Abstract
Background\Purpose
Despite the intense focus on outcomes following an anterior cruciate ligament (ACL) reconstruction, it is not yet known whether unresolved abnormal hip and trunk neuromuscular control exists. The purpose of this study was to compare trunk and hip kinematics during running, hip abductor and external rotator strength, and trunk control between females who had undergone an ACL reconstruction and healthy control participants.
Methods
We compared 20 ACL reconstructed females to 20 healthy individuals, measuring abduction and external rotation strength, a trunk control test, and performed an instrumented gait evaluation during running. Comparisons between groups were made for non-sagittal peak hip angles, forward trunk lean, trunk ipsilateral lean at initial contact, trunk control and hip abduction and external rotation strength.
Results
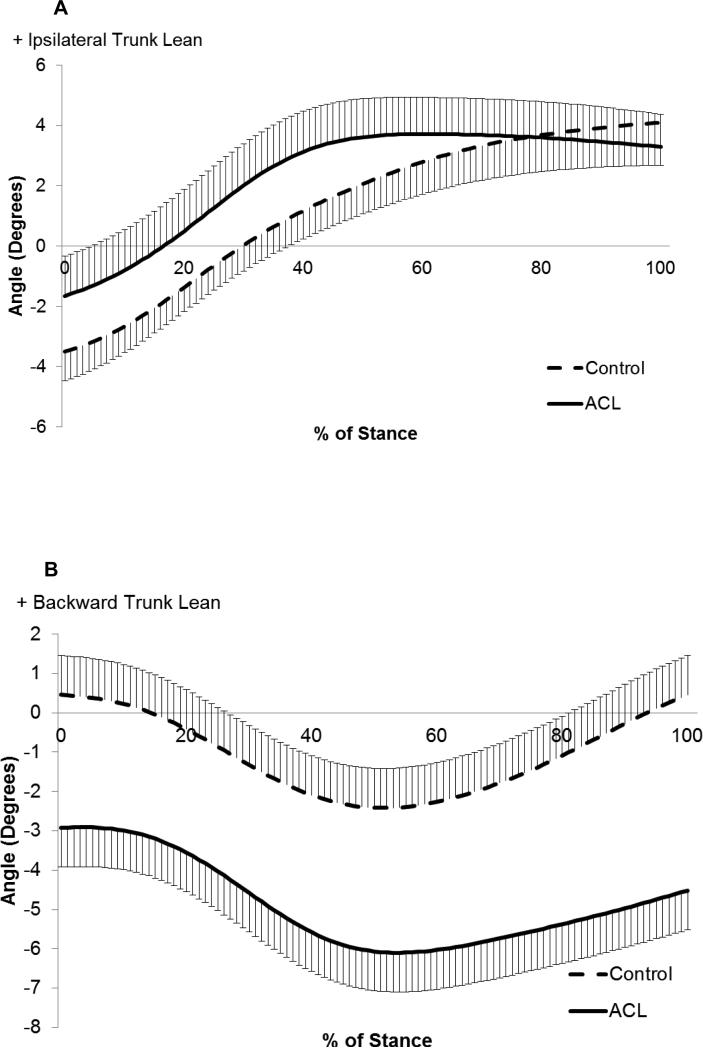
We found no significant differences in hip abduction (p = 0.25), hip external rotation strength (p = 0.63), peak hip adduction (p = 0.11) or hip internal rotation angle (p = 0.47). The ACL group did have a significantly greater ipsilateral trunk lean (p = 0.028), forward lean (p = 0.004), and had higher errors on the trunk stability test (p = 0.007).
Conclusion
We found significant differences in trunk control, suggesting further attention should be devoted to this component of rehabilitation.
Keywords: biomechanics, strength, trunk, knee, running
Introduction
An estimated 150,000-200,000 anterior cruciate ligament (ACL) tears occur annually in the United States [1]. Growing evidence suggests that these individuals remain at an elevated injury risk even after surgical reconstruction [2, 3]. Potential factors include muscular weakness and poor neuromuscular control of the trunk and injured limb [2, 4-6] [3, 7]. While performance deficits on hop tests and quadriceps strength are well defined after rehabilitation, little is known of the potential deficits in the hip and trunk neuromuscular function that may persist following rehabilitation for a ACL reconstruction [6].
Trunk neuromuscular control has been identified as an important risk factor for initial ACL injury. Several studies have shown that individuals who tear their ACL land with greater forward and ipsilateral trunk lean (leaning of the trunk over the injured stance limb,) [8-10] and have diminished capacity to resist trunk perturbations on laboratory based tests [11, 12]. Also, injury prevention programs focused on improving trunk neuromuscular control have been successful in reducing injury rates among female athletes [13-15]. A recent review has highlighted the lack of evidence for the specific role of trunk neuromuscular control exercises in lower extremity injury prevention programs, highlighting the need for continued research in this area [16]. While the trunk has been established as an important risk factor for initial injury, whether trunk control improves at all after surgical reconstruction of the ACL has not been as well studied [11, 12]. Also, potential identification of altered trunk neuromuscular control after surgery in lower level tasks, such as running and functional tests, could provide the clinician with an earlier time point to intervene before the individual has returned to high risk maneuvers such as jumping and cutting or has finished rehabilitation.
The hip plays a central role in the maintenance of stability between the trunk and knee during athletic tasks [17]. Dysfunction of the hip, may lead to altered knee loading, thus increasing the risk for injury [17, 18]. For example, weakness of the hip external rotator muscles has been shown to be predictive of who will have a second ACL tear [5]. Also, weakness of the hip abductor and external rotator muscles may result in greater hip adduction and internal rotation during dynamic tasks such as running and jumping, resulting in a compensatory ipsilateral trunk lean to maintain stability [17]. Interestingly, such a movement pattern after surgery would be very similar to the mechanics proposed as a mechanism of non-contact ACL injuries [19, 20]. To date, presence of hip abductor and external rotator weakness has been limited to one study which found no differences in strength between those with and those without an ACL reconstruction [21]. While informative, the study included both males and females who may have had differing strength profiles. The study also did not assess whether neuromuscular control of the hip is altered in those who have had an ACL reconstruction.
Despite tremendous gains in the understanding of knee recovery after an ACL reconstruction and understanding how proximal joints contribute to initial ACL injury, little is known on how these joints function after surgery, and whether abnormal functions still exists or is altered by rehabilitation. Therefore, the purpose of this paper was to assess trunk and hip neuromuscular control between a cohort of ACL patients who had recently completed rehabilitation to a healthy non-injured cohort. We hypothesized that compared to a healthy control group, the ACL patients would have poorer trunk control (as evidenced by greater forward trunk lean and ipsilateral side bending at initial contact during running, and as measured by a trunk control test), higher peak non-sagittal hip joint angles during running, and decreased non-sagittal hip strength.
Methods
Females between the ages of 16-40 were recruited for this study. Before beginning testing procedures all participants signed informed consent documents approved by the institutional review board. Individuals in the ACL cohort were recruited from the same orthopedic practice and could have had either a bone-patellar-bone or hamstring auto-graft . Also, they could have had a meniscus repair. The participant was required to have been cleared by their physician to return to sport, and have completed rehabilitation. The matched control group could not have had any previous surgeries or other conditions that may have affected their gait. Both groups completed a Tegner activity scale with the ACL cohort planning to return to sports with a minimum level of a 5 on the scale [22]. The matched control subjects were then matched to the ACL cohort for both the Tegner scale within ±2 and age ±5 years.
Following the completion of the initial intake forms, hip strength was assessed. Hip abduction and external rotation strength were determined following established protocols that have been shown to be reliable[23, 24] [25]. Hip abductor strength was assessed by placing the participant in a side lying position. They were instructed to attempt to raise the upper leg toward the ceiling while pressing against a hand held dynamometer (Lafayette Instruments, Lafayette, IN) placed 5 cm proximal to the tibiofemoral joint line that was secured with a stabilization strap. The external rotator muscles were assessed with the participant sitting in a chair with back support. Their thigh was then stabilized with a strap and they were instructed to push into the dynamometer which was placed on the medial aspect of the leg 5 cm superior to the ankle joint. For both strength tests, the participants were instructed to gradually increase how much they were pushing over three seconds and then hold their maximum effort for the next two seconds. One practice trial was performed followed by three testing trials. The values from the testing trials were then averaged for each participant and the raw force values normalized by segment length (as measured from the greater trochanter to the lateral joint line of the knee for the thigh and from the lateral joint line of the knee to the lateral malleolus for the tibia) and body mass.
The trunk control test was then performed. This test was modeled as a clinical version of the unstable trunk sitting test which has been previously used as a valid and reliable laboratory based test to assess differences in trunk control in patients with a variety of impairments [26, 27]. To perform the test the participant was asked to sit on a Swiss ball with both feet planted firmly on the ground. The ankle was placed in a neutral position, the knee in 90 degrees of flexion and the hips in 90 degrees of flexion (Figure 1). They were also asked to sit straight up and fold their arms. An initial practice trial was performed where they were instructed to keep their eyes open and lift one leg for 30 seconds, followed by the other leg for 30 seconds. In order to standardize the position of the raised leg, the subject was instructed to extend the knee so that the heel was at the same height as the ankle on planted foot (Figure 1). Following the practice trial, 3 trials per leg were collected where the individual repeated the same testing procedures except with their eyes closed. The individual was allowed to choose which leg to initially start with and then alternated legs between each trial. During the testing if they lost their balance they were instructed to regain a stable position as quickly as possible and continue with the test until the 30 second trial had ended. Errors that were tracked consisted of: foot touched the ground, reached for table, arms uncrossed, eyes opened, the knee of the lifted leg rested against the knee of the planted leg, or the planted foot shifting side to side or lifting off. If they were unable to return to the test position within 1 second of committing an error additional errors were assessed. For example, if they placed their foot on the ground and held it there for 4 seconds, 4 errors were assessed. The participant was placed between two objects, which could include tables, chairs or a next to a wall, such that if they lost balance they could reach for these objects to help them regain stability. The total number of errors per leg where then averaged for each participant. As part of the development of the methods we assessed the within session measurement error and reliability within the ACL cohort. We have found a measurement error of 0.25 errors as calculated by the typical error [28]. Also the within session reliability as quantified by an intraclass correlation coefficient (3,k) was found to be 0.93. To assess the effect of the potential of the reconstructed limb affecting the results of the trunk control test, we compared not only to the control group but between the injured and non-injured leg in the reconstructed group.
Figure 1.
Trunk Stability test: The participant first sits on a Swiss ball with their ankle in a neutral position, their knee flexed to 90 degrees and their hips flexed to 90 degrees. They then cross their arms and lift one foot slightly up and forward. After a practice test with the eyes open the participant closes their eyes and repeats the test. Breaking from this position is recorded as an error if one of the 6 following deviations was noted: Lifted foot touches the ground, they reach for the table\wall\chair, their planted foot shifts, the arms come uncrossed (but do not touch the table), they rest the lifted knee against the planted leg, or they open their eyes. To assist with the participant regaining stability if they lost balance two solid objects were placed on either side of them within reaching distance, these objects could include chairs, tables or a wall.
Following the assessment of hip strength and trunk control, running gait was recorded. First, retro-reflective markers were placed on the participant following previously established procedures for the placement of the tracking clusters on the thighs, shanks, and heels [29]. The anatomical markers were placed on the posterior aspect of the acromioclavicular joint, iliac crests, greater trochanters, femoral epicondyles, tibial plateaus, malleoli, as well as the first and fifth metatarsal heads. Additional tracking markers for the trunk were placed on the C7 vertebrae, the sternum, with the markers on the acromioclavicular joint also serving as tracking markers. All participants wore a New Balance WR662 (New Balance, Brighton, MA, USA) running shoe. After the application of the anatomical markers and the recording of the functional hip joint center trial, the participant warmed up at a self-selected walking speed for 5 minutes on an instrumented treadmill (Bertec Corporation, Columbus, OH). Following the warm-up period marker trajectories and force plate data were then recorded while the participant ran at their own self-selected speed for 2 minutes. The matched control participant ran within 0.2 m\s of the same speed as the ACL patient for whom they were matched to. Three-dimensional marker trajectories and force plate data were collected at 200 Hz using a 15 camera motion analysis system (Motion Analysis Corporation) and at 1200 Hz, respectively.
The data was processed with Visual 3D software (C-motion, Germantown, MD, USA). The data was filtered with a fourth-order low-pass zero-lag Butterworth filter at 8 Hz for marker trajectories and 35 Hz for force plate data. We choose the cutoff frequencies from a residual analysis of the data [30]. A functional hip joint center was calculated [31]. Hip and knee joint angles were calculated using an x-y-z Cardan angle sequence, referencing the distal segment to the proximal. Whereas the trunk angles used the same Cardan angle sequence but were calculated relative to the global coordinate system. The joint coordinate systems were determined from previously published procedures [32]. Joint moments were calculated from the proximal end of the distal segment and were normalized to body mass and height. A custom LabView code (National Instruments, Austin, TX, USA) was subsequently utilized to extract the peak angles during the first 75% of stance phase including, forward trunk bend, hip adduction, and hip internal rotation. We chose to capture trunk sidebending (ipsilateral lean), at the time of initial contact, as trunk lean during this period of stance has previously been found to be linked to injury while performing other activities such as jumping [8-10]. Data were collected from five trials for each subject, and then averaged to give discrete variables. Additionally, ensemble graphs were created by averaging the 5 individual trials per subject and then averaging that trial across each group. Because of this ensemble graphs may not directly match the values as reported in the discrete variables. The injured limb of the ACL patient was compared to the same limb in the matched control participant. Using SPSS (SPSS Inc., Chicago, IL), means, standard deviations, and group differences were determined using independent t-tests. Also effect sizes for each group were determined. The dependent variables assessed between the ACL group and healthy control were as follows, peak hip frontal and transverse plane angles. We also assessed ipislateral and forward trunk bending at the time of initial contact, hip abduction and external rotation strength, as well errors on the trunk control test. As a secondary analysis to better understand how the trunk may have affected the knee, we also assessed peak knee flexion angle and the knee extensor moment. Lastly, we also compared the error rate between limbs within the ACL cohort during the trunk control test with a paired t-test.
Results
There were a total of 20 ACL and 20 healthy control subjects enrolled into the study. The ACL and control participants were equally balanced for age (21.1 ± 5.9 years old, vs 22.8 ± 3.1 years old) and Tegner activity levels (6.5±1.6, vs, 6.8±1.5). The average time between injury and ACL reconstruction was 51.5 ± 52 days, and the average time between surgery and testing was 222.2 ± 44 days. The participants ran on the treadmill at 2.8 ± 0.27 m\s. We found no significant differences between the ACL group and the control group for hip angles (Table 1). However, significant differences were found at the trunk with the ACL group having significantly greater lean towards the ipsilateral side and forward trunk lean (Figure 2). While no significant differences were found between groups for hip abduction and external rotation strength the ACL group did have significantly greater errors on the trunk control test when either the injured on non-injured limb was compared to the control group (p = 0.00) (Table 1). We also found that there was no significant difference between limbs (p = 0.17) in the error rate on the trunk control test. Lastly, there was no significance difference in knee flexion angle between groups, but the ACL group did utilize a significantly smaller knee extensor moment (Table 1).
Table 1.
Variables of interest: Peak hip adduction, peak hip internal rotation, trunk side bending (ipsilateral trunk lean at the time of initial contact) , and peak knee extensor moment are all positive. Peak knee flexion angle and peak (forward) trunk lean angle are both negative.
| Variables | ACL group | Normal group | Difference | P-value | Effect Size |
|---|---|---|---|---|---|
| Peak hip adduction (deg) | 18.0 ± 4.9 | 15.9± 3.8 | 2.1 | 0.11 | 0.47 |
| Peak hip internal rotation (deg) | 11.1 ± 5.2 | 12.3± 5.6 | −1.2 | 0.47 | 0.22 |
| Trunk sidebending at initial contact (deg) | −2.0 ± 2.7 | −3.7± 1.9 | 1.7 | 0.02 | 0.72 |
| Peak Trunk lean (deg) | −6.3 ± 4.9 | −2.1± 3.5 | −4.2 | 0.00 | 0.98 |
| Hip Abduction strength (Nm/kg) | 16.0± 4.7 | 14.5± 3.5 | 1.5 | 0.25 | 0.36 |
| Hip external rotation strength (Nm/kg) | 6.9± 4.4 | 6.4± 1.5 | 0.5 | 0.63 | 0.15 |
| Trunk control test errors (injured limb down) | 7.3 ± 5.6 | 3.2± 3.1 | 4.1 | 0.00 | 0.90 |
| Trunk control test errors (non-injured limb down) | 5.8± 5.1 | 1.3± 1.1 | 4.5 | 0.00 | 1.22 |
| Peak knee Extension (deg) | −45.0± 6.3 | −47.6± 4.7 | 2.6 | 0.15 | 0.46 |
| Peak knee Extensor Moment (Nm/kg*height) | 0.8± 0.3 | 1.1± 0.3 | −0.3 | 0.01 | 1.00 |
Figure 2.
Ensemble curves of (a) ipsilateral trunk lean (trunk lean towards the stance leg is positive) and (b) Trunk lean (forward is negative) during stance. Solid line represents the ACL group, the dashed the control group, and the hash lines represent half of the standard deviation.
Discussion
The purpose of this study was to assess the proximal compensations in neuromuscular control and strength that occur as the result of an ACL reconstruction in female athletes. Our hypotheses were partially supported in that we did find that the ACL cohort had significantly higher errors on the trunk control test as well as a greater forward and ipsilateral trunk lean. However, no differences were found between groups for frontal and transverse plane hip strength and kinematics. These findings suggest that trunk neuromuscular control does not resemble healthy non-injured individuals, even after rehabilitation during activities that are deemed low impact, such as running.
While altered trunk neuromuscular control is cited as a common feature in non-contact ACL injuries in females, whether this persists following surgical reconstruction has not been well investigated to date [11-13]. In the current study, we found that those who had an ACL reconstruction made initial contact when running with their trunk positioned in less trunk lean towards the contralateral side than the control group, and as can be seen in Figure 2a transitioned to the ipislateral side sooner. Although the difference between the groups was modest (1.7 degrees), it was significantly different and associated with a large effect size, indicating a good degree of separation between the population distributions. While still speculative, the observed movement pattern may reflect a bias to land towards the injured side, which may leave the individual at higher risk for subsequent injuries when they go onto perform more high risk type movements such as jumping or cutting. Lastly, it is important to note that due to the cross sectional nature of the study, we are unable to define if the observed differences pre-dated the initial ACL injury, or are a consequence of the injury.
We also observed that the individuals in the ACL cohort ran with significantly greater forward trunk lean. This could have served as a compensation to reduce the knee extensor moment. To assess this possibility we conducted a secondary analysis of the sagittal plane knee kinematics and found no significant difference in knee flexion angle, but a significantly smaller knee extensor moment in the ACL cohort. The greater forward trunk lean observed in running is similar to what has been observed in jump landing tasks after an ACL reconstruction [33]. The greater forward trunk lean, may shift the center of mass forward, and consequently reduce the knee extensor moment [33]. If this compensation is maintained, it could reduce the demands on the quadriceps and perhaps contribute to the long term strength and activation deficits observed in this population [34, 35]. We cannot completely rule out that the smaller knee extensor moment may have been due to other reasons such as greater co-contraction of the hamstring muscles. Results from simulation studies have shown greater forward trunk lean may actually enhance hamstring activation and reduce the strain on the ACL [36]. Future research is needed to determine the optimal amount of forward trunk lean to help reduce ACL graft strain, while not contributing to long term reductions in the demands of the quadriceps.
The ACL cohort had a significantly higher number of errors during the trunk control test. Interestingly, we found no significant differences in the error rates regardless of what foot was planted on the ground. This would suggest that the error rate was not dependent on proprioceptive sense or control stemming from the reconstructed knee. The influence of the ankle, knee, and hip were also minimized by placing participants at 90 degrees [37]. By having the individual close their eyes the visual input to the maintenance of trunk postural control was further removed, resulting in participants relying more on their vestibular and proprioceptive systems to maintain their center of mass over their center of gravity [38]. The greater error rate in the ACL group suggests that these individuals were less adapted to use their vestibular and proprioceptive systems to maintain stability. As visual attention is often focused elsewhere during an athletic event, being able to appropriately rely on these systems may be a critical factor to further assess. Since the perturbations were generated internally and were relativity small, control was largely determined by the smaller postural muscles [39]. Further studies utilizing electromyography are needed to quantify which muscles are most active in those with good and poor error rates. While additional research is needed in this area, this test is easy to implement in a clinic and could help assess progress of trunk neuromuscular control in patients who have had an ACL reconstruction.
Altered hip strength and kinematics has been reported in individuals at risk for tearing their ACL, and is postulated to be a critical component of post-operative rehabilitation [4, 40]. In the current study we found no differences in hip strength or frontal and transverse plane kinematics in the ACL group when compared to the healthy control group. Our results are also in agreement with a recent mixed gender study assessing hip strength after an ACL reconstruction[21] . While there were no significant differences between groups, it may be that those with the weakest hip muscles are still at risk for a subsequent injury. In support of this premise a recent study found significantly greater hip transverse plane hip kinematics and lower hip external rotator strength in those who go onto have a second ACL tear [5].
There are several limitations to note in the current study. First, the study was cross sectional in design, and we cannot determine if the observed alterations in neuromuscular control are directly related to subsequent injury risk. Second, the strength testing for hip abduction and external rotation was done isometrically, which does not reflect how these muscles perform during dynamic activities. However, the strength testing protocol has been used in other populations where significant differences in strength were reported [25]. Lastly, while we are able to show an overall difference in trunk control, we are unable to determine which specific muscles or systems are responsible for the observed abnormal control. In addition, we were unable to directly compare the results we obtained from the trunk control test to earlier experimental approaches that described alterations in center of mass using the unstable trunk sitting test [26, 27]. Future studies are needed to compare how well clinical versions of trunk control compare to previously used and validated laboratory based tests.
In conclusion, we found significant differences in trunk, but not hip neuromuscular control, during running at the completion of the rehabilitation program for patients with an ACL reconstruction. The greater error rates in the ACL cohort during the trunk control test suggest there could be unresolved deficits in trunk control in this cohort. Our hypotheses for hip abduction and external rotation strength were not supported, in that there was no difference between the groups. These results suggest that alterations in trunk control persist at the end of rehabilitation and they can be observed during relativity low load\intensity conditions.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the National Institute of Arthritis And Musculoskeletal And Skin Diseases of the National Institutes of Health under Award Number K23AR062069. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Frank CB, Jackson DW. The science of reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 1997;79:1556–76. doi: 10.2106/00004623-199710000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of contralateral and ipsilateral anterior cruciate ligament (ACL) injury after primary ACL reconstruction and return to sport. Clin J Sport Med. 2012;22:116–21. doi: 10.1097/JSM.0b013e318246ef9e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barber-Westin SD, Noyes FR. Objective criteria for return to athletics after anterior cruciate ligament reconstruction and subsequent reinjury rates: a systematic review. Phys Sportsmed. 2011;39:100–10. doi: 10.3810/psm.2011.09.1926. [DOI] [PubMed] [Google Scholar]
- 4.Hewett TE, Di Stasi SL, Myer GD. Current Concepts for Injury Prevention in Athletes After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2013;41:216–224. doi: 10.1177/0363546512459638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paterno MV, Schmitt LC, Ford KR, Rauh MJ, Myer GD, Huang B, Hewett TE. Biomechanical Measures During Landing and Postural Stability Predict Second Anterior Cruciate Ligament Injury After Anterior Cruciate Ligament Reconstruction and Return to Sport. Am J Sports Med. 2010;38:1968–1978. doi: 10.1177/0363546510376053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schmitt LC, Paterno MV, Hewett TE. The impact of quadriceps femoris strength asymmetry on functional performance at return to sport following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2012;42:750–9. doi: 10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.ACL injuries in the female athlete : causes, impacts, and conditioning programs. Springer; New York: 2013. [Google Scholar]
- 8.Olsen OE, Myklebust G, Engebretsen L, Bahr R. Injury mechanisms for anterior cruciate ligament injuries in team handball: a systematic video analysis. Am J Sports Med. 2004;32:1002–12. doi: 10.1177/0363546503261724. [DOI] [PubMed] [Google Scholar]
- 9.Krosshaug T, Nakamae A, Boden BP, Engebretsen L, Smith G, Slauterbeck JR, Hewett TE, Bahr R. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359–67. doi: 10.1177/0363546506293899. [DOI] [PubMed] [Google Scholar]
- 10.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. Br J Sports Med. 2009;43:417–22. doi: 10.1136/bjsm.2009.059162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanicalepidemiologic study. Am J Sports Med. 2007;35:1123–30. doi: 10.1177/0363546507301585. [DOI] [PubMed] [Google Scholar]
- 12.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35:368–73. doi: 10.1177/0363546506297909. [DOI] [PubMed] [Google Scholar]
- 13.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes. A prospective study. Am J Sports Med. 1999;27:699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 14.Emery CA, Rose MS, McAllister JR, Meeuwisse WH. A prevention strategy to reduce the incidence of injury in high school basketball: a cluster randomized controlled trial. Clin J Sport Med. 2007;17:17–24. doi: 10.1097/JSM.0b013e31802e9c05. [DOI] [PubMed] [Google Scholar]
- 15.Gilchrist J, Mandelbaum BR, Melancon H, Ryan GW, Silvers HJ, Griffin LY, Watanabe DS, Dick RW, Dvorak J. A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players. Am J Sports Med. 2008;36:1476–83. doi: 10.1177/0363546508318188. [DOI] [PubMed] [Google Scholar]
- 16.Briggs MS, Givens DL, Best TM, Chaudhari AM. Lumbopelvic neuromuscular training and injury rehabilitation: a systematic review. Clin J Sport Med. 2013;23:160–71. doi: 10.1097/JSM.0b013e318280aabb. [DOI] [PubMed] [Google Scholar]
- 17.Powers CM. The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. J Orthop Sports Phys Ther. 2010;40:42–51. doi: 10.2519/jospt.2010.3337. [DOI] [PubMed] [Google Scholar]
- 18.Reiman MP, Bolgla LA, Lorenz D. Hip functions influence on knee dysfunction: a proximal link to a distal problem. J Sport Rehabil. 2009;18:33–46. doi: 10.1123/jsr.18.1.33. [DOI] [PubMed] [Google Scholar]
- 19.Chaudhari AM, Andriacchi TP. The mechanical consequences of dynamic frontal plane limb alignment for non-contact ACL injury. Journal of Biomechanics. 2006;39:330–8. doi: 10.1016/j.jbiomech.2004.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Dempsey AR, Lloyd DG, Elliott BC, Steele JR, Munro BJ, Russo KA. The effect of technique change on knee loads during sidestep cutting. Med Sci Sports Exerc. 2007;39:1765–73. doi: 10.1249/mss.0b013e31812f56d1. [DOI] [PubMed] [Google Scholar]
- 21.Thomas AC, Villwock M, Wojtys EM, Palmieri-Smith RM. Lower Extremity Muscle Strength After Anterior Cruciate Ligament Injury and Reconstruction. J Athl Train. 2013 doi: 10.4085/1062-6050-48.2.14. online ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985:43–9. [PubMed] [Google Scholar]
- 23.Jaramillo J, Worrell TW, Ingersoll CD. Hip isometric strength following knee surgery. J Orthop Sports Phys Ther. 1994;20:160–5. doi: 10.2519/jospt.1994.20.3.160. [DOI] [PubMed] [Google Scholar]
- 24.Cahalan TD, Johnson ME, Liu S, Chao EY. Quantitative measurements of hip strength in different age groups. Clin Orthop Relat Res. 1989:136–45. [PubMed] [Google Scholar]
- 25.Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671–6. doi: 10.2519/jospt.2003.33.11.671. [DOI] [PubMed] [Google Scholar]
- 26.van der Burg JC, van Wegen EE, Rietberg MB, Kwakkel G, van Dieen JH. Postural control of the trunk during unstable sitting in Parkinson's disease. Parkinsonism Relat Disord. 2006;12:492–8. doi: 10.1016/j.parkreldis.2006.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Cholewicki J, Polzhofer GK, Radebold A. Postural control of trunk during unstable sitting. J Biomech. 2000;33:1733–7. doi: 10.1016/s0021-9290(00)00126-3. [DOI] [PubMed] [Google Scholar]
- 28.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30:1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 29.Noehren B, Pohl MB, Sanchez Z, Cunningham T, Lattermann C. Proximal and distal kinematics in female runners with patellofemoral pain. Clin Biomech (Bristol, Avon) 2012;27:366–71. doi: 10.1016/j.clinbiomech.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Winter DA. Biomechanics and motor control of human movement. 3rd ed. John Wiley & Sons; Hoboken, New Jersey: 2005. [Google Scholar]
- 31.Schwartz MH, Rozumalski A. A new method for estimating joint parameters from motion data. Journal of Biomechanics. 2005;38:107–16. doi: 10.1016/j.jbiomech.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 32.Noehren B, Pohl MB, Sanchez Z, Cunningham T, Lattermann C. Proximal and distal kinematics in female runners with patellofemoral pain. Clinical Biomechanics. 2012;27:366–71. doi: 10.1016/j.clinbiomech.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oberlander KD, Bruggemann GP, Hoher J, Karamanidis K. Altered landing mechanics in ACL-reconstructed patients. Med Sci Sports Exerc. 2013;45:506–13. doi: 10.1249/MSS.0b013e3182752ae3. [DOI] [PubMed] [Google Scholar]
- 34.Hart JM, Pietrosimone B, Hertel J, Ingersoll CD. Quadriceps Activation Following Knee Injuries: A Systematic Review. J Athl Train. 2010;45:87–97. doi: 10.4085/1062-6050-45.1.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Palmieri-Smith RM, Thomas AC, Wojtys EM. Maximizing quadriceps strength after ACL reconstruction. Clin Sports Med. 2008;27:405–24. vii–ix. doi: 10.1016/j.csm.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 36.Kulas AS, Hortobágyi T, DeVita P. Trunk position modulates anterior cruciate ligament forces and strains during a single-leg squat. Clin Biomech. 2012;27:16–21. doi: 10.1016/j.clinbiomech.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 37.van Dieen JH, Koppes LL, Twisk JW. Postural sway parameters in seated balancing; their reliability and relationship with balancing performance. Gait Posture. 2010;31:42–6. doi: 10.1016/j.gaitpost.2009.08.242. [DOI] [PubMed] [Google Scholar]
- 38.Silfies SP, Cholewicki J, Radebold A. The effects of visual input on postural control of the lumbar spine in unstable sitting. Hum Mov Sci. 2003;22:237–52. doi: 10.1016/s0167-9457(03)00046-0. [DOI] [PubMed] [Google Scholar]
- 39.Hibbs AE, Thompson KG, French D, Wrigley A, Spears I. Optimizing performance by improving core stability and core strength. Sports Med. 2008;38:995–1008. doi: 10.2165/00007256-200838120-00004. [DOI] [PubMed] [Google Scholar]
- 40.Myer GD, Paterno MV, Ford KR, Hewett TE. Neuromuscular training techniques to target deficits before return to sport after anterior cruciate ligament reconstruction. J Strength Cond Res. 2008;22:987–1014. doi: 10.1519/JSC.0b013e31816a86cd. [DOI] [PubMed] [Google Scholar]