Abstract
Purpose
To evaluate the association between binocular visual field defects in drivers with glaucoma and risk of motor vehicle collision (MVC) involvement.
Methods
A retrospective cohort study was conducted on 438 drivers with glaucoma aged ≥ 55 years old using data from 1994 through 2000. Demographic, clinical, and driving characteristics were obtained from chart abstractions and patient survey. Binocular field measures were generated by combining data from the monocular (central 24° radius) fields whereby the binocular field measure was defined as the more sensitive point at each monocular field location. Measures included threshold (TH), total deviation (TD), and pattern deviation (PD); severe impairment in these measures was defined as falling into the worst quartile. MVC data was obtained from police records. Rate ratios (RR) and 95% confidence intervals (CI) were calculated.
Results
Drivers with severely impaired PD measures were twice as likely to have an at-fault MVC compared to those not severely impaired (RR 2.13, 95% CI 1.21-3.75); those with severely impaired TH (RR 1.49, 95% CI 0.81-2.74) and TD (RR 1.50, 95% CI 0.82-2.74) also had an increased rate of at-fault MVCs, although these were not significant. When the binocular central visual field was stratified into 9 regions, drivers with impaired TH, TD, or PD had similarly elevated MVC rates in all regions compared to those not severely impaired, though not all reached statistical significance.
Conclusions
Based on clinical measures of visual field routinely used in the management of glaucoma, drivers with glaucoma with severe PD field defects in the binocular field have a higher rate of at-fault MVC compared to those with less impaired or unimpaired binocular visual fields.
Introduction
Open angle glaucoma is a chronic progressive optic neuropathy characterized by changes of the optic disk, thinning of the retinal nerve fiber layer, and gradual loss of visual function beginning in the peripheral field and extending to central vision in advanced disease. It is the second leading cause of vision loss in the United States1 and the leading cause among African-Americans.2 More than 2.2 million Americans aged ≥40 years3 and 6.7 million people worldwide are affected by the disease.4 Numerous studies have observed that glaucoma patients have a decreased quality of life5-9 and reduced mobility.10,11
A number of studies have evaluated driver safety and performance among glaucoma patients, comparing them to non-glaucomatous drivers as well as to those with less severe disease. This body of research includes studies evaluating simulator and on-road driving performance as well as real-world motor vehicle collisions (MVCs). Haymes et al.12 compared the on-road performance of glaucoma patients to normally sighted age- and sex-matched controls and observed similar performance on many maneuvers and skills with the notable exception of detecting peripheral obstacles, with which the glaucoma patients had more difficulty. In two studies Szlyk et al.12,13 compared drivers with and without glaucoma with respect to simulator and self-reported MVCs and reported in one instance no difference13 and a higher frequency of both events in the other.14 Observational studies have also yielded inconsistent findings with some studies reporting no association15,16 between glaucoma and MVC occurrence and others reporting a positive association17-19 In one study, glaucoma was protective for MVCs,20 which might imply that glaucomatous drivers exercise greater cautiousness when behind the wheel. In a subsequent report we demonstrated that glaucomatous drivers with moderate to severe visual field impairment in the worse eye had an increased risk for MVC involvement and at-fault MVCs compared to glaucomatous drivers with no defect.21 This finding is consistent with prior studies highlighting that visual field impairment does not significantly elevate MVC risk until field loss is severe, although these studies did not focus on persons with glaucoma per se.22,23
The lack of an association observed in some studies might be attributed to patients compensating for field loss by self-regulating their driving behaviors and avoiding difficult driving situations.24,25 However, it is also important to bear in mind that the methodology used in previous studies was wide ranging including, for example, both police-16-18,20,21 and self-reported MVCs, 12,13,15,19 as well as clinically confirmed and self-reported glaucoma.17 Additionally, disagreement among prior studies may stem from some studies not accounting for driving exposure when assessing crash risk22 and limited sample sizes.12-14 A noteworthy limitation of previous studies on MVC involvement is that they relied on “single eye” analyses (e.g., better eye or worse eye analyses) and did not use binocular visual field indices, which may better reflect how drivers view the world. A practical limitation of many previous studies is the failure to utilize a measure of visual field impairment that is used in routine clinical practice so that ophthalmologists and optometrists can easily translate clinical findings to recommendations about driver safety.26
In the present study we evaluate the association between visual field defects in drivers aged ≥55 years with glaucoma and their risk of MVC involvement. We incorporate two design features absent in much of the previous work. First, we use visual field measures that are routinely used in the management of glaucoma (i.e., indices from automated perimetry print-outs) and, second, we use visual field measures that represent the binocular visual field, which is how a driver experiences the roadway environment.
Methods
Study Design and Cohort
A retrospective cohort study design was used to evaluate the possible association between visual field measurements and MVCs among subjects with a diagnosis of glaucoma. The study cohort consisted of individuals aged 55 years or greater who had been seen at least once between January 1994 and December 1995 in any of three university-affiliated ophthalmology and optometry practices specializing in the diagnosis and treatment of glaucoma.20 The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 365.1 and 365.2 were used to identify all potentially eligible patients with glaucoma seen at each of these locations. The medical records of each potentially eligible patient were abstracted to verify the diagnosis of glaucoma though information regarding the basis for that diagnosis was not obtained. Patients were excluded if (1) their primary cause of visual impairment was an ocular disorder other than glaucoma (e.g. macular degeneration, diabetic retinopathy, or clinically significant cataract for which surgery was recommended). Persons with diagnoses of refractive error, dry eye, and early cataract were eligible for the study. (2) Automated central visual field data (either a Humphrey Visual Field Analyzer 30-2 or 24-2 test (Carl Zeiss Meditec, Dublin CA)) for both eyes were not in the medical record during the study period; and (3) patients were not legally licensed to drive by the State of Alabama. Information on licensure status was obtained by cross-referencing each subject’s demographic and residential information obtained from the medical record with the Alabama Department of Public Safety (ADPS) database.
Data Collection
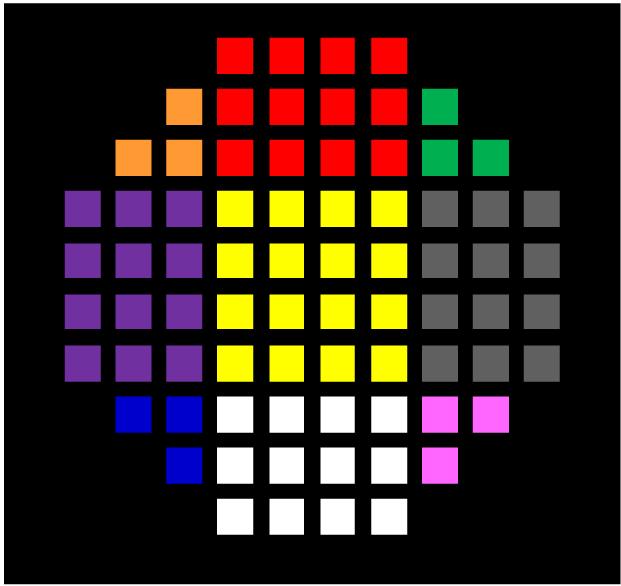
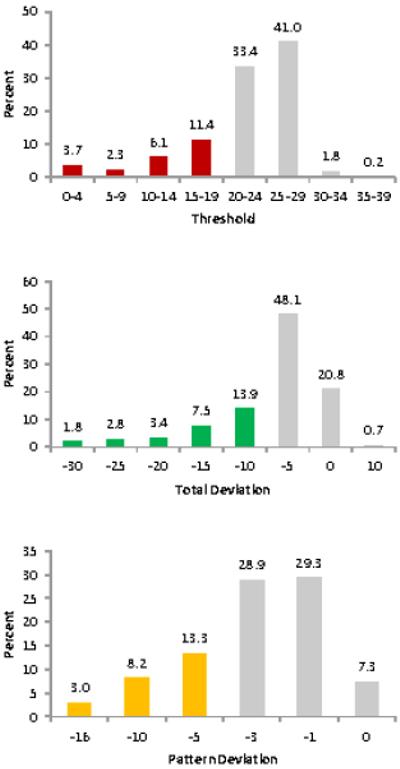
In addition to confirming the diagnosis of glaucoma, medical records from all visits during the study period (i.e., January 1994 and December 1995) were used to obtain information on best corrected visual acuity in each eye and visual field measurements (either a 30-2 or 24-2 test) in each eye. There were three types of visual field measurements used, which are available on the HFA print-out: (1) threshold (TH), a measure of differential light sensitivity (i.e. a measure of sensitivity to light in a region of the retina), (2) total deviation (TD), a deviation of the threshold value at each point from an age-matched normative database, and (3) pattern deviation (PD), a measure of irregularity in the field. For each patient, binocular visual field measures were created by taking the value for the better seeing eye on a point-by-point basis across the visual field area assessed by the 24-2 or 30-2 test.27 These binocular values were then averaged across all points in the field and categorized into quartiles according to the distribution values among the study cohort. The values in the lowest quartile were defined as severely impaired (TH: <20.4, TD: <−7.25, PD: <−3.97); those drivers in the other three quartiles served as the reference group (Figure 1). The central binocular visual field was further stratified into nine regions (Figure 2), and the average of all points for TH, TD and PD in each region was calculated. The aforementioned cut-points were then used to define severe impairment for each region as described above. For the purposes of this analysis, each patient’s first set of visual field measurements during the follow-up period was used.
Figure 1.
Distribution of binocular visual field measurements; lowest quartile, representing severe impairment, is defined by the bars in color.
Figure 2.
Binocular visual field regions
To obtain information on demographic characteristics, driving, general health, smoking and alcohol use, a telephone survey was conducted between February and June 2000. Demographic information was gathered by using standard questions regarding age, gender, and race. Respondents were asked to respond questions on driving habits using 1995 as the reference point. The Driving Habits Questionnaire (DHQ),28 previously shown to be reliable and valid among older drivers, was used to collect information on driving exposure defined in terms of estimated weekly mileage.29
Information regarding all MVCs that occurred between January 1994 and June 2000 wherein the study subject was the driver was obtained from the Alabama Department of Public Safety. Information of specific relevance to the study was abstracted from hard-copy accident reports, including the date of the accident and whether the study subject was deemed to be at fault according to the officer at the scene.
The Institutional Review Board for Human Use at the University of Alabama at Birmingham approved the study protocol. The study followed the tenets of the Declaration of Helsinki, and informed consent was obtained from the subjects.
Statistical Analysis
Descriptive statistics were generated for demographic, behavioral, driving and clinical characteristics. Poisson regression was used to calculate rate ratios (RRs) and 95% confidence intervals (CIs) for the association between TH, TD, and PD impairment in each region and the rate of MVC involvement. RRs were adjusted for age, gender, race and visual acuity.
Results
The final cohort consisted of 438 glaucoma patients who had a mean of 72.8 years; slightly over half were female (55.5%) and white (60.5%), the remainder black (Table 1). The average time of follow-up was 5.1 years and average annual mileage was 11,379, slightly less than the national average of 13,476.30 The mean acuity was 0.12 logMAR in the better eye and 0.32 logMAR in the worse eye. Fifty-seven at-fault MVCs occurred in the follow-up period.
Table 1. Demographic and visual function characteristics of the study participants.
| Mean (SD) or % (N) | |
|---|---|
| Age, in years | 72.8 (7.3) |
| Gender, female | 55.5 (243) |
| Race, white | 60.5 (265) |
| Follow-up, in years | 5.1 (1.2) |
| Annual mileage | 11,379 (12,885) |
| Visual Acuity, in logMar | |
| Better eye | 0.12 (0.16) |
| Worse eye | 0.32 (0.38) |
| At-fault MVCs | 13.0 (57) |
The overall rate of at-fault MVCs was 2.2 per million miles traveled (Table 2). Over the entire visual field assessed, participants with severely impaired TH or TD had a non-significant 49% and 50% increased rate of at-fault MVCs, respectively, compared to those in the reference group. Glaucoma patients in the severely impaired PD group had a significantly elevated at-fault MVC rate (RR 2.13, 95% CI 1.21-3.75) compared to those who were not severely impaired.
Table 2. Rate of at-fault motor vehicle collisions (MVC) per person-miles driven by visual field impairment.
| At- Fault MVCs |
Person-Miles | At-Fault MVC Rate (per million miles) |
RR (95% CI) | RR (95% CI)* | |
|---|---|---|---|---|---|
| Overall | 57 | 25,555,560 | 2.23 | --- | --- |
| Threshold | |||||
|
Not severely
impaired |
39 | 19,543,112 | 2.00 | 1.00 | 1.00 |
| Severely impaired | 18 | 5,945,927 | 3.03 | 1.52 (0.87-2.65) | 1.49 (0.81-2.74) |
| Total Deviation | |||||
|
Not severely
impaired |
39 | 19,670,715 | 1.98 | 1.00 | 1.00 |
| Severely impaired | 18 | 5,818,324 | 3.09 | 1.56 (0.89-2.73) | 1.50 (0.82-2.74) |
| Pattern Deviation | |||||
|
Not severely
impaired |
35 | 19,818,635 | 1.77 | 1.00 | 1.00 |
| Severely impaired | 22 | 5,670,404 | 3.88 | 2.20 (1.29-3.75) | 2.13 (1.21-3.75) |
Adjusted for age, gender, race and visual acuity.
Table 3 presents the number of at-fault MVCs and person-miles of travel for those with and without severe visual field impairment in each of the nine binocular visual field regions. Table 4 presents the associated adjusted RRs comparing the severely impaired group to the reference group with respect to at-fault MVCs for each of the nine binocular visual field regions. Compared to the reference group, subjects with severely impaired TH in the upper right region and upper left region of the central binocular field had significantly elevated MVC rates (RR 1.94; 95% CI 1.13-3.3 and RR 1.83; 95% CI 1.05-3.18, respectively). For subjects with impaired TD, significantly increased MVC rates were observed in the upper center (RR 2.18; 95% CI 1.23-3.87) and lower right (RR 2.12; 95% CI 1.17-3.85) regions compared to the reference group. Based on the PD measure, subjects in the severely impaired group were more likely to experience a MVC if the impairment was located in the middle left (RR 2.01; 95% CI 1.19-3.41), lower left (RR 2.03; 95% CI 1.13-3.65) or lower right (RR 2.69; 95% CI 1.48-4.87) regions compared to the reference group.
Table 3. Number of at-fault motor vehicle collisions and person-miles of travel according to severe visual field impairment by region.
| Severely Impaired | Severely Impaired | Severely Impaired | ||||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| Threshold | ||||||
| At-Fault Crashes | 25 | 32 | 23 | 34 | 25 | 32 |
| Person-Miles | 7,760,287 | 17,728,753 | 7,762,201 | 17,726,838 | 7,592,676 | 17,896,363 |
|
|
||||||
| At-Fault Crashes | 21 | 36 | 9 | 48 | 22 | 35 |
| Person-Miles | 6,650,912 | 18,838,127 | 2,119,066 | 23,369,973 | 6,922,807 | 18,566,233 |
|
|
||||||
| At-Fault Crashes | 17 | 40 | 13 | 44 | 17 | 40 |
| Person-Miles | 5,371,807 | 20,117,232 | 3,931,755 | 21,557,285 | 4,490,614 | 20,998,425 |
|
| ||||||
| Total Deviation | ||||||
| At-Fault Crashes | 20 | 37 | 21 | 36 | 18 | 39 |
| Person-Miles | 6,519,016 | 18,970,023 | 5,469,563 | 20,019,476 | 5,961,200 | 19,527,840 |
|
|
||||||
| At-Fault Crashes | 23 | 34 | 14 | 43 | 20 | 37 |
| Person-Miles | 7,258,753 | 18,230,287 | 3,625,093 | 21,863,946 | 7,663,822 | 17,825,217 |
|
|
||||||
| At-Fault Crashes | 17 | 40 | 15 | 42 | 19 | 38 |
| Person-Miles | 6,199,227 | 19,289,812 | 4,896,477 | 20,592,562 | 4,710,991 | 20,778,048 |
|
| ||||||
| Pattern Deviation | ||||||
| At-Fault Crashes | 21 | 36 | 25 | 32 | 20 | 37 |
| Person-Miles | 7,444,500 | 18,044,539 | 8,352,896 | 17,136,144 | 6,668,718 | 18,820,322 |
|
|
||||||
| At-Fault Crashes | 22 | 30 | 7 | 50 | 21 | 36 |
| Person-Miles | 8,089,991 | 17,399,049 | 2,792,013 | 22,697,027 | 7,681,970 | 17,807,069 |
|
|
||||||
| At-Fault Crashes | 19 | 38 | 15 | 42 | 21 | 36 |
| Person-Miles | 5,380,931 | 20,108,109 | 4,341,312 | 21,147,727 | 3,912,458 | 21,576,581 |
Table 4. Rate ratios (RR) and 95% confidence intervals (CI) for the association between severe visual field impairment by region and at-fault motor vehicle collision (MVC) involvement.
| Threshold RR (95% CI) | ||
|---|---|---|
|
1.83
(1.05-3.18) |
1.57 (0.90-2.74) |
1.94
(1.13-3.37) |
|
| ||
| 1.59 (0.89-2.85) |
1.57 (0.72-3.40) |
1.66 (0.94-2.94) |
|
| ||
| 1.82 (0.98-3.37) |
1.48 (0.76-2.88) |
1.73 (0.94-3.18) |
| Total Deviation RR (95% CI) | ||
|---|---|---|
| 1.59 (0.89-2.87) |
2.18
(1.23-3.87) |
1.58 (0.88-2.82) |
|
| ||
| 1.67 (0.95-2.96) |
1.54 (0.80-2.95) |
1.12 (0.63-1.99) |
|
| ||
| 1.52 (0.82-2.79) |
1.41 (0.75-2.64) |
2.12
(1.17-3.85) |
| Pattern Deviation RR (95% CI) | ||
|---|---|---|
| 1.37 (0.78-2.42) |
1.60 (0.92-2.76) |
1.47 (0.84-2.57) |
|
| ||
|
2.01
(1.19-3.41) |
1.00 (0.43-2.32) |
1.21 (0.69-2.12) |
|
| ||
|
2.03
(1.13-3.65) |
1.51 (0.81-2.84) |
2.69
(1.48-4.87) |
Adjusted for age, gender, race and visual acuity
Discussion
Our results suggest that drivers with glaucoma over 54 years old who have a severely impaired PD value for the binocular visual field have an elevated risk for at-fault MVC involvement, as compared to those who are unimpaired or less severely impaired in their binocular field. We sought to determine if sensitivity loss in any specific region of the central field made one more vulnerable to MVC involvement; however, for all visual field measures studied (TH, TD, PD), impaired drivers had elevated at-fault MVC rates in all regions, although not all were statistically significant. Moreover, no one region demonstrated a particularly elevated RR.
Our findings corroborate with and build upon other studies that examined visual field loss as a risk factor for MVCs. Johnson et al. reported drivers with severe binocular visual field loss (although not all attributable to glaucoma) had MVC rates twice as high as controls.22 In a study limited to glaucoma patients, McGwin et al.21 demonstrated that those with mild, moderate, and severe visual defects in the worse functioning eye were 1.9, 3.3, and 6.9-times more likely to be involved in an at-fault MVC, respectively compared to those with no defect; however, there was no such association in the better functioning eye. In our prior study,21 visual field defects were based on the AGIS scoring system, a visual field scoring system developed for clinical trials. In the current study, we extended this research to use TH, TD, and PD to define the extent of the visual field loss, indices that are listed on the print-out of a popularly used visual field testing apparatus. In addition, the prior study defined the extent of the field loss in terms of each eye separately (monocular) whereas the current study investigated patterns of binocular field loss, which is what is relevant for driving; drivers drive with both eyes open.
The RRs for MVC involvement were strongest for TD and PD, specifically for impairments in the upper and left aspects of the visual field. An explanation for these observations is not immediately clear. One explanation is that the A-pillar, the support between the front windshield and the front seat window, in the vehicle restricts a driver’s field of vision, making it more difficult for drivers with field loss in the left region to compensate with more eye and head movements. However, another possibility is that there is no distinct pattern to the RRs and any seeming pattern is simply due to random variation. Despite the lack of statistical significance, there is a general pattern of increased MVC rates among drivers with impaired visual field measurements across all regions of the visual field. From a clinical point of view, none of the estimates were sufficiently strong such that they would support prohibiting patients with glaucoma from driving. Rather, our results suggest that seriously impaired VF parameters should prompt clinicians to begin a dialogue with the patient about driving risks.
This study has several strengths. First, the medical records of all study subjects were reviewed to confirm glaucoma as the primary eye disorder and cause of visual dysfunction. Other eye diseases common in the elderly (e.g. diabetic retinopathy, age-related macular degeneration) that can cause central visual field impairment were excluded. Second, tests of visual field impairment (i.e. TH, TD and PD) that are popularly used in glaucoma management were used to define severity of field defect. Furthermore, visual field impairment was characterized for the binocular visual field (rather than a monocular field), which is how drivers experience the roadway environment. Third, crash data information on MVCs were obtained from the Alabama Department of Public Safety; self-report of crash involvement is known to be unreliable among older adults.31 Procurement of the accident report also allowed us to obtain information on who was responsible for the MVC and limit our analysis to those MVCs in which the study subject was deemed at fault. This study also collected information on person-miles of travel and person-years of travel, thus taking into account driving exposure when calculating MVC rates.
Several study limitations must also be acknowledged in interpreting the results. General health and driving habits were obtained in a telephone survey conducted several years after the beginning of the follow-up period and relied on participants’ ability to recall these characteristics, with 1995 as the reference point. However, there is little reason to suspect a difference among the cases and controls in the ability to recall the requested information accurately, and thus any misclassification should be non-differential and likely to bias our result towards the null. Second, the response rate for the telephone survey was relatively low (approximately 61% overall due). For those who did not complete the survey, multiple imputations were conducted to provide informed estimates for observations with the missing information. Fortunately, the primary independent variable (i.e. visual field defect) was obtained from each patient’s medical record and therefore not vulnerable to survey nonresponse. Moreover, when the adjusted analyses were restricted to patients with complete data, the overall results were highly consistent with the results based on all patients, suggesting that little bias resulted from the imputation process. Lastly, given that drivers move their eyes and heads when driving, it is possible that the observed results are subject to residual confounding of normal eye movements. Some degree of residential confounding may have diminished the associations detected; however, it is unlikely that they would be completely void.
In conclusion, this study suggests that severe binocular visual field impairment defined using a familiar clinical measure is associated with an increased risk of at-fault MVC involvement among older drivers with glaucoma. These results imply that glaucoma patients with high-risk binocular visual field defects have an adverse traffic safety risk. This finding has both practical and clinical relevance for ophthalmologists caring for patients with glaucoma. These measures can provide a clinical marker or set of markers that can be used not only to potentially identify glaucoma patients at risk of MVC involvement but also to begin a dialogue with the patient about driver safety.
Acknowledgments
This research was supported by National Institutes of Health grants R01EY018966, P30AG022838, the EyeSight Foundation of Alabama, the Able Trust, and Research to Prevent Blindness.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Quigley HA, Vitale S. Models of open-angle glaucoma prevalence and incidence in the United States. Invest Ophthalmol Vis Sci. 1997;38:83–91. [PubMed] [Google Scholar]
- 2.Sommer A, Tielsch JM, Katz J, et al. Racial differences in the cause-specific prevalence of blindness in east Baltimore. NEJM. 1991;325:1412–1417. doi: 10.1056/NEJM199111143252004. [DOI] [PubMed] [Google Scholar]
- 3.Prevent Blindness America and National Eye Institute [Accessed March 26, 2013];Vision problems in the U.S.: Prevalence of adult vision impairment and age-related eye disease in America. 2008 at http://www.preventblindness.net/site/DocServer/VPUS_2008_update.pdf.
- 4.Quigley HA. Number of people with glaucoma worldwide. British Journal of Ophthalmology. 1996;80:389–393. doi: 10.1136/bjo.80.5.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson P, Aspinall P, O’Brien C. Patients’ perception of visual impairment in glaucoma: a pilot study. Brit J Ophthalmology. 1999;83:546–552. doi: 10.1136/bjo.83.5.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherwood MB, Garcia-Siekavizza A, Meltzer MI, Hebert A, Burns AF, McGorray S. Glaucoma’s impact on quality of life and its relation to clinical indicators: A pilot study. Ophthalmology. 1998;105:561–566. doi: 10.1016/S0161-6420(98)93043-3. [DOI] [PubMed] [Google Scholar]
- 7.Wilson MR, Coleman AL, Yu F, et al. Functional status and well-being in patients with glaucoma as measured by the medical outcomes study short form-36 questionnaire. Ophthalmology. 1998;105:2112–2116. doi: 10.1016/S0161-6420(98)91135-6. [DOI] [PubMed] [Google Scholar]
- 8.Gutierrez P, Wilson MR, Johnson C, et al. Influence of glaucomatous visual field loss on health-related quality of life. Arch Ophthalmol. 1997;115:777–784. doi: 10.1001/archopht.1997.01100150779014. [DOI] [PubMed] [Google Scholar]
- 9.Parrish RK, II, Gedde SJ, Scott IU, et al. Visual function and quality of life among patients with glaucoma. Arch Ophthalmol. 1997;115:1447–1455. doi: 10.1001/archopht.1997.01100160617016. [DOI] [PubMed] [Google Scholar]
- 10.Turano KA, Geruschat DR, Stahl JW, Massof RW. Perceived visual ability for independent mobility in persons with retinitis pigmentosa. Invest Ophthalmol Vis Sci. 1999;40:865–877. [PubMed] [Google Scholar]
- 11.Turano KA, Massof RW, Quigley HA. A self-assessment instrument designed for measuring independent mobility in RP patients: Generalizability to glaucoma patients. Invest Ophthalmol Vis Sci. 2002;43(9):2874–2881. [PubMed] [Google Scholar]
- 12.Haymes S, LeBlanc R, Nicolela M, Chiasson L, Chauhan B. Glaucoma and on-road driving performance. Invest Ophthalmol Vis Sci. 2008;49(7):3035–3041. doi: 10.1167/iovs.07-1609. [DOI] [PubMed] [Google Scholar]
- 13.Szlyk JP, Taglia DP, Paliga J, Edward DP, Wilensky JT. Driving performance in patients with mild to moderate glaucomatous clinical vision changes. Journal Rehabil Res Dev. 2002;39:467–482. [PubMed] [Google Scholar]
- 14.Szlyk JP, Mahler CL, Seiple W, Edward DP, Wilensky JT. Driving performance of glaucoma patients correlates with peripheral visual field loss. J Glaucoma. 2005;14:145–150. doi: 10.1097/01.ijg.0000151686.89162.28. [DOI] [PubMed] [Google Scholar]
- 15.Adler G, Bauer MJ, Rottunda S, Kuskowski M. Driving habits and patterns in older men with glaucoma. Soc Work Health Care. 2005;40:75–87. doi: 10.1300/J010v40n03_05. [DOI] [PubMed] [Google Scholar]
- 16.Cross JM, McGwin G, Jr, Rubin GS, et al. Visual and medical risk factors for motor vehicle collision involvement among older drivers. Brit J Ophthalmol. 2009;93:400–404. doi: 10.1136/bjo.2008.144584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hu PS, Trumble DA, Foley DJ, al e. Crash risks of older drivers: A panel data analysis. Accid Anal Prev. 1998;30(5):569–581. doi: 10.1016/s0001-4575(98)00019-0. [DOI] [PubMed] [Google Scholar]
- 18.Owsley C, McGwin G, Jr., Ball K. Vision impairment, eye disease, and injurious motor vehicle crashes in the elderly. Ophthal Epidemiol. 1998;5:101–113. doi: 10.1076/opep.5.2.101.1574. [DOI] [PubMed] [Google Scholar]
- 19.Tanabe S, Yuki K, Ozeki N, et al. The association between primary open-angle glaucoma and motor vehicle collisions. Invest Ophthalmol Vis Sci. 2011;52:4177–4181. doi: 10.1167/iovs.10-6264. [DOI] [PubMed] [Google Scholar]
- 20.McGwin G, Mays A, Joiner W, DeCarlo DK, McNeal SF, Owsley C. Is glaucoma associated with motor vehicle collision involvement and driving avoidance. Invest Ophthalmol Vis Sci. 2004;45:3934–3939. doi: 10.1167/iovs.04-0524. [DOI] [PubMed] [Google Scholar]
- 21.McGwin G, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005;46(12):4437–4441. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 22.Johnson CA, Keltner JL. Incidence of visual field loss in 20,000 eyes and its relationship to driving performance. Arch Ophthalmol. 1983;101:371–375. doi: 10.1001/archopht.1983.01040010371002. [DOI] [PubMed] [Google Scholar]
- 23.Wood JM, Dique T, Troutbeck R. The effect of artificial visual impairment on functional visual fields and driving performance. Clin Vision Sci. 1993;8(6):563–575. [Google Scholar]
- 24.Ball K, Owsley C, Stalvey B, Roenker DL, Sloane M, Graves M. Driving avoidance and functional impairment in older drivers. Accid Anal Prev. 1998;30:313–322. doi: 10.1016/s0001-4575(97)00102-4. [DOI] [PubMed] [Google Scholar]
- 25.Coeckelbergh TRM, Cornelissen FW, Brouwer WH, Kooijman AC. The effect of visual field defects on eye movements and practical fitness to drive. Vision Res. 2002;42:669–677. doi: 10.1016/s0042-6989(01)00297-8. [DOI] [PubMed] [Google Scholar]
- 26.McGwin G, Jr, Xie A, Mays A, et al. Visual field defects and the risk of motor vehicle collisions among patients with glaucoma. Invest Ophthalmol Vis Sci. 2005;46:4437–4441. doi: 10.1167/iovs.05-0750. [DOI] [PubMed] [Google Scholar]
- 27.Nelson-Quigg JM, Cello K, Johnson CA. Predicting binocular visual field sensitivity from monocular visual field results. Invest Ophthalmol Vis Sci. 2000;41(8):2212–2221. [PubMed] [Google Scholar]
- 28.Owsley C, Stalvey B, Wells J, Sloane ME. Older drivers and cataract: Driving habits and crash risk. J Gerontol Biol Sci Med Sci. 1999;54A:M203–M211. doi: 10.1093/gerona/54.4.m203. [DOI] [PubMed] [Google Scholar]
- 29.Murakami E, Wagner DP. Comparison between computer-assisted self-interviewing using GPS with retrospective trip reporting using telephone interviews. Federal Highway Administration, U.S. Department of Transportation; Washington DC: 1997. [Google Scholar]
- 30.Federal Highway Administration. Average Annual Miles Per Driver by Age Group. U.S. Department of Transporation, 2011. Accessed December 30, 2012 at http://www.fhwa.dot.gov/ohim/onh00/bar8.htm
- 31.McGwin G, Jr, Owsley C, Ball K. Identifying crash involvement among older drivers: Agreement between self-report and state records. Accid Anal Prev. 1998;30:781–791. doi: 10.1016/s0001-4575(98)00031-1. [DOI] [PubMed] [Google Scholar]