Abstract
Preservation of the anterior cruciate ligament (ACL) remnant during ACL reconstruction has the advantages of improved vascularity and synovial encircling of the graft tendon. We describe a technique called single–anteromedial bundle biological augmentation (SAMBBA) using complete preservation of the ACL remnant, as well as preservation of the semitendinosus tibial insertion, that uses standard portals and equipment.
Improved knowledge of the anatomy, biomechanics, and biology of the anterior cruciate ligament (ACL) has increased considerably in the past 10 years. This knowledge has led to a modification of techniques for ACL reconstruction with the emergence of preservation techniques for the ACL remnant. Evidence suggests that preservation of the ACL remnant is beneficial in terms of vascularity and proprioception, which may improve recovery of joint positioning and enhance revascularization and integration of the graft.1-3 With this knowledge, a number of surgeons have pioneered techniques to augment the intact bundle of the ACL, especially in partial tears, with good clinical results. Complete preservation of the ACL remnant has rarely been described because it is technically challenging and because surgeons have to learn to debride the ACL remnant and proceed with a standard ACL reconstruction unhindered by the remnant within the notch.
With the goal of preserving the properties of the ACL remnant and the vascularity of the graft, we describe an ACL reconstruction and preservation technique using a minimally invasive approach. The tibial attachment of the semitendinosus (ST) graft is kept attached to the tibia to prevent avascular necrosis and is passed through the ACL remnant from the tibia to the femur.4 This technique is performed through standard portals without the need for any special equipment.
Surgical Technique
Surgical Setup
The patient is placed in the supine position, with a lateral post just proximal to the knee, at the level of the padded tourniquet, and a foot roll positioned with the knee at 90° of flexion (Video 1, Fig 1, Table 1). This allows the knee to be moved freely through its range of movement while preventing the hip from externally rotating.
Fig 1.
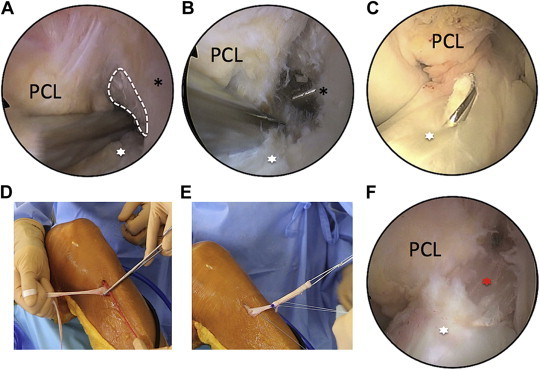
Intraoperative images showing steps during single–anteromedial bundle biological augmentation (SAMBBA) technique in a left knee undergoing ACL reconstruction. (A) Arthroscopic view showing area for minimal notch debridement in anteromedial ACL bundle. (B) Arthroscopic view showing FlipCutter emerging in area of anteromedial bundle. (C) Arthroscopic view showing tibial pin positioned in center of remnant ACL stump. (D) Intraoperative photograph showing use of FiberStick to measure graft length. (E) Intraoperative photograph showing quadrupled ST graft, loaded with TightRope RT, ready for passage into prepared graft tunnel. (F) Arthroscopic view showing final image of ST graft emerging from within ACL remnant toward its femoral socket. The black asterisks indicate the lateral femoral condyle; white asterisks, ACL remnant; white dotted line, area for minimal debridement of anteromedial bundle; and red asterisk, ST graft. (PCL, posterior cruciate ligament.)
Table 1.
Tips and Pearls
| 1. When harvesting the ST tendon, to preserve the tibial insertion, use a right-angled clamp to retract the tendon and cut the 2 expansions before using the stripper. |
| 2. Only debride the proximal notch just enough to visualize the femoral insertion of the ACL. Use a small shaver (4 mm in diameter) for cautious debridement. |
| 3. Use a guide with a ring-shaped target to better visualize the emergence of the guide pin inside the ACL stump. |
| 4. When drilling the tibial tunnel, first reposition the guide pin manually through the tunnel and then push it through the entire length of the ACL remnant before enlarging the tunnel by increasing the drill-bit diameter in 1-mm increments. |
| 5. When drilling to enlarge the tibial tunnel, ensure that the entire tip of the drill has passed through the intra-articular cortex. Using a low speed (revolutions per minute), the ACL remnant should move rhythmically—almost as if samba dancing—as the drill gently turns inside it. |
| 6. Deploy the femoral button under direct vision by placing the arthroscope in the lateral gutter. |
Graft Harvesting
Our chosen graft for the ACL reconstruction is the ST tendon. The goal is to obtain a graft with a diameter of 8 to 10 mm, with a 12-cm length from its tibial insertion. In most cases, this can be achieved with a tripled ST graft. The graft is harvested with an open-ended tendon stripper, allowing the tibial insertion to be preserved, thereby improving fixation and vascularity of the graft.4 Once harvested, the graft is evaluated to determine whether an 8- to 10-mm graft diameter with a 12-cm length can be obtained. This evaluation is performed by tripling or quadrupling the graft over 2 suture loops to determine the drill diameter for the bony tunnel. The ST graft is prepared and looped with TightRope RT (Arthrex, Naples, FL) after drilling the bony tunnels to ensure accuracy of length adjustments.
Femoral Guide Placement
The arthroscope is placed in the lateral gutter, and the best entrance point for the completed femoral tunnel is visualized with a standard needle. A small stab incision in then made at this chosen site. A 4-mm shaver is introduced through the stab incision in the lateral gutter, and the synovial tissue situated between the lateral cortex and the fascia lata is debrided to improve visualization of the button-flipping process over the lateral cortex. The femoral tunnel is prepared with an outside-in femoral guide (Arthrex). A minimal notch debridement is carried out (Fig 1A). The femoral guide is introduced through the anteromedial portal, introduced through the anteromedial portal and inserted at the femoral footprint of the ACL. The sleeve of the guide is then pushed through the stab incision at the chosen entrance point in the lateral gutter. A 20-mm femoral socket is created with a FlipCutter II device (Arthrex) with the size determined by the diameter of the graft (Fig 1B).
Tibial Tunnel Placement and Drilling
With the knee at 30° of flexion, the tibial ACL remnant is inspected. If fixed to the posterior cruciate ligament or a nonanatomic site on the femoral condyle, it is carefully mobilized, preserving its entire synovial cover and tibial attachment. The tibial guide is introduced through the anteromedial portal and positioned so that the guidewire either splits or stays within the center of the ACL tibial stump (Fig 1C). When the location of the guidewire is satisfactory, the tunnel is drilled with increasing drill-bit diameters, stopping as soon as the bone of the tibial plateau is breached. The drill remains strictly within the ACL remnant to conserve residual tissue. A shaver is passed through the tibial tunnel and into the remnant to emerge at its upper end so that the remnant is hollowed out for passage of the graft. The interior of the synovial sleeve is debrided to avoid overpacking of the intercondylar notch, which may cause anterior tissue impingement and an extension deficit.
Graft Length Measurement and Graft Preparation
Accurate graft length measurement is required to be able to tension the graft from its tibial insertion to the bottom of the femoral socket; the prepared graft should be slightly shorter than this distance. A FiberStick (Arthrex) is passed through the femoral and tibial sockets to measure this distance. The proximal tip of the FiberStick is blocked at the proximal margin of the femoral socket, and a forceps is clamped onto the FiberStick at the level of the graft's tibial insertion (Fig 2). The length between the forceps and the proximal margin of the FiberStick is equal to the distance between the graft's tibial insertion and the proximal end of the femoral socket (Fig 1D).
Fig 2.
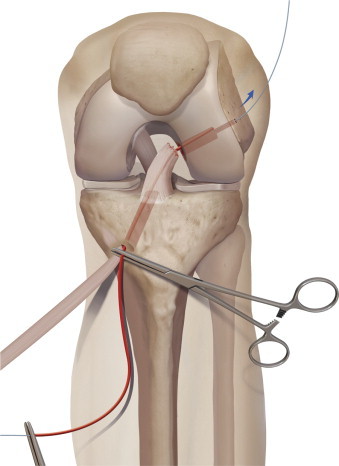
Measurement of graft length. A FiberStick is passed through the path of the graft to measure the distance between the graft's tibial insertion and the proximal margin of the femoral socket.
The graft is prepared with a length 5 mm shorter than the aforementioned distance to obtain adequate graft tensioning (Fig 3). A marking pen is used (Fig 3A) to mark the previously measured graft length minus 0.5 cm. For example, if the graft length is 12.5 cm, a pen mark is placed 12 cm from the ST tibial insertion. A second pen mark is placed 4 cm from the tibial insertion to obtain a minimum length of 8 cm for the tripled or quadrupled graft portion. The graft is then doubled (Fig 3B), tripled (Fig 3C), and possibly quadrupled (Fig 3D) over a TightRope RT between these 2 pen marks, and the looped graft is sutured to itself (Figs 1E and 3E).
Fig 3.
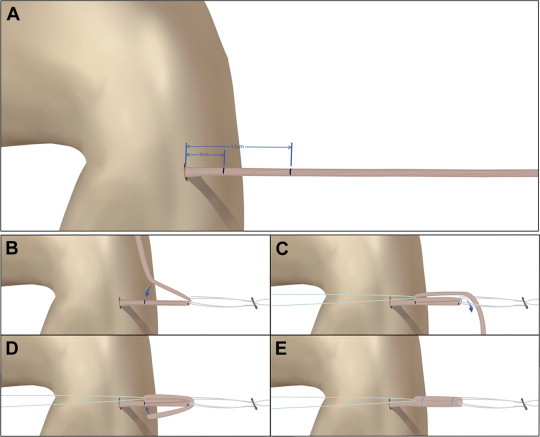
Steps in preparation of ST graft. (A) Pen marks are placed at the previously measured graft length, minus 0.5 cm, and at a point closer to the tibial insertion of the ST tendon to obtain a minimum graft length of 8 cm for the tripled or quadrupled graft portion. The graft is (B) doubled, (C) then tripled, and (D) finally (if required), quadrupled over a TightRope RT between these 2 pen marks. (E) The looped graft is sutured to itself.
Graft Passage
Leaving the knee at 90° of flexion, the surgeon then passes the graft from the tibia to the femur (Fig 1F). Introducing the arthroscope into the lateral gutter of the knee joint allows visualization of the exit point of the button on the lateral cortex of the femur and control of the passage of the TightRope button through the pin hole. The graft is secured on the femoral side with the TightRope tensioning device. The remaining segment of the tibial graft is completed with screw fixation in the standard fashion.
ACL reconstruction techniques with preservation of remnant tissues have been described previously; nevertheless, our technique exhibits some specificities:
-
•
The tibial attachment of the ST graft is kept attached to the tibia to reduce the risk of avascular necrosis.
-
•
The use of an outside-in technique for the femoral socket allows femoral tunnel placement with minimal notch debridement.
-
•
The retrograde drilling process enables the creation of a femoral socket rather than a transcondylar femoral tunnel, which further preserves bone stock.
-
•
The ST graft is placed inside the ACL remnant, which includes blood vessels, neural elements, and competent fibroblasts (Fig 4.)
Fig 4.
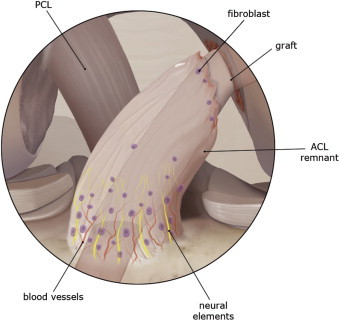
ST graft within ACL remnant, which includes blood vessels, neural elements, and competent fibroblasts. (PCL, posterior cruciate ligament.)
Discussion
Biologically, the ACL remnants have the capacity to improve the ligamentization of the graft,5 and preservation of the synovial sheath seems to play an important role in its vascularization.6 Matsumoto et al.7 noted that the area around the ACL septum contains a population of vascular-derived stem cells that may contribute to ligament regeneration and repair at the rupture site. In a canine model, they elucidated that transplantation of ACL-ruptured tissue contributed to early tendon-bone healing.1 Mifune et al.2 showed an increase in cellularity and angiogenesis and significantly higher biomechanical strength in the augmentation group compared with conventionally reconstructed grafts in a rat model. In a recent comparative study, Takazawa et al.3 showed significantly better postoperative anterior stability and a decreased graft rupture rate in the group in which the ACL remnant was preserved. It seems logical for surgeons to consider preserving the ACL remnant in an attempt to optimize the mechanical and biological outcome. Completing the femoral tunnel with an outside-in FlipCutter II permits retention of the remnant even with minimal notch debridement as opposed to the inside-out technique, which requires a major debridement to visualize the femoral insertion of the ACL and risks notch damage when reaming. Drilling the tibial tunnel with increasing drill-bit diameters and using a 4-mm shaver passed into the ACL remnant facilitate preservation of residual ACL tissue.
In a rabbit model, the ST autograft, which is harvested without detachment of its tibial insertion, was shown to retain its viability.4 In our opinion, retaining the tibial insertion of the ST autograft preserves its viability and bypasses the stages of avascular necrosis and revascularization that occur with the use of a free tendon autograft. To preserve the tibial insertion of the ST, use of an open-ended tendon stripper is mandatory. Using the described length measurement technique ensures a graft of 10 to 12 mm in diameter with a tripled or quadrupled ST tendon and preserves the gracilis tendon.
No comparative study has shown inferior results with the remnant-preservation technique for either stability, synovial coverage, or proprioception,8 either with or without the double-bundle technique.9 Concerns exist regarding an increased risk of impingement after ACL reconstruction with remnant preservation. Most reported cases have used the augmentation technique10 or double-bundle reconstruction.11 With our technique, specific attention is paid to avoid notch overstuffing. Once the graft is secured, it lies within the intact ACL stump with good circular synovial coverage. We have found that in acute ACL tears, the tibial remnant is very soft and can slip down to the tibial insertion of the graft, causing soft-tissue impingement with the intercondylar notch. In these rare cases, the synovial sheath is secured to the proximal part of the graft by a single resorbable stitch. We believe that this technique of ACL reconstruction, which preserves the remnant of the torn ACL, is both reliable and tissue preserving, and the technique uses the native graft vascularity to improve the healing process.
Footnotes
The authors report the following potential conflict of interest or source of funding: B.S-C. and M.T. receive support from Arthrex.
Supplementary Data
Technique of ACL reconstruction with single–anteromedial bundle biological augmentation (SAMBBA), which preserves both the ACL remnant and the ST tibial insertion and uses standard portals and equipment.
References
- 1.Matsumoto T., Kubo S., Sasaki K. Acceleration of tendon-bone healing of anterior cruciate ligament graft using autologous ruptured tissue. Am J Sports Med. 2012;40:1296–1302. doi: 10.1177/0363546512439026. [DOI] [PubMed] [Google Scholar]
- 2.Mifune Y., Ota S., Takayama K. Therapeutic advantage in selective ligament augmentation for partial tears of the anterior cruciate ligament: Results in an animal model. Am J Sports Med. 2013;41:365–373. doi: 10.1177/0363546512471614. [DOI] [PubMed] [Google Scholar]
- 3.Takazawa Y, Ikeda H, Kawasaki T, et al. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med in press, available online 27 September, 2013. doi:10.1177/2325967113505076. [DOI] [PMC free article] [PubMed]
- 4.Papachristou G., Nikolaou V., Efstathopoulos N. ACL reconstruction with semitendinosus tendon autograft without detachment of its tibial insertion: A histologic study in a rabbit model. Knee Surg Sports Traumatol Arthrosc. 2007;15:1175–1180. doi: 10.1007/s00167-007-0374-0. [DOI] [PubMed] [Google Scholar]
- 5.Zaffagnini S., De Pasquale V., Marchesini Reggiani L. Neoligamentization process of BTPB used for ACL graft: Histological evaluation from 6 months to 10 years. Knee. 2007;14:87–93. doi: 10.1016/j.knee.2006.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Gohil S., Annear P.O., Breidahl W. Anterior cruciate ligament reconstruction using autologous double hamstrings: A comparison of standard versus minimal debridement techniques using MRI to assess revascularisation. A randomised prospective study with a one-year follow-up. J Bone Joint Surg Br. 2007;89:1165–1171. doi: 10.1302/0301-620X.89B9.19339. [DOI] [PubMed] [Google Scholar]
- 7.Matsumoto T., Ingham S.M., Mifune Y. Isolation and characterization of human anterior cruciate ligament-derived vascular stem cells. Stem Cells Dev. 2012;21:859–872. doi: 10.1089/scd.2010.0528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hong L., Li X., Zhang H. Anterior cruciate ligament reconstruction with remnant preservation: A prospective, randomized controlled study. Am J Sports Med. 2012;40:2747–2755. doi: 10.1177/0363546512461481. [DOI] [PubMed] [Google Scholar]
- 9.Park S.Y., Oh H., Park S.W., Lee J.H., Lee S.H., Yoon K.H. Clinical outcomes of remnant-preserving augmentation versus double-bundle reconstruction in the anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:1833–1841. doi: 10.1016/j.arthro.2012.05.886. [DOI] [PubMed] [Google Scholar]
- 10.Ahn J.H., Wang J.H., Lee Y.S., Kim J.G., Kang J.H., Koh K.H. Anterior cruciate ligament reconstruction using remnant preservation and a femoral tensioning technique: Clinical and magnetic resonance imaging results. Arthroscopy. 2011;27:1079–1089. doi: 10.1016/j.arthro.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Sonnery-Cottet B., Lavoie F., Ogassawara R. Clinical and operative characteristics of cyclops syndrome after double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:1483–1488. doi: 10.1016/j.arthro.2010.02.034. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique of ACL reconstruction with single–anteromedial bundle biological augmentation (SAMBBA), which preserves both the ACL remnant and the ST tibial insertion and uses standard portals and equipment.


