ABSTRACT
BACKGROUND
Patients with obesity face widespread social bias, but the importance of this social stigma to patients relative to other quality of life (QOL) factors is unclear.
OBJECTIVE
Our aim was to examine the importance of obesity-related social stigma relative to other QOL factors on reducing patients’ overall well-being.
DESIGN
We used a cross-sectional telephone interview.
SETTING
The study was conducted at four diverse primary care practices in Greater Boston.
PARTICIPANTS
Three hundred and thirty-seven primary care patients aged 18–65 years and with a body mass index (BMI) of 35 kg/m2 or higher participated in the study.
MAIN MEASURES
Patients’ health utility (preference-based QOL measure) was determined via responses to a series of standard gamble scenarios assessing willingness to risk death to lose various amounts of weight or to achieve perfect health. We used the Impact of Weight on Quality of Life-lite instrument to assess QOL domains specific to obesity (physical function, self-esteem, sexual life, public distress or social stigma, and work), and we examined variation in utility explained by these domains.
KEY RESULTS
Depending on patients’ race/ethnicity, mean health utilities ranged from 0.92 to 0.99 among men and from 0.89 to 0.93 among women. After adjustment for race, BMI, and education, none of the QOL domains explained much of the variation in utility among men, except for work function among Hispanic men. In contrast, social stigma was the leading QOL contributor to utility for Caucasian women (explaining 6 % of the marginal variation beyond demographics and BMI). In contrast, sexual function was the most important contributor among African American women (3 % marginal variation), and work life was most important among Hispanic women (> 20 % in variation). Lower scores in one domain did not always translate into lower well-being. Moreover, QOL summary scores often explained less of the variation than some individual domains.
CONCLUSION
Obesity-related social stigma had disproportionate adverse effects on Caucasian women patients’ well-being, whereas weight-related impairment in work function was particularly important among Hispanic patients and impaired sexual function was important to diminished well-being among African American women although its impact appeared modest.
KEY WORDS: obesity, quality of Life, sex, race, stigma
INTRODUCTION
More than a third of U.S. adults are obese and 14 % have moderate to severe obesity with a body mass index (BMI) of 35 or greater.1 Obesity’s adverse effects are far-reaching. Not only is obesity a major contributor to reduced life-expectancy and many chronic health conditions,2–5 obesity has substantial negative physical, social, and economic effects that impair quality of life (QOL).6,7
Obesity’s adverse impact on QOL is distinctive, however, in that it impairs QOL not only because of its direct health burden, but also because obesity is socially stigmatizing.8 Compelling evidence suggests that obese persons experience bias in many facets in society, including education, employment, socialization, and even healthcare treatment.8 Not surprisingly, patients with obesity often report lower QOL in many non-traditional domains including reduced self-esteem and social stigma.7,9–12 Interestingly, QOL scores in obese individuals appear to vary by gender and race, with Caucasian women reporting the greatest impairments, particularly in the psychosocial domains, based on scores on health status QOL measures.7 However, while traditional health status QOL instruments are able to measure obesity’s impact on various general and obesity-specific QOL domains, what they cannot tell us is the relative importance each of these domains may have to different patients. For example, someone may have a lower QOL score in the area of sexual function than in their work function; however, to that patient, their weight’s adverse effect on work function may be more distressing and have a larger negative impact. Identifying factors that are particularly important in driving diminished overall well-being—especially if they vary across different demographic subgroups—may help us understand what motivates some patients to seek weight loss treatment and the degree to which they may or may not be motivated. In addition, a better understanding of the QOL domains most important to patients will help us identify QOL outcomes most relevant in evaluating the value and effectiveness of different weight treatments, and facilitate decision-making that incorporates these patients’ values.
To address this issue, we interviewed a sample of over 330 primary care patients with moderate to severe obesity seen in four diverse practices in greater-Boston. In addition to collecting information about QOL via traditional health status measures, we assessed patients’ preference for their current health and weight state by measuring their health utility, the gold standard method for having patients quantify the value of their current well- being.13 In another analysis, we found that patients’ overall QOL score was more important than their obesity-related comorbid conditions in explaining how obesity adversely affects patients’ health utility (manuscript under review). We extend this work by identifying the QOL domains most important to different gender and racial and ethnic subgroups. We hypothesized that reduced self-esteem and social stigma may be especially important considerations among women, whereas work dysfunction might be more important among men. We also hypothesized that the degree of these gender-specific effects would be more pronounced among Caucasian than among African American or Hispanic patients.
METHODS
Study Sample, Recruitment, and Data Collection
We studied a complex random sample of 337 primary care patients with moderate to severe obesity recruited from four diverse primary care practices in Greater Boston. By design, racial and ethnic minorities were oversampled and sampling weights were created so that our estimates could reflect the population of the practices from which patients were recruited. The goal of the broader study was to understand patient preferences for weight loss and weight loss treatment, especially bariatric surgery, and the factors that underlie variation. The four practices included a large, hospital-based academic practice, a community practice in a working class neighborhood, a community health center in a socioeconomically disadvantaged neighborhood, and a practice in an affluent suburb. Detailed research methods have been previously described.14 Eligible patients had a BMI ≥ 35, were aged 18 to 65 years, and had valid contact information and their physician’s approval to participate. Participants could be either English-speaking or Spanish-speaking. Participants were offered a $25 incentive for participating in a 45-minute telephone survey; 58 % of eligible patients responded. The survey was administered by trained interviewers; for Spanish-speaking patients, the interview was conducted in Spanish.
Health Utility
As a measure of patients’ well-being, we used a modified version of the standard gamble method to assess patients’ preference or “utility” for their current weight and health. We asked patients to consider a hypothetical choice of either 1) continuing at their current health and weight without any improvement, or 2) taking a gamble. The gamble has two possible outcomes; the positive outcome of “perfect health” and a negative outcome of immediate death. Because we have found in earlier work that patients don’t always value perfect health more than being at a lower body weight,15 we administered a series of additional scenarios where we substituted perfect health with achieving a pre-specified level of weight loss as the desired outcome, in order to anchor utilities to patients’ most desired health state. We then specified that the treatment was associated with a small risk of dying, and through an iterative process, we asked patients to estimate the highest risk of death they were willing to assume to achieve each weight outcome or perfect health. The specified weight loss, expressed in pounds, were, in order of presentation: patients’ self-reported “ideal” weight, weight loss associated with a BMI of 25 kg/m2 (framed as their “highest healthy weight”), 20 % weight loss, and 10 % weight loss.
Using their responses to the scenarios, we calculated patients’ utility relative to their most valued health state, whether it was perfect health or one of the lower weight states; the most valued state served as the reference state, with an assigned utility of 1.00. For example, if a patient responds that he/she is willing to assume the highest risk of death to achieve their ideal weight and that risk is 15 %, then he/she is calculated to have a current health utility of 0.85. Our group has used this approach in previous work, where willingness to assume risk to lose weight and weight-based utility has been shown to be associated with BMI and scores on health-related QOL measures.15,16
Health Status Measure of Qualify of Life
We assessed patients’ QOL via the Impact of Weight on Quality of Life-lite (IWQOL-lite), a 31-item instrument developed to capture QOL domains specific to obesity9—physical function, self-esteem, sexual life, public distress and work. The IWQOL-lite has been shown to display excellent psychometric properties and test-retest reliability.9 Patients are administered a series of statements that begin with “Because of my weight…” and then asked to rate whether the statements are “always true, usually true, sometimes true, rarely true or never true.” The Public Distress subscale asks whether the respondent experienced ridicule, teasing, or unwanted attention because of their weight, whether they worry about fitting into seats in public places, fitting into aisles, finding chairs that are strong enough, etc. and whether they experience discrimination. This subscale has been shown to have construct validity for measuring “weight stigma.”9,10 Each subscale is scored on a 0–100 scale,7 with higher scores reflecting better QOL.
Body Mass Index and Sociodemographic Factors
We estimated patients’ BMI by multiplying self-reported weight in pounds by 703 and dividing by the square of their height in inches. We also assessed patients’ age, sex, race and ethnicity, and educational level.
Data Analysis
We used descriptive statistics to characterize health utility and QOL scores by patient sex and race and ethnicity. We then developed multivariable linear regression models stratified by sex and race/ethnicity to examine the relative impact of the following factors on patients’ health utility: patient demographic factors (age, education), BMI, overall QOL via summary QOL scores, and individual subscale scores of each QOL domain measured by the IWQOL-lite. To assess the relative importance of each of these factors, we examined the change in model R2 with the addition of each subsequent variable relative to the previous model. The model R2 ranges up to 1.00 and can be interpreted as the proportion of the variability in outcome explained by variables in the model. Individual QOL subscales leading to the largest change in model R2 are deemed to be more important than other subscales that result in smaller changes in model R2.
RESULTS
Baseline characteristics have been previously described.17 Table 1 characterizes our sample by sex and race/ethnicity. Health utilities ranged from 0.89 to 0.99 among the subgroups, representing that on average, these groups of patients were willing to assume a 1 % to 11 % risk of dying to achieve their most valued health or weight state. Average health utilities were not statistically significantly different by sex or race and ethnicity.
Table 1.
Sample Characteristics of Primary Care Patients†
| Men | Overall (n=104) | Caucasian (n=50) | African American (n=19) | Hispanic (n=32) |
| Mean age | 45.7 | 50.1 | 43.1* | 40.1* |
| Mean BMI (kg/m2) | 39.3 | 40.0 | 39.3 | 38.3 |
| Mean Health Utility | 0.95 | 0.95 | 0.99 | 0.92 |
| Mean Quality of Life (Total) | 74.3 | 72.4 | 81.6 | 71.0 |
| Education, % | ||||
| High school or less | 39 | 20 | 63* | 50* |
| Some college or 2-year degree | 32 | 29 | 16* | 47* |
| 4-year college diploma or more | 29 | 51 | 21* | 3* |
| Women | Overall (n=230) | Caucasian (n=68) | African American (n=100) | Hispanic (n=51) |
| Mean age | 48.1 | 51.2 | 47.4* | 45.8* |
| Mean BMI (kg/m2) | 41.5 | 42.2 | 41.0 | 42.5 |
| Mean Health Utility | 0.92 | 0.93 | 0.94 | 0.89 |
| Mean Quality of Life (Total) | 68.0 | 62.0 | 72.7* | 65.3 |
| Education, % | ||||
| High school or less | 46 | 28 | 47* | 61* |
| Some college or 2-year degree | 27 | 22 | 33* | 22* |
| 4-year college diploma or more | 27 | 50 | 20* | 18* |
†Weighted samples were used to account for oversampling of nonwhites during recruitment
* and results in bold indicate statistically significant differences across the variable by race/ethnicity at p < 0.05. We used an ANOVA and Kruskal-Wallis one-way ANOVA for continuous and categorical variables, respectively, to determine if the specified variable was significant across all race/ethnicity groups. If the ANOVA or Kruskal-Wallis ANOVA tests were significant, a Dunnett’s pairwise comparison or Wilcoxon pairwise comparison test was used for continuous and categorical variables, respectively, to see if there were significant differences between Caucasian and African American patients or between Caucasian and Hispanic patients
Figure 1 presents QOL scores by sex and race and ethnicity after adjusting for age, BMI, and education. Men reported significantly higher QOL scores than women overall and in the domains of physical functioning, self-esteem, and public distress or weight-related social stigma. Similarly, African American patients consistently had significantly higher QOL scores overall and across many domains than Caucasians, whereas Hispanic patients had scores similar to Caucasians.
Figure 1.
Quality of life scores by sex and race among obese primary care patients after adjustment for age, BMI, race/ethnicity, and education. *P < 0.05 for a Wald test difference of means by sex. p < 0.05 for a Wald test difference of means by race/ethnicity African American compared to Caucasian; Hispanic compared to Caucasian were not significant for any of the models.
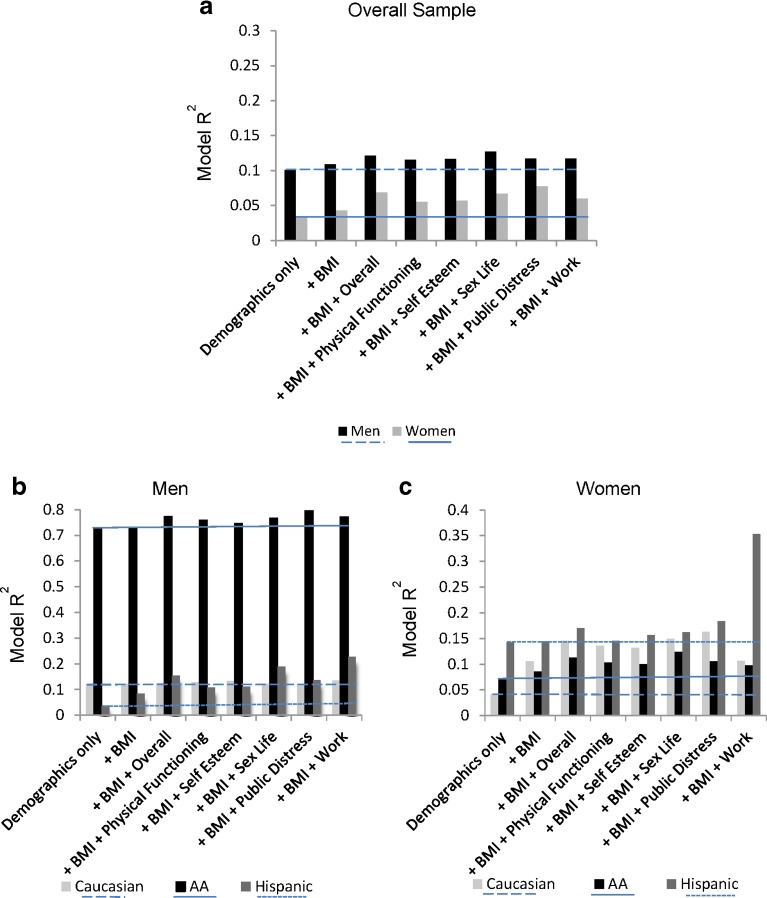
Figure 2 presents the relative importance of demographic factors, BMI, overall obesity-related QOL, and individual QOL domains in explaining the variation in utility expressed by men and women with obesity. Among men, demographic factors were associated with the largest change in model R2, explaining approximately 10 % of the variation in men’s utility; BMI only explained an additional 1 % of the variation (Fig. 2). Quality of life did not explain much of the marginal variation in utility. In contrast, among women, social stigma (public distress) and sexual function were both significantly associated with utility (see Table 2), with social stigma explaining the larger proportion of the variation in utility, comparable to the proportion explained by demographic factors and BMI together (see Fig. 2).
Figure 2.
Marginal contribution of individual quality of life domains in explaining the variation in patient’s health utility above and beyond demographic factors and BMI by sex and race/ethnicity for obese primary care patients. The first model (bar labeled “demographics only”) includes age, gender, and education. All subsequent models include the variables and/or subscales listed in addition to the variables in the first model. The area of the bars above the dotted or solid lines represents the additional/marginal contribution of the domain above and beyond demographic factors and BMI. There were only 19 African American men in the study; results pertaining to this group must be interpreted with extreme caution.
Table 2.
Association Between Quality of Life Domains and Health Utility+
| Men | Women | |||||||
|---|---|---|---|---|---|---|---|---|
| Overall | Caucasian | AA | Hispanic | Overall | Caucasian | AA | Hispanic | |
| Overall Score | 0.006±0.006 p=0.28 |
0.003±0.007 p=0.73 |
−0.003±0.002 p=0.16 |
0.024±0.017 p=0.18 |
0.017±0.008
p=0.02 |
0.021±0.014 p=0.12 |
0.017±0.011 p=0.12 |
0.023±0.022 p=0.31 |
| Physical Function | 0.004±0.004 p=0.43 |
0.003±0.007 p=0.60 |
−0.002±0.002 p=0.26 |
0.014±0.017 p=0.44 |
0.011±0.007 p=0.12 |
0.018±0.013 p=0.18 |
0.012±0.010 p=0.21 |
−0.004±0.020 p=0.86 |
| Self Esteem | 0.004±0.004 p=0.39 |
0.004±0.006 p=0.52 |
−0.001±0.001 p=0.43 |
0.012±0.015 p=0.41 |
0.009±0.006 p=0.09 |
0.013±0.011 p=0.22 |
0.009±0.008 p=0.26 |
0.012±0.018 p=0.49 |
| Sex Life | 0.006±0.004 p=0.20 |
0.000±0.005 p=0.95 |
−0.002±0.001 p=0.19 |
0.022±0.013 p=0.10 |
0.011±0.005
p=0.03 |
0.014±0.009 p=0.11 |
0.017±0.009 p=0.06 |
0.012±0.014 p=0.40 |
| Public Distress | 0.005±0.005 p=0.38 |
0.001±0.007 p=0.89 |
−0.004±0.002 p=0.07 |
0.017±0.014 p=0.25 |
0.018±0.007
p<0.01 |
0.024±0.013 p=0.06 |
0.013±0.010 p=0.18 |
0.021±0.016 p=0.21 |
| Work Life | 0.005±0.006 p=0.38 |
−0.005±0.008 p=0.48 |
−0.004±0.003 p=0.16 |
0.028±0.014
p=0.05 |
0.014±0.007 p=0.07 |
0.003±0.013 p=0.80 |
0.012±0.011 p=0.30 |
0.052±0.016
p<0.01 |
+ Quality of life was measured on a scale of 0 to 100 and utility on a scale of 0 to 1. The parameter estimates represent a ten-unit increase in the quality of life domains after adjustment for age, education, and BMI. Statistically significant results are in bold. There were only 19 African American men in the study; results pertaining to this group must be interpreted with extreme caution
When we stratified our results by race/ethnicity (Fig. 2, Table 2), however, we found differences in the relative importance of QOL on variation in utility among the various subgroups. While QOL was not an important correlate of utility among men generally (Fig. 2a), among Hispanic men, work life appeared to be an important correlate of utility, contributing 12 % of the marginal variation above demographic factors and BMI (Fig. 2b); for every ten-unit increase in score on the work-life subscale, utility increased significantly by 0.028 (Table 2). Among women, we found that social stigma and sex life were the two most important QOL domains contributing to disutility (Fig. 2c); both were statistically significant correlates (Table 2). This was especially the case for Caucasian women (accounting for 6 % of variation above and beyond demographics and BMI) (Fig. 2c). In contrast, impaired sexual function was the most important domain among African American women, although it did not quite reach statistical significance (p = 0.06); work life was the most important contributor to disutility among Hispanic women and explained a substantial proportion (more than 20 %) of the marginal variation in utility beyond demographic factors and BMI together (Fig. 2c); for every ten-point increase in subscale score for work function, utilities significantly increased by 0.05 (Table 2). Also interestingly, despite being a summary measure, the overall QOL score did not capture a higher degree of variation in utility than some individual domains.
DISCUSSION
In our study of over 330 primary care patients with moderate to severe obesity, we found that health utilities, or the value patients associate with their current weight and health, did not differ significantly by sex or by race and ethnicity. However, the degree to which QOL and individual QOL domains contributed to disutility or diminished well-being did appear to vary by sex and race/ethnicity. Quality of life factors did not explain much of the variation in utility among men, except for work function among Hispanic men. In contrast, obesity-related social stigma was the most important QOL determinant in obesity’s adverse effect on how Caucasian women patients valued their health. Obesity-related impairment in sexual function was the most important contributor for African American women, and obesity’s adverse impact on work life was the most important factor for Hispanic women. While QOL scores for most individual subscales played only a small role in explaining disutility among non-Hispanic patients, work life explained approximately 20 % of the variation in disutility among Hispanic women. Interestingly, the large contribution of work life was not reflected in the correlation between the overall QOL score reported by Hispanic patients and their health utility.
Prior studies have primarily characterized the QOL associated with obesity using health status measures. Consistent with our study’s findings, previous research suggests that women, Caucasian patients, and those seeking weight treatments tend to report lower QOL scores than their respective counterparts.7,9–12 However, few studies have examined the relative importance of specific QOL domains from the patient’s perspective. In an earlier study of patients seeking bariatric surgery, our group found that social stigma and impairment in work or role functioning were the two most important domains associated with health utility.18 However, whether these findings generalized to unselected primary care patients with obesity or among different demographic subgroups was unclear. Our current study was motivated by these unanswered questions.
A better understanding of the importance of QOL and individual QOL domains from the patient’s perspective is important for a variety of reasons. While clinicians and policy makers tend to focus on medical complications of obesity, evidence suggests that QOL factors may be just as, if not more, important to patients. An earlier analysis of our current study found that overall, QOL scores were a stronger correlate of patients’ health utility than the combination of BMI and comorbidities (manuscript under review). A better understanding of the QOL domains that are most important to patients will help us to better interpret the effectiveness and value of weight control and other obesity interventions in a patient-centered way.
While scores on health status measures can be compared across populations, the scores on individual domains are not necessarily directly comparable to one another. Importantly, our findings confirm this often overlooked concept, where a lower score on one domain does not necessarily portend a worse QOL for the patient than a higher score in another domain. This is because the same scores on two different domains may not have the same meaning to the patient, and may not translate to the same low level of QOL; a low score on one aspect of a patient’s QOL may be more problematic for the patient than a low score on another aspect. In addition, a patient may actually care about one QOL aspect more than another. For example, work life was a substantially more important QOL factor among Hispanic primary care patients with obesity than their Caucasian counterparts, explaining 20 % of the marginal variation in utility among Hispanic women; nevertheless, absolute QOL scores were similar between these two groups. Moreover, the overall QOL score is not a sum of its parts and in many instances, but especially among Hispanics, the overall QOL scores actually contributed less to explaining patients’ disutility or diminished well-being than the most important domain alone. The overall summary score is often an average (sometimes a weighted average, depending on the instrument) of all the subscales. However, it is not always clear that individuals prioritize and weight the importance of each domain the way that researchers might. Hence, summary scores can sometimes be misleading.
Our findings have important implications for how we interpret QOL measures and the importance of delivering patient-centered, preference-based, obesity-related care more effectively. Our findings may also lend some early insight into what is important to patients and the factors that might motivate them to pursue potentially risky weight treatments such as bariatric surgery. Obesity-related stigma is a leading contributor to health utility among Caucasian women in primary care, and may drive their decisions to pursue weight loss treatments. Our results also suggest that management of obesity in our patients may need to include interventions that ameliorate some of the adverse QOL effects associated with obesity, particularly as they relate to social bias, sexual dysfunction, and impairment in role or work function. Finally, our study also shows how little of the variation in a patients’ utility traditional QOL scores actually measure. This finding is not unique to the IWQOL-lite instrument. In earlier work, our group found that the widely used Short-form or SF-36 made similarly modest contributions in explaining the disutility experienced by patients with moderate to severe obesity.19
Our results must be interpreted in the context of the study’s limitations. Study subjects were recruited from primary care practices in Greater Boston and had at least moderate or Class II obesity, and so results may not generalize to all patients with obesity. Secondly, our sample size, particularly for some of our minority subgroups and especially African American men, was modest and we may be underpowered to detect small but clinically meaningful differences across these subgroups. Our results demonstrate associations and we cannot infer a causal link between specific QOL domains and low health utility, nor can we assume that improvements in these domains would necessarily improve patients’ utility. Finally, our results are influenced by how QOL domains were measured. One domain can appear more important than another domain if the latter is not as well-measured as the first.
In summary, the relative importance of different obesity-related QOL factors in adversely affecting patients’ well-being varies by sex and race/ethnicity. Obesity-related social stigma has important adverse effects on how Caucasian women patients devalue their health and weight, whereas impaired work function is especially important among Hispanic patients with obesity. Scores on traditional health status measures may be misleading in that lower scores in one domain do not always translate into a greater adverse impact for patients. Moreover, the overall QOL score may be less important than the scores on the domains most important to patients. Our findings suggest that we need to re-examine how QOL is assessed and interpreted in research studies. Clinicians may need to consider QOL in a more nuanced way when assessing the impact of obesity on their patients.
Acknowledgements
This study was funded by the National Institute of Diabetes, Digestive and Kidney Diseases (R01 DK073302, PI Wee). Dr. Wee is also supported by an NIH midcareer mentorship award (K24DK087932). The sponsor had no role in the design or conduct of the study; the collection, management, analysis, and interpretation of the data, and the preparation, review or approval of the manuscript. Dr. Wee conceived the research question, designed the study, obtained funding, supervised the conduct of the study and drafted the manuscript. Ms. Chiodi and Ms. Huskey had full access to all the data, conducted all analyses, and take responsibility for the integrity of the data and accuracy of the data analysis. Dr. Davis provided statistical expertise, and along with Drs. Hamel and Wee, interpreted the data. All authors provided critical revision of the manuscript for intellectual content and approved the final manuscript. We thank the patients for participating in our study.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
REFERENCES
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults—The Evidence Report. National Institutes of Health. Obes Res. 1998; 6 Suppl 2:51S-209S. [PubMed]
- 3.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 4.Resnick HE, Valsania P, Halter JB, Lin X. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care. 1998;21:1828–1835. doi: 10.2337/diacare.21.11.1828. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J. Impact of age on associations between weight and mortality. Nutr Rev. 2000;58:129–137. doi: 10.1111/j.1753-4887.2000.tb01847.x. [DOI] [PubMed] [Google Scholar]
- 6.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 7.White MA, O'Neil PM, Kolotkin RL, Byrne TK. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes Res. 2004;12:949–955. doi: 10.1038/oby.2004.116. [DOI] [PubMed] [Google Scholar]
- 8.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100:1019–1028. doi: 10.2105/AJPH.2009.159491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001;9:102–111. doi: 10.1038/oby.2001.13. [DOI] [PubMed] [Google Scholar]
- 10.Kolotkin RL, Head S, Hamilton M, Tse CK. Assessing Impact of Weight on Quality of Life. Obes Res. 1995;3:49–56. doi: 10.1002/j.1550-8528.1995.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 11.Wadden TA, Phelan S. Assessment of quality of life in obese individuals. Obes Res. 2002;10(Suppl 1):50S–57S. doi: 10.1038/oby.2002.190. [DOI] [PubMed] [Google Scholar]
- 12.Wee CC, Davis RB, Hamel MB. Comparing the SF-12 and SF-36 health status questionnaires in patients with and without obesity. Health Qual Life Outcome. 2008;6:11. doi: 10.1186/1477-7525-6-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell LB, Gold MR, Siegel JE, Daniels N, Weinstein MC. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–1177. doi: 10.1001/jama.1996.03540140060028. [DOI] [PubMed] [Google Scholar]
- 14.Wee CC, Huskey KW, Bolcic-Jankovic D, Colten ME, Davis RB, Hamel M. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014;29:68–75. doi: 10.1007/s11606-013-2603-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wee CC, Jones DB, Davis RB, Bourland AC, Hamel MB. Understanding patients' value of weight loss and expectations for bariatric surgery. Obes Surg. 2006;16:496–500. doi: 10.1381/096089206776327260. [DOI] [PubMed] [Google Scholar]
- 16.Wee CC, Hamel MB, Davis RB, Phillips RS. Assessing the value of weight loss among primary care patients. J Gen Intern Med. 2004;19:1206–1211. doi: 10.1111/j.1525-1497.2004.40063.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The standard of living in the United States. Science, 1890. 16(396): 131–133. [DOI] [PubMed]
- 19.Wee CC, Davis RB, Huskey KW, Jones DB, Hamel MB. Quality of life among obese patients seeking weight loss surgery: the role of obesity-related social stigma and functional status. J Gen Intern Med. 2013;28:231–238. doi: 10.1007/s11606-012-2188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]