Abstract
Purpose
To create clinically useful models that incorporate readily available demographic and cancer treatment characteristics to predict individual risk of heart failure among 5-year survivors of childhood cancer.
Patients and Methods
Survivors in the Childhood Cancer Survivor Study (CCSS) free of significant cardiovascular disease 5 years after cancer diagnosis (n = 13,060) were observed through age 40 years for the development of heart failure (ie, requiring medications or heart transplantation or leading to death). Siblings (n = 4,023) established the baseline population risk. An additional 3,421 survivors from Emma Children's Hospital (Amsterdam, the Netherlands), the National Wilms Tumor Study, and the St Jude Lifetime Cohort Study were used to validate the CCSS prediction models.
Results
Heart failure occurred in 285 CCSS participants. Risk scores based on selected exposures (sex, age at cancer diagnosis, and anthracycline and chest radiotherapy doses) achieved an area under the curve of 0.74 and concordance statistic of 0.76 at or through age 40 years. Validation cohort estimates ranged from 0.68 to 0.82. Risk scores were collapsed to form statistically distinct low-, moderate-, and high-risk groups, corresponding to cumulative incidences of heart failure at age 40 years of 0.5% (95% CI, 0.2% to 0.8%), 2.4% (95% CI, 1.8% to 3.0%), and 11.7% (95% CI, 8.8% to 14.5%), respectively. In comparison, siblings had a cumulative incidence of 0.3% (95% CI, 0.1% to 0.5%).
Conclusion
Using information available to clinicians soon after completion of childhood cancer therapy, individual risk for subsequent heart failure can be predicted with reasonable accuracy and discrimination. These validated models provide a framework on which to base future screening strategies and interventions.
INTRODUCTION
There are now more than 400,000 childhood cancer survivors in the United States,1 and cardiovascular disease is increasingly recognized as one of the leading contributors to late morbidity and mortality in this population.2–8 Survivors are at significant risk of cardiomyopathy leading to eventual congestive heart failure (CHF) compared with siblings and the general population, with risk ratios ranging from 5 to 15.3,6,9–12 Important risk factors for CHF include attained age, doses of chest radiotherapy and anthracyclines, presence of conventional cardiovascular risk factors such as hypertension, and, in some studies, age at initial cancer diagnosis and sex.13 Although CHF risk predictors exist for the general older adult population14–16 and have been recently reported for patients with breast cancer,17 given the increased incidence of CHF among adolescent and young adult survivors, this high-risk population may benefit from customized and validated risk prediction models starting at a time point soon after therapy completion, which, to our knowledge, currently do not exist.
Our goal was to use the large Childhood Cancer Survivor Study (CCSS) cohort to create clinically useful models that incorporate demographic and cancer treatment information available at the end of therapy to predict subsequent CHF risk with reasonable discrimination among 5-year survivors and to then validate the resulting risk scores among external cohorts. Importantly, many of the cancer treatments used in these cohorts remain in common use today.18,19 The development of a robust CHF prediction model for this population may help clinicians refine surveillance strategies to better identify and counsel patients at higher risk of future events.
PATIENTS AND METHODS
Primary Study Population
CCSS methodology and participant accrual have been reported previously.20,21 The cohort consists of children (diagnosed before age 21 years) treated for the most common types of childhood cancer at 26 institutions in the United States and Canada between 1970 and 1986 who survived at least 5-years after diagnosis. For our study, the analytic cohort excluded those who did not provide consent for medical record abstraction (n = 1,110) and those who experienced a major cardiovascular event (CHF, myocardial infarct, or stroke) within 5 years of their initial cancer diagnosis (n = 188, including 42 who experienced CHF), leaving 13,060 members of the original cohort (91%) available for analysis. A random sample of siblings served as a comparison population (n = 4,023). The protocol was approved by the human subjects committee at each institution. Participants provided informed consent.
Cancer Therapy Exposures
Chemotherapy, surgery, and radiotherapy information was abstracted from medical records. Anthracycline exposures included doxorubicin, daunorubicin, idarubicin, epirubicin, and mitoxantrone (an anthraquinone). In the primary analysis, anthracycline doses were based on the following doxorubicin hematologic toxicity equivalence: daunorubicin, 1.0; idarubicin, 3.0; epirubicin, 0.67; and mitoxantrone, 4.0.10 Sensitivity analyses considered the effect of alternative doxorubicin toxicity equivalence formulas: daunorubicin, 0.83; and idarubicin, 5.0.22,23
Radiotherapy records were centrally reviewed, and exposures to the neck, chest, and abdomen were categorized as yes versus no (yes if at least part of region was in direct treatment field); field-specific maximum total doses were calculated for the chest and abdomen separately.24 Chest fields included any abdominal treatment that included the lower part of the chest (ie, above diaphragm), as well as treatments directed at the thorax (eg, shoulders, ribs, and/or supraclavicular areas), even if the central chest was not a target. In defining dose-specific exposures for each region, radiation scatter from adjacent fields also was noted, but these exposures were categorized as < 5 Gy. Heart-specific absorbed doses were estimated by applying water phantom measurements to a three-dimensional mathematic phantom allowing simulation of a patient of any age or size.24
Outcome Definitions
CCSS participants completed a baseline questionnaire covering demographic characteristics, health care use, health conditions, and health-related behaviors and were then prospectively observed using periodic questionnaires (available on CCSS Web site25). Proxy responses from family members were used for 5-year survivors who had subsequently died, were age < 18 years, or were unable to complete the questionnaires. The cohort also was linked with the National Death Index to ascertain CHF-related deaths (International Classification of Diseases, ninth revision [ICD-9], codes 425 to 428 and V42.1 or ICD-10 codes I42 to I52). Using previously described methodology to define CHF,3,11 baseline and subsequent questionnaire items related to cardiomyopathy, CHF, and heart transplantation, including information on medications, were classified and graded using the Common Terminology Criteria for Adverse Events (CTCAE; version 4.03).26 Only those outcomes graded as severe (grade 3; self-reported cardiomyopathy or CHF, plus medications), life threatening (grade 4; requiring heart transplantation), or fatal (grade 5) were included. If insufficient information existed to distinguish between grades, the lower grade was applied. Outcomes were limited to those occurring by age 40 years, given the limited number of events beyond that age because of the relative youth of the cohort. Information on obesity, hypertension, dyslipidemia, and diabetes from the baseline questionnaire was defined as previously described.11,27
Statistical Analysis
Exposures selected a priori to be examined in our prediction models included sex, age at diagnosis (5-year increments), anthracyclines, alkylating agents, platinum agents, vinca alkaloids, and neck, chest, and abdominal radiotherapy. For chemotherapy, only cumulative anthracycline doses were categorized (none, < 100, 100 to 249, and ≥ 250 mg/m2), and for radiotherapy, only cumulative chest and heart doses were categorized (none, < 5, 5 to 14, 15 to 34, and ≥ 35 Gy). Three prediction models were created for different clinical scenarios: one, a simple model where cancer therapy–related exposures were categorized as yes or no only; two, a standard model where clinical dose information was known; and three, a standard with heart dose model that used average radiation dose to the heart in lieu of chest field dose because contemporary radiotherapy plans often provide heart-specific dosimetry. Secondary analyses explored the influence of obesity, hypertension, dyslipidemia, and diabetes on the performance of the standard model in a subset of survivors with available data.
Poisson regression models, adjusted for current age, estimated the relationships between selected exposures and CHF. Backward selection then determined the most influential predictors, adjusted for sex and age at diagnosis.28 Regression estimates that remained plus those associated with sex and age at diagnosis were then converted to integer risk scores for ease of summing in subsequent risk models (relative risks < 1.3, 1.3 to 1.9, 2.0 to 2.9, 3.0 to 4.9, and ≥ 5.0 corresponding to risk scores 0, 1, 2, 3, and 4, respectively).29 Cox regression models estimated the discriminatory and predictive power of a model based on the area under the curve (AUC) at age 40 years and the concordance (C) statistic (representing weighted average AUC from study start through age 40 years), with values around 0.5 suggesting a model does no better than chance, and values approaching 1 equating to perfect discrimination and prediction.30,31 Values ≥ 0.7 are considered reasonable, and values ≥ 0.8 are considered excellent. To minimize overfitting, the backward selection process and the C-statistics and AUCs reported were internally cross validated using random subsets of the CCSS cohort.32
Risk scores were then summed to create low-, moderate-, and high-risk groups for CHF based on the absolute (cumulative incidence at age 40 years)33 and relative risks compared with siblings (Poisson regression)34 associated with individual risk scores. The risk groupings were designed such that each group ideally was significantly distinct from both siblings as well as the immediate lower group (P < .05) per our regression models. Additional methodologic details, including software used, can be found in the Appendix (online only).
External Validation
We used several well-annotated childhood cancer populations with information on both therapeutic exposures and CHF occurring ≥ 5 years after cancer diagnosis for validation (Table 1): Emma Children's Hospital and Academic Medical Center (EKZ/AMC),7 the National Wilms Tumor Study (NWTS),35 and the St Jude Lifetime Cohort Study (SJLIFE; cohort and patient cases of CHF defined by minimum ≥ 10-year survivorship).8 In contrast to CCSS, in all three cohorts, CHF was ascertained via medical records if possible, supplemented by death records. Some EKZ/AMC and SJLIFE participants also had prospective clinical assessments. NWTS, similar to CCSS, accepted patient or family self-report if corroborated by concurrent use of appropriate cardiac medications. For each validation group, outcomes were restricted to CTCAE grade ≥ 3 conditions.
Table 1.
Characteristics of Study Cohorts
| Variable | Training Data Set CCSS (n = 13,060) | Validation Data Sets |
||
|---|---|---|---|---|
| EKZ/AMC (n = 1,362) | NWTS (n = 6,760)*† | SJLIFE (n = 1,695)* | ||
| Population | 26 North American centers; diagnosed age < 21 years between 1970 and 1986; survived ≥ 5 years | Single Dutch center; diagnosed age < 18 years between 1966 and 1997; survived ≥ 5 years | North American clinical trials group; kidney tumors only; diagnosed age < 16 years between 1969 and 2002; survived ≥ 5 years | Single US center; diagnosed at any age (if pediatric histology) between 1962 and 2001; alive and age ≥ 18 years at cohort entry; survived > 10 years |
| Exposure information | Chemotherapy doses, RT fields and doses, select organ-specific dosimetry (based on average dose) | Chemotherapy doses, RT fields and doses, select organ-specific dosimetry (maximum and EQD2 doses); chest RT fields defined similarly as CCSS | Chemotherapy doses, RT fields and doses, no organ-specific dosimetry; chest RT included any whole-abdomen or left-flank RT exposure | Chemotherapy doses, RT fields and doses, no organ-specific dosimetry; chest RT fields defined similarly as CCSS |
| Outcome definition | Self-report and death records; limited to CTCAE grades 3 to 5 occurring > 5 years from cancer diagnosis: cardiomyopathy or CHF requiring medication or cardiac transplantation or leading to death (n = 285) | Medical and death records; prospective clinical assessment; limited to CTCAE grades 3 to 5 occurring > 5 years from cancer diagnosis (n = 26) | Medical and death records; self-report accepted if patient also reported receiving appropriate medications; limited to CTCAE grades 3 to 5 occurring > 5 years from cancer diagnosis (n = 48) | Medical and death records; prospective clinical assessment; limited to CTCAE grades 3 to 5 occurring > 10 years from cancer diagnosis (n = 19) |
Abbreviations: CCSS, Childhood Cancer Survivor Study; CHF, congestive heart failure; CTCAE, Common Terminology Criteria for Adverse Events; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; EQD2, equivalent dose in 2-Gy fractions; NWTS, National Wilms Tumor Study; RT, radiotherapy; SJLIFE, St Jude Lifetime Cohort.
CCSS participants who also were part of NWTS and/or SJLIFE were excluded from NWTS and SJLIFE for this analysis.
Because NWTS did not have pre-existing chemotherapy dose information available, a nested case-cohort design was used for this analysis, which included all 48 patient cases of heart failure and 316 randomly selected members of overall cohort (as of December 31, 2012).
C-statistics and AUCs (through or at age 40 years) for CHF were estimated for each validation cohort based on the CCSS risk scores. Each individual in these cohorts was then categorized into the appropriate CCSS-based risk groupings, and the resulting cumulative incidence of CHF was plotted and compared against those derived from the CCSS.
RESULTS
Within the CCSS cohort, 37.3% of individuals received an anthracycline (Table 2; Appendix Table A1, online only), whereas 25.9% received chest radiotherapy, excluding scatter < 5 Gy. The median age at last follow-up among CCSS participants was 32 years (range, 6 to 59 years), and the median duration of follow-up was 19 years (range, 0 to 34 years). Among CCSS siblings (51.9% female), the median age at last follow-up was 34 years (range, 3 to 63 years). Compared with only 12 affected siblings (cumulative incidence, 0.3%; 95% CI, 0.1% to 0.5%), 285 CCSS participants had CHF (cumulative incidence, 2.8%; 95% CI, 2.4% to 3.2%) by age 40 years: 258 individuals receiving medications, 10 with history of heart transplantation, and 17 deaths resulting from CHF.
Table 2.
Demographic and Clinical Characteristics of ≥ 5-Year Childhood Cancer Survivor Cohorts
| Characteristic | Training Data Set CCSS (n = 13,060) |
Validation Data Sets |
||||||
|---|---|---|---|---|---|---|---|---|
| EKZ/AMC (n = 1,362) |
NWTS (n = 364) |
SJLIFE (n = 1,695) |
||||||
| No. | % | No. | % | No. | % | No. | % | |
| Female sex | 6,134 | 47.0 | 617 | 45.3 | 201 | 55.2 | 819 | 48.3 |
| Age at diagnosis, years | ||||||||
| < 5 | 5,251 | 40.2 | 596 | 43.8 | 270 | 74.2 | 553 | 32.6 |
| 5-9 | 2,891 | 22.1 | 378 | 27.8 | 81 | 22.3 | 410 | 24.2 |
| 10-14 | 2,622 | 20.1 | 308 | 22.6 | 10 | 2.7 | 436 | 25.7 |
| ≥ 15 | 2,296 | 17.6 | 80 | 5.9 | 3 | 0.8 | 296 | 17.5 |
| Cancer diagnosis | ||||||||
| Acute lymphoblastic leukemia | 3,987 | 30.5 | 302 | 22.2 | — | — | 482 | 28.4 |
| Other leukemia | 452 | 3.5 | 30 | 2.2 | — | — | 71 | 4.2 |
| Hodgkin lymphoma | 1,756 | 13.4 | 104 | 7.6 | — | — | 203 | 12.0 |
| Other lymphoma | 965 | 7.4 | 167 | 12.3 | — | — | 111 | 6.6 |
| Brain tumor | 1,687 | 12.9 | 124 | 9.1 | — | — | 214 | 12.6 |
| Neuroblastoma | 871 | 6.7 | 85 | 6.2 | — | — | 56 | 3.3 |
| Kidney tumor | 1,130 | 8.7 | 186 | 13.7 | 364 | 100.0 | 97 | 5.7 |
| Soft tissue sarcoma | 1,134 | 8.7 | 131 | 9.6 | — | — | 135 | 7.9 |
| Bone tumor | 1,078 | 8.2 | 126 | 9.3 | — | — | 97 | 5.7 |
| Other neoplasm | — | — | 107 | 7.9 | — | — | 229 | 13.5 |
| Anthracycline use | ||||||||
| Yes | 4,876 | 37.3 | 565 | 41.5 | 185 | 50.8 | 1,003 | 59.2 |
| No | 7,513 | 57.5 | 797 | 58.5 | 179 | 49.2 | 692 | 40.8 |
| Unknown | 671 | 5.1 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Anthracycline dose, mg/m2 | ||||||||
| None | 7,506 | 57.5 | 799 | 58.7 | 179 | 49.2 | 692 | 40.8 |
| < 100 | 422 | 3.2 | 32 | 2.3 | 23 | 6.3 | 218 | 12.9 |
| 100-249 | 1,354 | 10.4 | 263 | 19.3 | 95 | 26.1 | 549 | 32.4 |
| ≥ 250 | 2,584 | 19.8 | 259 | 19.0 | 61 | 16.8 | 231 | 13.6 |
| Unknown | 1,194 | 9.1 | 9 | 0.7 | 6 | 1.6 | 5 | 0.3 |
| Chest RT | ||||||||
| Yes | 3,382 | 25.9 | 217 | 15.9 | 158 | 43.4 | 500 | 29.5 |
| No | 8,783 | 67.3 | 1,092 | 80.2 | 206 | 56.6 | 1,195 | 70.5 |
| Unknown | 895 | 6.9 | 53 | 3.9 | 0 | 0.0 | 0 | 0.0 |
| Chest RT dose, Gy | ||||||||
| None | 7,577 | 58.0 | 825 | 60.6 | 164 | 45.1 | 1,195 | 70.5 |
| < 5 | 1,225 | 9.4 | 267 | 19.6 | 42 | 11.5 | 3 | 0.2 |
| 5-14 | 444 | 3.4 | 25 | 1.8 | 89 | 24.5 | 98 | 5.8 |
| 15-34 | 1,410 | 10.8 | 107 | 7.9 | 44 | 12.1 | 263 | 15.5 |
| ≥ 35 | 1,477 | 11.3 | 75 | 5.5 | 21 | 5.8 | 134 | 7.9 |
| Unknown | 927 | 7.1 | 63 | 4.6 | 4 | 1.1 | 2 | 0.1 |
| Heart RT dose, Gy | ||||||||
| None | 8,104 | 62.1 | 1,096 | 80.5 | ||||
| < 5 | 830 | 6.4 | 1 | 0.1 | ||||
| 5-14 | 853 | 6.5 | 34 | 2.5 | ||||
| 15-34 | 1,389 | 10.6 | 160 | 11.7 | ||||
| ≥ 35 | 930 | 7.1 | 61 | 4.5 | ||||
| Unknown | 954 | 7.3 | 10 | 0.7 | ||||
Abbreviations: CCSS, Childhood Cancer Survivor Study; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; NWTS, National Wilms Tumor Study; RT, radiotherapy; SJLIFE, St Jude Lifetime Cohort.
Poisson regression using backward selection identified the most influential CHF predictors for each model, from which corresponding scoring tables were created (Table 3; Appendix Table A2, online only). Using this approach, alkylating agents, vinca alkaloids, platinum agents, and neck and abdominal radiotherapy did not meet criteria to be included in any of the models. In secondary analyses, if survivors who had received 250 to 299 mg/m2 of anthracyclines were analyzed as a separate dose category, they had risk scores identical to those of survivors who received ≥ 300 mg/m2 (risk score 4), in contrast to those who received < 250 mg/m2 (risk score 3).
Table 3.
CHF Risk Scores and Corresponding Model Discrimination and Predictive Power*
| Characteristic | Simple Model† | Standard Model | Heart Dose Model |
|---|---|---|---|
| Sex | |||
| Male | 0 | 0 | 0 |
| Female | 1 | 1 | 1 |
| Age at diagnosis, years | |||
| < 5 | 1 | 2 | 2 |
| 5-9 | 0 | 1 | 1 |
| 10-14 | 0 | 0 | 1 |
| ≥ 15 | 0 | 0 | 0 |
| Anthracycline, mg/m2 | |||
| None | 0 | 0 | 0 |
| Any | 3 | — | — |
| < 100 | — | 1 | 2 |
| 100-249 | — | 3 | 3 |
| ≥ 250 | — | 4 | 4 |
| Chest or heart RT, Gy‡ | |||
| None | 0 | 0 | 0 |
| Any | 3 | — | — |
| < 5 | — | 0 | 0 |
| 5-14 | — | 2 | 1 |
| 15-34 | — | 2 | 3 |
| ≥ 35 | — | 4 | 4 |
| Cohort | |||
| CCSS (n = 285)§ | |||
| AUC | 0.71 | 0.74 | 0.76 |
| C-statistic | 0.72 | 0.76 | 0.77 |
| EKZ/AMC (n = 26) | |||
| AUC | 0.74 | 0.81 | 0.74 |
| C-statistic | 0.75 | 0.80 | 0.78 |
| NWTS (n = 48) | |||
| AUC | 0.76 | 0.72 | — |
| C-statistic | 0.79 | 0.82 | — |
| SJLIFE (n = 19) | |||
| AUC | 0.63‖ | 0.68 | — |
| C-statistic | 0.63‖ | 0.68‖ | — |
Abbreviations: AUC, area under the curve; C, concordance; CCSS, Childhood Cancer Survivor Study; CHF, congestive heart failure; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; NWTS, National Wilms Tumor Study; RT, radiotherapy; SJLIFE, St Jude Lifetime Cohort.
Risk scores 0, 1, 2, 3, and 4 correspond to relative risks < 1.3, 1.3 to 1.9, 2.0 to 2.9, 3.0 to 4.9, and ≥ 5.0, respectively.
Anthracycline and RT exposures classified as yes versus no only.
Simple model: patients who received only radiation scatter from adjacent fields classified as unexposed; standard model: scatter from adjacent fields classified as < 5 Gy; heart dose model: exposures based on heart-specific dosimetry.
Training data set, with estimates reflecting within CCSS cohort cross-validation.
Estimate is significantly different (P < .05) from corresponding CCSS estimate.
The resulting AUCs and C-statistics for CCSS-derived integer risk scores at or through age 40 years ranged from 0.71 to 0.77, with the standard and heart dose models performing modestly better than the simple model (Table 3). In general, AUCs and C-statistics were comparable, suggesting that estimates were stable at least through age 40 years. Prediction estimates associated with the original regression coefficients were virtually identical to those associated with integer risk scores (within 0.01 for five of six estimates and 0.04 for other estimate). Similarly, application of an alternative anthracycline drug toxicity equivalence formula22 resulted in 1.4% of CCSS participants (n = 181) being reclassified into different (ie, lower) dose categories (Appendix Table A3, online only). However, the AUCs and C-statistics using this alternative formula were virtually identical.
When conventional cardiovascular risk factors were first evaluated by CCSS (n = 10,521; on average, 15 years after cancer diagnosis; median age of 24 years at time of assessment), these conditions were still relatively rare: obesity (12.1%), hypertension (2.8%), diabetes (0.7%), and dyslipidemia (0.2%). Among this subset of the CCSS cohort, obesity and hypertension were found to be independently influential (Appendix Table A4, online only). However, the prior risk scores were otherwise minimally changed, and overall AUC and C-statistic for CHF at or through age 40 years increased only by 0.01. However, by shifting the prediction time point from 5 years after cancer diagnosis to this later time point, the number of available patient cases of CHF decreased from 285 to 182. This illustrates the value of having a prediction model that starts at an earlier time point, given the occurrence of a significant number of CHF events within 5 to 15 years of diagnosis.
Application of CCSS-based risk scores to the external cohorts showed that when compared with the CCSS results, the AUCs and C-statistics were similar when applied to the EKZ/AMC and NWTS cohorts (P > .2 for all comparisons) but lower when applied to SJLIFE (P = .01 to .06; Table 3). When the CCSS cohort was restricted to match SJLIFE more similarly (ie, patients alive at baseline who had survived > 10 years from cancer diagnosis and were age ≥ 18 years), the resulting AUCs and C-statistics were essentially unchanged for CCSS.
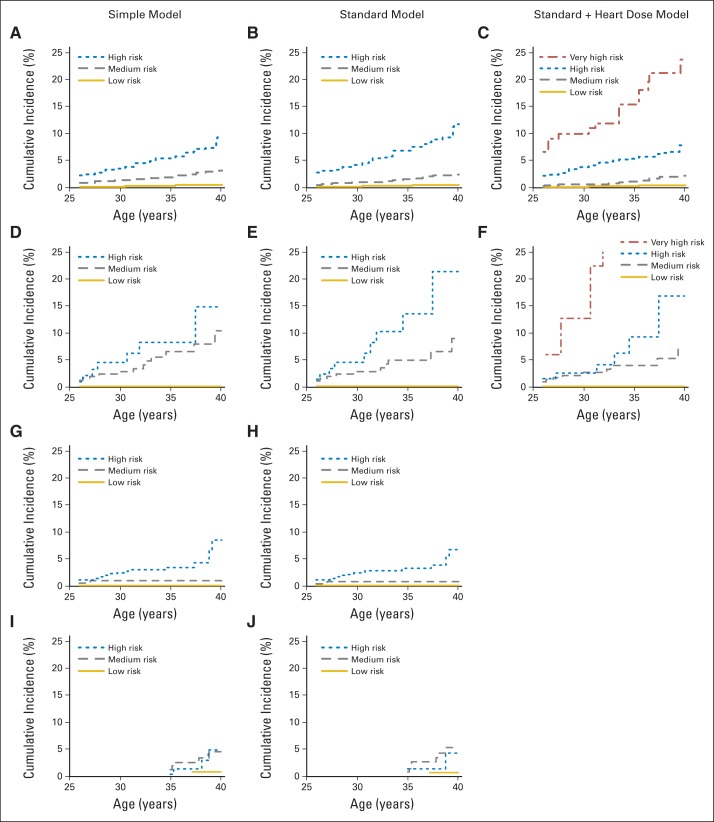
Risk scores were then summed for each individual, and the corresponding absolute and relative risks associated with each risk score value were estimated using rates among siblings as the referent group. Summed risk scores that shared similar relative and absolute risks were then grouped together to form low-, moderate-, and high-risk groups, corresponding to 40-year cumulative incidence rates of < 2.0%, 2.0% to 4.9%, and ≥ 5.0%, respectively (Table 4). For the heart dose model, a fourth, very high–risk group (≥ 15.0%) was also able to be defined. The low-risk groups had minimally increased cumulative incidences and relative risks of CHF compared with siblings (P > .05). For all other comparisons, the relative risks among survivor risk groups were statistically distinct from one another (P < .01). The CCSS risk groupings were able to segregate different groups within the EKZ/AMC and NWTS cohorts, although the SJLIFE moderate- and high-risk groups overlapped (Fig 1; Appendix Tables A5 and A6, online only). Compared with high-risk CCSS survivors, a smaller proportion of high-risk SJLIFE survivors had high anthracycline exposure (≥ 250 mg/m2; 33.8% v 67.6%, respectively; P < .001), which may have contributed to the lower incidence of CHF seen in the high-risk group of that cohort.
Table 4.
Classification of CHF Risk Groups Within CCSS Cohort Based on Summed Risk Scores
| Risk Group | Risk Score | No. of Events | No. of Patients at Risk* | Cumulative Incidence† | 95% CI | RR (v siblings) | 95% CI | RR (v preceding group)‡ | 95% CI |
|---|---|---|---|---|---|---|---|---|---|
| Siblings | — | 12 | 4,023 | 0.3 | 0.1 to 0.5 | 1.0 | Referent | — | — |
| Simple model | |||||||||
| Low | < 3 | 15 | 5,112 | 0.5 | 0.2 to 0.8 | 1.6 | 0.7 to 3.4 | — | — |
| Moderate | 3-4 | 160 | 4,857 | 3.1 | 2.5 to 3.7 | 14.6 | 8.0 to 26.4 | 9.2 | 5.4 to 15.6 |
| High | ≥ 5 | 92 | 2,030 | 9.2 | 6.8 to 11.6 | 33.0 | 18.0 to 60.7 | 2.3 | 1.7 to 3.0 |
| Standard model | |||||||||
| Low | < 3 | 18 | 5,199 | 0.5 | 0.2 to 0.8 | 1.8 | 0.9 to 3.8 | — | — |
| Moderate | 3-5§ | 122 | 4,233 | 2.4 | 1.8 to 3.0 | 12.1 | 6.6 to 22.0 | 6.6 | 4.0 to 10.8 |
| High | ≥ 6 | 108 | 2,059 | 11.7 | 8.8 to 14.5 | 41.5 | 22.7 to 75.9 | 3.4 | 2.6 to 4.5 |
| Heart dose model | |||||||||
| Low | < 3 | 15 | 5,187 | 0.5 | 0.2 to 0.7 | 1.6 | 0.7 to 3.3 | — | — |
| Moderate | 3-5§ | 103 | 3,883 | 2.3 | 1.7 to 2.9 | 11.3 | 6.2 to 20.8 | 7.3 | 4.2 to 12.5 |
| High | 6-8 | 105 | 2,236 | 7.8 | 5.9 to 9.7 | 32.8 | 17.9 to 60.1 | 2.9 | 2.2 to 3.8 |
| Very high | ≥ 9 | 25 | 164 | 23.7 | 14.5 to 32.9 | 118.1 | 58.8 to 236.9 | 3.6 | 2.3 to 5.6 |
Abbreviations: CCSS, Childhood Cancer Survivor Study; CHF, congestive heart failure; RR, relative risk.
No. at risk varies by outcome and model because it excludes individuals with missing data.
At age 40 years.
Comparisons are versus immediate preceding group (eg, moderate- v low-risk group, high- v moderate-risk group).
Survivors with total risk score of 3 under standard (n = 1,129) and heart dose (n = 1,179) models without both anthracycline and chest or heart radiotherapy exposures are classified as low risk; cumulative incidence of CHF at age 40 years among these individuals was 0.2%.
Fig 1.
Cumulative incidence of congestive heart failure by risk group for each study cohort: (A) to (C) Childhood Cancer Survivor Study (training data set), (D) to (F) Emma Children's Hospital (validation set), (G) to (H) National Wilms Tumor Study (validation set), and (I) to (J) St Jude Lifetime Cohort (SJLIFE; validation set). Curves start when all eligible cohort members have entered follow-up (age 26 years, except SJLIFE, which started at age 36 years); as such, initial values shown may be > 0%.
DISCUSSION
Various national groups have published recommendations regarding cardiomyopathy screening for childhood23,36,37 and adult cancer survivors38 based on available evidence and expert opinion. Using treatment and outcome data from one of the largest cohorts of childhood cancer survivors, we take this one step further by developing the CCSS-CHF risk score as an easy-to-use clinical tool that can accurately predict individual CHF risk through age 40 years (Appendix [online only] details how models can be applied to hypothetical patient; online calculator can also be found at the CCSS website38a). The information needed to determine the CCSS-CHF risk score is included in the elements of basic cancer survivorship care plans recommended by the Institute of Medicine.39 Although knowledge of more detailed cancer treatment information such as radiotherapy and anthracycline doses was associated with improved prediction, simple models based on the presence or absence of a given exposure performed well and permitted segregation of survivors into distinct risk groups. Although the CCSS patient cases were primarily defined by self-report and were not clinically ascertained and thus subject to potentially greater misclassification, we showed that these prediction models were robust when applied to several large external validation cohorts. Importantly, these external cohorts relied on medical records and prospective clinical assessment of outcomes, supporting the validity of the CCSS results.3,10,11,27
The CCSS-CHF risk score is designed for patients who have recently completed therapy (5 years after diagnosis; median age of 12 years in our cohort) when conventional cardiovascular risk factors such as hypertension, dyslipidemia, and diabetes are still typically rare. Although our analysis among an older subset of survivors (on average, 15 years after diagnosis) found that some of these conditions can be independent predictors, their contributions were modest because of their relatively low prevalence at the time point assessed. However, most of these conditions, along with CHF and other serious cardiovascular events, have been shown to increase sharply as survivors enter middle age, rising beyond age 40 years without any obvious plateau.5,6,8,11,12,27 Similar to models now being developed for survivors of adult cancers, future models conditioned on more extended survival examining the influence of these conditions in conjunction with cancer treatment exposures among older childhood cancer survivors will be important.17,40
Other refinements in prediction may occur with the inclusion of genetic characteristics pending validation.41–44 Although the mainstays of contemporary pediatric cancer therapy remain similar to the exposures assessed in this study,18,19 if newer agents such as trastuzumab, sorafenib, and sunitinib associated with ventricular dysfunction are increasingly used in pediatrics, future models will need to assess their influence.17,38
The use of continuous dose (v categorical) information may also improve prediction, although such changes may reduce the ease of clinical application, requiring greater bioinformatics support. In our choice of anthracycline dose categories, we chose, based on the CCSS data, a cutoff of 250 mg/m2 to denote the highest exposure category36 rather than the 300-mg/m2 cutoff currently recommended by some groups.23,37 However, the 250-mg/m2 threshold, as well as the 35-Gy chest radiotherapy threshold, we adopted is in concordance with those proposed by an international guideline harmonization group after a systematic review of the current literature.45
What remains unclear is the most appropriate method to convert different anthracycline derivatives to a doxorubicin equivalent dose, with many formulas based on hematologic toxicity, which may differ from cardiotoxicity.22,46 Our analyses with two commonly used formulas revealed similar results. We chose the formula that was less likely to classify individuals as lower risk, with the assumption that any benefits from overscreening would outweigh the risks for this particular outcome.47 Although these formulas do not account for alternative anthracycline formulations (eg, liposomal) and dosing strategies that may be associated with reduced cardiotoxicity (all information that we lacked), the efficacy data for these interventions are limited and mixed in pediatrics.13,48,49 The CCSS treatment era also largely predates the introduction of dexrazoxane as a cardioprotectant (no CCSS patient was recorded as exposed), but even today, dexrazoxane remains in limited pediatric use, with unclear long-term efficacy.13,50
In applying these models, users should be aware that our models are specific to the risk of CHF (ie, CTCAE grade ≥ 3) beginning 5 years after initial cancer diagnosis. Characteristics associated with earlier-onset CHF may possibly differ. Furthermore, the cumulative incidence of subclinical cardiomyopathy is likely greater than our estimates. The EKZ/AMC cohort reported a 27% prevalence of subclinical left ventricular dysfunction (defined as shortening fraction < 30%) among patients with echocardiographic data at an attained age of 23 years (n = 525).7 The overall prevalence of cardiomyopathy (defined as ejection fraction < 50% by echocardiogram) among SJLIFE participants was 6.2%, with 61% having CHF (ie, grade ≥ 3 cardiomyopathy).8 Nevertheless, the predictors we tested are also associated with subclinical cardiomyopathy, and our restriction to a clinical phenotype avoided issues related to variable definitions of subclinical cardiomyopathy used by different studies. Given the poor long-term prognosis associated with CHF, application of our prediction models will still help more clearly identify individual survivors who may benefit from earlier detection and intervention.13
Although there remains a paucity of evidence regarding the optimal screening strategy and the most appropriate intervention should abnormalities be detected,2,38,45 the CCSS-CHF prediction models provide a robust framework for personalized risk assessment. These models may help refine cardiomyopathy surveillance by reducing screening among low-risk survivors while identifying higher-risk individuals who may benefit from closer follow-up. Furthermore, they can serve as a platform to test interventions designed to reduce CHF-related morbidity.
Supplementary Material
Appendix
Application of Prediction Models
An 8-year-old girl who was diagnosed with acute lymphoblastic leukemia at age 3 years is seen for follow-up. As part of her cancer therapy, she received no radiotherapy but received doxorubicin 75 mg/m2 and daunorubicin 100 mg/m2, for a total cumulative anthracycline dose of 175 mg/m2. As noted in the primary text, some doxorubicin equivalence formulas adjust daunorubicin by a factor of 0.83, which would result in a total anthracycline dose of 158 mg/m2 (75 + 83 mg/m2). Conversion formulas for other anthracyclines are presented in the primary text. Her heart failure risk factors based on the standard model (Table 3) would include female sex (1 point), diagnosis at age < 5 years (2 points), anthracycline 100 to 249 mg/m2 (3 points), totaling 6 points and putting her into the high-risk group, with a predicted cumulative incidence of clinical cardiomyopathy or heart failure of approximately 12% by age 40 years (relative risk, approximately 40 v siblings; relative risk, approximately 3 v medium risk group; Table 4). Prediction is similar if the heart dose model is used, although a more refined categorization is available with a separate very high–risk group. If cumulative anthracycline dose information was not available, using the simple model, she would have a total of 5 points (female sex, 1 point; diagnosis at age < 5 years, 1 point; any anthracyclines, 3 points; Table 3) and still be classified as high risk (cumulative incidence of approximately 9% by age 40 years; relative risk, approximately 30 v siblings; Table 4). Because the performance of the standard model at least through age 40 years is superior to that of the simple model (Table 3), we recommend using the richer model (ie, standard or heart dose model) when possible. For convenience, an online calculator is available (The Childhood Cancer Survivor Study: CHF risk calculator. ccss.stjude.org/chfcalc).
Statistical Approach
Model selection.
The following variables were selected a priori for testing in our models: sex, age at diagnosis (5-year increments), and exposure to anthracyclines, alkylating agents, platinum agents, vinca alkaloids, and neck, chest, and abdominal radiotherapy (yes v no). For the standard and heart dose models, exposure doses were substituted for anthracyclines (none, < 100, 100 to 249, and ≥ 250 mg/m2) and chest or heart radiotherapy (none, < 5, 5 to 14, 15 to 34, and ≥ 35 Gy). Individuals with missing data relevant to each model were excluded. Using Poisson regression adjusted for current age as a cubic spline, models were built to examine the relationships between these independent variables and outcome (ie, congestive heart failure [CHF]). Current age was handled by splitting the records at each age (as integer) during follow-up. Backward selection was then used to determine the most influential treatment predictors accounting for sex and age at diagnosis.28 The least significant variable with P ≥ .05 (as determined by likelihood ratio test) was dropped, and the reduced model was refitted using the same rule until all remaining exposure variables were statistically significant (P < .05). To minimize the possibility of overfitting, we performed 10-fold internal cross validation of the variable selection process.32 Exploratory analyses examining potential interaction between therapeutic exposures and sex or age at diagnosis did not reveal any consistent relationships.
Risk score creation.
Regression estimates that remained after backward selection plus those associated with sex and diagnosis age were then converted to integer risk scores for ease of summing in subsequent risk models (relative risks < 1.3, 1.3 to 1.9, 2.0 to 2.9, 3.0 to 4.9, and ≥ 5.0 corresponding to risk scores 0, 1, 2, 3, and 4, respectively) based on previously published methods (Sorror ML et al: Bone Marrow Transplant 46:464-466, 2011).29 Notably, prediction estimates associated with the original regression coefficients were virtually identical to those associated with integer risk scores (within 0.01 for five of six estimates; 0.04 for other estimate).
Risk score discriminatory and predictive power.
Cox regression models based on an age time scale estimated the discriminatory and predictive power of our model.30 Specifically, we examined the area under the curve (AUC) at age 40 years and the concordance (C) statistic through age 40 years.31 The AUC(t) is the probability that a classifier will rank a randomly chosen positive higher than a randomly chosen negative on a given time t. The C(t)-statistic represents the weighted average of the AUC from study start time to time t. Similar to the initial model selection process, the reported AUCs and C-statistics also reflected 10-fold internal cross validation based on random subsets of the Childhood Cancer Survivor Study (CCSS) cohort.32
Risk group creation.
Although other general population predictors are often based on the sum of individual risk scores (McGill HC Jr et al: Circulation 117:1216-1227, 2008),14–16 given the relatively smaller number of patient cases we had available, estimates associated with individual risk scores were not always precise. Therefore, we collapsed risk scores into several risk groups predictive of low, moderate, and high risk of CHF.29 To determine the most appropriate groupings, the sums of individual risk scores were examined based on their absolute risks (cumulative incidence at age 40 years, treating death resulting from other causes as competing risk event33) and relative risks compared with siblings (Poisson regression, incorporating generalized estimating equation modification to account for potential within-family correlation34). The resulting low-, moderate-, and high-risk groups corresponded in general to cumulative incidence rates of < 2.0%, 2.0% to 4.9%, and ≥ 5.0% at age 40 years, respectively. For the heart dose model, a fourth, very high–risk group was also able to be defined, with cumulative incidence ≥ 20%. The risk groupings were designed such that each group ideally would be significantly distinct from both siblings as well as the immediate lower group (P < .05) per our Poisson regression models. However, for our CHF models, the lowest-risk group ended up not being statistically distinct (P > .05) from siblings.
External validation.
C-statistics and AUCs (through or at age 40 years) for CHF were estimated for each of the validation cohorts based on the CCSS risk scores. Each individual in these cohorts was then categorized into the appropriate CCSS-based risk grouping, and the resulting cumulative incidence of CHF was plotted and compared against those derived from the CCSS cohort. Notably, exposure data for the National Wilms Tumor Study (NWTS) were based on a nested case-cohort design (48 patient cases of CHF; 316 randomly selected members of overall cohort [n = 6,760]), in which Barlow's (Barlow WE: Biometrics 50:1064-1072, 1994) weighting method was applied for all estimates (Prentice RL: Biometrics 42:301-310, 1986). This study design was chosen because the NWTS did not have pre-existing chemotherapy dose information, and study resources did not allow for an exhaustive review of the entire cohort. We then assessed the difference of the AUCs and C-statistics of each model between the external cohorts and the CCSS using 1,000 bootstrap iterations (Good PI: New York, NY, Springer, 2005).
Software.
R software (version 3.0; http://www.r-project.org/), specifically the function risksetROC (version 1.0), was used to calculate the AUCs and C-statistics. SAS software (version 9.3; SAS Institute, Cary, NC) was used for the Poisson regression analyses. The codes used are available from the authors on request.
Table A1.
Distribution of Anthracycline Derivatives With Known Doses in Each Cohort
| Anthracycline or Anthraquinone | CCSS (n = 13,060) |
EKZ/AMC (n = 1,362) |
NWTS (n = 364) |
SJLIFE (n = 1,695) |
||||
|---|---|---|---|---|---|---|---|---|
| No. | %* | No. | %* | No. | %* | No. | %* | |
| None | 7,506 | 57.5 | 798 | 58.6 | 179 | 49.2 | 692 | 40.8 |
| Doxorubicin | 3,416 | 26.2 | 392 | 28.8 | 179 | 49.2 | 572 | 33.7 |
| Daunorubicin | 1,425 | 10.9 | 138 | 10.1 | 0 | 450 | 26.5 | |
| Idarubicin | 1 | 0.0 | 3 | 0.2 | 0 | 14 | 0.8 | |
| Epirubicin | 0† | 132 | 9.7 | 0 | 3 | 0.2 | ||
| Mitoxantrone | 0† | 25 | 1.8 | 0 | 18 | 1.1 | ||
| Unknown dose information | 1,194 | 9.1 | 9 | 0.7 | 6 | 1.6 | 5 | 0.3 |
Abbreviations: CCSS, Childhood Cancer Survivor Study; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; NWTS, National Wilms Tumor Study; SJLIFE, St Jude Lifetime Cohort.
Total percentages may exceed 100% because some patients may have received > one type of anthracycline.
Epirubicin and mitoxantrone were administered to four and 11 individuals, respectively, but doses were unknown.
Table A2.
Multivariable Poisson Regression Results for Each CHF Model in CCSS Cohort*
| Covariate | Simple Model |
Standard Model |
Heart Dose Model |
|||
|---|---|---|---|---|---|---|
| RR | 95% CI | RR | 95% CI | RR | 95% CI | |
| Sex | ||||||
| Male | 1.0 | Referent | 1.0 | Referent | 1.0 | Referent |
| Female | 1.6 | 1.3 to 2.1 | 1.7 | 1.3 to 2.2 | 1.7 | 1.3 to 2.1 |
| Age at diagnosis, years | ||||||
| < 5 | 1.5 | 1.0 to 2.3 | 2.2 | 1.4 to 3.4 | 2.6 | 1.6 to 4.1 |
| 5-9 | 1.2 | 0.8 to 1.9 | 1.6 | 1.0 to 2.4 | 1.9 | 1.2 to 2.9 |
| 10-14 | 1.2 | 0.9 to 1.6 | 1.2 | 0.9 to 1.7 | 1.4 | 1.0 to 2.0 |
| ≥ 15 | 1.0 | Referent | 1.0 | Referent | 1.0 | Referent |
| Anthracycline, mg/m2 | ||||||
| Any v none | 4.9 | 3.8 to 6.4 | — | — | — | — |
| None | — | — | 1.0 | Referent | 1.0 | Referent |
| < 100 | — | — | 1.9 | 0.7 to 5.1 | 2.1 | 0.8 to 5.9 |
| 100-249 | — | — | 3.3 | 2.1 to 5.2 | 3.7 | 2.3 to 5.9 |
| ≥ 250 | — | — | 8.6 | 6.4 to 11.5 | 10.5 | 7.7 to 14.4 |
| Chest RT, Gy† | ||||||
| Any v none | 3.2 | 2.5 to 4.1 | — | — | ||
| None | — | — | 1.0 | Referent | 1.0 | Referent |
| < 5 | — | — | 1.0 | 0.6 to 1.7 | 0.9 | 0.5 to 1.6 |
| 5-14 | — | — | 2.1 | 1.1 to 3.8 | 1.6 | 1.0 to 2.7 |
| 15-34 | — | — | 2.3 | 1.6 to 3.4 | 3.1 | 2.2 to 4.5 |
| ≥ 35 | — | — | 6.5 | 4.6 to 9.0 | 10.5 | 7.2 to 15.4 |
Abbreviations: CHF, congestive heart failure; RR, relative risk; RT, radiotherapy.
The following covariates were tested but not selected for inclusion in final analytic model: alkylating agents, platinum agents, vinca alkaloids, neck and/or abdominal RT (without any direct chest involvement).
Corresponding heart RT dose used for heart dose model.
Table A3.
Effect on Anthracycline Dose Categories Using Alternative Equivalence Formulas
| Anthracycline Dose (mg/m2) | CCSS (n = 13,060) |
EKZ/AMC (n = 1,362) |
SJLIFE (n = 1,695) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Formula One* |
Formula Two† |
Formula One* |
Formula Two† |
Formula One* |
Formula Two† |
|||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| None | 7,506 | 57.5 | 7,506 | 57.5 | 799 | 58.7 | 799 | 58.7 | 692 | 40.8 | 692 | 40.8 |
| < 100 | 422 | 3.2 | 513 | 3.9 | 32 | 2.3 | 63 | 4.6 | 218 | 12.9 | 368 | 21.7 |
| 100-249 | 1,354 | 10.4 | 1,353 | 10.4 | 263 | 19.3 | 236 | 17.3 | 549 | 32.4 | 402 | 23.7 |
| ≥ 250 | 2,584 | 19.8 | 2,494 | 19.1 | 259 | 19.0 | 255 | 18.7 | 231 | 13.6 | 228 | 13.5 |
| Unknown | 1,194 | 9.1 | 1,194 | 9.1 | 9 | 0.7 | 9 | 0.7 | 5 | 0.3 | 5 | 0.3 |
Abbreviations: CCSS, Childhood Cancer Survivor Study; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; SJLIFE, St Jude Lifetime Cohort.
Formula One: doxorubicin 1 mg/m2 = daunorubicin, 1; idarubicin, 3; epirubicin, 0.67; mitoxantrone, 4.
Formula Two: doxorubicin 1 mg/m2 = daunorubicin, 0.83; idarubicin, 5; epirubicin, 0.67; mitoxantrone, 4.
Table A4.
| Risk Factor | Standard Model Risk Score‡ |
|---|---|
| Original standard model | |
| Sex | |
| Male | 0 |
| Female | 1 |
| Age at diagnosis, years | |
| < 5 | 1 (2) |
| 5-9 | 1 |
| 10-14 | 0 |
| ≥ 15 | 0 |
| Anthracycline, mg/m2 | |
| None | 0 |
| < 100 | 1 |
| 100-249 | 2 (3) |
| ≥ 250 | 4 |
| Chest RT, Gy | |
| None | 0 (0) |
| < 5 | 1 (0) |
| 5-14 | 3 (2) |
| 15-34 | 3 (2) |
| ≥ 35 | 4 |
| Conventional risk factors§ | |
| Obesity | 1 |
| Diabetes | 0 |
| Dyslipidemia | 0 |
| Hypertension | 2 |
| Updated model | |
| AUC | 0.75‖ |
| C-index | 0.77‖ |
Abbreviations: AUC, area under the curve; C, concordance; CCSS, Childhood Cancer Survivor Study; CHF, congestive heart failure; RT, radiotherapy.
182 patient cases of CHF.
Restricted to CCSS participants with available information from baseline questionnaire who were free of grade ≥ 3 cardiomyopathy or CHF at time of baseline questionnaire.
No. in parentheses indicates value derived from original analytic population without accounting for the four additional conventional risk factors.
At time of baseline questionnaire, obesity defined by body-mass index ≥ 30 kg/m2 based on self-reported height and weight; diabetes, dyslipidemia, and hypertension defined as those who reported being diagnosed by a physician for the condition and who reported receiving specific medications prescribed for treatment of the condition for > 1 month or for ≥ 30 days in 1-year period during the previous 2 years.
AUC and C-index values per original standard model based on 10,521 survivors with 182 patient cases of heart failure were 0.74 and 0.76, respectively.
Table A5.
Classification of CHF Risk Groups Within External Cohorts Based on CCSS-Derived Risk Scores
| Risk Group | Risk Score | No. of Events | No. at Risk* | Cumulative Incidence† | P |
|---|---|---|---|---|---|
| EKZ/AMC simple model | |||||
| Low | < 3 | 1 | 646 | 0.2 | |
| Moderate | 3-4 | 17 | 477 | 10.3 | < .01 |
| High | ≥ 5 | 7 | 198 | 14.8 | .41 |
| EKZ/AMC standard model | |||||
| Low | < 3 | 1 | 651 | 0.2 | |
| Moderate | 3-5‡ | 14 | 468 | 9.0 | < .01 |
| High | ≥ 6 | 11 | 228 | 21.4 | .047 |
| EKZ/AMC heart dose model | |||||
| Low | < 3 | 1 | 469 | 0.2 | |
| Moderate | 3-5‡ | 12 | 590 | 7.0 | < .01 |
| High | 6-8 | 9 | 251 | 16.7 | .16 |
| Very high | ≥ 9 | 4 | 30 | 35.3 | .04 |
| NWTS simple model | |||||
| Low | < 3 | 1 | 162 | 0.03 | |
| Moderate | 3-4 | 5 | 40 | 1.0 | < .01 |
| High | ≥ 5 | 42 | 163 | 8.5 | .06 |
| NWTS standard model | |||||
| Low | < 3 | 1 | 158 | 0.03 | |
| Moderate | 3-5‡ | 5 | 48 | 0.9 | < .01 |
| High | ≥ 6 | 40 | 151 | 6.7 | .01 |
| SJLIFE simple model | |||||
| Low | < 3 | 1 | 512 | 0.8 | |
| Moderate | 3-4 | 13 | 726 | 4.6 | < .01 |
| High | ≥ 5 | 5 | 457 | 4.9 | .19 |
| SJLIFE standard model | |||||
| Low | < 3 | 1 | 603 | 0.7 | |
| Moderate | 3-5‡ | 12 | 740 | 5.3 | < .01 |
| High | ≥ 6 | 6 | 352 | 4.2 | .78 |
Abbreviations: CCSS, Childhood Cancer Survivor Study; CHF, congestive heart failure; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; NWTS, National Wilms Tumor Study; SJLIFE, St Jude Lifetime Cohort.
No. at risk varies by outcome and model because it excludes individuals with missing data.
At age 40 years, P value is for comparison with preceding risk group.
Survivors with total risk score of 3 with neither anthracycline nor chest or heart radiotherapy exposure are classified as low risk (EKZ/AMC, n = 137; NWTS, n = 66; SJLIFE, n = 107); none of these patients developed subsequent CHF.
Table A6.
Patients at Risk Over Time*
| Age (years) | CCSS (No. of patients) | EKZ/AMC (No. of patients) | NWTS† |
SJLIFE (No. of patients) | |
|---|---|---|---|---|---|
| No. of Patients | Total Survivors | ||||
| Baseline‡ | 13,060 | 1,362 | 364 | 6,760 | 1,695 |
| 26 | 9,398 | 757 | 89 | 1,619 | 870 |
| 30 | 7,350 | 531 | 60 | 1,162 | 738 |
| 35 | 4,961 | 297 | 25 | 475 | 403 |
| 40 | 2,744 | 115 | 7 | 151 | 204 |
Abbreviations: CCSS, Childhood Cancer Survivor Study; EKZ/AMC, Emma Children's Hospital and Academic Medical Center; NWTS, National Wilms Tumor Study; SJLIFE, St Jude Lifetime Cohort.
Alive, without congestive heart failure, and not censored for other reasons.
Case-cohort design with 364 patients used in actual analysis but based on 6,760 total survivors.
Five (CCSS, EKZ/AMC, NWTS) or 10 years after cancer diagnosis (SJLIFE); SJLIFE values at age 26 and 30 years exclude participants who had not yet entered cohort.
Footnotes
See accompanying editorial on page 379
Processed as a Rapid Communication manuscript.
Supported by Grants No. U24 CA55727, K07 CA151775, R01 CA054498, and P30 CA21765 from the National Institutes of Health and No. 257505 from PanCareSurFup EU and by the American Lebanese Syrian Associated Charities, Leukemia and Lymphoma Society, and Tom Voûte Fund.
Presented in part at the 12th International Conference on Long-Term Complications of Treatment of Children and Adolescents for Cancer, Williamsburg, VA, June 8-9, 2012.
The content of this research is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. No funder was involved with the review or approval of the manuscript.
Authors' disclosures of potential conflicts of interest are found in the article online at www.jco.org. Author contributions are found at the end of this article.
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Disclosures provided by the authors are available with this article at www.jco.org.
AUTHOR CONTRIBUTIONS
Conception and design: Eric J. Chow, Yan Chen, Charles A. Sklar, Yutaka Yasui
Financial support: Eric J. Chow, Leontien C. Kremer, Norman E. Breslow, Melissa M. Hudson, Leslie L. Robison
Administrative support: Eric J. Chow, Leontien C. Kremer, Norman E. Breslow, Melissa M. Hudson, Gregory T. Armstrong, Marilyn Stovall, Leslie L. Robison, Yutaka Yasui
Provision of study materials or patients: Leontien C. Kremer, Norman E. Breslow, Melissa M. Hudson, Daniel M. Green, Marilyn Stovall, Helena J. van der Pal, Rita E. Weathers, Leslie L. Robison
Collection and assembly of data: Eric J. Chow, Leontien C. Kremer, Norman E. Breslow, Melissa M. Hudson, Gregory T. Armstrong, Daniel M. Green, Lillian R. Meacham, Daniel A. Mulrooney, Kirsten K. Ness, Marilyn Stovall, Helena J. van der Pal, Rita E. Weathers, Leslie L. Robison
Data analysis and interpretation: Eric J. Chow, Yan Chen, Leontien C. Kremer, Gregory T. Armstrong, William L. Border, Elizabeth A.M. Feijen, Daniel M. Green, Lillian R. Meacham, Kathleen A. Meeske, Daniel A. Mulrooney, Kirsten K. Ness, Kevin C. Oeffinger, Charles A. Sklar, Marilyn Stovall, Helena J. van der Pal, Rita E. Weathers, Leslie L. Robison, Yutaka Yasui
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Individual Prediction of Heart Failure Among Childhood Cancer Survivors
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jco.ascopubs.org/site/ifc.
Eric J. Chow
No relationship to disclose
Yan Chen
No relationship to disclose
Leontien C. Kremer
No relationship to disclose
Norman E. Breslow
No relationship to disclose
Melissa M. Hudson
No relationship to disclose
Gregory T. Armstrong
No relationship to disclose
William L. Border
No relationship to disclose
Elizabeth A.M. Feijen
No relationship to disclose
Daniel M. Green
No relationship to disclose
Lillian R. Meacham
No relationship to disclose
Kathleen A. Meeske
No relationship to disclose
Daniel A. Mulrooney
No relationship to disclose
Kirsten K. Ness
No relationship to disclose
Kevin C. Oeffinger
No relationship to disclose
Charles A. Sklar
No relationship to disclose
Marilyn Stovall
No relationship to disclose
Helena J. van der Pal
No relationship to disclose
Rita E. Weathers
No relationship to disclose
Leslie L. Robison
No relationship to disclose
Yutaka Yasui
No relationship to disclose
REFERENCES
- 1.Robison LL, Hudson MM. Survivors of childhood and adolescent cancer: Life-long risks and responsibilities. Nat Rev Cancer. 2014;14:61–70. doi: 10.1038/nrc3634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipshultz SE, Adams MJ, Colan SD, et al. Long-term cardiovascular toxicity in children, adolescents, and young adults who receive cancer therapy: Pathophysiology, course, monitoring, management, prevention, and research directions—A scientific statement from the American Heart Association. Circulation. 2013;128:1927–1995. doi: 10.1161/CIR.0b013e3182a88099. [DOI] [PubMed] [Google Scholar]
- 3.Oeffinger KC, Mertens AC, Sklar CA, et al. Chronic health conditions in adult survivors of childhood cancer. N Engl J Med. 2006;355:1572–1582. doi: 10.1056/NEJMsa060185. [DOI] [PubMed] [Google Scholar]
- 4.Mertens AC, Liu Q, Neglia JP, et al. Cause-specific late mortality among 5-year survivors of childhood cancer: The Childhood Cancer Survivor Study. J Natl Cancer Inst. 2008;100:1368–1379. doi: 10.1093/jnci/djn310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reulen RC, Winter DL, Frobisher C, et al. Long-term cause-specific mortality among survivors of childhood cancer. JAMA. 2010;304:172–179. doi: 10.1001/jama.2010.923. [DOI] [PubMed] [Google Scholar]
- 6.Tukenova M, Guibout C, Oberlin O, et al. Role of cancer treatment in long-term overall and cardiovascular mortality after childhood cancer. J Clin Oncol. 2010;28:1308–1315. doi: 10.1200/JCO.2008.20.2267. [DOI] [PubMed] [Google Scholar]
- 7.van der Pal HJ, van Dalen EC, Hauptmann M, et al. Cardiac function in 5-year survivors of childhood cancer: A long-term follow-up study. Arch Intern Med. 2010;170:1247–1255. doi: 10.1001/archinternmed.2010.233. [DOI] [PubMed] [Google Scholar]
- 8.Hudson MM, Ness KK, Gurney JG, et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA. 2013;309:2371–2381. doi: 10.1001/jama.2013.6296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lipshultz SE, Lipsitz SR, Sallan SE, et al. Chronic progressive cardiac dysfunction years after doxorubicin therapy for childhood acute lymphoblastic leukemia. J Clin Oncol. 2005;23:2629–2636. doi: 10.1200/JCO.2005.12.121. [DOI] [PubMed] [Google Scholar]
- 10.Mulrooney DA, Yeazel MW, Kawashima T, et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: Retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ. 2009;339:b4606. doi: 10.1136/bmj.b4606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong GT, Oeffinger KC, Chen Y, et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J Clin Oncol. 2013;31:3673–3680. doi: 10.1200/JCO.2013.49.3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kero AE, Jarvela LS, Arola M, et al. Cardiovascular morbidity in long-term survivors of early-onset cancer: A population-based study. Int J Cancer. 2014;134:664–673. doi: 10.1002/ijc.28385. [DOI] [PubMed] [Google Scholar]
- 13.Armenian SH, Gelehrter SK, Chow EJ. Strategies to prevent anthracycline-related congestive heart failure in survivors of childhood cancer. Cardiol Res Pract. 2012;2012:713294. doi: 10.1155/2012/713294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kannel WB, D'Agostino RB, Silbershatz H, et al. Profile for estimating risk of heart failure. Arch Intern Med. 1999;159:1197–1204. doi: 10.1001/archinte.159.11.1197. [DOI] [PubMed] [Google Scholar]
- 15.D'Agostino RB, Vasan RS, Pencina MJ, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117:743–753. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 16.Conroy RM, Pyorala K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24:987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 17.Ezaz G, Long JB, Gross CP, et al. Risk prediction model for heart failure and cardiomyopathy after adjuvant trastuzumab therapy for breast cancer. J Am Heart Assoc. 2014;3:e000472. doi: 10.1161/JAHA.113.000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hudson MM, Neglia JP, Woods WG, et al. Lessons from the past: Opportunities to improve childhood cancer survivor care through outcomes investigations of historical therapeutic approaches for pediatric hematological malignancies. Pediatr Blood Cancer. 2012;58:334–343. doi: 10.1002/pbc.23385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Green DM, Kun LE, Matthay KK, et al. Relevance of historical therapeutic approaches to the contemporary treatment of pediatric solid tumors. Pediatr Blood Cancer. 2013;60:1083–1094. doi: 10.1002/pbc.24487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robison LL, Mertens AC, Boice JD, et al. Study design and cohort characteristics of the Childhood Cancer Survivor Study: A multi-institutional collaborative project. Med Pediatr Oncol. 2002;38:229–239. doi: 10.1002/mpo.1316. [DOI] [PubMed] [Google Scholar]
- 21.Robison LL, Armstrong GT, Boice JD, et al. The Childhood Cancer Survivor Study: A National Cancer Institute–supported resource for outcome and intervention research. J Clin Oncol. 2009;27:2308–2318. doi: 10.1200/JCO.2009.22.3339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le Deley MC, Leblanc T, Shamsaldin A, et al. Risk of secondary leukemia after a solid tumor in childhood according to the dose of epipodophyllotoxins and anthracyclines: A case-control study by the Societe Francaise d'Oncologie Pediatrique. J Clin Oncol. 2003;21:1074–1081. doi: 10.1200/JCO.2003.04.100. [DOI] [PubMed] [Google Scholar]
- 23.Shankar SM, Marina N, Hudson MM, et al. Monitoring for cardiovascular disease in survivors of childhood cancer: Report from the Cardiovascular Disease Task Force of the Children's Oncology Group. Pediatrics. 2008;121:e387–e396. doi: 10.1542/peds.2007-0575. [DOI] [PubMed] [Google Scholar]
- 24.Stovall M, Weathers R, Kasper C, et al. Dose reconstruction for therapeutic and diagnostic radiation exposures: Use in epidemiological studies. Radiat Res. 2006;166:141–157. doi: 10.1667/RR3525.1. [DOI] [PubMed] [Google Scholar]
- 25.The Childhood Cancer Survivor Study. Questionnaires. https://ccss.stjude.org/documents/questionnaires.
- 26.Cancer Therapy Evaluation Program. Common Terminology Criteria for Adverse Events (CTCAE), version 4.03. http://ctep.cancer.gov/
- 27.Meacham LR, Chow EJ, Ness KK, et al. Cardiovascular risk factors in adult survivors of pediatric cancer: A report from the childhood cancer survivor study. Cancer Epidemiol Biomarkers Prev. 2010;19:170–181. doi: 10.1158/1055-9965.EPI-09-0555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Draper NR, Smith H. Applied Regression Analysis. ed 3. New York, NY: Wiley; 1998. [Google Scholar]
- 29.Sorror ML, Maris MB, Storb R, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: A new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–2919. doi: 10.1182/blood-2005-05-2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heagerty PJ, Zheng Y. Survival model predictive accuracy and ROC curves. Biometrics. 2005;61:92–105. doi: 10.1111/j.0006-341X.2005.030814.x. [DOI] [PubMed] [Google Scholar]
- 31.Harrell FE, Lee KL, Mark DB. Multivariable prognostic models: Issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 32.Stone M. Cross-validatory choice and assessment of statistical predictions. J R Stat Soc. 1974;36:111–147. [Google Scholar]
- 33.Kalbfleisch JD, Prentice RL. The Statistical Analysis of Failure Time Data. ed 2. New York, NY: Wiley; 2002. [Google Scholar]
- 34.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- 35.Green DM, Grigoriev YA, Nan B, et al. Congestive heart failure after treatment for Wilms' tumor: A report from the National Wilms' Tumor Study Group. J Clin Oncol. 2001;19:1926–1934. doi: 10.1200/JCO.2001.19.7.1926. [DOI] [PubMed] [Google Scholar]
- 36.Skinner R, Wallace WH, Levitt GA. Long-term follow-up of people who have survived cancer during childhood. Lancet Oncol. 2006;7:489–498. doi: 10.1016/S1470-2045(06)70724-0. [DOI] [PubMed] [Google Scholar]
- 37.Sieswerda E, Postma A, van Dalen EC, et al. The Dutch Childhood Oncology Group guideline for follow-up of asymptomatic cardiac dysfunction in childhood cancer survivors. Ann Oncol. 2012;23:2191–2198. doi: 10.1093/annonc/mdr595. [DOI] [PubMed] [Google Scholar]
- 38.Lenihan DJ, Oliva S, Chow EJ, et al. Cardiac toxicity in cancer survivors. Cancer. 2013;119(suppl 11):2131–2142. doi: 10.1002/cncr.28061. [DOI] [PubMed] [Google Scholar]
- 38a.The Childhood Cancer Survivor Study. CHF risk calculator. ccss.stjude.org/chfcalc.
- 39.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 40.Landy DC, Miller TL, Lopez-Mitnik G, et al. Aggregating traditional cardiovascular disease risk factors to assess the cardiometabolic health of childhood cancer survivors: An analysis from the Cardiac Risk Factors in Childhood Cancer Survivors Study. Am Heart J. 2012;163:295.e2–301.e2. doi: 10.1016/j.ahj.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanco JG, Sun CL, Landier W, et al. Anthracycline-related cardiomyopathy after childhood cancer: Role of polymorphisms in carbonyl reductase genes—A report from the Children's Oncology Group. J Clin Oncol. 2012;30:1415–1421. doi: 10.1200/JCO.2011.34.8987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Visscher H, Ross CJ, Rassekh SR, et al. Validation of variants in SLC28A3 and UGT1A6 as genetic markers predictive of anthracycline-induced cardiotoxicity in children. Pediatr Blood Cancer. 2013;60:1375–1381. doi: 10.1002/pbc.24505. [DOI] [PubMed] [Google Scholar]
- 43.Lipshultz SE, Lipsitz SR, Kutok JL, et al. Impact of hemochromatosis gene mutations on cardiac status in doxorubicin-treated survivors of childhood high-risk leukemia. Cancer. 2013;119:3555–3562. doi: 10.1002/cncr.28256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wang X, Liu W, Sun CL, et al. Hyaluronan synthase 3 variant and anthracycline-related cardiomyopathy: A report from the Children's Oncology Group. J Clin Oncol. 2014;32:647–653. doi: 10.1200/JCO.2013.50.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kremer LC, Mulder RL, Oeffinger KC, et al. A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: A report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr Blood Cancer. 2013;60:543–549. doi: 10.1002/pbc.24445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.van Dalen EC, Michiels EM, Caron HN, et al. Different anthracycline derivates for reducing cardiotoxicity in cancer patients. Cochrane Database Syst Rev. 2010;5:CD005006. doi: 10.1002/14651858.CD005006.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong FL, Bhatia S, Landier W, et al. Efficacy and cost-effectiveness of the Children's Oncology Group long-term follow-up screening guidelines for childhood cancer survivors at risk of treatment-related heart failure. Ann Intern Med. 2014;160:672–683. doi: 10.7326/M13-2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Dalen EC, van der Pal HJ, Caron HN, et al. Different dosage schedules for reducing cardiotoxicity in cancer patients receiving anthracycline chemotherapy. Cochrane Database Syst Rev. 2009;4:CD005008. doi: 10.1002/14651858.CD005008.pub3. [DOI] [PubMed] [Google Scholar]
- 49.van Dalen EC, Caron HN, Dickinson HO, et al. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst Rev. 2011;6:CD003917. doi: 10.1002/14651858.CD003917.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Walker DM, Fisher BT, Seif AE, et al. Dexrazoxane use in pediatric patients with acute lymphoblastic or myeloid leukemia from 1999 and 2009: Analysis of a national cohort of patients in the Pediatric Health Information Systems database. Pediatr Blood Cancer. 2013;60:616–620. doi: 10.1002/pbc.24270. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.