Abstract
IMPORTANCE
Thousands of physicians attend scientific meetings annually. Although hospital physician staffing and composition may be affected by meetings, patient outcomes and treatment patterns during meeting dates are unknown.
OBJECTIVE
To analyze mortality and treatment differences among patients admitted with acute cardiovascular conditions during dates of national cardiology meetings compared with nonmeeting dates.
DESIGN, SETTING, AND PARTICIPANTS
Retrospective analysis of 30-day mortality among Medicare beneficiaries hospitalized with acute myocardial infarction (AMI), heart failure, or cardiac arrest from 2002 through 2011 during dates of 2 national cardiology meetings compared with identical nonmeeting days in the 3 weeks before and after conferences (AMI, 8570 hospitalizations during 82 meeting days and 57 471 during 492 nonmeeting days; heart failure, 19 282 during meeting days and 11 4591 during nonmeeting days; cardiac arrest, 1564 during meeting days and 9580 during nonmeeting days). Multivariable analyses were conducted separately for major teaching hospitals and nonteaching hospitals and for low-and high-risk patients. Differences in treatment utilization were assessed.
EXPOSURES
Hospitalization during cardiology meeting dates.
MAIN OUTCOMES AND MEASURES
Thirty-day mortality, procedure rates, charges, length of stay.
RESULTS
Patient characteristics were similar between meeting and nonmeeting dates. In teaching hospitals, adjusted 30-day mortality was lower among high-risk patients with heart failure or cardiac arrest admitted during meeting vs nonmeeting dates (heart failure, 17.5% [95% CI, 13.7%–21.2%] vs 24.8% [95% CI, 22.9%–26.6%]; P < .001; cardiac arrest, 59.1% [95% CI, 51.4%–66.8%] vs 69.4% [95% CI, 66.2%–72.6%]; P = .01). Adjusted mortality for high-risk AMI in teaching hospitals was similar between meeting and nonmeeting dates (39.2% [95% CI, 31.8%–46.6%] vs 38.5% [95% CI, 35.0%–42.0%]; P = .86), although adjusted percutaneous coronary intervention (PCI) rates were lower during meetings (20.8% vs 28.2%; P = .02). No mortality or utilization differences existed for low-risk patients in teaching hospitals or high- or low-risk patients in nonteaching hospitals. In sensitivity analyses, cardiac mortality was not affected by hospitalization during oncology, gastroenterology, and orthopedics meetings, nor was gastrointestinal hemorrhage or hip fracture mortality affected by hospitalization during cardiology meetings.
CONCLUSIONS AND RELEVANCE
High-risk patients with heart failure and cardiac arrest hospitalized in teaching hospitals had lower 30-day mortality when admitted during dates of national cardiology meetings. High-risk patients with AMI admitted to teaching hospitals during meetings were less likely to receive PCI, without any mortality effect.
Each year, thousands of physicians attend national scientific meetings. In 2006, for example, nearly 19 000 cardiologists and other health care professionals attended the American Heart Association (AHA) annual meeting,1 with numbers declining to approximately 16 000 and 13 000 by 2009 and 2013, respectively.2 A similar number of cardiologists and other professionals attend the American College of Cardiology (ACC) annual meetings.3 During conferences, physician staffing in hospitals may be lower than on nonmeeting dates, and the composition of physicians who remain to treat patients—rather than those who attend the meetings—may be different. These factors may affect treatment practices and outcomes for hospitalized patients.
Hospitalized patient outcomes during dates of scientific meetings are unknown but of interest, considering that adverse patient outcomes and delays in care have been associated with reducing staffing during off-hour and weekend hospitalizations.4–9 In contrast to these studies, however, comparisons of patient outcomes during dates of scientific meetings vs identical days in surrounding weeks may be more likely to isolate the effect of declines in physician staffing rather than the composite effect of declines in overall staffing (eg, nurses and other clinicians) that also occur on weekends and off-hours. Aside from differences in staffing levels, differences in the composition of physicians who remain to treat hospitalized patients during scientific meeting dates may also influence outcomes and treatment utilization.
We investigated differences in 30-day mortality among all Medicare fee-for-service beneficiaries who were hospitalized with acute myocardial infarction (AMI), heart failure, or cardiac arrest from 2002 to 2011 during the dates of 2 national cardiology meetings compared with identical nonmeeting days before and after conferences. We focused on conditions that are acute in nature rather than elective, to minimize the possibility that patients delayed care until after the meetings. We examined mortality differences separately for patients admitted to teaching and nonteaching hospitals and for low- and high-risk patients. We investigated whether rates of specific treatments (eg, percutaneous coronary intervention [PCI] and mechanical circulatory support), length of stay (LOS), and hospital charges varied between meeting and nonmeeting dates. We hypothesized that mortality would be higher and treatment utilization lower during cardiology meeting dates. We hypothesized that differences in outcomes would be largest in teaching hospitals, where a disproportionately larger fraction of cardiologists may attend cardiology meetings.
Methods
Data Sources
We used the Medicare Provider Analysis Review 20% files to identify hospitalizations from January 1, 2002, through November 31, 2011, with a primary diagnosis of AMI, heart failure, or cardiac arrest among Medicare fee-for-service beneficiaries 65 years or older. Patients with AMI and heart failure were identified according to International Classification of Diseases, Ninth Revision (ICD-9) criteria in the Agency for Health Care Research and Quality (AHRQ) Inpatient Quality Indicators,10 while patients with cardiac arrest were identified by ICD-9 primary diagnosis code 427.5. December 2011 discharges were excluded to allow 30-day postadmission follow-up. We used American Hospital Association annual surveys to identify major teaching hospitals based on a ratio of resident physicians per bed of greater than 0.60.11–13 The study was exempt from human subjects review at the University of Southern California.
Study Sample
Calendar dates for scientific sessions at 2 national cardiology meetings—the AHA and ACC annual meetings—were obtained for each year from 2002 to 2011. We identified all hospitalizations for AMI, heart failure, or cardiac arrest for which the admission dates were during the dates of these meetings (exposure group), as well as all admissions during identical days in the 3 weeks before and after the meetings (control group). For example, for the 2005 ACC meetings held Sunday, March 6, to Wednesday, March 9, the control group consisted of patients admitted Sunday through Wednesday in the 3weeks before and after the meetings. Our final sample for all hospitals consisted of 8570 AMI hospitalizations during meeting dates and 57 471 hospitalizations during nonmeeting dates; 19 282 heart failure hospitalizations during meetings and 11 4591 during nonmeeting dates; and 1564 cardiac arrest hospitalizations during meetings and 9580 during nonmeeting dates. To assess whether hospitalizations for other cardiovascular conditions declined during meeting dates, we also examined the distribution between meeting and nonmeeting dates of total cardiovascular hospitalizations excluding AMI, heart failure, and cardiac arrest, identified according to AHRQ clinical classification codes 96 to 108.
Outcome Measures
Our primary outcome was risk-adjusted all-cause 30-day mortality after admission for AMI, heart failure, or cardiac arrest among patients admitted during meeting vs nonmeeting dates. Because outcomes and treatment patterns during meeting and nonmeeting dates may be different for patients at low vs high predicted risk of inpatient mortality, we used a validated AHRQ risk adjustment tool to identify low- vs high-risk patients with AMI or heart failure.10 Patients with cardiac arrest were defined as high-risk.14 The AHRQ tool includes risk parameters for patient age, race, sex, and relevant diagnosis codes that have been estimated from national AMI and heart failure hospital discharge data. These preestimated risk coefficients can be applied to other claims-based data to predict patient-level inpatient mortality. Based on existing studies, a priori, we defined patients dichotomously to be at high risk after AMI or heart failure if their predicted mortality was in the top quartile for the respective disease and at low risk if their predicted mortality was in the bottom 3 quartiles.13,15 We conducted sensitivity analysis around these risk categorizations.
We also examined whether specific treatment rates varied between meeting and nonmeeting dates. For AMI, we estimated rates of PCI (ICD-9 procedure codes 00.66, 36.01, 36.02, 36.05, 36.06, 36.07, 36.09),16 mechanical circulatory support (defined as intra-aortic balloon pump counterpulsation, code 37.61, or percutaneous ventricular assist device, codes 37.60, 37.62, 37.65, 37.66, 37.68), and coronary artery bypass grafting (CABG) (codes 36.10–36.19). For heart failure, we estimated rates of diagnostic catheterization of the right side of the heart or invasive hemodynamic monitoring with tailored therapy (codes 37.21, 89.63, 89.64, 89.66-68) and CABG.17 For cardiac arrest, we estimated rates of PCI and CABG. For all conditions, we investigated whether LOS and hospital charges varied between meeting and nonmeeting dates.
Statistical Analysis
We first compared patient characteristics between meeting and nonmeeting dates, including patient age, sex, race, chronic comorbidities recorded in medical claims prior to the admission, and mortality predicted by the AHRQ tool. We accounted for correlation in characteristics across patients within hospitals by clustering standard errors at the hospital level. We also compared unadjusted 30-day mortality among low- and high-risk patients admitted with AMI or heart failure and patients admitted with cardiac arrest during meeting vs nonmeeting dates, again clustering standard errors at the hospital level. We then estimated a patient-level multivariable logistic model with hospital random effects that adjusted for the patient characteristics listed herein; for each disease, we reported adjusted 30-day mortality among patients admitted during meeting and nonmeeting dates. We conducted analyses separately for major teaching hospitals and nonteaching hospitals, since a larger proportion of cardiologists in major teaching hospitals may attend national cardiology meetings compared with nonteaching hospitals. For example, among attendees surveyed during the 2014 ACC meetings, approximately 41% reported a primary activity including medical research or medical teaching.18
We also examined whether specific treatment rates, LOS, and hospital charges varied among low- and high-risk patients admitted during meeting and nonmeeting dates. For each treatment and condition, we estimated multivariable logistic random-effects models with the same covariates as our mortality models. For LOS and hospital charges, both of which are continuous variables, we estimated multivariable linear regression models. We reported adjusted treatment rates, LOS, and hospital charges among patients admitted during meeting and nonmeeting dates.
The 95% confidence intervals around reported means reflects 0.025 in each tail. In all regression models, standard errors were clustered at the hospital level.
Sensitivity Analyses
We performed several sensitivity analyses. To assess for confounding in 30-day mortality among patients hospitalized during meeting vs nonmeeting dates, we conducted a set of falsification analyses.19–21 First, we examined whether 30-day mortality differences were present among patients admitted during dates of national gastroenterology (Digestive Disease Week), oncology (American Society of Clinical Oncology), and orthopedic (American Association of Orthopedic Surgery) meetings vs nonmeeting dates. We also examined whether differences in 30-day mortality after hospitalization for hip fracture or gastrointestinal tract hemorrhage existed among patients with these conditions admitted during meeting vs nonmeeting dates; hospitalizations were identified according to ICD-9 criteria in the AHRQ inpatient quality indicators.10 In either analysis, associations between 30-day mortality and hospitalization during meeting dates would suggest unmeasured confounding. Second, we considered alternative definitions of our control group (2 or 4 weeks surrounding meeting dates rather than 3 weeks) and alternative definitions of high risk (top tercile or quintile in AMI or heart failure rather than top quartile of predicted mortality). Third, we estimated models with hospital fixed effects to examine whether our results were driven by patients preferentially being admitted to specific hospitals during meeting vs nonmeeting dates (eg, hospitals of higher quality during meeting dates). Fourth, we considered 90-day mortality to explore longer-term effects. Fifth, we controlled for the hospital’s US Census Bureau division and size (number of medical and surgical adult beds from American Hospital Association surveys) in our analyses. Finally, we considered alternative model specifications (generalized linear model with log-link Poisson) for analyses of hospital charges and LOS, to better reflect skewness in these variables.
Results
Patient Characteristics During Meeting and Nonmeeting Dates
Between meeting and nonmeeting dates, patients in the overall sample had similar demographic characteristics and existing medical conditions (Table 1). Patients with AMI and heart failure admitted on meeting vs nonmeeting dates also had comparable predicted inpatient mortality based on the AHRQ risk tool (AMI, 11.8% vs 11.6%; P = .08; heart failure, 5.0% vs 5.0%; P = .28). Patient characteristics were also similar between meeting and nonmeeting dates for high-risk patients admitted to teaching hospitals (eTable 1 in the Supplement) and nonteaching hospitals (eTable 2 in the Supplement) and for low-risk patients admitted to teaching hospitals (eTable 3 in the Supplement) and nonteaching hospitals (eTable 4 in the Supplement).
Table 1.
Characteristics of Patients Hospitalized With Acute Myocardial Infarction, Heart Failure, or Cardiac Arrest During Dates of 2 National Cardiology Meetingsa
| Characteristics of Patient Sample |
Acute Myocardial Infarction | Heart Failure | Cardiac Arrest | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Meeting Dates |
Nonmeeting Dates |
P Value | Meeting Dates |
Nonmeeting Dates |
P Value | Meeting Dates |
Nonmeeting Dates |
P Value | |
| Patients, No. | 8570 | 51 471 | 19 282 | 114 591 | 1564 | 9580 | |||
| Mean age, y | 78.7 | 78.8 | .52 | 80.1 | 80.0 | .33 | 78.3 | 78.4 | .62 |
| Male | 50.7 | 50.1 | .22 | 43.2 | 42.9 | .41 | 49.5 | 49.8 | .83 |
| Race | |||||||||
| White | 87.5 | 86.7 | .04 | 81.1 | 81.2 | .82 | 81.1 | 80.4 | .53 |
| Black | 8.3 | 8.8 | .12 | 14.3 | 14.3 | .87 | 14.1 | 14.1 | .99 |
| Hispanic | 1.6 | 1.7 | .41 | 2.2 | 2.1 | .49 | 1.6 | 2.0 | .20 |
| Asian or Pacific Islander | 0.8 | 1.0 | .18 | 0.9 | 0.8 | .64 | 1.5 | 1.4 | .66 |
| Other | 1.9 | 1.9 | .76 | 1.5 | 1.6 | .39 | 1.7 | 2.0 | .34 |
| Preexisting comorbidities | |||||||||
| Ischemic heart disease | 68.9 | 68.8 | .88 | 83.3 | 83.5 | .52 | 66.8 | 69.4 | .04 |
| Dementia | 17.8 | 18.4 | .20 | 22.6 | 22.9 | .41 | 25.2 | 24.4 | .47 |
| Atrial fibrillation | 19.7 | 18.6 | .01 | 45.0 | 44.8 | .61 | 28.9 | 28.5 | .73 |
| Chronic kidney disease | 27.3 | 27.4 | .91 | 48.4 | 48.7 | .39 | 34.5 | 37.3 | .03 |
| Diabetes mellitus | 42.8 | 42.7 | .94 | 55.2 | 55.4 | .62 | 45.1 | 46.7 | .25 |
| COPD | 32.9 | 33.2 | .68 | 52.4 | 52.9 | .19 | 42.3 | 43.7 | .31 |
| Heart failure | 47.5 | 47.4 | .93 | 84.0 | 84.2 | .51 | 58.5 | 59.8 | .35 |
| Hyperlipidemia | 64.3 | 64.9 | .26 | 70.7 | 70.6 | .75 | 60.4 | 62.3 | .15 |
| Hypertension | 79.8 | 80.4 | .22 | 90.9 | 90.9 | .91 | 82.9 | 84.5 | .14 |
| Cancer | 14.5 | 14.8 | .59 | 16.5 | 16.9 | .16 | 17.1 | 18.2 | .27 |
| Hospitalized at a teaching hospital | 10.4 | 10.4 | .89 | 9.3 | 9.2 | .65 | 10.6 | 10.2 | .57 |
| AHRQ predicted mortality, mean | 11.8 | 11.6 | .08 | 5.0 | 5.0 | .28 | NA | NA | NA |
Abbreviations: AHRQ, Agency for Health Care Research and Quality; COPD, chronic obstructive pulmonary disease; NA, not applicable.
Data are given as percentages except where noted.
For each condition, hospitalizations were evenly distributed between meeting and nonmeeting dates, suggesting that hospitalizations were not simply delayed until after meetings (eTable 5 in the Supplement). For example, because the control group was defined as patients admitted during identical days in the 3-week periods before and after meeting dates, an even distribution between meeting and nonmeeting dates would imply a ratio of hospitalizations of approximately 1:6. In the full sample, the ratio of hospitalizations between meeting and nonmeeting dates was 1:6.0 for AMI, 1:6.0 for heart failure, and 1:6.1 for cardiac arrest. Similar ratios were observed for both low- and high-risk patients in teaching and nonteaching hospitals (eTable 5 in the Supplement). Overall cardiovascular hospitalizations were also evenly distributed evenly between meeting and nonmeeting dates, suggesting no decline in less urgent hospitalizations during meeting dates (eTable 5 in the Supplement).
Mortality During Meeting and Nonmeeting Dates
Unadjusted 30-day mortality was lower among patients with high-risk heart failure or cardiac arrest admitted to major teaching hospitals during meeting vs nonmeeting dates (Table 2). For example, in teaching hospitals, of 388 high-risk patients admitted with heart failure during meeting dates, 66 (17.0%) died within 30 days compared with 535 of 2154 (24.8%) admitted on nonmeeting dates (P < .001). Similarly, 98 of 166 patients (59.0%) admitted to teaching hospitals with cardiac arrest during meeting dates died within 30 days compared with 669 of 975 (68.6%) on nonmeeting dates (P = .02). Unadjusted mortality among high-risk patients with AMI admitted to teaching hospitals was similar on meeting and nonmeeting dates (40.4% vs 38.2%;P = .54). There was no difference in mortality among low-risk patients with AMI or heart failure admitted to teaching hospitals during meeting vs nonmeeting dates.
Table 2.
Unadjusted 30-Day Mortality Among Patients Admitted for Acute Myocardial Infarction, Heart Failure, or Cardiac Arrest During Dates of 2 National Cardiology Meetings
| Conditions | Predicted Mortality Risk | |||||
|---|---|---|---|---|---|---|
| Low | High | |||||
| Meeting Dates | Nonmeeting Dates | P Value | Meeting Dates | Nonmeeting Dates | P Value | |
| Teaching Hospitals | ||||||
| Acute myocardial infarction | ||||||
| Patients, No. | 710 | 4359 | .36 | 178 | 1001 | .54 |
| 30-d mortality, No. (%) | 55 (7.7) | 385 (8.8) | 72 (40.4) | 382 (38.2) | ||
| Heart failure | ||||||
| Patients, No. | 1410 | 8415 | .82 | 388 | 2154 | <.001 |
| 30-d Mortality, No. (%) | 71 (5.0) | 435 (5.2) | 66 (17.0) | 535 (24.8) | ||
| Cardiac arrest | ||||||
| Patients, No. | NA | NA | NA | 166 | 975 | .02 |
| 30-d Mortality, No. (%) | NA | NA | 98 (59.0) | 669 (68.6) | ||
| Nonteaching Hospitals | ||||||
| Acute myocardial infarction | ||||||
| Patients, No. | 6311 | 38 291 | .06 | 1371 | 7820 | .15 |
| 30-d Mortality, No. (%) | 659 (10.4) | 4298 (11.2) | 587 (42.8) | 3181 (40.7) | ||
| Heart failure | ||||||
| Patients, No. | 13 775 | 81 968 | .02 | 3709 | 22 054 | .66 |
| 30-d Mortality, No. (%) | 1045 (7.6) | 5738 (7.0) | 901 (24.3) | 5432 (24.6) | ||
| Cardiac arrest | ||||||
| Patients, No. | NA | NA | NA | 1398 | 8605 | .14 |
| 30-d Mortality, No. (%) | NA | NA | 980 (70.1) | 6197 (72.0) | ||
Abbreviation: NA, not applicable.
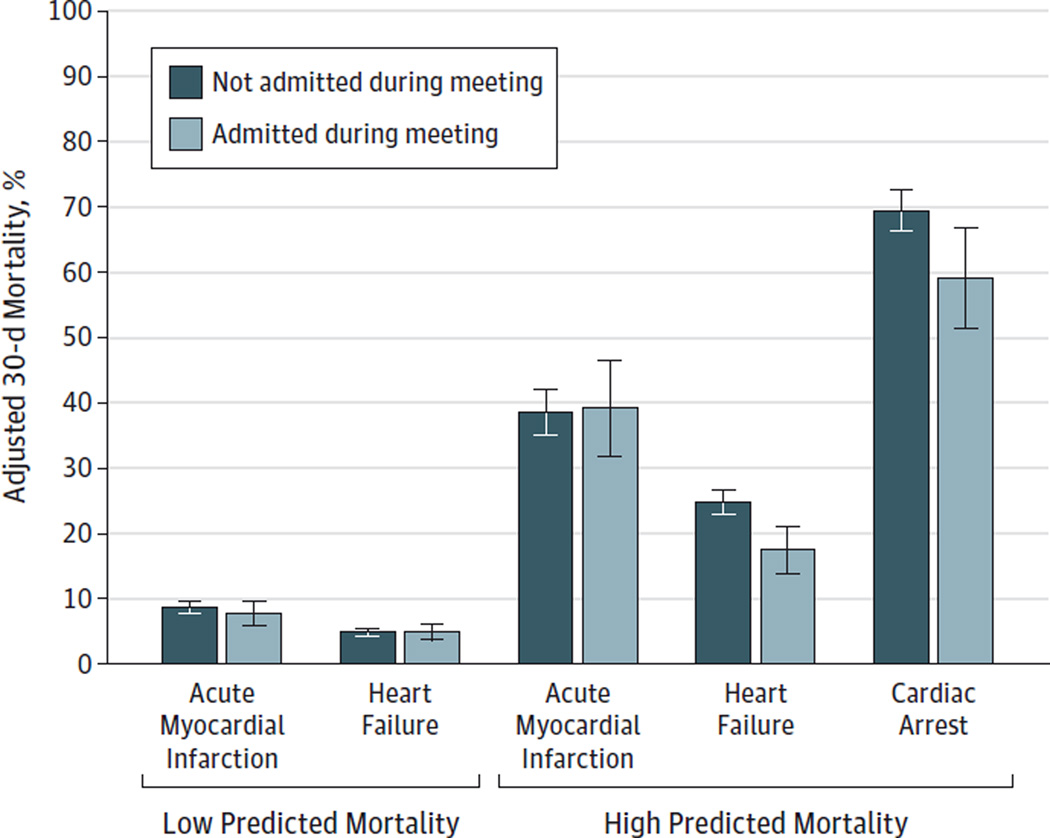
After covariate adjustment, 30-day mortality was lower among high-risk patients with heart failure or cardiac arrest admitted to teaching hospitals during meeting vs nonmeeting dates (heart failure, 17.5% [95% CI, 13.7%–21.2%] vs 24.8% [95% CI, 22.9%–26.6%]; P < .001; cardiac arrest, 59.1% [95% CI, 51.4%–66.8%] vs 69.4% [95% CI, 66.2%–72.6%]; P = .01) (Figure and eTable 6 in the Supplement). Adjusted mortality among high-risk patients with AMI admitted to teaching hospitals was similar between meeting and nonmeeting dates (39.2% [95% CI, 31.8%–46.6%] vs 38.5% [95% CI, 35.0%–42.0%]; P = .86).
Figure.
Adjusted 30-Day Mortality Among Patients Admitted to Teaching Hospitals With Acute Myocardial Infarction, Heart Failure, or Cardiac Arrest During Dates of 2 National Cardiology Meetings
Error bars indicate 95%CIs.
Adjusted mortality did not differ between meeting and nonmeeting dates for low-risk patients in teaching hospitals (eTable 6 in the Supplement). For example, among low-risk patients with heart failure in teaching hospitals, adjusted mortality during meeting and nonmeeting dates was 4.9% (95% CI, 3.7%–6.1%) and 4.9% (95% CI, 4.4%–5.5%), respectively (P = .93). Adjusted mortality also generally did not differ between meeting and nonmeeting dates for low- or high-risk patients in nonteaching hospitals (eTable 6 in the Supplement). For example, adjusted mortality for high-risk patients with heart failure during meeting and nonmeeting dates was 24.6% (95% CI, 23.2%–26.0%) and 24.5% (95% CI, 24.0%–25.1%), respectively (P = .91).
Treatment Utilization Among High-Risk Patients Admitted to Teaching Hospitals During Meeting Dates
Among high-risk patients with AMI admitted to teaching hospitals, adjusted PCI rates were significantly lower during meeting vs nonmeeting dates (20.8% [95% CI, 15.3%–26.3%] vs 28.2% [95% CI, 25.5%–30.8%]; P = .02; Table 3), while adjusted rates of mechanical circulatory support, CABG, LOS, and hospital charges did not vary. Among high-risk patients with heart failure admitted to teaching hospitals, adjusted rates of diagnostic catheterization of the right side of the heart or invasive hemodynamic monitoring with tailored therapy were generally low and did not vary between meeting and nonmeeting dates (2.2% [95% CI,0.8%–3.7%] vs 2.7% [95% CI, 1.8%–3.6%];P = .54), nor did LOS (8.2 vs 8.5 days; P = .43) or hospital charges ($50 779 vs $55 685; P = .17). Among patients with cardiac arrest admitted to teaching hospitals, adjusted rates of PCI, CABG, hospital charges, and LOS did not differ between meeting and nonmeeting dates.
Table 3.
Treatment Utilization Among High-Risk Patients Admitted to Teaching Hospitals for Acute Myocardial Infarction, Heart Failure, or Cardiac Arrest During Dates of 2 National Cardiology Meetings
| Condition and Treatment Utilization |
Adjusted (95% CI) | P Value | |
|---|---|---|---|
| Meeting Dates | Nonmeeting Dates | ||
| Acute Myocardial Infarction | |||
| PCI, % | 20.8 (15.3 to 26.3) | 28.2 (25.5 to 30.8) | .02 |
| Circulatory support, %a | 20.3 (14.5 to 26.1) | 20.1 (17.3 to 22.8) | .93 |
| CABG, % | 11.3 (7.9 to 14.7) | 8.6 (7.5 to 9.8) | .12 |
| Hospital charges, $ | 92 611 (76 165 to 109 058) | 88 562 (79 945 to 97 178) | .63 |
| Length of stay, d | 9.5 (8.1 to 10.9) | 9.3 (8.8 to 9.8) | .77 |
| Heart Failure | |||
| Catheterization or monitoring, %b | 2.2 (0.8 to 3.7) | 2.7 (1.8 to 3.6) | .54 |
| CABG, % | 1.1 (−0.5 to 2.8) | 0.6 (−0.1 to 1.2) | .32 |
| Hospital charges, $ | 50 779 (42 329 to 59 228) | 55 685 (49 011 to 62 358) | .17 |
| Adjusted length of stay, d | 8.2 (7.5 to 8.9) | 8.5 (8.0 to 8.9) | .43 |
| Cardiac Arrest | |||
| PCI, % | 6.5 (2.7 to 10.4) | 5.9 (3.8 to 8.0) | .75 |
| CABG, % | 3.1 (0.4 to 5.8) | 2.3 (1.0 to 3.6) | .50 |
| Hospital charges, $ | 112 716 (84 313 to 141 119) | 86 322 (76 858 to 95 787) | .07 |
| Length of stay, d | 11.7 (9.2 to 14.3) | 9.3 (8.3 to 10.3) | .07 |
Abbreviations: CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention.
Includes intra-aortic balloon pump counterpulsation or peripherally inserted ventricular assist device.
Diagnostic catheterization of the right side of the heart or invasive hemodynamic monitoring with tailored therapy.
Sensitivity Analysis
We found no evidence that unmeasured confounding explained lower mortality among high-risk patients with heart failure or cardiac arrest during meeting vs nonmeeting dates. Adjusted mortality rates among high-risk patients admitted to teaching hospitals with AMI, heart failure, or cardiac arrest were similar between national oncology, gastroenterology, and orthopedic meeting dates and identical days in weeks before and after conferences (Table 4). Similarly, adjusted mortality among patients admitted with gastrointestinal tract hemorrhage or hip fracture was similar between cardiology meeting dates and noncardiology meeting dates (eTable 7 in the Supplement). Our findings were also unaffected by alternative definitions of our control group (eTable 8 in the Supplement); alternative definitions of high risk (eTable 9 in the Supplement); the inclusion of hospital fixed effects to assess whether our results were driven by patients being preferentially admitted to higher-quality hospitals during meeting dates (eTable 10 in the Supplement); the inclusion of hospital size and US Census division (eTable 11 in the Supplement); and alternative model specifications of the hospital charge and LOS analyses (generalized linear model with log-link). The significant 30-day mortality differentials among high-risk patients treated in teaching hospitals were slightly smaller in magnitude at 90 days and trended toward significance (eTable 12 in the Supplement).
Table 4.
Adjusted 30-Day Mortality Among Patients Admitted to Teaching Hospitals for Acute Myocardial Infarction, Heart Failure, or Cardiac Arrest During Dates of National Oncology, Gastroenterology, and Orthopedic Surgery Meetings
| Condition | Predicted Mortality Risk | |||||
|---|---|---|---|---|---|---|
| Low | High | |||||
| Meeting Dates | Nonmeeting Dates | P Value | Dates | Nonmeeting Dates | P Value | |
| Acute myocardial infarction | ||||||
| Patients, No. | 1258 | 7272 | .70 | 289 | 1581 | .29 |
| Adjusted 30-d mortality, % (95% CI) | 7.8 (6.3–9.3) | 8.1 (7.5–8.8) | 40.9 (35.0–46.7) | 37.6 (34.7–40.4) | ||
| Heart failure | ||||||
| Patients, No. | 2604 | 14 286 | .39 | 595 | 3531 | .44 |
| Adjusted 30-d mortality, % (95% CI) | 5.1 (4.2–6.0) | 5.5 (5.1–6.0) | 24.8 (21.3–28.3) | 23.4 (21.9–24.9) | ||
| Cardiac arrest | ||||||
| Patients, No. | NA | NA | NA | 315 | 1644 | .61 |
| Adjusted 30-d mortality, % (95% CI) | NA | NA | 68.1 (62.5–73.6) | 69.5 (66.6–72.4) | ||
Abbreviation: NA, not applicable.
Discussion
We found substantially lower adjusted 30-day mortality among high-risk patients with heart failure or cardiac arrest admitted to major teaching hospitals during dates of national cardiology meetings. The PCI rates among high-risk patients with AMI admitted to major teaching hospitals were significantly lower during meetings, without any decrement to survival. We found no differences in mortality between meeting and nonmeeting dates for low-risk patients in teaching hospitals or for high- or low-risk patients in nonteaching hospitals.
Our mortality results for high-risk patients in teaching hospitals are unlikely to be explained by patients delaying care until after cardiology meetings, both because patients were observationally similar between meeting and nonmeeting dates and because hospitalizations for AMI, heart failure, and cardiac arrest were evenly distributed between meeting and nonmeeting dates. Moreover, we found no effect of gastroenterology, oncology, and orthopaedics meetings on cardiac mortality, nor did we find an effect of cardiology meetings on gastrointestinal tract hemorrhage or hip fracture mortality; both findings argue against unmeasured confounding.
Several explanations of our findings are possible. First, selective declines in cardiologist staffing, combined with changes in the composition of physicians who remain to treat hospitalized patients, may partly account for different outcomes. Cardiologists who remain at home while a conference is under way may be different than those who attend meetings. This factor may be particularly relevant at major teaching hospitals where a greater proportion of cardiologists may attend national meetings, and a specific rotation of physicians may provide coverage back home. If diagnostic and procedural capabilities of these physicians differ, physician compositional changes during meetings may result in differences in patient outcomes and treatment patterns.
Second, declines in intensity of care during meetings—driven either by changes in physician composition and practice styles, reluctance to perform interventions in patients whose primary cardiologist is unavailable, or reluctance of cardiologists to intervene in high-risk patients without adequate back-up—may produce mortality reductions among high-risk patients with cardiovascular disease if the usual interventions performed on these patients on nonmeeting dates are actually unnecessary. Interventions foregone during meeting dates are more likely to be those for which the risk-benefit tradeoff is less clear and may involve harms that outweigh benefits in high-risk patients. Our finding that substantially lower PCI rates for high-risk patients with AMI admitted to teaching hospitals during cardiology meetings are not associated with improved survival suggests potential overuse of PCI in this population. This interpretation is consistent with evidence that public reporting of PCI outcomes is associated with lower rates of PCI among high-risk patients with AMI, without any effect on mortality.16 More broadly, this interpretation may align with other studies of medical care which demonstrate that “less is more” for intensive care patients (eg, conservative transfusion thresholds for hospitalized patients with ischemic heart disease and anemia,22 conservative [rather than intensive] glucose regulation in patients with hyperglycemia with acute coronary syndrome treated with PCI,23 and abstinence from use of high-dose systemic corticosteroids in septic shock24).
Third, declines in the volume of less urgent cardiovascular hospitalizations during meeting dates could allow physicians to focus greater attention on remaining high-risk patients, thereby improving outcomes. Although we found no evidence that total cardiovascular hospitalization volume declined during meeting dates, it is possible that rates of same-day elective procedures and outpatient visits may have declined, which could have the same positive effect on patient outcomes. To our knowledge, no studies exist on the association between daily patient workload and mortality among patients with cardiovascular disease, although in obstetrics, higher-than-predicted daily hospital birth volume has been associated with greater rates of neonatal asphyxia,25 and in neonatal intensive care, infants admitted to neonatal intensive care units on full- vs half-capacity days have greater mortality.26 Although all 3 explanations we provide are possible, our data cannot definitively distinguish among these possibilities.
Our findings may seem to conflict with our a priori hypothesis and studies that demonstrate worse patient outcomes during off-hours.4–9 However, because we specifically compared hospitalizations during cardiology meeting dates with identical days in the surrounding weeks, our analysis explored the effect of selective reductions in cardiologist and not ancillary staffing as well as the effect of changes in the specific composition of cardiologists treating patients. Our results echo paradoxical findings documented during a labor strike by Israeli physicians in 2000, in which hundreds of thousands of outpatient visits and elective surgical procedures were cancelled, but by many accounts mortality rates dramatically fell during the year.27 Similar reports of decreased mortality during physician labor strikes exist elsewhere, with most hypotheses attributing mortality declines to lower rates of non-urgent surgical procedures.28
The principal limitation of our study was an inability to establish the mechanism by which high-risk patients with heart failure and cardiac arrest experienced lower 30-day mortality when admitted during dates of cardiology meetings. For example, among high-risk patients with heart failure, we found no difference between meeting and nonmeeting dates in adjusted rates of diagnostic catheterization of the right side of the heart or invasive hemodynamic monitoring, CABG, hospital charges, or LOS. Among patients with cardiac arrest, we found no differences in adjusted PCI or CABG rates, hospital charges, or LOS. Although important, each of these measures may miss important clinical decisions that do not appear in administrative data (eg, administration of vasoactive and inotropic medications29,30 or nonbilled diagnostic and therapeutic procedures). We did, however, identify lower PCI rates among high-risk patients with AMI admitted to teaching hospitals during meeting dates, which may suggest lower intensity of care during these dates. We could also not directly assess how the staffing and composition of cardiologists who treated patients differed between meeting and nonmeeting dates. An additional limitation is that unmeasured confounders may explain mortality reductions during cardiology meeting dates. For example, cancellation of outpatient cardiology clinics or the absence of a given patient’s cardiologist may lead to delays in care that create a sample of inpatients that are at higher risk of mortality. However, not only were patients nearly identical between meeting and nonmeeting dates with respect to age, sex, race, and 10 chronic comorbidities, but we also found no evidence that hospitalizations were delayed until after the meetings ended. Moreover, our sensitivity analyses argue against unmeasured confounding. Our analysis was also restricted to the Medicare population and may not generalize to the commercially insured. Finally, the mortality effects we found among high-risk patients treated at teaching hospitals were unaffected by applying a Bonferroni correction for the comparison of multiple outcomes for each condition.31
Conclusions
We observed lower 30-day mortality among patients with high-risk heart failure or cardiac arrest admitted to major teaching hospitals during the dates of 2 national cardiology meetings, as well as substantially lower PCI rates among high-risk patients with AMI, without any detriment to survival. One explanation for these findings is that the intensity of care provided during meeting dates is lower and that for high-risk patients with cardiovascular disease, the harms of this care may unexpectedly outweigh the benefits.
Supplementary Material
Acknowledgments
Funding/Support: Dr Jena has received funding from the Office of the Director, National Institutes of Health (NIH Early Independence Award, grant 1DP5OD017897-01). Drs Goldman and Romley have received funding from the National Institute of Aging (grant 5P01AG033559).
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Supplemental content at jamainternalmedicine.com
Author Contributions: Dr Jena had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Jena, Prasad, Romley.
Acquisition, analysis, or interpretation of data: Jena, Goldman, Romley.
Drafting of the manuscript: Jena, Prasad.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Jena, Romley.
Obtained funding: Jena, Goldman.
Study supervision: Jena, Goldman.
Conflict of Interest Disclosures: Dr Goldman is a partner at Precision Health Economics, a health care consultancy conducting research in the life sciences. No other disclosures are reported.
REFERENCES
- 1.Sedlis S. Meeting Perspectives: American Heart Association Scientific Sessions 2009. Clinical Correlations: The NYU Langone Online Journal of Medicine. [Accessed September 2, 2014]; http://www.clinicalcorrelations.org/?p=2123. [Google Scholar]
- 2.American Heart Association. Scientific Sessions, 2014. [Accessed September 2, 2014]; http://www.exhibitatsessions.org/. [Google Scholar]
- 3.Alexander W. 2012 American College of Cardiology 61st Annual Scientific Session & Expo. PT. 2012;37(5):303–305. [PMC free article] [PubMed] [Google Scholar]
- 4.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345(9):663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 5.Kostis WJ, Demissie K, Marcella SW, Shao YH, Wilson AC, Moreyra AE Myocardial Infarction Data Acquisition System (MIDAS 10) Study Group. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356(11):1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 6.Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta-analysis. BMJ. 2014;348:f7393. doi: 10.1136/bmj.f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lairez O, Roncalli J, Carrié D, et al. Relationship between time of day, day of the week and in-hospital mortality in patients undergoing emergency percutaneous coronary intervention. Arch Cardiovasc Dis. 2009;102(12):811–820. doi: 10.1016/j.acvd.2009.09.010. [DOI] [PubMed] [Google Scholar]
- 8.Assali AR, Brosh D, Vaknin-Assa H, et al. The impact of circadian variation on outcomes in emergency acute anterior myocardial infarction percutaneous coronary intervention. Catheter Cardiovasc Interv. 2006;67(2):221–226. doi: 10.1002/ccd.20608. [DOI] [PubMed] [Google Scholar]
- 9.Maier B, Behrens S, Graf-Bothe C, et al. Time of admission, quality of PCI care, and outcome of patients with ST-elevation myocardial infarction. Clin Res Cardiol. 2010;99(9):565–572. doi: 10.1007/s00392-010-0158-2. [DOI] [PubMed] [Google Scholar]
- 10.Guide to Inpatient Quality Indicators: Quality of Care in Hospitals–Volume, Mortality, and Utilization. Rockville, MD: Agency for Healthcare Research and Quality; 2007. Agency for Healthcare Research and Quality. [Google Scholar]
- 11.Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among patients in VA hospitals in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):984–992. doi: 10.1001/jama.298.9.984. [DOI] [PubMed] [Google Scholar]
- 12.Volpp KG, Rosen AK, Rosenbaum PR, et al. Mortality among hospitalized Medicare beneficiaries in the first 2 years following ACGME resident duty hour reform. JAMA. 2007;298(9):975–983. doi: 10.1001/jama.298.9.975. [DOI] [PubMed] [Google Scholar]
- 13.Jena AB, Sun EC, Romley JA. Mortality among high-risk patients with acute myocardial infarction admitted to U.S. teaching-intensive hospitals in July: a retrospective observational study. Circulation. 2013;128(25):2754–2763. doi: 10.1161/CIRCULATIONAHA.113.004074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girotra S, Chan PS. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2013;368(7):680–681. doi: 10.1056/NEJMc1215155. [DOI] [PubMed] [Google Scholar]
- 15.Volpp KG, Rosen AK, Rosenbaum PR, et al. Did duty hour reform lead to better outcomes among the highest risk patients? J Gen Intern Med. 2009;24(10):1149–1155. doi: 10.1007/s11606-009-1011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joynt KE, Blumenthal DM, Orav EJ, Resnic FS, Jha AK. Association of public reporting for percutaneous coronary intervention with utilization and outcomes among Medicare beneficiaries with acute myocardial infarction. JAMA. 2012;308(14):1460–1468. doi: 10.1001/jama.2012.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiener RS, Welch HG. Trends in the use of the pulmonary artery catheter in the United States, 1993–2004. JAMA. 2007;298(4):423–429. doi: 10.1001/jama.298.4.423. [DOI] [PubMed] [Google Scholar]
- 18.American College of Cardiology, Attendee Demographics. [Accessed November 8, 2014]; http://www.expo.acc.org/ACC14/public/Content.aspx?ID=45950&sortMenu=105001. [Google Scholar]
- 19.Prasad V, Jena AB. Prespecified falsification end points: can they validate true observational associations? JAMA. 2013;309(3):241–242. doi: 10.1001/jama.2012.96867. [DOI] [PubMed] [Google Scholar]
- 20.Jena AB, Sun E, Goldman DP. Confounding in the association of proton pump inhibitor use with risk of community-acquired pneumonia. J Gen Intern Med. 2013;28(2):223–230. doi: 10.1007/s11606-012-2211-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ioannidis JP. Are mortality differences detected by administrative data reliable and actionable? JAMA. 2013;309(13):1410–1411. doi: 10.1001/jama.2013.3150. [DOI] [PubMed] [Google Scholar]
- 22.Carson JL, Carless PA, Hébert PC. Outcomes using lower vs higher hemoglobin thresholds for red blood cell transfusion. JAMA. 2013;309(1):83–84. doi: 10.1001/jama.2012.50429. [DOI] [PubMed] [Google Scholar]
- 23.de Mulder M, Umans VA, Cornel JH, et al. Intensive glucose regulation in hyperglycemic acute coronary syndrome: results of the randomized BIOMarker study to identify the acute risk of a coronary syndrome-2 (BIOMArCS-2) glucose trial. JAMA Intern Med. 2013;173(20):1896–1904. doi: 10.1001/jamainternmed.2013.10074. [DOI] [PubMed] [Google Scholar]
- 24.Kox M, Pickkers P. “Less is more” in critically ill patients: not too intensive. JAMA Intern Med. 2013;173(14):1369–1372. doi: 10.1001/jamainternmed.2013.6702. [DOI] [PubMed] [Google Scholar]
- 25.Snowden JM, Darney BG, Cheng YW, McConnell KJ, Caughey AB. Systems factors in obstetric care: the role of daily obstetric volume. Obstet Gynecol. 2013;122(4):851–857. doi: 10.1097/AOG.0b013e3182a2dd93. [DOI] [PubMed] [Google Scholar]
- 26.Tucker J UK Neonatal Staffing Study Group. Patient volume, staffing, and workload in relation to risk-adjusted outcomes in a random stratified sample of UK neonatal intensive care units: a prospective evaluation. Lancet. 2002;359(9301):99–107. doi: 10.1016/s0140-6736(02)07366-x. [DOI] [PubMed] [Google Scholar]
- 27.Siegel-Itzkovich J. Doctors’ strike in Israel may be good for health. BMJ. 2000;320(7249):1561. doi: 10.1136/bmj.320.7249.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cunningham SA, Mitchell K, Narayan KM, Yusuf S. Doctors’ strikes and mortality: a review. Soc Sci Med. 2008;67(11):1784–1788. doi: 10.1016/j.socscimed.2008.09.044. [DOI] [PubMed] [Google Scholar]
- 29.De Backer D, Biston P, Devriendt J, et al. SOAP II Investigators. Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362(9):779–789. doi: 10.1056/NEJMoa0907118. [DOI] [PubMed] [Google Scholar]
- 30.Tavazzi L, Maggioni AP, Lucci D, et al. Italian survey on Acute Heart Failure Investigators. Nationwide survey on acute heart failure in cardiology ward services in Italy. Eur Heart J. 2006;27(10):1207–1215. doi: 10.1093/eurheartj/ehi845. [DOI] [PubMed] [Google Scholar]
- 31.Shaffer JP. Multiple hypothesis testing. Annu Rev Psychol. 1995;46:561–584. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.