,000-$49,999, $50,000-$74,999, ≥ $75,000. Years of education were categorized into 4 units: less than high school, high school graduate, college education, and more than college education. Employment was dichotomized as not employed and employed.
Subjective Social Status
Subjective Social Status (SSS) is a perceived measure of social status where respondents mark on a ladder with 10 rungs where they would place themselves where 10 are people with the most money, education and well respected jobs, and 1 are people with the least money, education and well respected jobs. [31] Responses were categorized based on quartiles into a 4 category categorical variable.
Fatalism
Fatalism is a psychological state characterized by perceptions of despair, hopelessness, and powerlessness. [32] It was assessed with the Diabetes Fatalism Scales (DFS); a 12-item scale where higher scores represent greater diabetes fatalism. [32] The DFS has a Cronbach’s alpha of 0.80. [32]
Self-Efficacy
Self-efficacy was assessed with the Perceived Diabetes Self-Management Scale (PDSMS); an 8-item measure where higher scores indicate higher self-efficacy. [33] This is a valid and reliable measure of diabetes self efficacy (Cronbach alpha = 0.83). [33]
Depression
Depression was assessed with the Patient Health Questionnaire (PHQ-9); a 9 item scale based on DSM-IV criteria for depression with sensitivity of 88% and a specificity of 88% for major depression. [34,35]
Diabetes Distress
Distress was assessed with the Diabetes Distress Scale (DDS); a 17-item measure with questions about disease management, support, emotional burden and access to care. [36] The sensitivity and specificity ranged from 0.85 to 0.97. [36]
Serious Psychological Distress
Serious Psychological Distress (SPD) was assessed with the Kessler-6 (K6); a 6-item scale with higher scores representing higher probability of severe mental illness. The scale has good precision and consistent psychometric properties across major sociodemographic samples. [37]
Social Support
Social Support was assessed with the Medical Outcomes Study (MOS) Social Support Survey; a 19-item scale measuring tangible support, affection, positive social interaction, and emotional or informational support. The total scale (α=0.97) has high internal consistency, good criterion and discriminant validity, and one-year test-retest reliability (0.72 to 0.76). [38]
Perceived Stress
Stress was assessed with the Perceived Stress Scale (PSS); a 4-item scale assessing the frequency over the previous month with which the respondent finds situations stressful. [39] The Cronbach alpha value is 0.69 and scores are highly correlated with stress, depression and anxiety. [40]
2.3 Diabetes Self-care
Self-Reported Medication Adherence
Medication Adherence was assessed with the Morisky Medication Adherence Scale (MMAS); an 8-item scale with higher values indicating higher adherence. [41]
Behavioral Skills
Diabetes behavior was assessed with the Summary of Diabetes Self-Care Activities (SDSCA) scale; an 11-item scale measuring frequency of self-care activity in the last 7 days for general diet (follow healthy diet), specific diet (ate fruits/two fat diet), exercise, blood glucose testing, and foot care [42].
2.4 Sample Size
The target sample size for this study was 600 adults to provide the recommended 20:1 ratio (subjects to variables) necessary given the large number of social determinants of health variables. [14,43] Sample size influences the calculation of minimum fit function and smaller sample sizes do not give enough information without saturating the model with variables. [14] Given the 18 factors each with numerous observed variables, this sample size leads to more precise estimates while minimizing the possibility of over-saturating the model.
2.5 Statistical Analysis
We used SEM, which combines a measurement model with a structural model. [14] It is important to note, however, that SEM does not provide evidence of causation. [13] Non-experimental designs can be analyzed using SEM, but interpretation of results should be realistic and within the confines of the data. [13] A priori specifications were designed based on the WHO model of social determinants of health and a literature search for important socioeconomic and psychosocial factors that influence diabetes self-care. SEM determines if the pre-specified model is supported by the data, and alternative models can exist. [13] Thus, we used SEM is to create a model that is theoretically sound, reasonably parsimonious and supported by the data. [13]
First, descriptive statistics were used to describe the data and check for normality. Second, a series of confirmatory factor analyses (CFA) were used to identify the latent factors underlying socioeconomic determinants (social status), psychosocial determinants (psychological distress, self-efficacy, social support), and self-care (diet, exercise, foot care, glucose testing, and medication adherence). Alpha statistics and factor analysis were used to examine the loading of each hypothesized factor. Variables with low loading (<0.32) or non-significant loading were removed from the latent variable, unless it was determined that theoretically the factor should not be removed. [43] CFA was used to test goodness of fit of hypothesized latent variables and factors. Diet, exercise, foot care, glucose testing, and medication adherence were hypothesized to load on a single self-care latent variable. Income, education, employment and subjective social status were hypothesized to load on a single social status latent variable. Psychosocial factors were hypothesized to load on three latent variables: psychological distress, self-efficacy and social support. The different psychosocial factors were analyzed to find which loaded the highest and was the most parsimonious for use in the final model. Factors were analyzed using principle component factor analysis. Parameters were estimated using maximum likelihood.
Third, SEM was used to investigate the relationship between determinants and self-care. SEM analysis followed the five step process recommended by Schumacker & Lomax [14]: model specification, model identification, model estimation, model testing, and model modification. Given the large sample size in this study, there were a sufficient number of measurements to estimate the covariance matrix and provide stability of parameter estimates with an acceptable ratio of 10-20 participants per parameter estimated. [44] After ensuring data were multivariate normal, linearly related and at least interval scale to meet assumptions [45], analyses were performed using the robust maximum likelihood estimation procedure. As CFA is particularly sensitive to missing data [44,45], the ‘mlmv option’ in STATA version13 was used which retains variables rather than using listwise deletion. As a result, all parameters were estimated directly, rather than imputing data. All analyses were completed using STATA Version13 using standardized estimates. Standardized estimates are interpreted as the change in standard deviation of the outcome due to one standard deviation increase in the predictor, and are useful when variable scales are incongruent as is the case in this study. [12] Model testing involved numerous fit statistics to determine how well the data fit the model and to what extent the theoretical model was supported by the obtained sample data. Global fit statistics included chi-square goodness of fit, RMSEA, and CFI. The model was considered a good fit with a chi-square that was not significant, RMSEA<0.08 and CFI>0.9. The model was also evaluated by inspecting the direction and magnitude of individual parameters and path coefficients. If model fit was not ideal, modification followed by examining both statistical and practical significance of parameters until the best fitting and most parsimonious model was finalized. The final model estimated parameters for a trimmed version incorporating modification indices.
3. RESULTS
3.1 Sample Demographics
Demographic characteristics for this sample of 615 adults with type 2 diabetes are shown in Table 1. The mean age was 61 years, with the majority being men (61.6%), non-Hispanic black (64.9%), and employed (65.3%). 13% had less than a high school diploma, and 41.6% earned less than $20,000 annually. Descriptive information on measures included in latent variables are presented in Table 2.
Table 1.
Sample demographic characteristics (n=615)
| % or Mean ± standard deviation | |
|---|---|
|
| |
| Age | 61.3 ± 10.9 |
| 18-34 years | 1.6 |
| 35-44 years | 5.2 |
| 45-64 years | 53.6 |
| 65+ years | 39.6 |
| Gender | |
| Women | 38.4 |
| Men | 61.6 |
| Race/Ethnicity | |
| Non-Hispanic Black | 64.9 |
| Non-Hispanic Whites | 33.0 |
| Hispanic/Other | 2.1 |
| Marital Status | |
| Married | 49.7 |
| Not Married | 50.3 |
| Educational level | |
| Less than high school graduate | 13.0 |
| High school graduate | 28.2 |
| College education | 47.1 |
| More than college | 11.7 |
| Employment status | |
| Employed | 34.7 |
| Not employed | 65.3 |
| Annual income level | |
| <$20,000 | 41.6 |
| $20,000-$49,000 | 38.9 |
| $50,000-$74,999 | 10.1 |
| $75,000+ | 9.4 |
| Subjective Social Status | |
| 1st quartile | 13.85 |
| 2nd quartile | 32.50 |
| 3rd quartile | 19.89 |
| 4th quartile | 33.75 |
| Systolic Blood Pressure | 129.7 ± 16.6 |
| Blood Pressure Control (<140/80) | |
| Controlled | 58.9 |
| Not Controlled | 41.1 |
| LDL | 96.9 ± 66.7 |
| Lipid Control (LDL<100) | |
| Controlled | 62.8 |
| Not Controlled | 37.2 |
| HbA1c % (mmol/mol) | 7.9 ± 1.8 (63 ± 19.7) |
| Glycemic Control (HbA1c<8% or 64 mmol/mol) | |
| Controlled | 57.9 |
| Not Controlled | 42.1 |
Table 2.
Self-Care and Psychological Factors
| Measures | Means ± standard deviation |
|---|---|
|
| |
| Self-Care | |
| General Diet | 4.7 ± 2.0 |
| Special Diet | 4.0 ± 1.5 |
| Exercise | 2.6 ± 2.2 |
| Blood Sugar Testing | 4.6 ± 2.5 |
| Foot Care | 4.3 ± 2.5 |
| Medication Adherence | 5.9 ± 2.0 |
| Serious Psychological Distress | |
| SPD-1 | 1.2 ± 1.2 |
| SPD-2 | 0.7 ± 1.2 |
| SPD-3 | 1.2 ± 1.3 |
| SPD-4 | 0.7 ± 1.2 |
| SPD-5 | 1.2 ± 1.3 |
| SPD-6 | 0.6 ± 1.1 |
| Self-Efficacy | |
| PDSMS-1 | 3.4 ± 1.1 |
| PDSMS-2 | 3.2 ± 1.1 |
| PDSMS-3 | 3.8 ± 0.9 |
| PDSMS-4 | 3.8 ± 0.9 |
| PDSMS-5 | 3.7 ± 0.9 |
| PDSMS-6 | 3.5 ± 1.1 |
| PDSMS-7 | 3.4 ± 1.1 |
| PDSMS-8 | 3.8 ± 0.9 |
| Social Support | |
| MOS-16 | 3.9 ± 1.2 |
| MOS-17 | 3.9 ± 1.3 |
| MOS-18 | 3.9 ± 1.3 |
3.2 Latent Variable for Diabetes Self Care
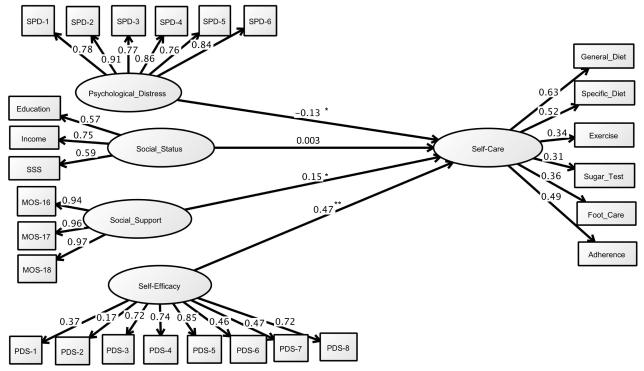
CFA was used to assess the measurement properties of a possible latent variable for diabetes self care using six variables (general diet, specific diet, exercise, blood sugar testing, foot care and medication adherence). The alpha statistic for the six items was 0.61. The variables loaded onto one factor explaining 35% of the variance with factor loadings ranging from 0.46 to 0.70. The fit of final model was satisfactory (chi2(8)=9.94, p=0.26; RMSEA=0.02 and CFI=0.99. The six measures of self-care have substantial loading that is significant at the p<0.001 level. The standardized loadings ranged from 0.33 to 0.65. The final self-care latent variable is shown in Figure 1.
Figure 1.
Confirmatory Factor Analysis of Diabetes Self Care Behaviors Measurement Model. Note: Overall model fit chi2(8, n=604)=9.94, p=0.2692, CFI=0.99, RMSEA=0.02 (90% CI:0.00, 0.05). All factor loadings significant at p<0.001.
3.3 Latent Variable for Social Status
CFA was used to assess the measurement properties of a latent variable for social status based on four initial variables (income, education, employment, and social subjective status). The alpha statistic was low and factor analysis showed low loading for employment, so it was removed, leaving high internal consistency (alpha=0.65). The remaining three variables loaded on one factor explaining 60% of the variance with factor loadings ranging from 0.74 to 0.82. The fit of the initial model was satisfactory so no further changes were made. Standardized loadings ranged from 0.55 to 0.77.
3.4 Latent Variable for Psychosocial Factors
Based on a review of the literature for the most important psychosocial factors influencing self-care, the CFA model hypothesized three factors: psychological distress, social support and self-efficacy. After examining the alpha and factor loading for each of the possible indicator scales it was determined that 1) SPD would be used for psychological distress since along with diabetes distress it had the highest alpha, but given the smaller number of items, SPD would be the most parsimonious and would provide a more general measure of distress; 2) self-efficacy would be used instead of fatalism for the self-efficacy factor, as similarly with fewer items it was more parsimonious and loaded higher, and 3) the positive social interaction portion of the social support scale would be used as a parsimonious summary of the MOS scale and would provide a more general measure of support. The alpha statistic for psychological distress was 0.92. The variables loaded onto one factor explaining 73% of the variance, with factor loadings ranging 0.79 to 0.89. The alpha statistic for self-efficacy was 0.83. The variables loaded onto one factor explaining 47% of the variance, with factor loadings ranging from 0.59 to 0.78. The alpha statistic for social support was 0.97. The variables loaded onto one factor explaining 94% of the variance with factor loadings ranging from 0.96 to 0.97.
The fit of the psychological distress model was satisfactory (chi2(6)=10.61, p=0.101, RMSEA=0.04 and CFI=0.99). The standardized loadings ranged from 0.74 to 0.89. The fit of the self-efficacy model was satisfactory (chi2(13)=18.33, p=0.145 RMSEA=0.26 and CFI=0.99). The standardized loadings ranged from 0.14 to 0.85. Using the positive social interaction portion of the MOS as a social support model resulted in excellent model fit statistics with no modifications needed. The standardized loadings ranged from 0.94 to 0.97.
3.5 Structural Model
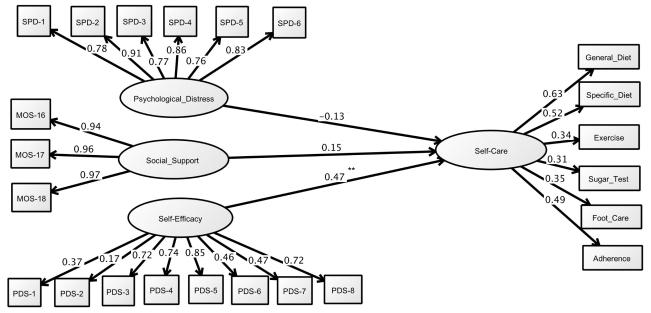
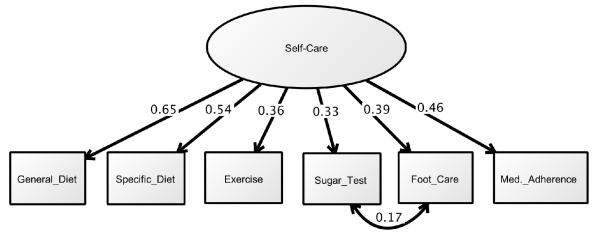
Figure 2 shows the theoretical relationships tested. This initial model (chi2(254)=388.04, p<0.001, RMSEA=0.03, CFI=0.98) showed that lower psychological distress (r=-0.13, p=0.019), higher social support (r=0.15, p=0.008), and higher self-efficacy (r=0.47, p<0.001) were significantly related to diabetes self-care. Social status was not significantly related to self-care (r=0.003, p=0.952). Since social status was not significant, it was removed for the final trimmed structural model. In the trimmed model (chi2(189)=211.40, p=0.126, RMSEA=0.01, CFI=0.99) lower psychological distress (r=-0.13, p=0.016), higher social support (r=0.15, p=0.007), and higher self-efficacy (r=0.47, p<0.001) remained significantly related to diabetes self-care. The trimmed model is shown in Figure 3.
Figure 2.
Initial Social Determinants of Self-Care model. Note: Coefficients are standardized path coefficients. Overall model fit chi2 (254, n=615)=388.04, p<0.001, RMSEA=0.03 (90% CI:0.02,0.04), CFI=0.98. All factor loadings significant at p<0.001. For paths *p<0.01, **p<0.001.
Figure 3.
Final Social Determinants of Self-Care model (Trimmed). Note: Coefficients are standardized path coefficients. Overall model fit chi2(189, n=615)=211.40, p=0.126, RMSEA=0.01 (90% CI:0.00,0.02), CFI=0.99. All factor loadings significant at p<0.001. For paths *p<0.01, **p<0.001.
4. DISCUSSION AND CONCLUSION
4.1 Discussion
Using structural relationships, we found that in a sample of adults with type 2 diabetes, social determinants are significantly associated with diabetes self-care. Consistent with our hypothesis, psychological distress was negatively associated with self-care, while self-efficacy and social support were positively associated with self-care behaviors. Contrary to our hypothesis, social status was not significantly related to diabetes self-care. In addition, we found that psychosocial factors can be conceptualized as three domains: psychological distress, social support and self-efficacy. This suggests that psychosocial factors should not be viewed as a single influence on patients with type 2 diabetes, but a set of positive and negative influences.
Though prior research has investigated social status and psychosocial factors individually, this is the first to our knowledge that accounts for measurement error in both self-care and social determinant of health factors by using latent variables and SEM. In addition to the use of SEM, this study is unique in the large sample size allowing comparison of two different models for psychosocial factors. The study was designed to maintain power while accounting for the numerous factors conceptually related to self-care based on theoretical models for diabetes self-management training and social determinants of health. Previous work did not use SEM to incorporate latent variables for psychological distress, self-efficacy, social support, and social status. The use of latent variables for these constructs, rather than measured variables in regression or path analysis, provides a way to take measurement error into account. Without adjustment for measurement error, biased parameter estimates can result and may have serious consequences in result interpretation. [14] Therefore, this study is unique in that it addresses possible bias in understanding the determinants of diabetes self-care. As self-care plays a central role in diabetes management and is a major focus of diabetes education, this work provides a better understanding of how to develop behavioral interventions to improve care. Additionally, as general measures of distress and social support were chosen to represent these factors, these results suggest these concepts are important to consider beyond only diabetes specific distress and diabetes specific support.
These results correspond to prior regression based analyses suggesting that better self-care is associated with lower psychological distress, higher social support and higher self-efficacy. [18-20,25] In addition, the results agree with previous studies using SEM and path analysis to investigate factors associated with the self-care latent construct. [26-28] Work by Egede and Osborn [27] using SEM found that less depressive symptoms, less fatalistic attitudes and more social support were independent, direct predictors of self-care behavior. A recent path analysis in patients with type 2 diabetes found that illness perception and provider-patient communication also show direct paths to improved self-care, supporting the importance of psychosocial factors. [28] This study builds on the literature by suggesting that all three constructs influence self-care separately while accounting for measurement error by using latent variables for all constructs investigated. Based on these results, the strongest determinant of self-care behavior is self-efficacy and psychosocial factors are more strongly associated with self-care than social status factors. Future work should further investigate these constructs and the direct and indirect influences they have on both self-care in patients with diabetes.
The strengths of this analysis include the use of latent variables to account for measurement error and hypothetical constructs that cannot be directly measured, and the large sample size allowing for SEM analysis. Some limitations exist, however, including the cross-sectional study design, which precludes conclusions regarding causality or direction of the associations observed. Secondly, the study was conducted in the southeast United States and may not be representative of other areas. The sample also had primary representation from individuals with lower income and may not be generalizable to populations with higher socioeconomic status. Finally, while only validated scales were used, the data in this analysis is self-report.
4.2 Conclusion
In conclusion, psychosocial factors are more strongly associated with self-care than social status factors. Psychosocial factors can be separated into three latent constructs: psychological distress, social support and self-efficacy. Better self-care is associated with lower psychological distress, higher social support, and higher self-efficacy. Given three separate psychosocial constructs influence self-care behavior, future interventions should incorporate strategies to address these factors.
4.3 Practice Implications
While self-efficacy was the strongest predictor of self-care, both psychological distress and social support also had an influence on behavior. A consensus report regarding empowering clinicians and patients to individualize treatment recommends consideration of family, social and community environment. [5] Results of this study suggest that psychosocial factors should be taken into account when developing patient self-care goals, and may be an additional area to highlight in recommendations to clinicians. Additionally, results of this study suggest these factors may need to be addressed separately rather than considering psychosocial influences as one group. A discussion of individualizing glycemic targets suggests consideration of a patient’s psychological, social, and economic conditions be considered as an influence on self-management targets. [7] However, only depression is noted when discussing psychological status and social support is framed only in relation to patient safety. This study suggests additional psychosocial factors should be taken into consideration when working with patients to develop self-management goals, including assessment of self-efficacy, a broader definition of social support, and consideration of psychological distress rather than depression alone.
Reviews of psychological interventions in patients with type 2 diabetes found effectiveness in improving both glycemic control and psychological distress. [6,46,47] Interventions included in the reviews incorporated a variety of therapies, the majority of which included cognitive behavioral therapy and associated strategies such as relaxation techniques, problem solving, and enlisting social support. [46,47] Additional therapies included counseling therapy and more intensive psychological therapies. [46,47] Alam et al. found that generalists are equally effective as psychological specialists at delivering psychological interventions [47], suggesting that additional training for clinicians could allow delivery of psychological therapies. Given the results of this study, and the literature supporting the importance of psychosocial factors in patients with type 2 diabetes, multi-component interventions incorporating both behavioral and psychological strategies are recommended to improve self-care.
Highlights.
Structured equation modeling evaluated role of social determinants on diabetes self-care (n=615)
Social determinants latent factors included distress, self-efficacy, and social support
Psychological distress, social support, and self-efficacy were significantly related to self-care
Study shows that social determinants of health are associated with diabetes self-care
Thus, social determinants should be taken into account when developing self-care intervention
Acknowledgments
Funding Source: This study was supported by Grant K24DK093699-01 from The National Institute of Diabetes and Digestive and Kidney Disease (PI: Leonard Egede).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors report no potential conflicts of interest relevant to this article.
Author Contributions: LEE obtained funding for the study. RJW and LEE designed the study, acquired, analyzed and interpreted the data. RJW, MG, BMH and LEE developed the analysis, contributed to interpretation and critically revised the manuscript for important intellectual content. All authors approved the final manuscript.
REFERENCES
- 1.International Diabetes Federation . IDF Diabetes Atlas. 6th edn International Diabetes Federation; Brussels, Belgium: 2013. [Google Scholar]
- 2.American Diabetes Association Standards of Medical Care in Diabetes – 2014. Diabetes Care. 2014;37(Supplement 1):S14–S80. doi: 10.2337/dc14-S014. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention . National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; Atlanta, GA: 2011. [Google Scholar]
- 4.Funnel MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Maryniuk M, Peyrot M, Piette JD, Reader D, Siminerio LM, Weigner K, Weiss MA. National standards for diabetes self-management education. Diabetes Care. 2012;35(Supplement 1):S101–S108. doi: 10.2337/dc12-s101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marrero DG, Ard J, Delamater AM, Peragallo-Dittko V, Mayer-Davis EJ, Nwankwo R, Fisher EB. Twenty-first century behavioral medicine: a context for empowering clinicians and patients with diabetes: a consensus report. Diabetes Care. 2013 Feb;36(2):463–470. doi: 10.2337/dc12-2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Delamater AM, Jacobson AM, Anderson B, Cox D, Fisher L, Lustman P, Rubin R, Wysocki T. Psychosocial therapies in diabetes: Report of the psychosocial therapies working group. Diabetes Care. 2001;24:1286–1292. doi: 10.2337/diacare.24.7.1286. [DOI] [PubMed] [Google Scholar]
- 7.Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011;154:554–559. doi: 10.7326/0003-4819-154-8-201104190-00007. [DOI] [PubMed] [Google Scholar]
- 8.Healthy People Secretary’s Advisory Committee on Health Promotion and Disease Prevention Objectives for 2020. Healthy People 2020: An Opportunity to Address the Societal Determinants of Health in the United States. 2010 Jul 26; Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39.
- 9.Marmot M. Fair society, healthy lives (the Marmot review) Department of Health; London: 2010. [Google Scholar]
- 10.Whiting D, Unwin V, Roglic G. Equity, social determinants and public health programs. World Health Organization; Geneva: 2010. Diabetes: equity and social determinants; pp. 77–94. [Google Scholar]
- 11.Walker RJ, Small BL, Campbell JA, Strom Williams JL, Egede LE. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine. 2014 Feb 15; doi: 10.1007/s12020-014-0195-0. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanchez BN, Budtz-Jorgensen E, Ryan LM, Hu H. Structural equation models: a review with applications to environmental epidemiology. J American Statistical Association. 2005;100:1443–1455. [Google Scholar]
- 13.Kline RB. Principles and Practice of Structural Equation Modeling. The Guilford Press; New York, NY: 2011. [Google Scholar]
- 14.Schumacker RE, Lomax Richard G. A Beginner’s Guide to Structural Equation Modeling. Third Edition Taylor and Francis Group; New York, NY: 2010. [Google Scholar]
- 15.Bollen KA. Latent variables in psychology and the social sciences. Annu Rev Psychol. 2002;53:605–634. doi: 10.1146/annurev.psych.53.100901.135239. [DOI] [PubMed] [Google Scholar]
- 16.Dray-Spira R, Gary-Webb TL, Brancati FL. Educational disparities in mortality among adults with diabetes in the US. Diabetes Care. 2010;33(6):1200–1205. doi: 10.2337/dc09-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804e18. doi: 10.1093/ije/dyr029. [DOI] [PubMed] [Google Scholar]
- 18.Egede LE, Dismuke CE. Serious psychological distress and diabetes: a review of the literature. Curr Psychiatry Rep. 2012;14(1):15–22. doi: 10.1007/s11920-011-0240-0. [DOI] [PubMed] [Google Scholar]
- 19.Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87(3):302–312. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 20.Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010;33(5):1034–1036. doi: 10.2337/dc09-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher L, Gonzalez JS, Polonsky WH. The confusing tale of depression and distress in patients with diabetes: a call for greater clarity and precision. Diabet Med. 2014;31:764–772. doi: 10.1111/dme.12428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- 23.Sigurdardottir AK. Self-care in diabetes: model of factors affecting self-care. Journal of Clinical Nursing. 2005;14:301–314. doi: 10.1111/j.1365-2702.2004.01043.x. [DOI] [PubMed] [Google Scholar]
- 24.Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res and Clin Prac. 2011;93:1–9. doi: 10.1016/j.diabres.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 25.Gao J, Wang J, Zheng P, Haardorfer R, Kegler MC, Zhu Y, Fu H. Effects of self-care, self-efficacy, social support on glycemic control in adults with type 2 diabetes. BMC Fam Pract. 2013;14:66. doi: 10.1186/1471-2296-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Osborn CY, Egede LE. Validation of an information-behavioral skills model of diabetes self-care (IMB-DSC) Patient Educ Couns. 2010;79(1):49–54. doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Egede LE, Osborn CY. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educ. 2010;36(2):276–283. doi: 10.1177/0145721710361389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tahmasebi R, Noroozi A, Sadat Tavafian S. Determinants of self-management among diabetic patients: a path analysis. Asia-Pacific J of Public Health. 2014 doi: 10.1177/1010539513475652. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 29.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, Karter AJ, Safford M, Waitzfelder B, Prata PA, Beckles GL. Socioeconomic position and health among persons with diabetes mellitus: a conceptual framework and review of the literature. Epidemiologic Reviews. 2004;26:63–77. doi: 10.1093/epirev/mxh002. [DOI] [PubMed] [Google Scholar]
- 30.National Center for Health Statistics . Survey Questionnaire, National Health Interview Survey, 2002. National Center for Health Statistics; Hyattsville, Maryland: 2004. Available at: cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2002/ [Google Scholar]
- 31.Cundiff JM, Smith TW, Uchino BN, Berg CA. Subjective social status: construct validity and associations with psychosocial vulnerability and self-rated health. Int J Behav Med. 2013;20(1):148–158. doi: 10.1007/s12529-011-9206-1. [DOI] [PubMed] [Google Scholar]
- 32.Egede LE, Ellis C. Development and psychometric properties of the 12-item diabetes fatalism scale. J Gen Intern Med. 2010;25:61–66. doi: 10.1007/s11606-009-1168-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wallston K, Rothman R, Cherrington A. Psychometric Properties of the Perceived Diabetes Self-Management Scale (PDSMS) J Behav Med. 2007;30:395–401. doi: 10.1007/s10865-007-9110-y. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): a diagnostic meta-analysis. J Gen Intern Med. 2007;22:1596–602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Annuls Fam Med. 2008;6(3):246–252. doi: 10.1370/afm.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SLT, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalence and trends in non-specific psychological distress. Psychological Medicine. 2002;32:959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 38.Sherbourne CD, Stewart AL. The MOS Social Support Survey. Social Science and Medicine. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 39.Cohen S, Williamson G. Perceived Stress in a Probability Sample of the United States. In: Spacapan S, Oskamp S, editors. The Social Psychology of Health. Sage; Newbury Park, CA: 1988. [Google Scholar]
- 40.Andreou E, Alexopoulos EC, Lionis C, Varvogli L, Gnardellis C, Chrousos GP, Darviri C. Perceived stress scale: reliability and validity study in Greece. Int J Environ Res Public Health. 2011;8:3287–3298. doi: 10.3390/ijerph8083287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self reported measure of medication adherence. Med Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- 42.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 43.Costello AB, Osborne JW. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Practical Assessment, Research and Evaluation. 2005;10(7) [Google Scholar]
- 44.Schreiber JB. Core reporting practices in structural equation modeling. Research in Social and Administrative Pharmacy. 2008;4:83–97. doi: 10.1016/j.sapharm.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 45.Byrne B. Factor analytic models: viewing the structure of an assessment instrument from three perspectives. Journal of Personality Assessment. 2005;85(1):17–32. doi: 10.1207/s15327752jpa8501_02. [DOI] [PubMed] [Google Scholar]
- 46.Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomized controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363:1589–1597. doi: 10.1016/S0140-6736(04)16202-8. [DOI] [PubMed] [Google Scholar]
- 47.Alam R, Sturt J, Lall R, Winkley K. An updated meta-analysis to assess the effectiveness of psychological specialists and generalist clinicians on glycaemic control and on psychological status. Patient Education and Counseling. 2009;75:25–36. doi: 10.1016/j.pec.2008.08.026. [DOI] [PubMed] [Google Scholar]