Abstract
Giant-cell arteritis (GCA) is a systemic autoimmune disease affecting primarily the elderly. Giant cell arteritis can cause sudden and potentially bilateral sequential vision loss in the elderly. Therefore, it is considered a medical emergency in ophthalmology and a significant cause of morbidity in an increasingly aging population. Ophthalmologists need to be able to recognize the classic symptoms and signs of this disease, and then be able to work-up and treat these patients in an efficient manner. An in-depth review of GCA from the literature as well as personal clinical experience follows.
Keywords: Giant cell arteritis, Temporal arteritis, Cranial arteritis, Granulomatous arteritis, Arteritic ischemic optic neuropathy
Introduction
Giant cell arteritis (GCA), also known as temporal or cranial or granulomatous arteritis, is a systemic autoimmune disease affecting primarily the elderly. It is characterized by granulomatous inflammation of the large and medium-sized arteries. GCA is most prevalent in the white population of European origin. There is an association with HLA-DR4 and HLA-DRB1 which suggests a genetic predisposition.1 Most patients affected are over the age of 60 years. The mean age is 70 years old. Women are affected more often. The incidence can be as high as 27 cases in 100,000 people aged greater than 50 years old. With the rapidly growing proportion of older persons in most developed countries, the incidence of GCA will most likely increase.2
Permanent visual loss has been reported to occur in as high as 15–20% of these patients,3 making early and correct diagnosis critical.4 Several attempts, such as the American College of Rheumatology (ACR) criteria,1 have been made to diagnosis GCA without temporal artery biopsy. However, Murchison et al. found that the use of ACR criteria alone could miss up to 25% of GCA diagnoses.5 Thus, temporal artery biopsy remains the diagnostic gold standard for GCA.
The symptoms of giant cell arteritis can overlap with its cousin disease polymyalgia rheumatica (PMR). PMR similarly is an autoimmune disease that affects the elderly. Its hallmark symptoms include muscle pain and weakness affecting the large muscle groups especially in the hips and shoulders. Patients with PMR have trouble getting out of a chair and reaching for objects in cupboards. PMR symptoms also include low-grade fever, malaise, poor appetite, and weight loss. When symptoms affect the neck and higher, giant cell arteritis can be at work. Five to 15% of PMR patients will be diagnosed with giant cell arteritis, and 50% of giant cell arteritis patients have PMR symptoms.
The medium-sized extracranial arteries are most frequently affected clinically in GCA. However, occasionally, the aorta and its branches to the arms and neck or elsewhere are involved.1
Systemic symptoms
The classic systemic symptoms of GCA include headache, scalp tenderness, and jaw claudication. Headache especially located at the temples is the most common symptom. Jaw claudication is the most specific symptom. It is important to remember that jaw claudication means pain with chewing. This symptom is not constant jaw pain. Patients develop a significant jaw ache while chewing, so they decrease their food intake and thereby lose weight and feel weak. A good way to ask about scalp tenderness is to ask whether combing or brushing the hair hurts the scalp. Infrequently, a patient may notice an inflamed artery on the scalp or temple and tell his or her doctor that it is tender leading to the diagnosis. GCA patients may also suffer from ear pain and neck pain. Again they may share the symptoms of PMR with intermittent low-grade fever, weight loss, malaise, and joint/muscle pain.
Visual symptoms
Sudden, severe, and sequential vision loss is the hallmark of giant cell arteritis. The vision loss is usually discovered upon awakening in the morning. Visual acuity is usually less than 20/200 in greater than 60% of patients who lose vision. The fellow eye usually gets involved within days to weeks of the initial eye. In addition to causing a sudden permanent vision loss, GCA can present weeks earlier with amaurosis fugax or a temporary loss of vision which is due to partial occlusion of the short posterior ciliary arteries or central retinal artery causing transient ischemia. GCA may initially also present with diplopia or eye pain.6 Cranial nerve palsies (3, 4, or 6) or ischemic myopathy may rarely occur. This reinforces the point that any elderly patient presenting to the eye clinic with visual symptoms or eye pain should be considered to be a GCA suspect until proven otherwise. This mode of thinking will help minimize permanent vision loss in GCA patients.
AION in GCA
Sudden vision loss in GCA occurs most often due to an inflammatory thrombosis of the short posterior ciliary arteries. The short posterior ciliary arteries form a fine vascular network that supplies the optic disk. When these vessels become thrombosed with inflammation, a stroke to the optic disk occurs. This is called anterior ischemic optic neuropathy or AION (Fig. 1). AION is characterized by a swollen optic disk accompanied by hemorrhages and sometimes exudates. The swollen optic disk may have a chalky white appearance in GCA. This pallid swelling (Fig. 2) is due to the extreme ischemia of GCA. Rarely, the ischemia to the optic nerve occurs posteriorly, and therefore there is no disk swelling. In this instance, it is called posterior ischemic optic neuropathy or PION.
Figure 1.
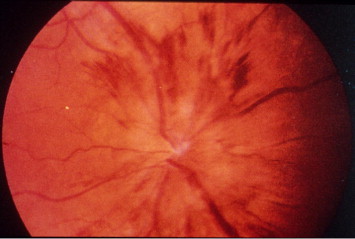
Anterior ischemic optic neuropathy (AION) is characterized by a swollen optic disk accompanied by hemorrhages.
Figure 2.
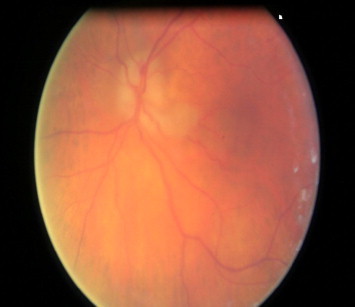
The pallid disk swelling may have a chalky white appearance in GCA.
GCA may also sometimes cause a central retinal artery occlusion (CRAO). About 5% of patients over age 50 with CRAO have GCA. A classic cherry red spot in the macula occurs, but no cholesterol or calcific embolus will be seen since again this is due to an inflammatory thrombosis. GCA may also rarely cause a cilio-retinal artery occlusion or ocular ischemic syndrome. The ocular ischemic syndrome is characterized by eye pain, iritis, and hypotony.
About 5–10% of anterior ischemic optic neuropathy (AION) cases over the age of 60 are due to giant cell arteritis. The other 90–95% are due to garden-variety non-arteritic ischemic optic neuropathy (NAION). The risk factors for NAION include the disk-at-risk appearance of the optic disk (cup-to-disk ratio < 0.1), nocturnal hypotension (taking blood pressure medicines at night), sleep apnea, uncontrolled hypertension, diabetes, and tobacco abuse.
Bilateral involvement of anterior ischemic optic neuropathy in temporal arteritis is not uncommon. In untreated cases, it occurs 54–95% of the time. Cotton wool spots may also be seen in the retina and indicate concurrent retinal ischemia. Fluorescein angiography (FA) may be helpful to identify choroidal hypoperfusion and aid in the timely diagnosis of GCA.7
Laboratory diagnosis
The two most important labs to order to help make the diagnosis of GCA are the Erythrocyte Sedimentation Rate (ESR) and the C-Reactive Protein (CRP). These two lab values, if elevated, indicate systemic inflammation. If either blood value is high, this may point you to a diagnosis of GCA, but one must remember that the ESR and/or CRP may be elevated from other causes of systemic inflammation like infection, malignancy, Diabetes, or other auto-immune diseases like Lupus or Rheumatoid arthritis. Top normal for ESR in men can be calculated by Age divided by 2, women (Age + 10) divided by 2.8 This rule may disagree with normal values from individual laboratories but tends to be more correct.
The combination of ESR and CRP is 97% specific for the diagnosis of GCA according to Hayreh et al.9 In Dr. Hayreh’s study, the CRP was 100% sensitive for detection of GCA. The ESR was 92% sensitive. The mean ESR value in GCA cases in this study was 70 mm/h. However, the ESR can be normal in up to 16% of cases. Parikh et al. reported a sensitivity of 99% when ESR and CRP were used together.10 Only 1 of their 119 biopsy-proven GCA patients (0.8%) had normal ESR and CRP. Two patients (1.7%) had a normal CRP with an elevated ESR.
Thrombocytosis or increased platelets is also a sign of active inflammation in the body, so it is wise to order a complete blood count (CBC) at the same time as ESR and CRP to help cinch the diagnosis. Elevated platelet counts and CRP can be more sensitive inflammatory markers than ESR.2,11 Also ordering the CBC is important to check for anemia, since the ESR tends to rise with anemia.
Occult GCA
There is an entity called occult giant cell arteritis which occurs about 20% of the time. In this special form of GCA, there is an absence of the systemic symptoms listed above. It is defined as ocular involvement by GCA without any systemic symptoms or signs. Hayreh et al. published a prospective study in 1998 which included 85 patients with a positive temporal artery biopsy and ocular involvement. Eighteen of these 85 patients or 21% had occult GCA.12 The ESR and CRP lab values in this occult group were significantly lower than the rest of the patients however the results were still abnormal. In this occult GCA group, 17 of the 18 patients or 94% had anterior ischemic optic neuropathy, while 2 of the 18 patients or 11% had central retinal artery occlusion. A normal ESR or CRP may not rule out GCA nor does a lack of systemic symptoms. The physician must watch out for early massive visual loss (counting fingers vision or worse), sequential vision loss within days or weeks, and chalky white disk edema.
Management
The management of a suspected GCA patient must be done quickly because there is a risk of permanent sequential vision loss (blindness) if treatment is delayed. This is why giant cell arteritis is the number one medico-legal entity in ophthalmology in the developed world. The physician must carefully review the three aspects of the patient’s clinical presentation: history, examination, and lab results. You suspect that the patient may have giant cell arteritis due to the history: he or she admits to headaches at the temples, scalp tenderness, neck pain, malaise, weight loss, low-grade fever, and/or jaw claudication. Your ophthalmic examination is consistent with GCA: Swollen or chalky white disk, CRAO, cotton wool spots in the retina, choroidal hypoperfusion on FA, and/or tender temporal artery. Lastly, stat ESR or CRP or both are elevated on the lab review.
A good rule of thumb is if 2 out of the 3 above parameters are positive, treatment and temporal artery biopsy must follow. The temporal artery biopsy is considered the gold standard in diagnosis. But do not wait for the results of the temporal artery biopsy before treating the patient. You must begin high-dose steroids immediately. Oral prednisone should be started at a dose of 1 milligram/kilogram per day. Try to have prednisone tablets available in your office or clinic to give to the patient to start immediately; if not, the patient may develop blindness before they have their prescription filled. If in your judgment, you believe the patient is too ill to go home, it is always a good idea to admit the patient to the hospital for IV Solu-Medrol 250 milligrams every 6 h for 3–5 days followed by high dose prednisone. The patient should remain on high dose steroids until the temporal artery biopsy results are completed. If you believe that there is a low suspicion of GCA, 40 milligrams of prednisone daily is a good dose to keep patients on till the biopsy is completed. The temporal artery biopsy should be scheduled within 1–2 weeks. After this period of time, it is more difficult to diagnose GCA in the pathologic specimen due to the steroid’s influence in removing the inflammation from the artery.13 Although there are other clues in the artery specimen that may indicate GCA. These signs include the presence of fibrosis in the artery wall and fragmentation or loss of the internal elastic lamina (healed arteritis).
High-dose steroid therapy is usually effective in preventing further visual loss. A few eyes may demonstrate visual deterioration during the first 5 days of treatment, and, conversely, a few eyes may show a mild improvement in visual acuity with high-dose corticosteroids.14,15 However, for the most part, the vision loss is permanent. There is no evidence that intravenous high dose steroids are more effective than oral steroids in halting visual deterioration.16
The physician must discuss with the patient and his or her family about the risks of prednisone use. Side effects include stomach upset due to acid reflux, increased appetite and weight gain, osteoporosis leading to fractures with falls, increased blood sugars in diabetics and blood pressure, increased anxiety, and poor sleep. Long-term, high-dose glucocorticoid treatment is not benign and can result in the development of serious adverse effects including stomach ulcers, glaucoma, cataracts, bone avascular necrosis, myopathy, and heightened risk for infection. Over-the-counter acid blockers like ranitidine should be recommended while taking prednisone to protect the stomach. The prednisone dose should be taken in the morning to minimize its side effects of poor sleep. As you can see, prednisone can have marked side-effects; that is why a positive temporal artery biopsy is needed to support the continued use of long-term steroids in these elderly patients.17
When the patient returns for the temporal artery biopsy, the physician should ask the patient whether the prednisone helped the GCA symptoms. If the classic GCA symptoms improved on prednisone, this would correlate well with the diagnosis of GCA. If the opposite is true, and the patient’s symptoms of headache, scalp tenderness, and jaw claudication did not improve with prednisone, this finding would go against the diagnosis of GCA, even before the biopsy was done.
The temporal artery biopsy can be performed by a variety of surgeons, including ophthalmologists, ENT specialists, general surgeons, and plastic surgeons. It can be done in a minor procedure room under local anesthesia or in the operating room. It usually takes less than one hour. Pathologic specimens should be 2–3 cm long because of the occurrence of skip lesions (discontinuous arterial involvement) in GCA. False negative results can occur in 3–9%. A contralateral biopsy should be considered after a negative initial biopsy if clinical suspicion is high for GCA.
It is wise to mark out the course of the superficial temporal artery with a marking pen while the patient is seated upright before subcutaneous anesthesia is infiltrated. Also, the biopsy should be taken on the side of the head which has more symptoms. Palpate the pulse of the temporal artery with your fingers or use a Doppler ultrasound. Start at least 2 fingerbreadths above the lateral canthus of the eye. This will decrease your risk of cutting the facial nerve which travels with the temporal artery in front of the ear. Other risks of this surgical procedure include bleeding, bruising, infection, scalp necrosis, and the possibility of having to repeat the procedure on the other side.
After being formally diagnosed with GCA via a positive temporal artery biopsy (the gold standard), the high-dose prednisone should be tapered very slowly over about 1 year while monitoring the ESR and CRP lab values periodically. The clinical response should be assessed as well. Alternate day steroid treatment is inadequate for GCA. Although it is expected that the visual prognosis is poor after suffering ischemic optic neuropathy or central retinal artery occlusion, the patient’s non-ocular symptoms such as headache, scalp tenderness, and jaw claudication as well as PMR symptoms such as muscle pains and weakness should all resolve with the prednisone. If prednisone’s side effects and risks outweigh its benefits, a steroid-sparing agent like methotrexate may be used through consultation with rheumatology. Steroid tapering must be slow and careful because there is a risk of recurrent ischemic optic neuropathy in 7% of patients. Recurrent symptoms should prompt re-evaluation.
Pathologic diagnosis
First of all, make sure that your pathologist is familiar with this disease. A telephone call in advance may ensure that the pathologist and ophthalmologist are on the same page concerning the patient. Multiple cross sections of the temporal artery will need to be examined under the microscope due to the occurrence of skip lesions in GCA.
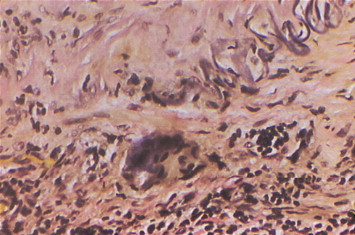
Histopathologically, two patterns are considered diagnostic of giant cell arteritis: those with inflammation of the vessel wall (active arteritis) and those with post-inflammatory alterations (healed arteritis). With active arteritis (Fig. 3) cellular infiltration of the artery wall is seen. The adventitia, media, and intima are thickened with a preponderance of lymphocytes, macrophages, and giant cells. It is important to remember that multi-nucleated giant cells which are a coalescence of macrophages (Fig. 4) do not have to be present in a positive temporal artery biopsy. The primary inciting cause of the inflammation is unknown but may be due to a bacterial or viral antigen. Healed arteritis lacks the active inflammation but will show fibrosis of the vessel wall with disruption of the internal elastic lamina. Elastin stains may be used to highlight a fragmented or disrupted internal elastic lamina (Fig. 5).
Figure 3.
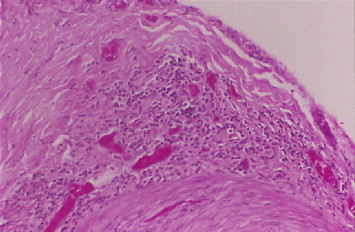
Lymphocytic infiltration of the artery wall is seen in active arteritis.
Figure 4.
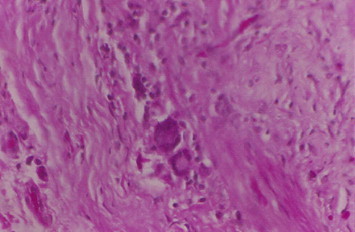
Multinucleated giant cells in a temporal artery biopsy specimen.
Figure 5.
Elastin stain highlights a fragmented or disrupted internal elastic lamina.
Positive biopsies, whether active or healed, are treated the same initially with high dose steroids. Few investigators have examined the differences between these two groups and their outcomes with treatment. Borg et al. found patients with healed arteritis had lower ESR and higher hemoglobin levels, theorizing that those with healed arteritis represented a relatively benign subgroup with milder clinical presentation and a good prognosis.18 Borg et al. suggested that a lower initial dose of prednisone (15 mg/day) may be used for this subgroup compared to the active arteritis subgroup which should begin treatment with an initial dose of prednisone of 40–60 mg/day or higher. Another rheumatology group, Lee et al. found similar results.19 These studies were reported in the rheumatology literature and were focused on the rheumatologic signs and symptoms of GCA.
Imaging
Many studies have compared temporal artery ultrasound findings with histologically proven giant cell arteritis. Ultrasound has the highest resolution of all imaging techniques used for the diagnosis of vasculitis.20 One large meta-analysis by Karassa et al. showed that sensitivity of temporal artery duplex ultrasound was 87% and specificity 96%.21 As the quality of ultrasound technology improves, more centers are becoming experienced with temporal artery ultrasound, and in some cases, are replacing temporal artery biopsy with definitive clinic and ultrasound findings.22
MRA is another modality used to aid in the diagnosis of vasculitis. In one case series of 7 patients with giant cell arteritis, Markl et al. found that 3T high-field MR system had the ability to detect visualization of inflammatory changes in the vessel walls of all patients23; however, this imaging technique is still largely investigational and a protocol to achieve the finest resolution is still being debated.
Conclusion
Giant cell arteritis is a systemic autoimmune disease of the elderly that has potentially devastating visual consequences. Early diagnosis and treatment are critical. This review of GCA hopefully will help ophthalmologists become better acquainted with this disease in order to prevent unnecessary vision loss.
Conflict of interest
The authors declared that there is no conflict of interest.
Acknowledgement
This work was supported in part by Research to Prevent Blindness and the Pat & Willard Walker Eye Research Center.
References
- 1.Hunder G.G., Bloch D.A., Michel B.A. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33(8):1122–1128. doi: 10.1002/art.1780330810. [DOI] [PubMed] [Google Scholar]
- 2.Niederkohr R.D., Levin L.A. Management of the patient with suspected temporal arteritis: a decision-analytic approach. Ophthalmology. 2005;112(5):744–756. doi: 10.1016/j.ophtha.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 3.Evans J.M., Hunder G.G. Polymyalgia rheumatica and giant cell arteritis. Rheum Dis Clin North Am. 2000;26:493–515. doi: 10.1016/s0889-857x(05)70153-8. [DOI] [PubMed] [Google Scholar]
- 4.Aiello P.D., Trautmann J.C., McPhee T.J. Visual prognosis in giant cell arteritis. Ophthalmology. 1993;100:550–555. doi: 10.1016/s0161-6420(93)31608-8. [DOI] [PubMed] [Google Scholar]
- 5.Murchison A.P., Gilbert M.E., Bikyk J.R. Validity of the American college of rheumatology criteria for the diagnosis of giant cell arteritis. Am J Ophthalmol. 2012;154:617–619. doi: 10.1016/j.ajo.2012.03.045. [DOI] [PubMed] [Google Scholar]
- 6.Hayreh S.S., Podhajsky P.A., Zimmerman B. Ocular manifestations of giant cell arteritis. Am J Ophthalmol. 1998;125(4):509–520. doi: 10.1016/s0002-9394(99)80192-5. [DOI] [PubMed] [Google Scholar]
- 7.Slavin M.L., Barondes M.J. Visual loss caused by choroidal ischemia preceding anterior ischemic optic neuropathy in giant cell arteritis. Am J Ophthalmol. 1994;117(1):81–86. doi: 10.1016/s0002-9394(14)73018-1. [DOI] [PubMed] [Google Scholar]
- 8.Miller A., Green M., Robinson D. Simple rule for calculating normal erythrocyte sedimentation rate. BMJ. 1983;286(1):266. doi: 10.1136/bmj.286.6361.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hayreh S.S., Podhajsky P.A., Raman R. Giant cell arteritis: validity and reliability of various diagnostic criteria. Am J Ophthalmol. 1997;123(3):285–296. doi: 10.1016/s0002-9394(14)70123-0. [DOI] [PubMed] [Google Scholar]
- 10.Parikh M., Miller N.R., Lee A.G. Prevalence of a normal c-reactive protein with an elevated erythrocyte sedimentation rate in biopsy-proven giant cell arteritis. Ophthalmology. 2006;113(10):1842–1845. doi: 10.1016/j.ophtha.2006.05.020. [DOI] [PubMed] [Google Scholar]
- 11.Foroozan R., Danesh-Meyer H., Savino P.J. Thrombocytosis in patients with biopsy-proven giant cell arteritis. Ophthalmology. 2007;109:1267–1271. doi: 10.1016/s0161-6420(02)01076-x. [DOI] [PubMed] [Google Scholar]
- 12.Hayreh S.S., Podhajsky P.A., Zimmerman B. Occult giant cell arteritis: ocular manifestations. Am J Opthalmol. 1998;125(4):521–526. doi: 10.1016/s0002-9394(99)80193-7. [DOI] [PubMed] [Google Scholar]
- 13.Deacon B.S., Chacko J.G. Case of the missed opportunity for temporal artery biopsy. J Arkansas Med Soc. 2009;106(4):86–87. [PubMed] [Google Scholar]
- 14.Foroozan R., Deramo V.A., Buono L.M. Recovery of visual function in patients with biopsy-proven giant cell arteritis. Ophthalmology. 2003;110(3):539–542. doi: 10.1016/S0161-6420(02)01775-X. [DOI] [PubMed] [Google Scholar]
- 15.Liu G.T., Glaser J.S., Schatz N.J. Visual morbidity in giant cell arteritis. Ophthalmology. 1994;101(11):1779–1785. doi: 10.1016/s0161-6420(94)31102-x. [DOI] [PubMed] [Google Scholar]
- 16.Hayreh S.S., Zimmerman B. Visual deterioration in giant cell arteritis patients while on high doses of corticosteroid therapy. Ophthalmology. 2003;110(6):1204–1215. doi: 10.1016/S0161-6420(03)00228-8. [DOI] [PubMed] [Google Scholar]
- 17.Danesh-Meyer H.V. Editorial, temporal artery biopsy: skip it at your patient’s peril. Am J Ophthalmol. 2012;154(4):617–619. doi: 10.1016/j.ajo.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 18.Borg E.J., Haanen H.C., Seldenrijk C.A. Relationship between histological subtypes and clinical characteristics at presentation and outcome in biopsy-proven temporal arteritis. Clin Rheumatol. 2007;26 doi: 10.1007/s10067-006-0332-0. 559-532. [DOI] [PubMed] [Google Scholar]
- 19.Lee Y.C., Padera R.F., Noss E.H. Clinical course and management of a consecutive series of patients with “healed temporal arteritis”. J Rheum. 2012;39:295–302. doi: 10.3899/jrheum.110317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schmidt W. Role of ultrasound in the understanding and management of vasculitis. Ther Adv Musculoskelet Dis. 2014;6(2):39–47. doi: 10.1177/1759720X13512256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Karassa F., Matsagas M., Schmidt W., Ioannidis J. Meta-analysis: test performance of ultrasonography for giant-cell arteritis. Ann Internal Med. 2005;142:359–369. doi: 10.7326/0003-4819-142-5-200503010-00011. [DOI] [PubMed] [Google Scholar]
- 22.Schirmer M., Duftner C., Schmidt W., Dejaco C. Ultrasonography in inflammatory rheumatic disease: an overview. Nat Rev Rheumatol. 2011;7:479–488. doi: 10.1038/nrrheum.2011.95. [DOI] [PubMed] [Google Scholar]
- 23.Markl M., Uhl M., Wieben O. High resolution 3T MRI for the assessment of cervical and superficial cranial arteries in giant cell arteritis. J Magn Reson Imaging. 2006;24:423–427. doi: 10.1002/jmri.20639. [DOI] [PubMed] [Google Scholar]


