Abstract
Background
Adequate physical activity promotes physical and mental health and decreases obesity risk. However, most adolescents do not attain recommended physical activity levels and effective interventions are lacking. Physical activity trials rarely incorporate built environment use patterns.
Purpose
This paper describes the design and rationale of the Children’s Use of the Built Environment (CUBE) Study, an office-based intervention designed to teach youth how to use their surrounding built environment to increase physical activity.
Methods
CUBE is a 6-month intervention trial among 60 overweight and obese 10-16 year old adolescents from a community health center in Massachusetts. The study began in the winter of 2013. Patients are sequentially assigned to either the intervention or control group. Baseline physical activity by accelerometry and location by GPS, along with measured height, weight, and blood pressure are collected. Control subjects receive standard of care lifestyle counseling. Intervention subjects receive tailored recommendations on how to increase their physical activity based on their accelerometer and GPS data. Data collections are repeated at end-of-treatment, and again 3 months later.
Conclusion
The findings from this study should help guide future efforts to design interventions aimed at increasing adolescent physical activity as well as to inform design professionals and government officials charged with creating outdoor spaces where adolescents spend time.
Keywords: Physical Activity, Built Environment, Adolescents, Obesity, Intervention
Introduction and Background
Nearly one third of US adolescents are overweight or obese,1 with insufficient physical activity along with dietary factors known contributors. Current national physical activity guidelines recommend that children and adolescents obtain 60 minutes of moderate-to-vigorous physical activity (MVPA) a day,2 yet few adolescents achieve these recommendations.3,4 A recent systematic review and meta-analysis of childhood and adolescent physical activity interventions found that physical activity interventions have had only small effects, resulting on average in only a four minute increase in daily walking or running.5 The built environment is known to be associated with adolescent physical activity,6-8 but much of the science base describing the interplay between the built environment and physical activity and obesity risk relies on cross-sectional data. To date, no trials have tested the potential of teaching adolescents how to use their surrounding built environment to increase their physical activity.
The CUBE study will determine the feasibility and potential impact of using the built environment, compared to standard of care, to increase adolescent physical activity. We hypothesize that providing adolescents with personalized feedback on the locations of their physical activity along with individually tailored instruction on how to use the built environment to increase daily activity will increase adolescent physical activity. The primary outcome is to increase daily moderate-to-vigorous physical activity, the secondary outcome is to increase the percent of adolescents achieving the recommended 60 minutes of daily MVPA. The results of this study have the potential to offer novel approaches for increasing daily physical activity and decreasing obesity risk in youth. In this paper we report the design and rationale for the CUBE study.
Methods
Theoretical Framework
The CUBE intervention is informed by two theoretical frameworks, the health belief model and ecological theory. The Health Belief Model (HBM) was developed to identify, explain, and predict health behaviors, and has been widely used to help develop messages aimed at promoting healthy decisions, including engaging in physical activity.9,10 The HBM focuses on identifying personal factors influencing health behaviors, and can be adapted to the built environment (see Table). Guided by the HBM, we use maps which detail a subject’s surrounding built environment and physical activity patterns to assess an adolescent’s knowledge, attitudes, and beliefs on physical activity, and seek to find ways along with the adolescent to maximize physical activity by promoting use of the built environment. The ecological model of health behavior,11 as adapted for active living by Sallis et al., offers a more comprehensive model based on ecological theory that acknowledges the impact that macro-level environmental components can have on health, and specifically identifies the relationship between the individual and his/her surrounding physical environment.12 The ecological model of health behavior posits that interventions seeking to increase physical activity must focus on multiple levels beyond the individual. To increase physical activity, this intervention engages and leverages multiple levels associated with behavior change, including the individual, the family, the healthcare organization, and the surrounding neighborhood.
Table.
Application of Health Belief Model to the CUBE Study and Accompanying Behavior Change Techniques
| Concept | Use of the Built Environment to Promote Physical Activity |
|---|---|
| 1. Perceived Susceptibility | Youth believe they are at risk for weight gain and developing health problems from lack of exercise. Technique: counseling. |
| 2. Perceived Severity | Youth believe the consequences of gaining weight and developing health problems are significant enough to try to avoid. Technique: counseling. |
| 3. Perceived Benefits | Youth believe that the recommendation to increase physical activity by using the built environment can protect them from gaining weight and developing health problems. Technique: counseling, family support, goal setting, importance of setting for physical activity. |
| 4. Perceived Barriers | Youth identify their personal barriers to physical activity and active use of the built environment (i.e., unaware of locations of favorable built environments), and explore ways to reduce or eliminate these barriers (i.e., instructed on the location of local built environments that foster physical activity). Technique: counseling, family support, goal setting. |
| 5. Cues to Action | Youth receive personally tailored recommendations from pediatrician’s office and reminder cues in the form of reminder messages. Technique: counseling, goal setting, reminders, incentives. |
| 6. Self-Efficacy | Youth confident in their ability to use the built environment to be physically active. Technique: counseling, feedback on performance, goal setting, reminders, incentives. |
While both diet and physical activity are important for weight control, youth are able to more fully be in control of physical activity decisions. Although adolescence represents an age of increasing autonomy, adolescents continue to rely on adults for purchase and provision of food at home and in school. In contrast, decisions about using the surrounding publically available built environment for physical activity can be made primarily by the individual adolescent. We therefore designed a study which provides both dietary and physical activity recommendations to adolescents but focuses primarily on physical activity, testing a novel approach to obesity treatment where the locus of control resides in the adolescent.
Participants and Recruitment
Patients followed at an academic outpatient community health center in Massachusetts and who resided in surrounding low- and middle-income towns within the greater metropolitan Boston area, are invited to participate in the study. Eligibility criteria include being 10-16 years old, being overweight or obese by age- and sex-specific body mass index (BMI) percentile (≥85th percentile), and having no health limitations restricting ambulation. This age group was chosen because it represents an age range where youth are capable of making independent physical activity choices but are not yet old enough to drive. All eligible patients are identified via electronic health record on the day prior to their scheduled health center visit, and approached and invited to participate on the appointment day by study staff. Flyers are installed around the health center to raise awareness of the study, and eligible adolescents hearing of the study by word of mouth are also allowed to participate. This study is approved by the Partners HealthCare institutional review board and the protocol is registered on ClinicalTrials.gov (NCT 01939405). Written informed consent is obtained from parents or guardians along with child assent.
Study Design
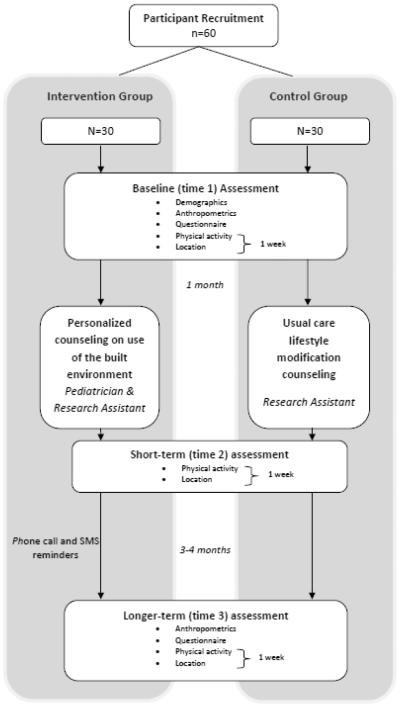
The CUBE study is a prospective intervention trial that will test the feasibility of increasing youth physical activity by encouraging adolescents to actively engage their surrounding built environment. Subjects are sequentially assigned in a 1:1 fashion to either the intervention or control group upon enrollment. Given the substantial variation in temperature over the year in Massachusetts and the known variations in physical activity which occur by season with marked decreases during colder months,6 a sequential assignment study design was employed to achieve an even distribution of subjects in each group by weather and temperature, an outcome which might not have been assured had we used a traditional randomization approach. Time 1 measurements occur at study enrollment, and began in October 2013, with a recruitment period of one year. Time 2 measurements occur approximately one month after time 1, and time 3 measurements are obtained approximately three to four months after time 2, the exact follow-up schedules depending on school vacations. The intervention is delivered at time 2 prior to data collection. Figure 1 represents a timeline of the study design.
Figure 1.
Study timeline for the CUBE intervention.
Study Variables, Measures, and Data Collection
Using the data sources enumerated below, this study will compare change over time between the intervention and control groups in physical activity level and BMI. The primary outcome is change in MVPA (minutes per day). The secondary outcome is change in percent of adolescents achieving the recommended 60 minutes of daily MVPA.
Demographic data: All study participants complete a questionnaire at enrollment with self-reported information on age, gender, race/ethnicity, home address, school, and parent-reported highest level of education.
Built environment knowledge: Self-reported beliefs, attitudes and knowledge about health, physical activity, and the built environment, along with perceived self-efficacy of using the built environment for physical activity are collected using questionnaires at enrollment and time 3. Built environment items were adapted from the validated “Active Where? Study”.13
Anthropometric data: Height and weight are measured by trained research staff at time 1 and time 3 using a stadiometer (SECA, HANOVER, MD) and a digital scale (LifeSource MD; A&E Engineering, Inc., San Jose, CA), with participants wearing indoor clothing, pockets emptied, and shores removed. Measurements are taken in duplicate then averaged. BMI is calculated using age- and sex-specific CDC growth curves.14
Physical activity data: To obtain MVPA and sedentary time, participants are asked to wear the GT3x accelerometer (ActiGraph LLC, Ft Walton Beach, FL) on a belt over the hip during waking hours for 7 days each at times 1, 2, and 3. The GT3x is a tri-axial accelerometer that measures acceleration in three planes, vertical acceleration data are used for these physical activity analyses. Physical activity data are recorded every 30 seconds.15 A thirty second epoch has been used in prior studies collecting combined GPS-accelerometer data and allows for a reasonable approximation of physical activity in adolescents while limiting the large data return that comes with collecting data over one week.7,15,16 A valid day is defined as ≥4 hours (240 minutes) of wear time, with non-wear periods defined as >60 minutes of consecutive zeros with a spike tolerance of 2 minutes, consistent with prior studies using combined GPS and accelerometer data.17-19 A valid dataset includes ≥3 days of valid data. Data collected between the hours of 12:00am and 5:00am are considered sleep time and removed prior to analyses.20 Age-specific thresholds are used to classify accelerometer data, with sedentary activity defined as <100 counts per minute and MVPA ≥2296 counts per minute.21,22 Total minutes above the MVPA threshold, divided by the number of valid days, is used to calculate daily minutes of MVPA for each subject. Daily minutes of sedentary time is similarly calculated by dividing total minutes below the sedentary threshold by the number of valid days for each subject.
Location data: Location is measured by GPS times 1, 2, and 3 and mapped using geographic information systems. Participants are asked to wear the QStarz BT-100XT GPS receiver on a belt alongside the accelerometer. Location data are set to record every 30 seconds.
Accelerometer and GPS data are manually reviewed upon equipment return by study personnel to ensure adequate data capture and compliance. Participants without sufficient data return are asked to repeat the data collection period.
Activity and location data are merged by date/time stamp using the Personal Activity and Location Measurement System (PALMS), an encrypted web-based software program for merging and processing accelerometer and GPS data (http://ucsd-palms-project.wikispaces.com/).23 Merged data are collapsed into one minute epochs and then classified by physical activity intensity, with MVPA and sedentary time categories retained for further analyses. As the purpose of the intervention is to test for changes in physical activity, motorized activity (> 25 km/h) is removed prior to analyses. To determine location, merged data are then entered into ArcGIS and hierarchically assigned a land-use category (home, school, playground or park, streets and sidewalks, other) based on previously observed adolescent physical activity patterns, as previously described.6 Daily minutes of MVPA and sedentary time are calculated for each land-use category.
Intervention
Prior to designing the intervention, we reviewed the literature on pediatric and adolescent physical activity and obesity studies to identify successful interventions. Several concepts and approaches were identified as successful in promoting physical activity and achieving weight loss through lifestyle modifications, including: family support, physician involvement, goal setting with realistic goals, use of incentives, the importance of setting for physical activity, physical activity as fun, regular reminders, and encouraging the reduction of non-academic sedentary behaviors.24-27 We also reviewed the relevant built environment literature describing associations between the built environment and physical activity and obesity in adolescents, including the importance of parks, playgrounds, street connectivity, sidewalks, traffic, and safety. From these literatures, we developed a ‘best practices’ obesity intervention that targets the built environment to promote physical activity in adolescents.
We conducted six focus groups (n=38) prior to the intervention to identify barriers and facilitators to engaging and maintaining physical activity. Adolescents were recruited by direct contact at a community health center and at a community youth center, by flyer, and by word of mouth. Adolescents aged 11-15 years who were overweight or obese and who resided in the study towns were eligible for participation. Informed parental consent and adolescent assent were obtained; all participants received $25 as remuneration. Working off a discussion guide containing questions on physical activity, the built environment, and health counseling, open-ended questions with prompts and follow-up probes were used to collect qualitative data. Two study team members (NMO, AIR) separately reviewed the focus group notes and transcripts and identified common themes. Factors that would promote physical activity included involvement of other family members, no cost, and locations that could be accessed close to home or school. Important barriers to physical activity were concerns about peer stigmatization and safety concerns. Based on this information, we modified our initial intervention concept, paying special attention to identifying free activities located within subject’s surrounding home and school environments, focusing on activities identified by or approved by the participant, and formulating an intervention that incorporated accompanying family members. After finalizing the intervention, we began recruiting adolescents for the study.
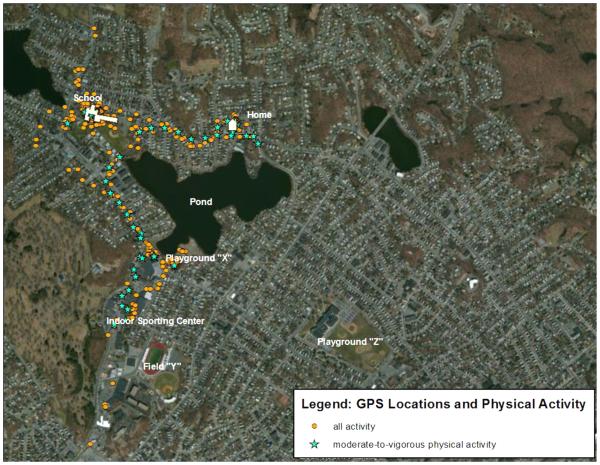
The CUBE intervention aims to increase the opportunity and likelihood that adolescents will achieve the nationally recommended sixty minutes of MVPA a day by following the recommendation that pediatric obesity care counseling incorporate use of the built environment to achieve these physical activity goals (figure 2).28,29 At time 2, intervention subjects meet with a team that is led by a pediatrician and includes a research assistant. During the thirty minute team meeting, subjects are told their mean daily MVPA, and receive standard of care counseling on lifestyle modifications - which includes spoken and printed information on eating a healthful diet, increasing physical activity, reducing screen time, and obtaining sufficient sleep, along with personalized recommendations developed in consultation with the patient and family on using the built environment to increase physical activity. These personalized recommendations are based on a subject’s geo-referenced physical activity data collected during time 1, with the data pictorially displayed on color printed paper maps which are reviewed with and then provided to the participant and the accompanying family (figure 3). Parents and family are encouraged to be present at time 2 and time 3 meetings, based on focus group feedback which highlighted family as a motivator for engaging in physical activity. The mapped data are used to review the subject’s current physical activity locations and to identify new neighborhood opportunities for physical activity. Along with family input, the participant and pediatrician discuss and agree upon a new physical activity goal, which the subject aims to do two to three times per week and which involves a new use of the surrounding built environment (walking to school, playing in a local park or playground, a new family walking route, taking a lap around the block prior to going home after school). Intervention subjects receive regular reminders after their time 2 meeting on their agreed-upon built environment goals and overall physical activity goals by phone call or text message. Intervention subjects also receive a physical-activity promoting gift valued under $5 (bouncing ball, juggling balls, jumping rope, badminton set) at time 2 along with financial incentives ($5 to the subject, $10 to the family) for meeting the agreed upon activity goal, based on operative learning theory applied in prior physical activity and obesity interventions which have shown incentives to help subjects successfully meet their target goals.24,30 Intervention subjects also compete for a reward valued at several hundred dollars for the subject with the greatest increase in daily MVPA over the course of the study. At time 3, the pediatrician-led team meets one last time with intervention subjects and their accompanying family to inform subjects of their time 2 daily MVPA and to again briefly review the subject’s personal built environment goals. In all, the total “dose” of the intervention includes two team meetings, 15-20 reminders, up to 2 financial incentives totaling up to $25, one small gift, and one potential grand prize.
Figure 2.
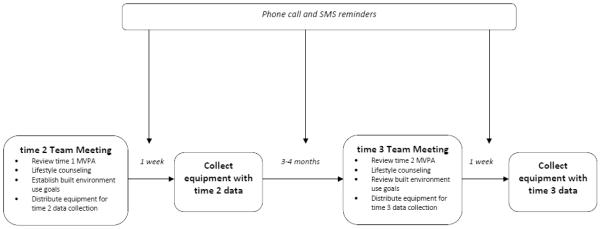
CUBE intervention.
Figure 3.
Example of a physical activity map provided to intervention subjects showing the subject’s combined GPS and accelerometer data.
Subjects assigned to the control group follow a similar study timeline as subjects in the intervention group, coming in for data collection visits at times 2 and 3. During these visits, control subjects meet with a research assistant and receive their mean daily MVPA values along with standard of care counseling on lifestyle modifications for overweight and obesity, including spoken and printed information on eating a healthful diet, increasing physical activity, reducing screen time, and obtaining sufficient sleep.
Analysis Plan
Descriptive statistics will report the study sample by study group assignment and baseline characteristics. Study feasibility will be assessed by reporting recruitment and retention statistics. For the primary outcome, change in mean daily minutes of MVPA, we will conduct ANCOVA analyses to adjust for covariates as groups are not randomized following the intention-to-treat principle. Monte Carlo Markov chain algorithms will be used to impute missing data.31 We will assess short-term change in MVPA from time 1 to time 2 as well as longer term change from time 1 to time 3. For the secondary outcome, McNemar’s test will be used to compare the percent of subjects in each group meeting the recommended 60 minutes of MVPA a day after the intervention, at time 2 and at time 3. The study will also assess for change in BMI among the control and intervention subjects, although this study is not powered to detect weight differences, and we do not anticipate seeing any differences in this outcome measure. A significance level of p<0.05 will be set a priori for all statistical tests. All analyses will be performed using SAS software (SAS Institute, Inc, Cary NC).
A power analysis was performed to identify the appropriate sample size for a power of 0.80 and alpha level of 0.05. Based on the results of prior physical activity interventions,5 we anticipate requiring a sample size of 50 to provide sufficient power to detect a mean daily difference of 8 minutes of MVPA. Given an anticipated drop-out rate of 20%, 60 subjects will be recruited.
Discussion
The CUBE study offers a novel approach to increasing adolescent physical activity by leveraging the built environment, an existing infrastructure available in some form to every adolescent. The study seeks to determine whether teaching youth to use their surrounding built environment can increase physical activity. By learning how to interact with their specific built environments during youth, adolescents may develop and sustain lifelong healthy practices in their ongoing weight management efforts.
Most data on the association between the built environment and physical activity and obesity have been cross-sectional. This study will test whether an existing use pattern can be analyzed and then modified to promote optimal physical activity within that built environment. While study participants will not be randomized to account for seasonal effects, and the potential for selection bias exists, multivariable model analyses will adjust for individual level characteristics. Obesity is exceedingly difficult to treat once established. Recent evidence indicates that studies that combine multiple modalities to promote weight loss, including, shared goal setting, feedback on performance, written instructions and visual materials, subject incentives and prizes, family involvement, and frequent reminders, have a higher likelihood of successfully achieving obesity-related outcomes.24-27 We accordingly use a best practices approach in our obesity intervention, employing multiple strategies to encourage participant adherence and retention and maximize interest in the study among intervention subjects. Providing financial incentives may make it difficult to differentiate any improvement resulting from the intervention from that resulting from financial incentives. Given the known difficulties in increasing physical activity in youth, we believe it is necessary to use a best practices approach and build upon proven successful obesity study methods, which includes the use of financial incentives, and combine this with novel counseling on built environment use in order to maximize the adoption of health promoting behavior change by adolescents. We supplement best practices approaches by incorporating health behavior strategies that encourage promoters and seek to overcome barriers to physical activity identified by adolescents during formative work, thus increasing the relevance and acceptability of the intervention among the targeted youth.
A unique aspect and strength of this study is that it does not require creating, implementing, or funding any specific or de novo physical activity curriculum or program. Rather, it simply leverages the hidden potential of the existing physical infrastructure and counsels on it use. Pediatricians are accustomed to counseling on physical activity, and routinely in accordance with national obesity guidelines.28,29 Teaching youth to use the built environment to increase their daily physical activity has several substantial advantages and benefits. First, it provides the opportunity for daily physical activity by finding opportunities for activity which can be accomplished every day and can be built into daily routines (eg, active commuting to school, taking the stairs at school, using the nearby park after school) without requiring advanced planning or scheduling (eg, finding time to go to the gym). Second, the approach is universal, something which can be adopted by all children and adolescents, regardless of race, ethnicity, or geographic origin, as everybody has a surrounding built environment. Third, it is a free or low-cost activity for youth, and does not require membership or equipment fees. Finally, it helps youth build lifelong healthy habits by teaching them how to use their surrounding environments to lead healthier lives. Such lifelong health skills are especially important to obese children and adolescents, who have an increased likelihood of being obese as adults.32
Conclusion
This study will identify the impact of CUBE, an intervention designed to teach adolescents how to use the built environment to increase their physical activity. This study builds on the strong foundation of literature which demonstrates an association between the built environment and physical activity and obesity. The results of this intervention will identify novel ways to increase physical activity by teaching overweight and obese adolescents important new life skills – how to leverage the surrounding environment for lifestyle modifications and weight control.
Acknowledgements
The authors wish to thank the CUBE study participants and the Massachusetts General Hospital Revere HealthCare Center staff for their participation and cooperation. This trial is sponsored by the National Institutes of Health/National Heart, Lung, and Blood Institute grant #5K23HL103841.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the united states, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.U.S. Department of Health and Human Services 2008 physical activity guidelines for americans. 2008.
- 3.Nader PR, Bradley RH, Houts RM, McRitchie SL, O'Brien M. Moderate-to-vigorous physical activity from ages 9 to 15 years. JAMA. 2008;300(3):295–305. doi: 10.1001/jama.300.3.295. [DOI] [PubMed] [Google Scholar]
- 4.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the united states measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 5.Metcalf B, Henley W, Wilkin T. Effectiveness of intervention on physical activity of children: Systematic review and meta-analysis of controlled trials with objectively measured outcomes (EarlyBird 54) BMJ. 2012;345:e5888. doi: 10.1136/bmj.e5888. [DOI] [PubMed] [Google Scholar]
- 6.Oreskovic NM, Blossom J, Field AE, Chiang SR, Winickoff JP, Kleinman RE. Combining global positioning system and accelerometer data to determine the locations of physical activity in children. Geospat Health. 2012;6(2):263–272. doi: 10.4081/gh.2012.144. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez DA, Cho GH, Evenson KR, et al. Out and about: Association of the built environment with physical activity behaviors of adolescent females. Health Place. 2012;18(1):55–62. doi: 10.1016/j.healthplace.2011.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jago R, Baranowski T, Baranowski JC. Observed, GIS, and self-reported environmental features and adolescent physical activity. Am J Health Promot. 2006;20(6):422–428. doi: 10.4278/0890-1171-20.6.422. [DOI] [PubMed] [Google Scholar]
- 9.Becker MH. The health belief model and personal health behavior. Health Education Monographs. 1974;2:324–473. [Google Scholar]
- 10.Glanz K, Rimer BK, Lewis FM. Health behavior and health education: Theory, research, and practice. 3rd Wiley & Sons; San Francisco: 2002. [Google Scholar]
- 11.Bronfenbrenner U. Ecological models of human development. In: Elsevier, editor. International encyclopedia of education. 2nd Vol. 3. Oxford: 1994. pp. 37–43. [Google Scholar]
- 12.Sallis JF, Cervero RB, Ascher W, Henderson KA, Kraft MK, Kerr J. An ecological approach to creating active living communities. Annu Rev Public Health. 2006;27:297–322. doi: 10.1146/annurev.publhealth.27.021405.102100. [DOI] [PubMed] [Google Scholar]
- 13.Grow HM, Saelens BE, Kerr J, Durant NH, Norman GJ, Sallis JF. Where are youth active? roles of proximity, active transport, and built environment. Med Sci Sports Exerc. 2008;40(12):2071–2079. doi: 10.1249/MSS.0b013e3181817baa. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health and Human Services A SAS program for the CDC growth charts. http://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/sas.htm. Updated 2005. Accessed November, 2006.
- 15.Treuth MS, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 16.Rainham DG, Bates CJ, Blanchard CM, Dummer TJ, Kirk SF, Shearer CL. Spatial classification of youth physical activity patterns. Am J Prev Med. 2012;42(5):e87–96. doi: 10.1016/j.amepre.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 17.Jerrett M, Almanza E, Davies M, et al. Smart growth community design and physical activity in children. Am J Prev Med. 2013;45(4):386–392. doi: 10.1016/j.amepre.2013.05.010. [DOI] [PubMed] [Google Scholar]
- 18.Cooper AR, Page AS, Wheeler BW, Hillsdon M, Griew P, Jago R. Patterns of GPS measured time outdoors after school and objective physical activity in english children: The PEACH project. Int J Behav Nutr Phys Act. 2010;7:31. doi: 10.1186/1479-5868-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lachowycz K, Jones AP, Page AS, Wheeler BW, Cooper AR. What can global positioning systems tell us about the contribution of different types of urban greenspace to children's physical activity? Health Place. 2012;18(3):586–594. doi: 10.1016/j.healthplace.2012.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oreskovic NM, Goodman E, Robinson AI, Perrin EM, Perrin JM. Adolescent report of lifestyle counseling. Child Obes. 2014;10(2):107–113. doi: 10.1089/chi.2013.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- 22.Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–1368. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- 23.Kerr J, Norman GJ, Godbole S, Raab F, Demchak B, Patrick K. Validating GPS data with the PALMS system to detect different active transportation modes. Med Sci Sports Exerc. 2012;44(5S):S25–S29. [Google Scholar]
- 24.Finkelstein EA, Tan YT, Malhotra R, Lee CF, Goh SS, Saw SM. A cluster randomized controlled trial of an incentive-based outdoor physical activity program. J Pediatr. 2013;163(1):167–72. doi: 10.1016/j.jpeds.2013.01.009. e1. [DOI] [PubMed] [Google Scholar]
- 25.Alberga AS, Medd ER, Adamo KB, et al. Top 10 practical lessons learned from physical activity interventions in overweight and obese children and adolescents. Appl Physiol Nutr Metab. 2013;38(3):249–258. doi: 10.1139/apnm-2012-0227. [DOI] [PubMed] [Google Scholar]
- 26.Lison JF, Real-Montes JM, Torro I, et al. Exercise intervention in childhood obesity: A randomized controlled trial comparing hospital-versus home-based groups. Acad Pediatr. 2012;12(4):319–325. doi: 10.1016/j.acap.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 27.DeBar LL, Stevens VJ, Perrin N, et al. A primary care-based, multicomponent lifestyle intervention for overweight adolescent females. Pediatrics. 2012;129(3):e611–20. doi: 10.1542/peds.2011-0863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barlow SE, Expert Committee Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120(Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 29.Committee on Environmental Health The built environment: Designing communities to promote physical activity in children. Pediatrics. 2009;123(6):1591–1598. doi: 10.1542/peds.2009-0750. [DOI] [PubMed] [Google Scholar]
- 30.John LK, Loewenstein G, Troxel AB, Norton L, Fassbender JE, Volpp KG. Financial incentives for extended weight loss: A randomized, = controlled trial. J Gen Intern Med. 2011;26(6):621–626. doi: 10.1007/s11606-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan Y. Multiple imputation for missing data: Concepts and new development, version 9.0. 2000 Web site. http://support.sas.com/rnd/app/papers/abstracts/multipleimputation.html. Accessed June 23, 2010.
- 32.Freedman DS, Khan LK, Serdula MK, Dietz WH, Srinivasan SR, Berenson GS. The relation of childhood BMI to adult adiposity: The bogalusa heart study. Pediatrics. 2005;115(1):22–27. doi: 10.1542/peds.2004-0220. [DOI] [PubMed] [Google Scholar]