Abstract
Despite decades of work, behavioral interventions for obesity are not yet able to facilitate long-term weight loss maintenance for most participants. The current manuscript proposes an acceptance-based, self-regulation framework for understanding the challenge of maintaining changes in weight-related behavior and describes how this framework can be integrated into the behavioral treatment of obesity. According to this framework, intrinsic drives to consume palatable, high-calorie food interact with a modern environment in which high calorie foods are easily accessible. This combination produces a chronic desire to eat unhealthy foods that exists in opposition to individuals’ weight control goals. Similarly, energy expenditure requirements in the modern environment are limited, and people’s innate preferences to conserve energy typically prevent the concerted effort that would be necessary to engage in lifestyle activity and structured activity. Both external (e.g., sight of food) and internal (e.g., an aversive emotion) cues motivate overeating and sedentary behavior. However, individuals vary in their responsivity to these cues. While standard behavior skills may enable those lower in responsivity to successfully achieve weight control, we suggest that those higher in responsivity need specialized self-regulatory skills to maintain healthy eating and exercise behaviors. These skills include an ability to tolerate uncomfortable internal reactions to triggers and a reduction of pleasure, behavioral commitment to clearly-defined values, and metacognitive awareness of decision-making processes. So-called “acceptance-based” interventions based on these skills have so far proven efficacious for weight control, especially for those who are the most susceptible to eating in response to internal and external cues (as predicted by the model). Despite the current empirical support for the postulated model and for the interventions which stem from it, much remains to be learned including whether acceptance-based interventions will prove efficacious in the longer-term.
Keywords: Acceptance, mindfulness, behavioral therapy, weight control, weight loss, self-regulation
Current Status of Obesity Problem and Obesity Interventions
Obesity is associated with serious health problems and with a high proportion of the nation’s annual health care budget (Cawley & Meyerhoefer, 2012; Centers for Disease Control and Prevention, 2012; Danaei et al., 2009; Finkelstein, Trogdon, Cohen, & Dietz, 2009). Yet, a full two-thirds of adults in the United States are overweight (body mass index or BMI > 25 kg/m2) or obese (BMI > 30 mg/m2; Flegal, Carroll, Kit, & Ogden, 2012). Individuals who attempt to lose weight on their own commonly report that they abandon their efforts due to frustration with amount or rate of weight loss (Levy & Heaton, 1993; C. F. Smith, Burke, & Wing, 2000). Fewer than 20% of overweight adults in the general population have reported success with long-term weight loss (i.e., a reduction in weight of at least 10% maintained for at least 1 year; McGuire, Wing, & Hill, 1999).
Several categories of interventions have been aimed at the obesity epidemic with mixed success. For example, pharmacological and surgical treatments are moderately successful, but have considerable safety and efficacy concerns in the long-term and are considered second-line treatments and only for the most obese (Low, Bouldin, Sumrall, Loustalot, & Land, 2006; National Institutes of Health, 2000; Wadden, Crerand, & Brock, 2005; Yanovski & Yanovski, 2002). Public health interventions (e.g., taxing sugary drinks) have the potential to be highly impactful in the long-term, but only to the (so far minimal) extent that public/political support are in place (Wadden, Brownell, & Foster, 2002).
Cognitive-behavioral treatments have emerged as the gold standard and the first line of intervention for obesity (Jensen et al., 2013). These treatments (which we refer to as standard behavioral treatments to distinguish them from newer forms of behavioral treatments discussed later) typically include dietary and physical activity (PA)-related psychoeducation and prescriptions, behavioral skills such as self-monitoring and stimulus control, and cognitive strategies such as thought restructuring. Standard behavioral treatments commonly produce body weight reductions of 7–10% that are accompanied by decreases in risk factors for heart disease and diabetes (Butryn, Webb, & Wadden, 2011). Those who fully adhere to these regimens experience large weight losses and minimal weight regain (Klem, Wing, McGuire, Seagle, & Hill, 1997; Shick et al., 1998).
For all its successes, standard behavioral treatments yield relatively low adherence rates to calorie and PA prescriptions, and, as a result, participants receiving behavioral treatment lose far less weight than is achieved by individuals in a controlled environment in which adhere to these same prescriptions is guaranteed (Brownell & Jeffery, 1987; Hall, 2010; Heymsfield et al., 2007; K. G. Wilson, 1994). Moreover, most experience significant weight regain within a year of treatment ending and substantial, if not full, regain within 5 years (Fontaine & Cheskin, 1997; Jeffery et al., 2000; Kramer, Jeffery, Forster, & Snell, 1989; Stalonas, Perri, & Kerzner, 1984; Wadden & Butryn, 2003; Wadden & Frey, 1997; Wadden, Sternberg, Letizia, Stunkard, & Foster, 1989). Some weight regain appears attributable to changes in metabolic efficiency that are known to occur during and following weight loss (Rosenbaum, Kissileff, Mayer, Hirsch, & Leibel, 2010). However, these metabolic changes only account for a small degree of observed weight regain (de Boer, van Es, Roovers, van Raaij, & Hautvast, 1986; Heymsfield et al., 2007; Weinsier et al., 2000). Fundamentally, the disappointing long-term results of standard behavior treatment stem from difficulty making and/or maintaining recommended changes in dietary and PA behavior (Lowe, 2003). In the current manuscript, we argue that the difficulty maintaining adherence stems from an inability to exert behavioral self-control in the face of biologically-based responses to internal and external (environmental) cues.
Challenge of Behavior Change
A priority for addressing the obesity epidemic is to better understand the difficulty of successfully modifying and maintaining desired dietary and PA behaviors. Those who participate in obesity interventions are usually motivated to lose weight and receive extensive education in the behavioral changes that are required for successful weight control. However, it has been hypothesized that these motivations are (eventually) overwhelmed by a biological predisposition to consume high-energy foods, which are universally available in the modern environment. A large body of literature, which began with work of Schacter (1968), has established the importance of external environmental cues in influencing eating behavior. The modern environment is filled with readily available, high-energy, palatable foods, and labor-saving devices also appear to exploit a predisposition to conserve energy (Church et al., 2011; Diliberti, Bordi, Conklin, Roe, & Rolls, 2004; French, Story, & Jeffery, 2001; Hill & Peters, 1998; Hill, Wyatt, Reed, & Peters, 2003; Raynor & Epstein, 2001; Wansink, 2004). Susceptibility (or responsivity) to food cues has been shown to vary across individuals, and is a robust predictor of the ability to resist cravings (Appelhans et al., 2011), dietary success (Epstein et al., 2004; Stroebe, Papies, & Aarts, 2008), and BMI (Schultes, Ernst, Wilms, Thurnheer, & Hallschmid, 2010). In the modern environment, expending a sufficient amount of energy requires, for many individuals, purposeful and consistent choices to engage in lifestyle and/or structured PA (Catenacci et al., 2011; Jeffery, Wing, Sherwood, & Tate, 2003; Weinsier et al., 2002). This deliberate choice to be active is likely at odds with our intrinsic preference to conserve energy, and can be easily overridden by internal or external cues prompting sedentary behavior.
Our biology makes us highly susceptible to these internal and external cues for inactivity and overeating. Most individuals experience strong enough intrinsic cue responsiveness such that attempts to resist reactions to these cues are met with failure. Overeating in response to internal (e.g., emotional experiences) and external (presence of palatable high-calorie food) cues and/or engaging in inadequate amount of physical activity can be understood as a failure of self-regulation.
Psychological Skills Necessary for Successful Weight Control
In the modern environment, the chronicity of our desires combined with the pervasive ability to eat and be at rest suggest that overeating and sedentariness are default positions, i.e., the decisions we will make (whether implicitly or explicitly) unless we deliberately apply psychological skills designed to resist the powerful forces at work (Schulz et al., 2006; Tordoff, 2002; Wansink, 2006). Our synthesis of the literature and our recent work suggest several specific psychological skills that are needed to succeed at self-regulation in this regard.
Achieving values clarity and committing to values-linked behavioral goals
Pressure from the environment and innate tendencies degrade motivation to engage in weight control behaviors. In the most global sense, non-default, effortful choices are not likely to be made unless the individual has clearly linked these choices to goals that are part of an articulated, deeply felt values system (Eccles & Wigfield, 2002; Halpern, Ubel, & Asch, 2007). Thus, someone is less likely to forego a favorite dessert or get up early to walk unless she is clearly aware of and has committed to a value such as “being a physically active and fit grandparent” (Deci & Ryan, 2000; Hayes, Strosahl, & Wilson, 1999; Lillis, Hayes, Bunting, & Masuda, 2009; K. G. Wilson & Murrell, 2004). Motivation also may decrease after weight loss ends because there are fewer reinforcers for weight control behaviors (Wadden & Bell, 1992). Several studies have linked autonomous motivation and commitment to change with weight loss outcomes (M. H. Kearney, Rosal, Ockene, & Churchill, 2002; Williams, Grow, Freedman, Ryan, & Deci, 1996), and self- motivation predicts adherence to a PA regimen (Dishman & Ickes, 1981). A recent analog study demonstrated that participant exercise intensity was closer to a target heart rate when presented with statements related to values they had rated highly, relative to values rated as neutral or inconsistent with their own (Jackson et al., under review). These results are consistent with Self-Determination Theory (i.e., lasting behavior change is facilitated by internalizing values for change and accepting responsibility for autonomous regulation of behaviors; Deci & Ryan, 1987).
Metacognitive awareness
Social and cognitive psychology research indicates that implicit, automatic cognitive processes play a major role in the generation of behaviors, including those relevant to eating and PA. Evidence also indicates that people often simultaneously hold incompatible goals, such as hedonic pleasure and long-term health, and that implicit processes favoring certain goals are strengthened in the presence of specific stimuli. For instance, the sight of a tasty food has been shown to activate hedonic motivations and behaviors (Lowe & Butryn, 2007) and other cues, such as television, are likely to engage implicit processes leading to sedentary behavior. Importantly, one is typically not aware of the processes governing one’s health behavior decisions (e.g., what to eat, whether to go to the gym; Devine, 1989; Marcus, Rossi, Selby, Niaura, & Abrams, 1992; Wadden et al., 2002; T. D. Wilson, Lindsey, & Schooler, 2000; World Health Organization, 2010). Implicit processes are likely to favor hedonic pleasure, comfort, and sedentariness over long-term objectives (Friese, Hofmann, & Wänke, 2008; Mai et al., 2011). Thus, dietary and PA adherence demands self-regulation, which depends on the ability to maintain a continued awareness both of one's current behavior and of how that behavior compares with a relevant standard (Baumeister, 1998; Carver & Scheier, 1981, 1998; Miller, Galanter, & Pribram, 1960). Lack of awareness of behavior and its consequences results in “mindless” (Wansink, 2006) eating and activity decisions. Increased awareness and better understanding of our decision-making processes (metacognitive awareness) is likely to result in healthier decisions (Metcalfe & Mischel, 1999).
Of note, a large body of literature has examined one particular type of awareness – appetite awareness training – as a skill that may be necessary for weight control (Craighead & Allen, 1996; Kristeller, Wolever, & Sheets, 2014). The conceptual model presented next draws on some elements of that literature, in recognizing that awareness of hunger and fullness is one potentially useful element of eating-related decision making. However, research also suggests that “hunger” can be intensely experienced even in the absence of physiological need (e.g., hedonic hunger that is the result of environmental cues or craving that is the consequence of palatable food intake) (Lowe & Butryn, 2007). As such, it is possible that for some vulnerable individuals, eating-related decisions need to be guided by factors other than or in addition to hunger and fullness.
Ability to tolerate experiential distress and reduction in pleasure
Certain internal experiences (e.g., troubling thoughts, cravings, urges, sadness and anxiety) are universally experienced as aversive; however, individuals vary in the extent to which they tolerate or “accept” unpleasant experiences versus feel driven to diminish them psychologically (e.g., via suppression or distraction) or behaviorally (e.g., by performing an action likely to produce change in the experience; Hayes, Follette, & Linehan, 2004). Efforts to avoid or escape are negatively reinforced by temporary reductions of the unpleasant state, but such efforts tend to intensify distress over time. The degree to which one accepts versus strives to avoid such experiences is a robust predictor of health and psychological outcomes (e.g., binge eating; Telch, Agras, & Linehan, 2001), alcohol abuse (Brown, Evans, Miller, Burgess, & Mueller, 1997; Patten, Drews, Myers, Martin, & Wolter, 2002) and smoking (Brown, Lejuez, Kahler, & Strong, 2002; Patten et al., 2002).
We have argued that participants attempting to refrain from hedonically-motivated eating will experience internal discomfort such as cravings, powerful urges to eat, feelings of deprivation and thoughts about eating/food (Forman, Hoffman, et al., 2007). To the extent that individuals cannot tolerate the distress associated with experiencing these states, they will be motivated to eat in order to reduce this distress. In support of this notion, among women who completed a behavioral weight control program, the degree to which they were able to overcome urges to eat (as a ratio of overcoming urges to total urges) was predictive of weight loss from the end of treatment to 1-year follow-up (Bonato & Boland, 1987). Similarly, for many, PA results in unpleasant activity-related physiological sensations such as fatigue or sweating, boredom, or anxiety about time (Butryn, Forman, Hoffman, Shaw, & Juarascio, 2009). Lower tolerance for these internal experiences likely diminishes compliance with prescribed PA goals, especially as motivation decreases. A series of studies has demonstrated links between activity intensity, perceived aversiveness and choices made in regard to PA (Cabanac & Gosselin, 1996; Dishman, 1994; Lind, Joens-Matre, & Ekkekakis, 2005).
A second category of distress intolerance is the inability to tolerate negative affect. For instance, weight regainers have been shown to use eating to regulate and distract themselves from aversive emotional states (Byrne, Cooper, & Fairburn, 2003), and sadness and anxiety intolerance are associated with lapses (“emotional eating”) in weight control programs (Carels et al., 2001; Drapkin, Wing, & Shiffman, 1995; Finlayson, King, & Blundell, 2008; Grilo, Shiffman, & Wing, 1989; M. H. Kearney et al., 2002).
By referring to “experiential distress” and “distress tolerance” we are echoing terms that are now in common usage. However, we believe that successful self-control requires an ability not just to tolerate distress, but the ability to accept a state that is predicted/perceived to be less hedonically pleasurable than an alternative state. For example, a person may face a choice of eating an apple or a slice of birthday cake. Eating an apple is not a fundamentally aversive experience for most individuals, but choosing to eat an apple rather than a slice of birthday cake requires that the individual accept the reduced amount of pleasure he anticipates experiencing short-term from an apple compared to cake. Similarly, someone choosing to shut off the television and go for a walk is accepting the reduced pleasure (or at least the anticipation of reduced pleasure) that comes with walking versus watching television, but that needn’t imply that walking is judged to be distressing.
Conceptual Model
In our conceptual model (Figure 1), evolved neurobiological drives generate a chronic “wanting” for food and the desire to conserve energy (Finlayson et al., 2008; Rowland, 1998). These drives are activated by the presence of food and sedentary cues that are omnipresent in the current environment (Lowe et al., 2003). Internal states (emotion, fatigue) also cue a desire to move towards or maintain a higher hedonic state through consuming tasty foods and avoiding physical activity (Lowe et al., 2009). The model does not assume that healthy behavior has objectively less hedonic value than unhealthy behavior; instead, the assumption is that unhealthy behavior is sometimes perceived as having a higher hedonic value at the time a decision is made --often implicitly--to engage in the behavior.
Figure 1.
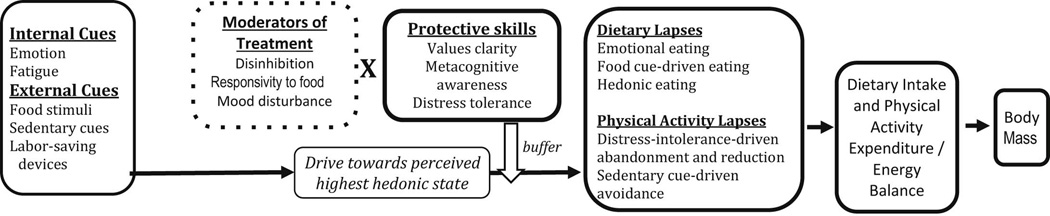
Conceptual model of weight gain and overweight.
An assumption of the model is that momentary cues produce drives to engage in behavior perceived to increase or maintain hedonic state. These drives often result in behavior that as at odds with intentions, i.e., dietary and PA lapses. (The cues and lapses specified in the model are exemplars, and are not meant to be exhaustive). Thus overconsumption and underactivity become default positions unless specific skills are engaged to protect against unhealthy decisions (Halpern et al., 2007). We posit that important self-regulation skills in this regard are: values clarity and behavioral commitment (which makes it more likely that health behavior decisions are tied to important life values), metacognitive awareness (which allows individuals to be aware of and override automatic decision making) and distress tolerance (which helps individuals tolerate reduction in pleasure as well as aversive cravings, physiological sensations and emotions).
Participants with high initial levels of disinhibition (Cuntz, Leibbrand, Ehrig, Shaw, & Fichter, 2001; Karlsson et al., 1994; Niemeier, Phelan, Fava, & Wing, 2007), responsivity to food (Cappelleri et al., 2009) and/or mood disturbance (McGuire, Wing, Klem, Lang, & Hill, 1999) are especially vulnerable to the cues that trigger dietary and PA lapses and therefore we propose that they will be in particular need of the protective skills. We conceptualize overconsumption/underactivity as momentary behaviors that, among those who have decided to lose/maintain weight, represent “lapses” in relation to intentions. Various types of eating (e.g., emotional eating, mindless overeating) and physical activity lapses (e.g., reducing the length of a bout of activity because of boredom, or failure to engage in a planned activity because of a sedentary cue) accumulate and eventuate the longer-spanning patterns of caloric consumption and activity expenditure that determine body mass.
An Acceptance-based Behavioral Approach to Dietary and Physical Activity Change
Behavioral treatments have evolved over time, with some scholars noting three waves of development: behavioral, cognitive and most recently the integration mindfulness- and experiential acceptance-based constructs (Hayes, 2004). Treatments in this “third wave” category, also referred to as acceptance-based therapies (ABTs), which include Mindfulness-based Cognitive Therapy (Segal, Teasdale, & Williams, 2004; Segal, Williams, & Teasdale, 2012), Dialectical Behavior Therapy (Linehan, 1993) and Acceptance and Commitment Therapy (ACT; Hayes, Strosahl, et al., 1999), have risen to prominence with exponential increases in empirical work and clinical usage (Forman & Herbert, 2009). These treatments differ from conventional cognitive-behavior therapies in that their goal is not to reduce the frequency of aversive experiences; rather, the aim is to foster willingness to experience potentially aversive internal experiences while simultaneously promoting behavior that is consistent with desired goals and values (Forman & Herbert, under review; Hayes, Strosahl, et al., 1999)..
A strong body of evidence, including several meta-analyses, supports the effectiveness of ACT and other ABTs for treating a wide range of problems, including depression and anxiety (Forman, Hebert, Moitra, Yeomans, & Geller, 2007), smoking cessation (Gifford et al., 2004), chronic pain (Veehof, Oskam, Schreurs, & Bohlmeijer, 2011), and diabetes management behaviors (i.e., diet, PA, glucose monitoring; Gregg, Callaghan, Hayes, & Glenn-Lawson, 2007; Hayes, Luoma, Bond, Masuda, & Lillis, 2006). In a recent meta-analytic synthesis, Ruiz (2012) found that ACT was superior to CBT for primary outcomes in 16 studies (N = 954, Hedges’ g = 0.40). Vollestad et al (2012) also reported an overall between-group Hedges’ g of 0.72–0.83 for studies comparing ABTs to an active control.
Analog laboratory studies and mediational analyses of outcome studies suggest that acceptance-based strategies are effective at promoting adaptive behavior (Annunziato, Zettle, & Bissett, 2003; Gifford et al., 2004; Hayes, Bissett, et al., 1999a; Woods, Wetterneck, & Flessner, 2006). Moreover, whereas the lack of support for postulated mechanisms of action in standard cognitive-behavioral interventions (e.g., cognitive change) has been increasingly noted by researchers (Dimidjian et al., 2006; Hayes, Strosahl, et al., 1999; Longmore & Worrell, 2007) theorized mediators of acceptance-based approaches, and ACT, in particular (Zettle & Hayes, 1987), have enjoyed strong support in trials of smoking cessation (Hernández-López, Luciano Soriano, Bricker, Roales-Nieto, & Montesinos Marin, 2009), diabetes management (Gregg et al., 2007), binge eating (Kristeller & Hallett, 1999) and obesity (Forman, Hoffman, et al., 2007; Lillis et al., 2009). Similarly, traditional cognitive components appear to offer no benefit over and above behavioral approaches, and yet acceptance-based cognitive components have been shown to be independently efficacious in laboratory studies (Levin, Hildebrandt, Lillis, & Hayes, 2012). For example, an isolated analog intervention that promoted mindful acceptance of smoking cravings resulted in longer ability to withstand a period of smoking abstinence (Bowen & Marlatt, 2009; Brewer et al., 2011).
We posit that acceptance-based strategies represent a particularly promising approach to weight control because the skills they build are a match for the capabilities that our model posits are necessary to achieve dietary and PA goals within an obesogenic environment. In particular, acceptance-based interventions focus on increasing the ability to tolerate distress, to achieve behavioral commitment towards better-articulated values and to be more metacognitively aware of in-the-moment decision-making processes.
Acceptance-based strategies focus on increasing the ability to tolerate aversive internal experiences, which is hypothesized to be a prerequisite to compliance with dietary and PA prescriptions. As opposed to traditional methods of behavior therapy that are based on attempts to control unpleasant internal states, acceptance-based strategies focus on experiential acceptance, which is defined as approaching (versus avoiding) psychologically aversive internal experiences while behaving adaptively. Acceptance-based strategies are consistent with the notion that we have limited ability to suppress, distract from, or modify thoughts and urges, and that adaptive behavior depends on the ability to tolerate unpleasant internal experiences. The approach explicitly teaches strategies (e.g., uncoupling urge and action) designed to increase tolerance in the service of goal-directed behavior, such as healthful eating and PA. Analog laboratory studies and mediational analyses of outcome studies suggest that these strategies are effective at promoting adaptive behavior (Annunziato et al., 2003; Bond & Bunce, 2000; Bond & Bunce, 2003; Gifford et al., 2004; Hayes, Bissett, et al., 1999b; Levitt, Brown, Orsillo, & Barlow, 2004; McCracken & Eccleston, 2006; Woods et al., 2006).
Acceptance-based strategies, and ACT in particular, are designed to facilitate the identification and internalization of values and lasting commitment to behavior consistent with these values, and thus should act against the waning of commitment generally observed among participants of long-term weight loss and PA interventions. As evident from its name, increasing commitment to valued goals is a key component of ACT (Hayes, Strosahl, et al., 1999). ACT theory recognizes that a behavior that continues or increases aversive internal experiences will only be undertaken when the individual has committed to higher-order life values. Thus, the therapy facilitates the identification/clarification of and commitment to such values. Moreover, the approach aims to make the participants’ moment-by-moment behavior choices referendums on whether one is remaining committed to one’s ultimate values versus a more immediate wish to decrease an aversive state (or increase a pleasurable one). ACT, in contrast to interventions that have added discrete motivational components (D. E. Smith, Heckemeyer, Kratt, & Mason, 1997; Woollard et al., 1995), is organized such that commitment and motivational issues pervade the entire treatment. Support for the importance of values-based interventions comes from a recent study which randomized participants who had completed a self-selected weight loss program (e.g., Weight Watchers) to a waitlist or a 1-day ACT workshop that was heavily centered around identifying and clarifying life values. At 3-months follow-up, waitlisted participants regained weight while those in the ACT condition continued to lose weight (t = 2.96, p < .01; Lillis et al., 2009).
Acceptance-based strategies also directly promote greater meta-cognitive awareness of in-the-moment perceptual, cognitive and affective experiences necessary to make health behavior decisions. Increased awareness of weight control goals, surroundings, and eating behavior itself will work against the disinhibiting effects of affective-cognitive load and poor contextual cues (e.g. container size) that constantly challenge people’s ability to exercise dietary restraint (Rolls, Roe, Kral, Meengs, & Wall, 2004; Wansink, 2004; Ward & Mann, 2000). Similarly, mindful awareness of activity-linked implicit processes (e.g., automatic anticipation of discomfort when anticipating physical activity rather than the pleasant and beneficial aspects of activity) is likely to result in pro-PA decisions.
Efficacy of Acceptance-Based Interventions for Weight Control
Until recently, only theoretical support existed for the notion that incorporating acceptance-based strategies into behavioral interventions would improve outcomes for treating obesity. However, the past few years has seen accumulating empirical support for acceptance-based behavioral interventions for weight control in the form of analog studies, open trials, workshop studies and randomized controlled trials.
Analog studies
Analog studies, while having limited external validity, are excellent methods of testing the initial efficacy of an intervention component under controlled, laboratory conditions. For example, we conducted two analog studies investigating the effectiveness of strategies for coping with food cravings, which was theorized to be critical to weight loss maintenance. In the first study, participants who regularly ate chocolate were asked to maintain a transparent box of Hershey’s kisses on their person for 48 hours, but were asked not to eat these or any other chocolates during the 48-hour time period. Before receiving the kisses, participants were randomized to receive one of two brief, one-session quasi-interventions: a standard cognitive-behavioral mini-intervention based on Brownell’s LEARN (Brownell, 2000) or an acceptance-based mini-intervention adapted from Hayes et al. (Hayes, Strosahl, et al., 1999). Results suggested that receiving the acceptance mini-intervention was associated with lower craving intensity and higher rates of successful chocolate abstinence among those most susceptible to food stimuli (Forman, Hoffman, et al., 2007). These results were echoed in a similar study in which all participants were overweight, the abstinence period was lengthened to 72 hours and the abstinence category was widened to include all sweets (Forman, Hoffman, Juarascio, Butryn, & Herbert, 2012).
Hooper and his colleagues (2012) randomized participants to one of three conditions: thought suppression instruction, defusion instruction (an acceptance-based strategy to step back and see thoughts, feelings and cravings as mental processes) or no instruction. Both active interventions were equally effective during a six-day abstinence period, but participants in the acceptance-based condition showed reduced rebound eating at a final, lab-based chocolate taste test.
Workshop studies
Several workshop studies have demonstrated that exposing overweight participants to a relatively low number of hours of intervention can have surprisingly long-lasting effects. For example, a 6-hour ACT-based workshop for individuals who had completed a weight loss program found that it produced an additional 1.5% weight loss at 3 months, relative to a 0.3% gain among waitlist controls (Lillis et al., 2009). Another study randomized 62 women to four 2-hour ACT workshops or to a control condition. Those assigned to the ACT workshop exhibited greater reductions in BMI at 6 months (−0.54 vs −0.04 kg/m2) and greater increases in PA (+2.2 vs −0.6 bouts/wk) compared to controls (Tapper et al., 2009). A weight gain prevention study which randomized 58 university students to 8 hours of ABT or an assessment-only control reported a 0.47 kg/m2 decrease in BMI for those receiving ABT at one year follow versus a gain of 0.74 kg/m2 for control participants (Katterman, Goldstein, Butryn, Forman, & Lowe, 2013).
Open trials
In a preliminary test of effectiveness and feasibility, we conducted an open trial of a 12-week group ABT for weight control (Forman, Butryn, Hoffman, & Herbert, 2009). Participants (n = 19) on average, lost 8.1% of their initial body weight during the 12-week intervention (i.e., 7.9 kg), and maintained weight loss (additional 1.7 kg or 2.2% loss) by 6-month follow-up. A small trial with cardiac patients resulted in clinically significant decreases in weight (M = 0.9 kg/week), and calorie, saturated fat and sodium intake, and increases in PA, as well as in theorized mediators (awareness and acceptance). In another uncontrolled trial, Niemeier (Niemeier, Leahey, Palm Reed, Brown, & Wing, 2012) administered a 24-session ABT program to overweight individuals with disinhibited eating, which is known to be resistant to standard weight control efforts. Post-treatment weight losses (12.0 kg) were considerably higher than expected, as was 3-month post-treatment weight loss maintenance (12.1 kg). Moreover, greater decreases in experiential avoidance were associated with greater weight losses, supporting the proposed mechanism of action in this population.
Full-scale randomized controlled trial
To our knowledge, only one full-scale RCT of ABT for obesity has been completed. We randomized 128 overweight participants to a year-long, 40-session group-based standard behavioral treatment or ABT. Prescriptions for calorie intake, physical activity, and weight loss were identical across conditions and all core components of behavioral treatment (i.e., those listed in “Components Common to Standard Behavioral Treatment and ABT” in Table 1) were included in both conditions. Weight loss at a 18 months, i.e., 6-month follow-up, was somewhat larger for those receiving ABT, but moderation analyses revealed that this advantage was especially powerful for participants with particular vulnerabilities, i.e., mood disturbance, elevated responsivity to food cues and high disinhibition (Forman et al., 2013). Moreover, when administered by weight control experts, as opposed to graduate student trainees, weight loss was significantly higher in ABT than standard behavioral treatment at 6-month follow-up (11.0% vs. 4.8). This result raises the possibility that those who have more experience in administering behavioral weight control interventions may be more successful at integrating acceptance-based principles into the behavioral program.
Table 1.
Commonalities of, and distinctions between, standard behavioral interventions and acceptance-based behavioral treatment
| Domain | Example Components Common to Both Standard Behavioral Treatment and ABT |
Example Components Unique to or More Strongly Emphasized in ABT |
Example Components Unique to or More Strongly Emphasized in Standard Behavioral Treatment |
|---|---|---|---|
| Psychoeducation |
|
|
|
| Awareness |
|
|
|
| Motivation |
|
|
|
| Meeting Challenges to Dietary Adherence |
|
|
|
| Meeting Challenges to PA Adherence |
|
|
|
Are some individuals better candidates for acceptance-based interventions for obesity?
The conceptual model predicts that acceptance-based treatments will be especially efficacious for those with greater susceptibility to cue-based eating. Consistent with that prediction, in our analog craving studies, ABT was more effective at promoting abstinence only for those who rated themselves as more susceptible to food cues. Moreover, the high weight loss maintenance in the Niemeier study was observed in a subgroup that had reported especially high disinhibited eating. In addition, in our RCT, moderation analyses revealed a powerful advantage of ABT over standard behavioral treatment only in those potentially more susceptible to eating cues. For example, mean weight losses in those with greater baseline depression symptomatology were 11.2% in ABT and 4.6% in standard behavioral treatment. A similar pattern of results was obtained for those higher in emotional eating (MABT = 10.5% vs. MBT = 6.0%), disinhibition (MABT = 8.3% vs. MBT = 6.4%), and responsivity to food cues (MABT = 9.7% vs. MBT = 4.5%). In combination, these results across studies strongly suggest that ABT is especially efficacious for those with particular susceptibility to eating in response to internal (e.g., feelings, thoughts, cravings) and external cues. This pattern of moderation is consistent with ABT’s focus on tolerating difficult internal experiences. Future research should determine whether individuals would be better off being matched to acceptance-based, traditional CBT or other type of weight control interventions on the basis of specific baseline characteristics.
Exemplar of an Acceptance-based Behavioral Treatment for Obesity
A variety of acceptance-based treatments have been developed including those that emphasize distress tolerance (Telch et al., 2001), those that emphasize mindful awareness of eating (Dalen et al., 2010; Kristeller & Hallett, 1999; Kristeller, Wolever, & Sheets, 2013), and those that emphasize developing fully internalized motivation not emanating from self-stigma (Lillis et al., 2009; Lillis & Kendra, 2014). In our analysis, no one pre-existing treatment is a perfect fit for weight control. ACT is likely the closest fit (see Lillis & Kendra, 2014 for an extended discussion of ACT for weight control), given its emphasis on values-based behavior change and behavioral commitment. However, its focus on building an ability to accept highly aversive internal experiences—as opposed to the loss of pleasure we posit is necessary to make adaptive health decisions—may be more suited to medical and psychological disorders characterized by emotional and physical pain. Also, according to Lillis and Kendra (2014) a conventional ACT framework would be skeptical of several standard behavior practices (e.g., use of frequent self-monitoring of weight; use of stimulus control to prevent temptation to avoid eating certain foods) and even the goal of weight loss itself because they may be viewed as forms of experiential avoidance for some individuals.
Mindfulness-based interventions that help people become better attuned to hunger and satiety cues offer promise. However, evidence suggests they are more successful at reducing binge eating than achieving weight loss, and it isn’t clear that mindfulness practice itself is useful in the context of resisting chronic drives to consume highly palatable foods (D. J. Kearney et al., 2012; Kristeller et al., 2013; Telch et al., 2001). We advocate a synthesis of behavioral change strategies best fitting the challenge of self-regulation in an obesogenic environment, including those drawn from traditional behavioral approaches and acceptance-based approaches.
Our treatment is behavioral at core, but with a heavy focus on acceptance- and commitment-based strategies (Hayes, Strosahl, et al., 1999). The treatment fuses state-of-the-art, comprehensive behavioral approaches (e.g., Diabetes Prevention Program; Brownell, 2000; Diabetes Prevention Program) and Look AHEAD (Look AHEAD Research Group, 2006) and the acceptance-based principles outlined above that are designed to facilitate participants’ dietary and PA adherence. Behavioral skills and goals are taught through the prism of acceptance-based concepts. In many instances, behavioral strategies are presented as necessary but not sufficient. For example, participants may have a specific stimulus control goal of limiting high-calorie dessert purchases, but to facilitate this goal they will use deliberate awareness of values and goals and distress tolerance when they walk by a bakery. To facilitate engagement in self-monitoring of weight and eating, the treatment teaches participants to use willingness to engage in this behavior, even when their initial response may be to avoid it. To prepare for specific upcoming challenges to dietary adherence, relapse prevention and planning for high-risk situations will be conducted, but participants will understand that there may remain a “gap” between their intention and their behavior that these techniques are not able to completely bridge, and a supplementary technique, such as urge surfing, may need to be used. Table 1 outlines differences and similarities between standard treatment acceptance-based behavioral treatments for weight control. The intervention can be described in terms of its three main components: commitment enhancement, distress tolerance and metacognitive awareness training.
Values clarity/commitment enhancement
Consistent with principles of ACT (Hayes, Strosahl, et al., 1999) and intrinsic motivation theory (Deci & Ryan, 1985), ABT emphasizes that participants must choose goals that emanate from freely-chosen, personal life values (e.g. living a long and healthy life; being a present, loving, active grandmother). A structured process for the identification of such life values will be followed and the connections between these values and eating and PA behaviors will be emphasized. Participants are taught that commitment to difficult behavioral goals, especially those that contain sustained exposure to unpleasant experiential states, is only likely to be maintained when one connects psychologically with life values important enough and meaningful enough to make such effort and sacrifice worthwhile. Participants also learn skills for being aware of their moment-by-moment behavior choices, and increasing the likelihood these reflect one’s ultimate goals (or values) rather than a more immediate wish to decrease an aversive state. Commitment is explicitly presented as a critical component of maintaining changes to the personal food and PA environment.
Distress tolerance
The intervention aims to help participants recognize that, 1) eating-related distress (urges to eat, hunger, cravings, feelings of deprivation) is bound to occur with high intensity and frequency in today’s obesogenic environment, and 2) attempts to avoid these internal experiences are ineffectual or even counterproductive. Participants learn to tolerate aversive states related to eating (e.g., cravings) and PA (e.g., boredom, discomfort) while continuing to engage in the desired behaviors. For example, in one session participants hold themselves in the “plank” (unsupported sitting) position and practice mindful awareness of the sensations generated. “Willingness” (simultaneously engaging in a valued action while accepting the discomfort it generates) is framed as more adaptive than distress intolerance (i.e., eating foods or ceasing/avoiding activity in order to avoid being uncomfortable). “Urge surfing” (to “ride” on top of waves of discomfort) and “defusion” (ability to distance oneself from unpleasant thoughts and feelings that could lead to overeating or sedentary behavior if they are acted upon) are examples of willingness skills (Marlatt & Kristeller, 1999). Experiential exercises allow participants to practice distancing themselves from thoughts and feelings in a way that enhances willingness to experience them, thereby reducing the necessity of acting (i.e. ending a walk early, eating a chocolate bar) to alter the experience. Participants are taught that attempts to suppress, distract from, or modify thoughts and urges are not expected to be productive; rather, long-term adherence to health behaviors depends on the ability to tolerate unpleasant internal experiences (e.g., fatigue, hunger, cravings, a sense of deprivation). Distress tolerance is also presented as a critical component of making and maintaining key environmental modifications. Participants are also taught to broadly conceive of tolerance as acceptance of a less pleasurable state over a more pleasurable state, when doing so is in the service of a valued goal.
Awareness training
The intervention incorporates training designed to help individuals increase awareness of the perceptual, cognitive and affective experiences that guide eating and PA decision making. Metaphors and experiential exercises are utilized to train participants to become more present-centered and aware, thereby reducing the likelihood that they will engage in “mindless” eating and activity behaviors. Participants are asked to monitor their bodily reactions and feelings before, during, and after eating and exercise to explore their cognitive and affective responses. Unlike conventional mindful eating interventions, this training has a major focus on helping participants more consistently make “mindful” deliberate behavioral choices including what food to buy and eat, when to eat, when to stop eating, when to start and stop PA, and even decisions relevant to one’s personal food/PA environment. These skills are designed to interrupt automatic, nonconscious influences on eating behavior that can lead to overeating and/or sedentary behavior.
Conclusion
Behavioral treatments for obesity have proven moderately successful in the short-term, but largely unsuccessful in the long-term. As such, the field is pressed to develop models of overweight that account for the failure of standard behavioral treatments and suggest alternative methods of intervention. In the model posited in the current manuscript, weight gain and regain is the product of a combination of our intrinsic drives to consume palatable food and minimize activity and an environment in which high calorie foods and labor saving devices are easily accessible. This combination produces a chronic tension between individuals’ explicit health goals and inherent drives. The attempted restraint will break down, resulting in poor eating and activity decisions (lapses), in response to both external (e.g., sight of food) and internal (e.g., an aversive emotion) cues. Disinhibition of restraint will occur frequently enough that high body mass is inevitable unless individuals are able to employ particular skills. We posit that these skills are: behavioral commitment to clearly-defined values, distress tolerance and metacognitive awareness of decision-making processes. The fact that standard behavioral treatments spend relatively little time on these skills may account for its limited success. In contrast, these skills are at the center of acceptance-based behavioral treatments. Perhaps it is not surprising, then, that a range of analog, workshop, open trial and randomized controlled trials have supported the efficacy of acceptance-based behavioral treatments for obesity. As predicted from the model, a pattern of results has emerged from these studies suggesting that ABT is particularly effective for those who are the most susceptible to eating in response to internal and external cues.
Despite the promise of acceptance-based treatments for obesity a number of important questions remain. For example, with a few exceptions (e.g., Carels et al., 2001), no research has been conducted using ecologically-valid, real-time measurement to convincingly reveal which implicit and explicit processes lead to eating and physical activity decisions. Of great import, acceptance-based treatments have not yet been tested in the longer term which is when the failure of behavioral treatments has been most evident. In addition, we do not yet have strong evidence which of the individual acceptance, standard cognitive and behavioral components of treatment are the most active ingredients of weight loss and weight loss maintenance. Thus, while the current acceptance-based behavioral framework may be a promising start for understanding and reversing the obesity epidemic, much works remains.
Highlights.
A self-regulation framework is applied to the challenge of weight control
The framework calls for a acceptance-, commitment-based behavioral treatment
A critical skill to develop is the ability to tolerate discomfort/reduction of pleasure
A 2nd key self-regulation skill is behavioral commitment to clearly-defined values
A third important skill is metacognitive awareness of decision-making processes
Treatments incorporating these elements have demonstrated promising results
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Annunziato RA, Zettle RD, Bissett RT. Acceptance and commitment therapy (act) vs. Systematic desensitization in treatment of mathematics anxiety. Psychological Record. 2003;53(2):197–215. [Google Scholar]
- Appelhans BM, Woolf K, Pagoto SL, Schneider KL, Whited MC, Liebman R. Inhibiting food reward: Delay discounting, food reward sensitivity, and palatable food intake in overweight and obese women. Obesity. 2011;19(11):2175–2182. doi: 10.1038/oby.2011.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumeister R. The self. In: Gilbert D, Fiske S, Lindzey G, editors. The handbook of social psychology. Boston: McGraw-Hill; 1998. [Google Scholar]
- Bonato DP, Boland FJ. Predictors of weight loss at the end of treatment and 1-year follow-up for a behavioral weight loss program. Int J Eat Disord. 1987;6:573–577. [Google Scholar]
- Bond FW, Bunce D. Mediators of change in emotion-focused and problem-focused worksite stress management interventions. Journal of Occupational Health Psychology. 2000;5(1):156–163. doi: 10.1037//1076-8998.5.1.156. [DOI] [PubMed] [Google Scholar]
- Bond FW, Bunce D. The role of acceptance and job control in mental health, job satisfaction, and work performance. J Appl Psychol. 2003;88(6):1057–1067. doi: 10.1037/0021-9010.88.6.1057. [DOI] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: Brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors. 2009;23(4):666. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, Weinstein AJ. Mindfulness training for smoking cessation: Results from a randomized controlled trial. Drug and alcohol dependence. 2011;119(1):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Evans DM, Miller IW, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. J Consult Clin Psychol. 1997;65(5):715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111(1):180–185. [PubMed] [Google Scholar]
- Brownell KD. The learn program for weight management. Dallas, TX: American Health; 2000. [Google Scholar]
- Brownell KD, Jeffery RW. Improving long-term weight loss: Pushing the limits of treatment. Behavior Therapy. 1987;18(4):353–374. [Google Scholar]
- Butryn ML, Forman EM, Hoffman KL, Shaw JA, Juarascio AS. A pilot study of acceptance and commitment therapy for promotion of physical activity. doi: 10.1123/jpah.8.4.516. in press. [DOI] [PubMed] [Google Scholar]
- Butryn ML, Webb V, Wadden TA. Behavioral treatment of obesity. Psychiatr Clin North Am. 2011;34(4):841. doi: 10.1016/j.psc.2011.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne S, Cooper Z, Fairburn C. Weight maintenance and relapse in obesity: A qualitative study. Int J Obes Relat Metab Disord. 2003;27(8):955–962. doi: 10.1038/sj.ijo.0802305. [DOI] [PubMed] [Google Scholar]
- Cabanac M, Gosselin C. Ponderostat: Hoarding behavior satisfies the condition for a lipostat in the rat. Appetite. 1996;27(3):251–261. doi: 10.1006/appe.1996.0050. [DOI] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Karlsson J, Lowe MR. Evaluating the power of food scale in obese subjects and a general sample of individuals: Development and measurement properties. International Journal of Obesity. 2009;33(8):913–922. doi: 10.1038/ijo.2009.107. [DOI] [PubMed] [Google Scholar]
- Carels RA, Hoffman J, Collins A, Raber AC, Cacciapaglia H, O'Brien WH. Ecological momentary assessment of temptation and lapse in dieting. Eat Behav. 2001;2(4):307–321. doi: 10.1016/s1471-0153(01)00037-x. [DOI] [PubMed] [Google Scholar]
- Carver CS, Scheier MF. Attention and self-regulation: A control-theory approach to human behavior. New York: Springer; 1981. [Google Scholar]
- Carver CS, Scheier MF. On the self-regulation of behavior. New York: Cambridge University Press; 1998. [Google Scholar]
- Catenacci VA, Grunwald GK, Ingebrigtsen JP, Jakicic JM, McDermott MD, Phelan S, Wyatt HR. Physical activity patterns using accelerometry in the national weight control registry. Obesity. 2011;19(6):1163–1170. doi: 10.1038/oby.2010.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawley J, Meyerhoefer C. The medical care costs of obesity: An instrumental variables approach. Journal of health economics. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Overweight and obesity. 2012 Retrieved July 24, 2012, from http://www.cdc.gov/obesity/
- Church TS, Thomas DM, Tudor-Locke C, Katzmarzyk PT, Earnest CP, Rodarte RQ, Bouchard C. Trends over 5 decades in u.S. Occupation-related physical activity and their associations with obesity. PLoS ONE. 2011;6(5):e19657. doi: 10.1371/journal.pone.0019657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craighead LW, Allen HN. Appetite awareness training: A cognitive behavioral intervention for binge eating. Cognitive and Behavioral Practice. 1996;2(2):249–270. [Google Scholar]
- Cuntz U, Leibbrand R, Ehrig C, Shaw R, Fichter MM. Predictors of post-treatment weight reduction after in-patient behavioral therapy. Int J Obes Relat Metab Disord. 2001;25(Suppl 1):S99–S101. doi: 10.1038/sj.ijo.0801710. [DOI] [PubMed] [Google Scholar]
- Dalen J, Smith BW, Shelley BM, Sloan AL, Leahigh L, Begay D. Pilot study: Mindful eating and living (meal): Weight, eating behavior, and psychological outcomes associated with a mindfulness-based intervention for people with obesity. Complementary therapies in medicine. 2010;18(6):260–264. doi: 10.1016/j.ctim.2010.09.008. [DOI] [PubMed] [Google Scholar]
- Danaei G, Ding EL, Mozaffarian D, Taylor B, Rehm J, Murray CJ, Ezzati M. The preventable causes of death in the united states: Comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS medicine. 2009;6(4):e1000058. doi: 10.1371/journal.pmed.1000058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer JO, van Es AJ, Roovers LC, van Raaij JM, Hautvast JG. Adaptation of energy metabolism of overweight women to low-energy intake, studied with whole-body calorimeters. Am J Clin Nutr. 1986;44(5):585–595. doi: 10.1093/ajcn/44.5.585. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. [Google Scholar]
- Deci EL, Ryan RM. The support of autonomy and the control of behavior. J Pers Soc Psychol. 1987;53(6):1024–1037. doi: 10.1037//0022-3514.53.6.1024. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. The "what" and "why" of goal pursuits: Human needs and the self-determination of behavior. Psychological Inquiry: An International Journal for the Advancement of Psychological Theory. 2000;11(4):227–268. [Google Scholar]
- Devine PG. Stereotypes and prejudice: Their automatic and controlled components. J Pers Soc Psychol. 1989;56:5–18. [Google Scholar]
- Diabetes Prevention Program. Retrieved November 8, 2007, from University of Pittsburgh http://www.bsc.gwu.edu/dpp/manuals.htmlvdoc.
- Diliberti N, Bordi PL, Conklin MT, Roe LS, Rolls BJ. Increased portion size leads to increased energy intake in a restaurant meal. Obesity research. 2004;12(3):562–568. doi: 10.1038/oby.2004.64. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, Jacobson NS. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology. 2006;74(4):658–670. doi: 10.1037/0022-006X.74.4.658. [DOI] [PubMed] [Google Scholar]
- Dishman RK. Prescribing exercise intensity for healthy adults using perceived exertion. Medicine & Science in SPorts & Exercise. 1994;26(9):1087–1094. [PubMed] [Google Scholar]
- Dishman RK, Ickes W. Self-motivation and adherence to therapeutic exercise. Journal of behavioral medicine. 1981;4(4):421–438. doi: 10.1007/BF00846151. [DOI] [PubMed] [Google Scholar]
- Drapkin RG, Wing RR, Shiffman S. Responses to hypothetical high risk situations: Do they predict weight loss in a behavioral treatment program or the context of dietary lapses? Health Psychol. 1995;14(5):427–434. doi: 10.1037//0278-6133.14.5.427. [DOI] [PubMed] [Google Scholar]
- Eccles JS, Wigfield A. Motivational beliefs, values, and goals. Annual review of psychology. 2002;53:109–132. doi: 10.1146/annurev.psych.53.100901.135153. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Wright SM, Paluch RA, Leddy J, Hawk LW, Jr, Jaroni JL, Lerman C. Food hedonics and reinforcement as determinants of laboratory food intake in smokers. Physiology & Behavior. 2004;81(3):511–517. doi: 10.1016/j.physbeh.2004.02.015. [DOI] [PubMed] [Google Scholar]
- Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health affairs. 2009;28(5):w822–w831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- Finlayson G, King N, Blundell J. The role of implicit wanting in relation to explicit liking and wanting for food: Implications for appetite control. Appetite. 2008;50(1):120–127. doi: 10.1016/j.appet.2007.06.007. [DOI] [PubMed] [Google Scholar]
- Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among us adults, 1999–2010. Jama. 2012;307(5):491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- Fontaine KR, Cheskin LJ. Self-efficacy, attendance, and weight loss in obesity treatment. Addict Behav. 1997;22:567–570. doi: 10.1016/s0306-4603(96)00068-8. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn M, Juarascio A, Bradley L, Lowe M, Herbert J, Shaw J. The mind your health project: A randomized controlled trial of an innovative behavioral treatment for obesity. Obesity. 2013 doi: 10.1002/oby.20169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Hoffman KL, Herbert JD. An open trial of an acceptance-based behavioral treatment for weight loss. Cognitive and Behavioral Practice. 2009;16:223–235. [Google Scholar]
- Forman EM, Hebert JD, Moitra E, Yeomans PD, Geller PA. A randomized controlled effectiveness trial of acceptance and commitment therapy and cognitive therapy for anxiety and depression. Behavior Modification. 2007;31(6):772–799. doi: 10.1177/0145445507302202. [DOI] [PubMed] [Google Scholar]
- Forman EM, Herbert JD. New directions in cognitive behavior therapy: Acceptance-based therapies. General principles and empirically supported techniques of cognitive behavior therapy. 2009:77–101. [Google Scholar]
- Forman EM, Herbert JD. Comparing and contrasting cognitive behavior therapy and acceptance and commitment therapy: Theory, technology, effectiveness, and mechanisms. (under review) [Google Scholar]
- Forman EM, Hoffman K, McGrath KB, Herbert J, Brandsma L, Lowe MR. A comparison of acceptance- and control-based strategies for coping with food cravings: An analog study. Behaviour Research and Therapy. 2007;45(10):2372–2386. doi: 10.1016/j.brat.2007.04.004. [DOI] [PubMed] [Google Scholar]
- Forman EM, Hoffman KL, Juarascio AS, Butryn ML, Herbert JD. Comparison of acceptance-based and standard cognitive-based coping strategies for craving sweets in overweight and obese women. Eating behaviors. 2012 doi: 10.1016/j.eatbeh.2012.10.016. [DOI] [PubMed] [Google Scholar]
- French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- Friese M, Hofmann W, Wänke M. When impulses take over: Moderated predictive validity of explicit and implicit attitude measures in predicting food choice and consumption behaviour. British Journal of Social Psychology. 2008;47(3):397–419. doi: 10.1348/014466607X241540. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35(4):689–705. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: A randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75(2):336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- Grilo CM, Shiffman S, Wing RR. Relapse crises and coping among dieters. J Consult Clin Psychol. 1989;57(4):488–495. doi: 10.1037//0022-006x.57.4.488. [DOI] [PubMed] [Google Scholar]
- Hall KD. Predicting metabolic adaptation, body weight change, and energy intake in humans. American Journal of Physiology-Endocrinology and Metabolism. 2010;298(3):E449. doi: 10.1152/ajpendo.00559.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. The New England journal of medicine. 2007;357(13):1340–1344. doi: 10.1056/NEJMsb071595. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies. Behavior Therapy. 2004;35(4):639–665. doi: 10.1016/j.beth.2016.11.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Bissett RT, Korn Z, Zettle RD, Rosenfarb I, Cooper L, Grundt A. The impact of acceptance versus control rationales on pain tolerance. The Psychological Record. 1999a;49:33–47. [Google Scholar]
- Hayes SC, Bissett RT, Korn Z, Zettle RD, Rosenfarb IS, Cooper LD, Grundt AM. The impact of acceptance versus control rationales on pain tolerance. Psychological Record. 1999b;49(1):33–47. [Google Scholar]
- Hayes SC, Follette VM, Linehan MM. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York, NY: Guilford Press; 2004. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behav Res Ther. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Hernández-López M, Luciano Soriano MC, Bricker JB, Roales-Nieto JG, Montesinos Marin F. Acceptance and commitement therapy for smoking cessation: A preliminary study of its effectivenedd in comparison with cognitive behavioral therapy. Psychology of Addictive Behaviors. 2009;23(4):723–730. doi: 10.1037/a0017632. [DOI] [PubMed] [Google Scholar]
- Heymsfield SB, Harp JB, Reitman ML, Beetsch JW, Schoeller DA, Erondu N, Pietrobelli A. Why do obese patients not lose more weight when treated with low-calorie diets? A mechanistic perspective. The American journal of clinical nutrition. 2007;85(2):346–354. doi: 10.1093/ajcn/85.2.346. [DOI] [PubMed] [Google Scholar]
- Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280(5368):1371–1374. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: Where do we go from here? Science. 2003;299(5608):853–855. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- Hooper N, Sandoz EK, Ashton J, Clarke A, McHugh L. Comparing thought suppression and acceptance as coping techniques for food cravings. Eating behaviors. 2012;13(1):62–64. doi: 10.1016/j.eatbeh.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Jackson ML, Williams LW, Hayes SC, Humphreys T, Gauthier B, Westwood R. Whatever gets your heart pumping: Using implicit measures to select motivative exercise statements. (under review) [Google Scholar]
- Jeffery RW, Epstein LH, Wilson GT, Drewnowski A, Stunkard AJ, Wing RR. Long-term maintenance of weight loss: Current status. Health Psychol. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? The American journal of clinical nutrition. 2003;78(4):684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, Yanovski SZ. 2013 aha/acc/tos guideline for the management of overweight and obesity in adults: A report of the american college of cardiology/american heart association task force on practice guidelines and the obesity society. Circulation. 2013 [Google Scholar]
- Karlsson J, Hallgren P, Kral J, Lindroos AK, Sjostrom L, Sullivan M. Predictors and effects of long-term dieting on mental well-being and weight loss in obese women. Appetite. 1994;23(1):15–26. doi: 10.1006/appe.1994.1031. [DOI] [PubMed] [Google Scholar]
- Katterman SN, Goldstein SP, Butryn ML, Forman EM, Lowe MR. Efficacy of an acceptance-based behavioral intervention for weight gain prevention in young adult women. Journal of Contextual Behavioral Science. 2013 [Google Scholar]
- Kearney DJ, Milton ML, Malte CA, McDermott KA, Martinez M, Simpson TL. Participation in mindfulness-based stress reduction is not associated with reductions in emotional eating or uncontrolled eating. Nutrition Research. 2012;32(6):413–420. doi: 10.1016/j.nutres.2012.05.008. [DOI] [PubMed] [Google Scholar]
- Kearney MH, Rosal MC, Ockene JK, Churchill LC. Influences on older women's adherence to a low-fat diet in the women's health initiative. Psychosom Med. 2002;64(3):450–457. doi: 10.1097/00006842-200205000-00009. [DOI] [PubMed] [Google Scholar]
- Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66(2):239–246. doi: 10.1093/ajcn/66.2.239. [DOI] [PubMed] [Google Scholar]
- Kramer FM, Jeffery RW, Forster JL, Snell MK. Long-term follow-up of behavioral treatment for obesity: Patterns of weight regain among men and women. Int J Obes. 1989;13:123–136. [PubMed] [Google Scholar]
- Kristeller JL, Hallett C. An exploratory study of a meditation-based intervention for binge eating disorder. Journal of Health Psychology. 1999;4:357–363. doi: 10.1177/135910539900400305. [DOI] [PubMed] [Google Scholar]
- Kristeller JL, Wolever RQ, Sheets V. Mindfulness-based eating awareness training (mb-eat) for binge eating: A randomized clinical trial. Mindfulness. 2013:1–16. [Google Scholar]
- Kristeller JL, Wolever RQ, Sheets V. Mindfulness-based eating awareness training (mb-eat) for binge eating: A randomized clinical trial. Mindfulness. 2014;5(3):282–297. [Google Scholar]
- Levin ME, Hildebrandt MJ, Lillis J, Hayes SC. The impact of treatment components suggested by the psychological flexibility model: A meta-analysis of laboratory-based component studies. Behav Ther. 2012;43(4):741–756. doi: 10.1016/j.beth.2012.05.003. [DOI] [PubMed] [Google Scholar]
- Levitt JT, Brown TA, Orsillo SM, Barlow DH. The effects of acceptance versus suppression of emotion on subjective and psychophysiological response to carbon dioxide challenge in patients with panic disorder. Behavior Therapy. 2004;35(4):747–766. [Google Scholar]
- Levy AS, Heaton AW. Weight control practices of us adults trying to lose weight. Annals of Internal Medicine. 1993;119:661–666. doi: 10.7326/0003-4819-119-7_part_2-199310011-00007. (7_Part_2) [DOI] [PubMed] [Google Scholar]
- Lillis J, Hayes SC, Bunting K, Masuda A. Teaching acceptance and mindfulness to improve the lives of the obese: A preliminary test of a theoretical model. Annals of Behavioral Medicine. 2009;37(1):58–69. doi: 10.1007/s12160-009-9083-x. [DOI] [PubMed] [Google Scholar]
- Lillis J, Kendra KE. Acceptance and commitment therapy for weight control: Model, evidence, and future directions. Journal of Contextual Behavioral Science. 2014 doi: 10.1016/j.jcbs.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lind E, Joens-Matre RR, Ekkekakis P. What intensity of physical activity do previously sedentary middle-aged women select? Evidence of a coherent pattern from physiological perceptual, and affective markers. Preventive Medicine. 2005;40:407–419. doi: 10.1016/j.ypmed.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive-behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy? Clinical Psychology Review. 2007;27(2):173–187. doi: 10.1016/j.cpr.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Look AHEAD Research Group. The look ahead study: A description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring, Md.) 2006;14(5):737. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Low AK, Bouldin MJ, Sumrall CD, Loustalot FV, Land KK. A clinician's approach to medical management of obesity. Am J Med Sci. 2006;331(4):175–182. doi: 10.1097/00000441-200604000-00003. [DOI] [PubMed] [Google Scholar]
- Lowe MR. Self-regulation of energy intake in the prevention and treatment of obesity: Is it feasible? Obes Res. 2003;(11 Suppl):44S–59S. doi: 10.1038/oby.2003.223. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Annunziato R, Riddell L, Didie ER, Crerand C, Butryn ML, McKinney S. Reduced energy density eating and weight loss maintenance: 18-month follow-up results from a randomized controlled trial; Paper presented at the Annual meeting of the North American Association for the Study of Obesity; Fort Lauderdale, FL. 2003. [Google Scholar]
- Lowe MR, Butryn ML. Hedonic hunger: A new dimension of appetite? Physiology & Behavior. 2007;91(4):432–439. doi: 10.1016/j.physbeh.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Butryn ML, Didie ER, Annunziato RA, Thomas JG, Crerand CE, Halford J. The power of food scale. A new measure of the psychological influence of the food environment. Appetite. 2009;53(1):114–118. doi: 10.1016/j.appet.2009.05.016. [DOI] [PubMed] [Google Scholar]
- Mai R, Hoffmann S, Helmert JR, Velichkovsky BM, Zahn S, Jaros D, Rohm H. Implicit food associations as obstacles to healthy nutrition: The need for further research. The British Journal of Diabetes & Vascular Disease. 2011;11(4):182–186. [Google Scholar]
- Marcus BH, Rossi JS, Selby VC, Niaura RS, Abrams DB. The stages and processes of exercise adoption and maintenance in a worksite sample. Health Psychology. 1992;11(6):386–395. doi: 10.1037//0278-6133.11.6.386. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Kristeller JL. Mindfulness and meditation. In: Miller WR, editor. Integrating spirituality in treatment. Washington, DC: American Psychological Association; 1999. pp. 67–84. [Google Scholar]
- McCracken LM, Eccleston C. A comparison of the relative utility of coping and acceptance-based measures in a sample of chronic pain sufferers. European Journal of Pain. 2006;10(1):23–29. doi: 10.1016/j.ejpain.2005.01.004. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Hill JO. The prevalence of weight loss maintenance among american adults. International Journal of Obesity & Related Metabolic Disorders. 1999;23(12) doi: 10.1038/sj.ijo.0801075. [DOI] [PubMed] [Google Scholar]
- McGuire MT, Wing RR, Klem ML, Lang W, Hill JO. What predicts weight regain in a group of successful weight losers? Journal of Consulting and Clinical Psychology. 1999;67:177–185. doi: 10.1037//0022-006x.67.2.177. [DOI] [PubMed] [Google Scholar]
- Metcalfe J, Mischel W. A hot/cool-system analysis of delay of gratification: Dynamics of willpower. Psychological review. 1999;106(1):3–19. doi: 10.1037/0033-295x.106.1.3. [DOI] [PubMed] [Google Scholar]
- Miller GA, Galanter E, Pribram KH. Plans and the structure of behavior. New York: Holt, Rinehart & Winston; 1960. [Google Scholar]
- National Institutes of Health. The practical guide: Identification, evaluation, and treatment of overweight and obesity in adults (nih publication no. 00–4084) 2000
- Niemeier HM, Leahey T, Palm Reed K, Brown RA, Wing RR. An acceptance-based behavioral intervention for weight loss: A pilot study. Behavior Therapy. 2012;43(2):427–435. doi: 10.1016/j.beth.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niemeier HM, Phelan S, Fava JL, Wing RR. Internal disinhibition predicts weight regain following weight loss and weight loss maintenance. Obesity. 2007;15(10):2485–2494. doi: 10.1038/oby.2007.295. [DOI] [PubMed] [Google Scholar]
- Patten CA, Drews AA, Myers MG, Martin JE, Wolter TD. Effect of depressive symptoms on smoking abstinence and treatment adherence among smokers with a history of alcohol dependence. Psychol Addict Behav. 2002;16(2):135–142. doi: 10.1037//0893-164x.16.2.135. [DOI] [PubMed] [Google Scholar]
- Raynor HA, Epstein LH. Dietary variety, energy regulation, and obesity. Psychological bulletin. 2001;127(3):325–341. doi: 10.1037/0033-2909.127.3.325. [DOI] [PubMed] [Google Scholar]
- Rolls BJ, Roe LS, Kral TV, Meengs JS, Wall DE. Increasing the portion size of a packaged snack increases energy intake in men and women. Appetite. 2004;42(1):63–69. doi: 10.1016/S0195-6663(03)00117-X. [DOI] [PubMed] [Google Scholar]
- Rosenbaum M, Kissileff HR, Mayer LE, Hirsch J, Leibel RL. Energy intake in weight-reduced humans. Brain research. 2010;1350:95–102. doi: 10.1016/j.brainres.2010.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowland TW. The biological basis of physical activity. Medicine and Science in Sports and Exercise. 1998;30(3):392–399. doi: 10.1097/00005768-199803000-00009. [DOI] [PubMed] [Google Scholar]
- Ruiz FJ. Acceptance and commitment therapy versus traditional cognitive behavioral therapy: A systematic review and meta-analysis of current empirical evidence. International journal of psychology and psychological therapy. 2012;12(3):333–358. [Google Scholar]
- Schultes B, Ernst B, Wilms B, Thurnheer M, Hallschmid M. Hedonic hunger is increased in severely obese patients and is reduced after gastric bypass surgery. The American journal of clinical nutrition. 2010;92(2):277–283. doi: 10.3945/ajcn.2009.29007. [DOI] [PubMed] [Google Scholar]
- Schulz LO, Bennett PH, Ravussin E, Kidd JR, Kidd KK, Esparza J, Valencia ME. Effects of traditional and western environments on prevalence of type 2 diabetes in pima indians in mexico and the us. Diabetes Care. 2006;29(8):1866–1871. doi: 10.2337/dc06-0138. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams JMG. Mindfulness-based cognitive therapy: Theoretical rationale and empirical status. 2004 [Google Scholar]
- Segal ZV, Williams JMG, Teasdale JD. Mindfulness-based cognitive therapy for depression. Guilford Press; 2012. [Google Scholar]
- Shick SM, Wing RR, Klem ML, McGuire MT, Hill JO, Seagle H. Persons successful at long-term weight loss and maintenance continue to consume a low-energy, low-fat diet. J Am Diet Assoc. 1998;98(4):408–413. doi: 10.1016/S0002-8223(98)00093-5. [DOI] [PubMed] [Google Scholar]
- Smith CF, Burke LE, Wing RR. Vegetarian and weight-loss diets among young adults. Obesity research. 2000;8(2):123–129. doi: 10.1038/oby.2000.13. [DOI] [PubMed] [Google Scholar]
- Smith DE, Heckemeyer CM, Kratt PP, Mason DA. Motivational interviewing to improve adherence to a behavioral weight-control program for older obese women with niddm. A pilot study. Diabetes Care. 1997;20(1):52–54. doi: 10.2337/diacare.20.1.52. [DOI] [PubMed] [Google Scholar]
- Stalonas PM, Perri MG, Kerzner AB. Do behavioral treatments of obesity last? A five-year follow-up investigation. Addict Behav. 1984;9:175–183. doi: 10.1016/0306-4603(84)90054-6. [DOI] [PubMed] [Google Scholar]
- Stroebe W, Papies EK, Aarts H. From homeostatic to hedonic theories of eating: Self-regulatory failure in food-rich environments. Applied Psychology. 2008;(1):57. 172–193. [Google Scholar]
- Tapper K, Shaw C, Ilsley J, Hill AJ, Bond FW, Moore L. Exploratory randomised controlled trial of a mindfulness-based weight loss intervention for women. Appetite. 2009;52(2):396–404. doi: 10.1016/j.appet.2008.11.012. [DOI] [PubMed] [Google Scholar]
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. J Consult Clin Psychol. 2001;69(6):1061–1065. doi: 10.1037//0022-006x.69.6.1061. [DOI] [PubMed] [Google Scholar]
- Tordoff MG. Obesity by choice: The powerful influence of nutrient availability on nutrient intake. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 2002;282(5):R1536–R1539. doi: 10.1152/ajpregu.00739.2001. [DOI] [PubMed] [Google Scholar]
- Veehof MM, Oskam MJ, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain. 2011;152(3):533–542. doi: 10.1016/j.pain.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Vøllestad J, Nielsen MB, Nielsen GH. Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis. British Journal of Clinical Psychology. 2012;51(3):239–260. doi: 10.1111/j.2044-8260.2011.02024.x. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Bell ST. Obesity. In: Bellack AS, Hersen M, Kazdin AE, editors. International handbook of behavior modification and therapy. Vol. 2. New York: Plenum Press; 1992. pp. 449–473. [Google Scholar]
- Wadden TA, Brownell KD, Foster GD. Obesity: Responding to the global epidemic. J Consult Clin Psychol. 2002;70(3):510–525. doi: 10.1037//0022-006x.70.3.510. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinol Metab Clin North Am. 2003;32(4):981–1003. doi: 10.1016/s0889-8529(03)00072-0. x. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Crerand CE, Brock J. Behavioral treatment of obesity. Psychiatr Clin North Am. 2005;28(1):151–170. doi: 10.1016/j.psc.2004.09.008. ix. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Frey DL. A multicenter evaluation of a proprietary weight loss program for the treatment of marked obesity: A five-year follow-up. Int J Eat Disord. 1997;22(2):203–212. doi: 10.1002/(sici)1098-108x(199709)22:2<203::aid-eat13>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Sternberg JA, Letizia KA, Stunkard AJ, Foster GD. Treatment of obesity by very low calorie diet, behavior therapy, and their combination: A five-year perspective. Int J Obes. 1989;13(Suppl 2):39–46. [PubMed] [Google Scholar]
- Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annual review of nutrition. 2004;24:455–479. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- Wansink B. Mindless eating: Why we eat more than we think. New York: Bantam; 2006. [Google Scholar]
- Ward A, Mann T. Don't mind if i do: Disinhibited eating under cognitive load. Journal of personality and social psychology. 2000;78(4):753. doi: 10.1037//0022-3514.78.4.753. [DOI] [PubMed] [Google Scholar]
- Weinsier RL, Hunter GR, Desmond RA, Byrne NM, Zuckerman PA, Darnell BE. Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight. The American journal of clinical nutrition. 2002;75(3):499–504. doi: 10.1093/ajcn/75.3.499. [DOI] [PubMed] [Google Scholar]
- Weinsier RL, Nagy TR, Hunter GR, Darnell BE, Hensrud DD, Weiss HL. Do adaptive changes in metabolic rate favor weight regain in weight-reduced individuals? An examination of the set-point theory. The American journal of clinical nutrition. 2000;72(5):1088–1094. doi: 10.1093/ajcn/72.5.1088. [DOI] [PubMed] [Google Scholar]
- Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70(1):115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- Wilson KG. Behavioral treatment of obesity: Thirty years and counting. Advances in Behaviour Research & Therapy. 1994;16(1):31–75. [Google Scholar]
- Wilson KG, Murrell AR. Values work in acceptance and commitment therapy: Setting a course for behavioral treatment. In: Hayes SC, Follette VM, Linehan M, editors. Mindfulness & acceptance: Expanding the cognitive-behavioral tradition. New York: Guilford Press; 2004. pp. 120–151. [Google Scholar]
- Wilson TD, Lindsey S, Schooler TY. A model of dual attitudes. Psychol Rev. 2000;107:101–126. doi: 10.1037/0033-295x.107.1.101. [DOI] [PubMed] [Google Scholar]
- Woods DW, Wetterneck CT, Flessner CA. A controlled evaluation of acceptance and commitment therapy plus habit reversal for trichotillomania. Behav Res Ther. 2006;44(5):639–656. doi: 10.1016/j.brat.2005.05.006. [DOI] [PubMed] [Google Scholar]
- Woollard J, Beilin L, Lord T, Puddey I, MacAdam D, Rouse I. A controlled trial of nurse counseling on lifestyle change for hypertensives treated in general practice: Preliminary results. Clin Exl Pharmacol Physiol. 1995;22:466–468. doi: 10.1111/j.1440-1681.1995.tb02046.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Cardiovascular disease: Prevention and control. 2010 Retrieved January 31, 2010, 2010, from http://www.who.int/dietphysicalactivity/publications/facts/cvd/en/
- Yanovski SZ, Yanovski JA. Obesity. N Engl J Med. 2002;346(8):591–602. doi: 10.1056/NEJMra012586. [DOI] [PubMed] [Google Scholar]
- Zettle RD, Hayes SC. Component and process analysis of cognitive therapy. Psychol Rep. 1987;61(3):939–953. doi: 10.2466/pr0.1987.61.3.939. [DOI] [PubMed] [Google Scholar]


