Abstract
Exercising or working in a hot, humid environment can results in the onset of heat-related illness when an individual's temperature is not carefully monitored. The purpose of the present study was to compare three techniques (data loggers, thermal imaging, and wired electrodes) for the measurement of peripheral (bicep) and central (abdominal) skin temperature. Young men and women (N = 30) were recruited to complete the present study. The three skin temperature measurements were made at 0 and every 10-min during 40-min (60% VO2max) of cycling in a hot (39±2°C), humid (45±5% RH) environment. Data was statistically analyzed using the Bland-Altman method and correlation analysis. For abdominal skin temperature, the Bland-Altman limits of agreement indicated that data loggers (1.5) were a better index of wired than was thermal imaging (3.5), For the bicep skin temperature the limits of agreement was similar between data loggers (1.9) and thermal (1.9), suggesting the both were suitable measurements. We also found that when skin temperature exceeded 35°C, we observed progressively better prediction between data loggers, thermal imaging, and wired skin sensors. This report describes the potential for the use of data loggers and thermal imaging to be used as alternative measures of skin temperature in exercising, human subjects.
Keywords: data loggers, non-invasive, thermal imaging, heat illness
INTRODUCTION
Physical laborers, athletes, soldiers, fire fighters, and law enforcement officials are routinely required to exercise or work in hot, humid environments [1–8]. Exposure to environmental heat stress is dangerous due to the onset of heat-related illness. Complications from heat-related illness result in loss of practice and work time [4–8], which is particularly detrimental to athletes in the field of sport science. Technological advances have resulted to the emergence of new, low-cost devises that may be suitable alternatives for the measurement of skin temperature during exercise or work performance. Other researchers have described the use of compact data loggers for the study of skin temperature in sleep analysis, obesity/metabolic, and exercise studies [9–12]; however, these studies have not specifically examined a heat stress environment. Compact temperature data loggers and thermal imaging represent potentially promising alternatives due to their relatively low cost and/or ability to extract large volumes of data with minimal effort. Despite the potential in these methods, to our knowledge no published studies have compared data loggers and thermal imaging during exercise in a mixed population of men and women. The purpose of this study was to compare different methods of measuring skin temperature during exercise in a hot, humid environment.
MATERIALS AND METHODS
Subjects
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. Prior to formal testing of subjects, all procedures described in this report were reviewed and approved by the committee for the protection of human subjects at the University of Houston (12080-01). Subjects gave their written informed consent for participating after being explained the risks and benefits associated with participation by a member of the study staff. A total of 30 individuals (14 men and 16 women; Age = 22±4 y) participated in this study. Subjects were screened to ensure they had average fitness (determined by graded exercise test with gas exchange measurement; O2max = 41.6 ± 2.9 ml · min−1 · kg−1) and were of normal body weight (determined via whole body DXA scan; BMI = 23.4±1.8; 18.1±3.5% Body Fat).
Exercise Trial
Prior to arriving at the laboratory, subjects were instructed to abstain from food (>8h) and exercise (>12h). After arriving at the laboratory, subjects were asked to provide a small urine sample to screen for hydration status using urine specific gravity (Atago; Livermore, CA). Subjects were fitted with a Polar heart rate monitor and completed 40-min of cycling at a wattage that yielded 60% of aerobic capacity in a hot (39.2±0.2°C), humid (55±5% RH) environment. During exercise, subjects were allowed ad libitum water intake. The subjects did not wear any clothing covering either of the temperature measurement sites and air movement in the chamber was static. Skin temperature was measured at the bicep and abdomen every 10-min during exercise using the three methods (described in detail below).
Wired Skin Sensors
Wired, YSI400 series skin electrodes (Measurement Specialties; Hampton, VA) were mounted on the skin using adhesive tape and connected to a Cole-Parmer tele-thermometer (Vernon Hills, IL). According to the manufacture, the accuracy of the wired sensors used in this study was 0.1°C.
Data Logger Temperature Measurement
iButtons (DS1921H; Maxim Integrated; San Jose, CA) were activated using computer software and mounted on the subjects skin using adhesive tape (Cover-Roll; BSN Medical; USA). According to the manufacture, the accuracy of the data loggers used in this study was 0.125°C.
Thermal Imaging Temperature Measurement
Thermal skin temperature was determined by capturing thermal skin images (Razr-IR MAX; Sierra Pacific Innovations; Las Vegas, NV). The camera used in this study incorporates a microbolometer UFPA (uncooled focal plane array) 25µm detector and thermal sensitivity of ≤ 0.1°C. A telephoto thermal lens was attached to increase the small pixel field of view. Images were taken by positioning the camera lens perpendicular to the targeted skin temperature site at a distance of 25.4 cm. Care was taken to ensure that the iButton and wired skin electrode were visible within each thermal image, allowing direct comparison of the skin temperature at approximately the same anatomical location.
Statistical Analysis
All statistical analysis was completed in SPSS (v.20.0; Chicago, IL). Prior to formal statistical testing data was assessed for normality and constant error variance. No significant gender effects were noted, thus men and women were combined to complete the statistical testing in the present study. Measurement methods were compared in a pairwise fashion using the methods described by Bland-Altman [13]. In each comparison, wired skin temperature measurement was used as the criterion. The SDs of the mean differences were calculated and multiplied by the 1.96 value (.95 confidence level) from the normal distribution to provide the expected limits of agreement between the wired and other measures. We plotted the differences (y axis) across the averages (x axis) of the compared measurements. Separate analyses were completed for bicep and abdominal sites. Pearson correlations were also completed to compare either data loggers or thermal skin temperature to wired skin temperature as a function of exercise time. Significance was set at P < 0.05 for all analyses.
RESULTS
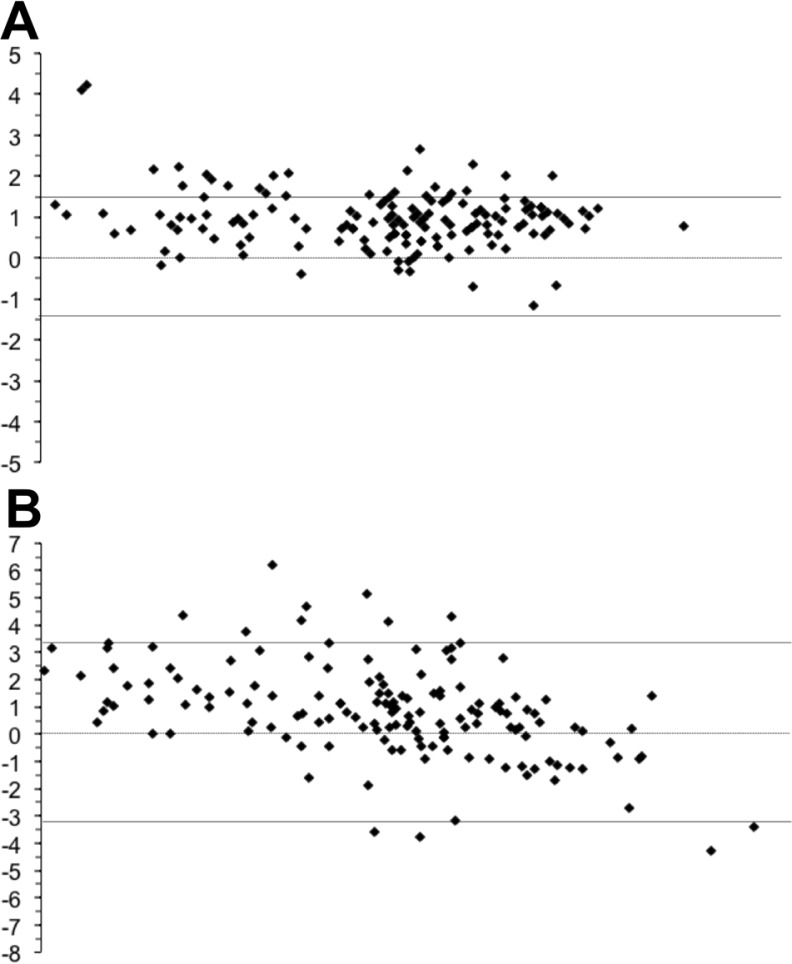
Wired vs. Data Logger Abdominal Temperature
We found the limits of agreement to be ±1.53 (Figure 1A). Inspection of the plot revealed that 1) wired measurements were greater than the data logger measurements, 2) The distribution of the differences was consistent across the range of temperatures, and 3) A relatively small number of differences were above the limit of agreement and none were below the limit. We found significant correlations between data wired and data logger across all exercise time points: 0 (R = 0.488, P = 0.006), 10 (0.616, <0.0001), 20 (0.668, <0.0001), 30(0.783, <0.0001), and 40 (0.867, <0.0001). When collapsed across time points the correlation was R = 0.885 (P < 0.0001).
FIG. 1.
Bland-Altman plots for Wired vs. Wireless (A) and Wired vs. Thermal (B) measurements of abdominal skin temperature.
Based on the limits of agreement, Wireless, but not Thermal imaging is a suitable alternative for wired abdominal skin temperature. Also, when the actual skin temperature exceeded 35°C, the limit of agreement was further improved between wired and wireless skin measurements.
Wired vs. Thermal Abdominal Temperature
We found the limits of agreement to be ±3.43 (Figure 1B). These limits of agreement were 133% larger than wired vs. wireless abdominal skin temperature. Inspection of the plot revealed that 1) The wired measurements are generally higher than the thermal measurements, 2) An increasing number of thermal measures exceed the wired measures at higher temperatures (which demonstrated inconsistency in the pattern of the differences), and 3) A small number of differences fall outside the limits of agreement. We only found a significant correlation between wired and thermal temperature at 20-min (R = 0.376; P = 0.040). When collapsed across time points the correlation was R = 0.623 (P < 0.0001).
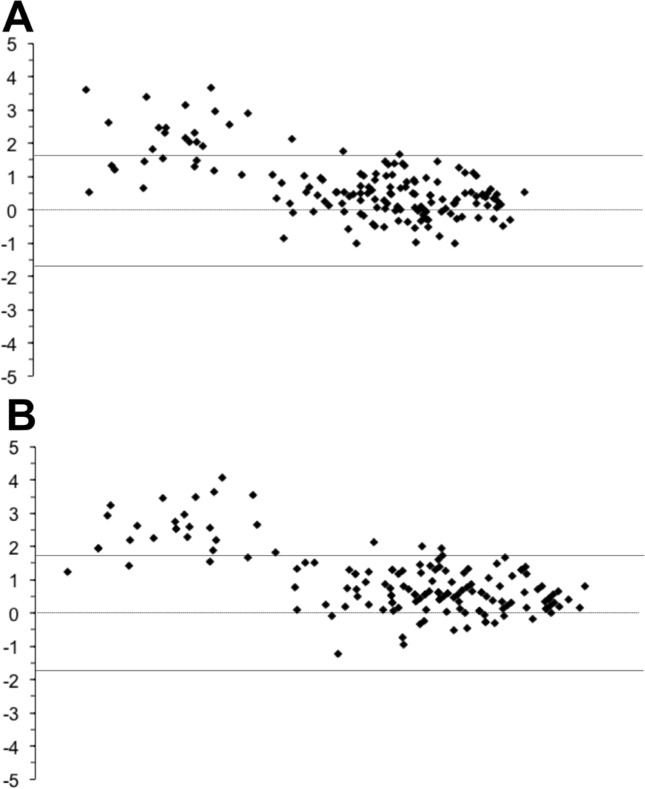
Wired vs. Data Logger Bicep Temperature
We found the limits of agreement to be ±1.9 (Figure 2A). The limits of agreement for the bicep comparison was only slightly higher than limits of agreement for abdominal wired vs. wireless. Inspection of the plot indicated 1) The wired measures were consistently higher than the wireless measures, 2) The distribution of differences varied across the range of temperatures with the differences being greater at lower temperatures, and 3) There was a higher number of differences above the limit of agreement at lower temperatures (<35 degrees). We found a significant correlation between wired and data loggers at 10 (R = 0.560, P = 0.01), 20 (0.626, <0.0001), 30 (0.658, <0.0001), and 40 (0.791, <0.0001) minutes of exercise. When collapsed across time points the correlation was R = 0.869 (P < 0.0001).
FIG. 2.
Bland-Altman plots for Wired vs. Wireless (A) and Wired vs. Thermal (B) measurements of bicep skin temperature.
Based on the limits of agreement, it appears that either wireless or thermal are a suitable alternative for wired bicep skin temperature. Also, when the actual skin temperature exceeded 35°C, the limit of agreement was further improved between for both alternate measurement techniques.
Wired vs. Thermal Bicep Temperature
We found the limits of agreement to be ±1.82 when comparing wired vs. thermal abdominal temperature (Figure 2B). Inspection of this plot indicated that 1) As with the other three comparisons, the wired measures were consistently higher than the wireless measures, 2) Similar to previous comparison, the distribution of differences varied across the range of temperatures with the differences being greater at lower temperatures, 3) There was a higher number of differences above the limit of agreement at lower temperatures (<35 degrees). We found a significant correlation between wired and data loggers at 10 (R = 0.560, P = 0.001), 20 (0.626, <0.0001), 30 (0.689, <0.0001), and 40 (0.725, <0.0001) minutes of exercise. When collapsed across time points the correlation was R = 0.868 (P < 0.0001).
DISCUSSION
The key finding of the present study were that the skin temperature measured using data logger and wired sensors were similar at both locations; however, the corresponding thermal temperature only matched these two when measured at the bicep. At the bicep, the data logger and thermal images had a measurement bias that ranged between 1.5 and 1.8°C. In contrast, at the abdomen, data loggers had a measurement bias of 1.9°C, but the thermal image temperature had a measurement bias of 3.4°C. The other skin temperature measurements were fairly consistent; however, given the greater measurement bias of thermal images at the abdomen, this may not be the ideal measurement technique for this anatomical location. The most likely explanation for inconsistencies in thermal abdominal skin temperature may be due to underlying subcutaneous adipose tissue. A systemic bias <2 was considered acceptable for these measurements because the typical range of skin temperature change during exercise is roughly 3°C, thus a bias <2 allowed sufficient variance to detect exercise-induced changes. The present study addresses the experimental design limitations of previous studies [10, 11, 14, 15] by including multiple measures of skin temperature in the same subjects over time.
Another interesting finding of the present study was that regardless of measurement method, when skin temperature exceeded 35°C (at approximately 25-min of exercise), the measurement bias for data loggers and thermal imaging compared to wired sensors decreased, with the exception of thermal image temperature on the abdomen. To further evaluate this effect, we completed additional analysis focusing on values >35°C and found that in all cases except for abdominal wired vs. thermal, the limits of agreement decreased in a range of 4%-7%, meaning that the two methods better matched one another. Bland-Altman described this result as one where the consistency between measurements is highly dependent on the magnitude of the response being measured [13]. The pattern we observed was similar to what Smith et al. reported when comparing data loggers and wired skin sensors [10]. One limitation of the present study is due to the volume of measurements being collected; we were limited to exploring the change in skin temperature at only one peripheral and one central anatomical site. In future projects, we will strive to extend the present comparison to include additional locations.
CONCLUSIONS
The key findings of the present study provide new information concerning measurement bias of skin temperature measured via data loggers and thermal imaging at two different anatomical locations. These two locations were selected such that the quantity of body fat beneath the measurement site would differ, thus providing a differential change in temperature during exercise. While the present study was completed in a controlled, laboratory environment, the observed measurement bias reflects the conclusion that data loggers and thermal imaging may be suitable alternatives for the measurement of peripheral and central skin temperature in a field setting. The key findings of the present study also have implication for the sport science field because accurate monitoring of skin temperature may allow for better tracking of the risk of heat-related illness. Complications associated with heat-related illness routine result in the loss of practice and competition days. One future application of this work within the field of sport science would be to develop computational algorithms that allow for the assessment of the risk of heat-related illness based on change in skin temperature.
Acknowledgements
This project was funded in part by a grant to Dr. McFarlin from the University of North Texas (Research Initiation Grant).
Conflict of interests
The authors declared no conflict of interests regarding the publication of this manuscript.
REFERENCES
- 1.Mitchell JB, Dugas JP, McFarlin BK, Nelson MJ. Effect of exercise, heat stress, and hydration on immune cell number and function. Med Sci Sports Exerc. 2002;34(12):1941–50. doi: 10.1097/00005768-200212000-00013. [DOI] [PubMed] [Google Scholar]
- 2.McFarlin BK, Mitchell JB. Exercise in hot and cold environments: differential effects on leukocyte number and NK cell activity. Aviat Space Environ Med. 2003;74(12):1231–6. [PubMed] [Google Scholar]
- 3.Carpenter KC, Breslin WL, Davidson T, Adams A, McFarlin BK. Baker's yeast β-glucan supplementation increases monocytes and cytokines post-exercise: implications for infection risk? Br J Nutr. 2013;109(3):478–86. doi: 10.1017/S0007114512001407. [DOI] [PubMed] [Google Scholar]
- 4.Casa DJ, Armstrong LE, Kenny GP, O'Connor FG, Huggins RA. Exertional heat stroke: new concepts regarding cause and care. Curr Sports Med Rep. 11(3):115–23. doi: 10.1249/JSR.0b013e31825615cc. [DOI] [PubMed] [Google Scholar]
- 5.Bergeron MF. Reducing sports heat illness risk. Pediatr Rev. 2013;34(6):270–9. doi: 10.1542/pir.34-6-270. [DOI] [PubMed] [Google Scholar]
- 6.Kuennen M, Gillum T, Dokladny K, Schneider S, Moseley P. Fit persons are at decreased (not increased) risk of exertional heat illness. Exerc Sport Sci Rev. 2013;41(2):134–5. doi: 10.1097/JES.0b013e3182877ced. [DOI] [PubMed] [Google Scholar]
- 7.Kazman J Ben, Heled Y, Lisman PJ, Druyan A, Deuster PA, O'Connor FG. Exertional heat illness: the role of heat tolerance testing. Curr Sports Med Rep. 12(2):101–5. doi: 10.1249/JSR.0b013e3182874d27. [DOI] [PubMed] [Google Scholar]
- 8.Rohe ST. Exertional heat illness in a Marine training on the endurance course. JAAPA. 2012;25(6):34,36–8. doi: 10.1097/01720610-201206000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Hasselberg MJ, McMahon J, Parker K. The validity, reliability, and utility of the iButton® for measurement of body temperature circadian rhythms in sleep/wake research. Sleep Med. 2013;14(1):5–11. doi: 10.1016/j.sleep.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 10.Smith ADH, Crabtree DR, Bilzon JLJ, Walsh NP. The validity of wireless iButtons and thermistors for human skin temperature measurement. Physiol Meas. 2010;31(1):95–114. doi: 10.1088/0967-3334/31/1/007. [DOI] [PubMed] [Google Scholar]
- 11.van Marken Lichtenbelt WD, Daanen HAM, Wouters L, Fronczek R, Raymann RJEM, Severens NMW, Van Someren EJW. Evaluation of wireless determination of skin temperature using iButtons. Physiol Behav. 2006;88(4- 5):489–97. doi: 10.1016/j.physbeh.2006.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Corbalán-Tutau MD, Madrid JA, Ordovás JM, Smith CE, Nicolás F, Garaulet M. Differences in daily rhythms of wrist temperature between obese and normal-weight women: associations with metabolic syndrome features. Chronobiol Int. 2011;28(5):425–33. doi: 10.3109/07420528.2011.574766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10. [PubMed] [Google Scholar]
- 14.Bourlai T, Pryor RR, Suyama J, Reis SE, Hostler D. Use of thermal imagery for estimation of core body temperature during precooling, exertion, and recovery in wildland firefighter protective clothing. Prehosp Emerg Care. 2012;16(3):390–9. doi: 10.3109/10903127.2012.670689. [DOI] [PubMed] [Google Scholar]
- 15.Formenti D, Ludwig N, Gargano M, Gondola M, Dellerma N, Caumo A, Alberti G. Thermal imaging of exercise-associated skin temperature changes in trained and untrained female subjects. Ann Biomed Eng. 2013;41(4):863–71. doi: 10.1007/s10439-012-0718-x. [DOI] [PubMed] [Google Scholar]