Abstract
Objectives
We describe the medication information-seeking behaviors of arthritis patients’ partners and explore whether partner medication information-seeking and information-sharing are associated with patient medication adherence.
Methods
Arthritis patients and their partners (n=87 dyads) completed an on-line questionnaire. Partners indicated how often they obtained medication information from 14 sources, how much they trusted these sources, and whether they shared medication information with the patient. Patients reported their medication adherence. Bivariate associations were calculated to explore the relationships between partner information-seeking, information-sharing, and patient medication adherence.
Results
Partners sought little information about the patient's medications. Partners sought more information if the patient's medication regimen was more complex (r=0.33, p= 0.002). Most partners (~98%) shared medication information with the patient; older partners shared more information with the patient (r=0.25, p=0.03). Neither partner information-seeking (r=0.21, p=0.06) nor partner information-sharing (r=0.12, p=0.31) were significantly associated with patient medication adherence.
Conclusions
Although partners of arthritis patients do not seek large amounts of medication information, the vast majority share this information with the patient.
Practice Implications
Involving partners in medical consultations can help them better understand the patient's medications, have questions answered by providers, and engage in more informed discussions with patients about their medications.
Keywords: Arthritis, Partner, Information-seeking, Information-sharing
1. Introduction
Emotional and instrumental support from partners can increase patient medication adherence [1, 2], but the effects of partner-provided medication-related informational support remain unexplored. The Information-Motivation-Behavioral Skills Model (IMB) posits that better informed, more motivated patients are more adherent [3, 4]. Studies of the IMB model show that medication information and perceptions of adherence-related support positively affect adherence behavioral skills [5-10] and medication adherence [5, 9, 10]. Thus, when partners provide patients with medication information, the information itself, as well as patient perceptions of partner support, could improve patient medication adherence.
Because arthritis is painful and can impact patients’ ability to engage in daily activities, partners may seek information about the patient's medications as an adaptive coping mechanism or to supplement information from professional sources [11, 12]. Using cross-sectional data from 87 arthritis patient-partner dyads, we: 1) describe which medication information sources partners use and trust; 2) explore whether patient and partner demographic/clinical characteristics, including patient arthritis type, are associated with partners’ medication information-seeking and information-sharing; and 3) examine whether partner information-seeking and information-sharing are associated with patient medication adherence.
2. Methods
2.1 Participants and methods
Online questionnaire data were collected as part of a larger study [13, 14]. Eligible patients had a self-reported diagnosis of osteoarthritis (OA) or rheumatoid arthritis (RA), were ≥18 years old, could read English, had Internet access, and were currently taking ≥ 1 medication to treat their arthritis on a routine basis. Individuals taking medications “as needed” were ineligible. The 30-45 minute patient and partner surveys included 84 and 52 questions, respectively. This study was approved by (name blinded) Institutional Review Board.
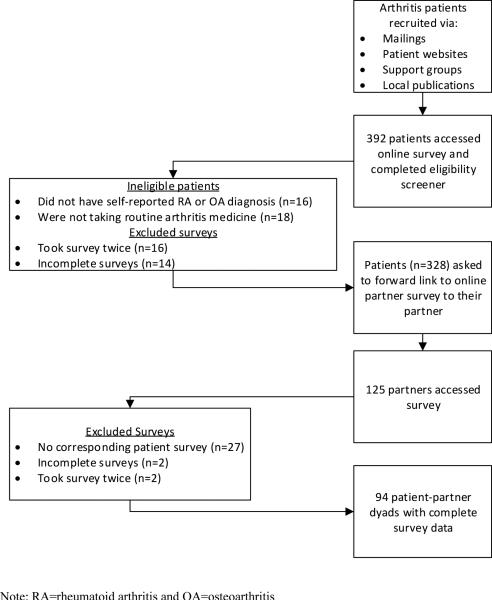
We mailed recruitment letters to patients with an OA or RA (ICD-9 diagnosis code of 714 or 715) diagnosis listed in the (name blinded) hospital's electronic health record (Figure 1). We also advertised the study on arthritis websites and in local media publications, distributed brochures at local clinics and support groups, and mailed recruitment letters to patients who participated in other (university) arthritis studies.
Figure 1.
Recruitment flow chart for arthritis patients and their partners
Patients’ partners were recruited by a snowball technique in which patients were asked to share the study website with their partners. Participants received a $10 incentive.
2.2 Measures
2.2.1 Information source use and trust
We asked partners, “when your spouse/partner begins taking a new arthritis medicine, how much information do you get from the people and places listed below?” Responses ranged from 1= “none” to 4= “a lot.” A mean partner source use score was created by averaging use across 14 sources.
Partners also reported, “with regards to your partner's arthritis medicines, how trustworthy do you consider the following source to be?” Responses ranged from 1= “not at all trustworthy” to 4= “very trustworthy.”
2.2.2 Partner information-sharing
Partners reported how often they shared arthritis medicine information with the patient. Responses ranged from 1= “never” to 4= “often.” Partners also reported how often they discussed seven topics, including drug effectiveness and side effects, with the patient; responses ranged from 1= “we never discuss it’” to 4= “we discuss it a lot.”
2.2.3 Patient medication adherence
Patients self-reported medication adherence using a validated Visual Analog Scale [15-17]. Patients were asked, “All things considered, how much of the time do you take ALL of your medications EXACTLY as directed?” Responses ranged from 0-100; higher scores indicated better adherence.
2.2.4 Sociodemographic and clinical characteristics
Partners and patients reported their gender, race, age, education, and marital status. Patients reported their disease duration, years taking arthritis medications, arthritis type, health insurance status, perceived complexity of their medication regimen (1= “not at all complex” to 10= “extremely complex”), and perceived arthritis severity (1= “not at all severe” to 10= “extremely severe”). Patients who reported both RA and OA were categorized as having RA.
2.3 Data analysis
We used IBM SPSS Statistics v19 to generate univariate statistics to characterize the sample. Non-parametric tests of association were calculated to explore the relationships between all partner and patient demographic/clinical characteristics with partner information-seeking, information-sharing, and patient medication adherence; α=0.05.
3. Results
Table 1 summarizes the sample of 87 patient-partner dyads. Partners sought minimal medication information (M=1.92, SD=0.54). Table 2 presents the amount of medication information partners of OA and RA patients obtained from each source, and Table 3 presents partners’ perceived trust of each source. Partners obtained the most medication information from the patient and physicians and trusted physicians, pharmacists, nurses, and the patient most.
Table 1.
Characteristics of arthritis patients and their partners (n=87 dyads)
| Patient | Partner | |||
|---|---|---|---|---|
| Characteristic | Mean (SD) or n(%) | Range | Mean (SD) or n (%) | Range |
| Age | 55.9 (13.8) | 22.0-85.0 | 54.7 (13.6) | 24.0-83.0 |
| Female | 60 (69.0) | 27 (31.0) | ||
| Race | ||||
| White | 74 (85.1) | 75 (86.2) | ||
| Black | 8 (9.2) | 9 (10.3) | ||
| Other | 5 (5.7) | 3 (3.4) | ||
| Education | ||||
| High school diploma or less | 20 (23.0) | 23 (26.4) | ||
| Some college | 19 (21.8) | 17 (19.5) | ||
| Associates degree or more | 48 (55.1) | 47 (54.0) | ||
| Years married/partnered | 25.5 (16.5) | 1.0-59.0 | ||
| Patient arthritis type | ||||
| Osteoarthritis | 44 (50.6) | |||
| Rheumatoid arthritis | 43 (49.4) | |||
| Patient disease duration (in years) | 11.4 (8.7) | 0.5-42.5 | ||
| Patient perceived disease severity | 6.2 (1.8) | 1.0-10.0 | ||
| Patient perceived regimen complexity | 2.9 (2.2) | 1.0-9.0 | ||
| Partner has arthritis | 20 (23.0) | |||
Table 2.
Partners’ use of medication information sources (n=87)
| Patient has OA (n=44) n(%) | Patient has RA (n=43) n(%) | |||||
|---|---|---|---|---|---|---|
| Source | None | A little/some | A lot | None | A little/some | A lot |
| Patient | 2(4.5) | 26(59.1) | 16(36.4) | 5(11.6) | 15(44.9) | 23(53.5) |
| Physicians | 16(36.4) | 16(34.1) | 13(29.5) | 12(27.9) | 19(44.2) | 12(27.9) |
| Medicine package inserts | 13(29.5) | 24(54.5) | 7(15.9) | 13(30.2) | 23(53.5) | 6(14.0) |
| Internet | 21(47.7) | 19(43.2) | 4(9.1) | 12(27.9) | 18(41.9) | 11(25.6) |
| Pharmacists | 20(45.5) | 15(34.1) | 9(20.5) | 17(39.5) | 18(41.9) | 7(16.3) |
| Brochures/pamphlets | 16(36.4) | 23(52.3) | 5(11.4) | 13(30.2) | 23(53.5) | 7(16.3) |
| Research articles/books | 25(56.8) | 17(38.6) | 2(4.5) | 16(37.2) | 23(53.5) | 4(9.3) |
| Family members | 20(45.5) | 23(52.2) | 1(2.3) | 21(48.8) | 21(48.8) | 1(2.3) |
| Nurses/other health professionals | 25(56.8) | 15(34.1) | 4(9.1) | 26(60.5) | 13(30.3) | 3(7.0) |
| Media sources (TV, magazines, radio)* | 28(63.6) | 16(36.3) | 0(0.0) | 16(37.2) | 23(53.5) | 4(9.3) |
| Friends | 21(47.7) | 21(47.7) | 1(2.3) | 23(53.5) | 18(41.9) | 2(4.7) |
| Newsletters | 34(77.3) | 9(20.4) | 0(0.0) | 27(62.8) | 13(30.2) | 2(4.7) |
| Support groups | 37(84.1) | 7(15.9) | 0(0.0) | 35(81.4) | 7(16.3) | 1(2.3) |
| Podcasts | 40(90.9) | 2(4.5) | 0(0.0) | 39(90.7) | 2(4.7) | 0(0.0) |
Note: response options included: 1= “none”, 2= “a little”, 3= “some”, and 4= “a lot”
Some rows do not total to 100% due to missing data
RA partners more likely to use media sources χ2(2)=8.52; p=0.01
Table 3.
Partners’ perceived trust of medication information sources (n=87)
| Patient has OA (n=44) n(%) |
Patient has RA (n=43) n(%) |
|||||
|---|---|---|---|---|---|---|
| Source | Not at all trustworthy |
A little/somewhat trustworthy |
Very trustworthy |
Not at all trustworthy |
A little/somewhat trustworthy |
Very trustworthy |
| Patient | 1(2.3) | 20(45.4) | 22(50.0) | 2(4.7) | 10(23.3) | 29(67.4) |
| Physicians | 0(0.0) | 12(27.3) | 32(72.7) | 0(0.0) | 19(44.2) | 24(55.8) |
| Medicine package inserts | 0(0.0) | 27(61.3) | 16(36.4) | 2(4.7) | 27(62.8) | 13(30.2) |
| Internet | 5(11.4) | 35(79.5) | 4(9.1) | 4(9.3) | 34(79.0) | 3(7.0) |
| Pharmacists | 0(0.0) | 14(31.8) | 30(68.2) | 0(0.0) | 21(48.9) | 20(46.5) |
| Brochures/pamphlets | 2(4.5) | 35(79.5) | 7(15.9) | 4(9.3) | 32(74.5) | 4(11.6) |
| Research articles/books | 2(4.5) | 32(79.7) | 10(22.7) | 3(7.0) | 31(72.1) | 9(20.9) |
| Family members | 2(4.5) | 34(77.3) | 7(15.9) | 6(14.0) | 30(69.8) | 4(9.3) |
| Nurses/other health professionals | 1(2.3) | 24(54.6) | 18(40.9) | 0(0.0) | 30(69.8) | 10(23.3) |
| Media sources (TV, magazines, radio) | 9(20.5) | 33(75.0) | 1(2.3) | 14(32.6) | 28(65.1) | 1(2.3) |
| Friends | 6(13.6) | 33(75.0) | 5(11.4) | 7(16.3) | 28(65.1) | 5(11.6) |
| Newsletters | 10(22.7) | 30(68.1) | 3(6.8) | 7(16.3) | 30(69.7) | 2(4.7) |
| Support groups | 13(29.5) | 29(65.9) | 1(2.3) | 8(18.6) | 27(62.8) | 2(4.7) |
| Podcasts | 20(45.5) | 19(43.2) | 3(6.8) | 17(39.5) | 16(37.2) | 0(0.0) |
Note: response options included: 1= “not at all trustworthy”, 2= “a little trustworthy”, 3= “somewhat trustworthy”, and 4= “very trustworthy”
Some rows do not total to 100% due to missing data
Most partners (97.7%) shared arthritis medication information with the patient; 15.1% shared rarely, 41.9% shared sometimes, and 40.7% shared often. Medication effectiveness was the topic partners discussed most with patients (Table 4).
Table 4.
Medication topics partners discussed most often with patients (n=87)
| Patient has OA (n=44) n(%) | Patient has RA (n=43) n(%) | |||
|---|---|---|---|---|
| Topic | Never/Hardly ever | A fair amount/A lot | Never/Hardly ever | A fair amount/A lot |
| How effective arthritis medicines are at treating your spouse/partner's symptoms | 15(34.1) | 29(65.9) | 7(16.3) | 35(81.4) |
| Arthritis medicines (general) | 16(36.3) | 28(63.6) | 12(27.9) | 30(69.8) |
| Arthritis medicines’ side effects | 17(38.6) | 27(61.3) | 16(37.2) | 26(60.4) |
| How arthritis medicines interact with other medicines your spouse/partner is taking | 23(52.3) | 21(47.7) | 17(39.6) | 25(58.1) |
| How to take arthritis medicines (with meals, with water, in the morning) | 23(52.3) | 22(45.4) | 21(48.9) | 21(48.9) |
| The financial costs of your spouse/partner's medicines | 23(52.3) | 21(47.7) | 24(55.9) | 18(41.8) |
| Alternative/ complementary/ holistic medicines or therapies | 27(61.4) | 17(38.6) | 26(60.5) | 16(37.2) |
Note: response options included: 1= “we never discuss it”, 2= “we hardly ever discuss it”, 3= “we discuss it a fair amount”, and 4= “we discuss it a lot”
Some rows do not total to 100% due to missing data
Partner information-seeking and information-sharing were positively associated (r=0.51, p<0.001). Partners sought more information about the patient's arthritis medications if the patient reported a more complex medication regimen (r= 0.33, p= 0.002). Older partner age was associated with sharing more information with the patient (r=0.25, p=0.03). No other variables were associated with partner information-seeking or information-sharing (supplementary materials).
Neither partner information-seeking (r=0.21, p=0.06) nor partner information-sharing (r=0.12, p=0.31) were significantly associated with patient medication adherence.
4. Discussion and Conclusion
When partners provide patients with medication information, the medication information itself, as well as patient perceptions of partner support, could lead to improved medication adherence [3, 4]. In our sample, however, partner information-seeking was not significantly associated with better patient adherence. Partners sought more information if the patient reported a more complex medication regimen. A complex regimen may cause patients to explicitly ask their partners for treatment-related support, which may trigger partners to seek treatment-related information. Older partners in our sample shared more information about the patient's medications than younger partners, which may reflect that older adults are more likely to search for treatment information than younger adults [12, 18].
Partners also highly trusted and used the patient for medication information, which could be due to ease of access to the patient [19, 20]. Although partners’ trusted professional sources, they used these sources minimally, possibly due to previous negative experiences during clinical encounters [21-23].
4.1.2 Limitations
Several limitations deserve mention. First, past research suggests that patients may over-report medication adherence [24, 25]. Partners may have also over-reported their information-seeking and information-sharing. The information-seeking and information–sharing measures have not been validated and ask partners to recall information-seeking at one point in time: when the patient receives a new arthritis medication, which may occur rarely. Furthermore, patients may interpret discussions about medications as general support rather than informational support. Partners in our convenience sample may have used more medication sources because they had Internet access and could have been more supportive than the general population of partners. Thus, our results may overestimate the amount of medication information partners seek and share and may not generalize to the larger population of arthritis patient-partner dyads.
4.2 Conclusion
This study adds new knowledge about partner use and trust of medication information sources. Although our sample of arthritis patients’ partners did not seek large amounts of medication information, the vast majority shared that information with the patient. Future qualitative studies should investigate the nature of medication information exchange between patients and partners and explore why partners seek medication information for the patient and how they intend to use information to support the patient. Research that examines patient-partner variation in acquisition and discussion of medication information would provide a more in-depth understanding of the relationships between information, support, and adherence. Longitudinal studies using daily diaries may reveal interesting patterns in partner information-seeking and sharing since source use and preferences may change over time [26, 27].
4.3 Practice Implications
Partners share medication information with the patient. Providers can invite patients to involve partners in their health care. Involving partners in medical consultations can help them better understand the patient's medications, engage in more informed discussions with the patient, and have their medication questions answered by providers, who are their most trusted source of medication information.
Supplementary Material
Acknowledgments
Funding support: This work was supported by the Thurston Arthritis Research Center Postdoctoral Fellowship (T32AR007416) and Novartis Pharmaceuticals. Dr. Carpenter's salary was partially supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR000084. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Delesha M. Carpenter, Division of Pharmaceutical Outcomes and Policy University of North Carolina Asheville, USA.
Emily A. Elstad, Department of Health Behavior University of North Carolina Chapel Hill, USA.
Adam J. Sage, RTI International Durham, USA.
Lorie L. Geryk, Division of Pharmaceutical Outcomes and Policy University of North Carolina Chapel Hill, USA.
Robert F. DeVellis, Thurston Arthritis Research Center University of North Carolina Chapel Hill, USA.
Susan J. Blalock, Division of Pharmaceutical Outcomes and Policy University of North Carolina Chapel Hill, USA.
REFERENCES
- 1.Dimatteo MR. Social support and patient adherence to medical treatment: A meta-analysis. Health Psychol. 2004;23:207–18. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- 2.Gallant MP. The influence of social support on chronic illness self-management: A review and directions for research. Health EducBehav. 2003;30:170–95. doi: 10.1177/1090198102251030. [DOI] [PubMed] [Google Scholar]
- 3.Fisher WA, Fisher JD, Harman JJ, Suls J, Wallston K. Social psychological foundations of health and illness. Blackwell Publishing Ltd; Malden, MA: 2003. The Information-Motivation-Behavioral Skills Model: A general social psychological approach to understanding and promoting health behavior. pp. 82–106. [Google Scholar]
- 4.Fisher JD, Fisher WA, DiClemente R, Crosby R, Kegler M. Emerging theories in health promotion practice and research. Jossey Bass Publishers; San Francisco, CA: 1992. The Information-Motivation Behavioral Skills Model. pp. 40–70. [Google Scholar]
- 5.Kalichman SC, Rompa D, DiFonzo K, Simpson D, Austin J, Luke W, et al. HIV treatment adherence in women living with HIV/AIDS: Research based on the Information-Motivation-Behavioral Skills Model of health behavior. J Assn Nurses AIDS Care. 2001;12:58–67. doi: 10.1016/S1055-3290(06)60217-3. [DOI] [PubMed] [Google Scholar]
- 6.Amico KR, Toro-Alfonso J, Fisher JD. An empirical test of the Information, Motivation and Behavioral Skills model of antiretroviral therapy adherence. AIDS Care. 2005;17:661–73. doi: 10.1080/09540120500038058. [DOI] [PubMed] [Google Scholar]
- 7.Starace F, Massa A, Amico KR, Fisher JD. Adherence to antiretroviral therapy: An empirical test of the Information-Motivation-Behavioral Skills model. Health Psychol. 2006;25:153–62. doi: 10.1037/0278-6133.25.2.153. [DOI] [PubMed] [Google Scholar]
- 8.Amico KR, Barta W, Konkle-Parker DJ, Fisher JD, Cornman DH, Shuper PA, et al. The Information-Motivation-Behavioral Skills model of ART adherence in a deep south HIV+ clinic sample. AIDS Behav. 2009;13:66–75. doi: 10.1007/s10461-007-9311-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horvath KJ, Smolenski D, Amico KR. An empirical test of the Information-Motivation-Behavioral Skills model of ART adherence in a sample of HIV-positive persons primarily in outof-HIV-care settings. AIDS Care. 2014;26:142–51. doi: 10.1080/09540121.2013.802283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayberry LS, Osborn CY. Empirical validation of the Information–Motivation–Behavioral Skills model of diabetes medication adherence: A framework for intervention. Diabetes Care. 2014;37:1246–53. doi: 10.2337/dc13-1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson JD. Cancer-related information seeking. Hampton Press, Inc.; Cresskill, N.J.: 1997. [Google Scholar]
- 12.Sadasivam RS, Kinney RL, Lemon SC, Shimada SL, Allison JJ, Houston TK. Internet health information seeking is a team sport: Analysis of the Pew Internet Survey. Int J Med Inform. 2013;82:193–200. doi: 10.1016/j.ijmedinf.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 13.Carpenter DM, Elstad EA, Blalock SJ, DeVellis RF. Conflicting medication information: Prevalence, sources, and relationship to medication adherence. J Health Comm. 2014;19:67–81. doi: 10.1080/10810730.2013.798380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elstad E, Carpenter DM, Devellis RF, Blalock SJ. Patient decision making in the face of conflicting medication information. Int J Qual Studies Health Well-being. 2012:7. doi: 10.3402/qhw.v7i0.18523. Available online: doi 10.3402/qhw.v7i0.18523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walsh JC, Mandalia S, Gazzard BG. Responses to a 1 month self-report on adherence to antiretroviral therapy are consistent with electronic data and virological treatment. AIDS. 2002;16:269–77. doi: 10.1097/00002030-200201250-00017. [DOI] [PubMed] [Google Scholar]
- 16.Giordano TP, Guzman D, Clark R, Charlebois ED, Bangsber DR. Measuring adherence to antiretroviral therapy in a diverse population using a visual analog scale. HIV Clin Trials. 2004;5:74–9. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- 17.Amico KR, Fisher WA, Cornman DH, Shuper PA, Redding CG, Konkle-Parker DJ, et al. Visual Analog Scale of ART adherence: Association with 3-day self-report and adherence barriers. J Acquir Immune Defic Syndr. 2006;42:455–9. doi: 10.1097/01.qai.0000225020.73760.c2. [DOI] [PubMed] [Google Scholar]
- 18.Fox S. [September 10, 2014];Health information online: Eight in ten internet users have looked for health information online, with increased interest in diet, fitness, drugs, health insurance, experimental treatments, and particular doctors and hospitals: Pew Internet & American Life Project. 2005 Available at: http://www.pewinternet.org/2005/05/17/health-information-online/
- 19.Lambert SD, Loiselle CG. Health Information-Seeking Behavior. Qual Health Res. 2007;17:1006–19. doi: 10.1177/1049732307305199. [DOI] [PubMed] [Google Scholar]
- 20.Rees CE, Bath PA, Lloyd-Williams M. The information concerns of spouses of women with breast cancer: patients' and spouses' perspectives. J Ad Nurs. 1998;28:1249–58. doi: 10.1046/j.1365-2648.1998.00833.x. [DOI] [PubMed] [Google Scholar]
- 21.Feltwell AK, Rees CE. The information-seeking behaviours of partners of men with prostate cancer: a qualitative pilot study. Patient Educ Couns. 2004;54:179–85. doi: 10.1016/S0738-3991(03)00212-X. [DOI] [PubMed] [Google Scholar]
- 22.Rees CE, Bath PA. The information needs and source preferences of women with breast cancer and their family members: a review of the literature published between 1988 and 1998. J Adv Nurs. 2000;31:833–41. doi: 10.1046/j.1365-2648.2000.01341.x. [DOI] [PubMed] [Google Scholar]
- 23.McCarthy B. Family members of patients with cancer: What they know, how they know and what they want to know. Eur J Oncol Nurs. 2011;15:428–41. doi: 10.1016/j.ejon.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 24.Nau DP, Steinke DT, Williams K, Austin R, Lafata JE, Divine G. Adherence analysis using visual analog scale versus claims-based estimation. Ann Pharmacother. 2007;41:1792–7. doi: 10.1345/aph.1K264. [DOI] [PubMed] [Google Scholar]
- 25.Treharne GJ, Lyons AC, Hale ED, Douglas KMJ, Kitas GD. ‘Compliance’ is futile but is ‘concordance’ between rheumatology patients and health professionals attainable? Rheumatology. 2006;45:1–5. doi: 10.1093/rheumatology/kei223. [DOI] [PubMed] [Google Scholar]
- 26.Mills ME, Davidson R. Cancer patients’ sources of information: Use and quality issues. Psycho-Oncology. 2002;11:371–8. doi: 10.1002/pon.584. [DOI] [PubMed] [Google Scholar]
- 27.Squiers L, Rutten LJF, Treiman K, Bright MA, Hesse BW. Cancer patients’ information needs across the cancer care continuum: Evidence for the Cancer Information Service. J Health Comm. 2005;10:15–34. doi: 10.1080/10810730500263620. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.