Abstract
Purpose
To evaluate changes in anterior corneal topography and higher-order aberrations (HOA) after 14-days of rigid gas-permeable (RGP) contact lens (CL) wear in keratoconus subjects comparing two different fitting approaches.
Methods
Thirty-one keratoconus subjects (50 eyes) without previous history of CL wear were recruited for the study. Subjects were randomly fitted to either an apical-touch or three-point-touch fitting approach. The lens’ back optic zone radius (BOZR) was 0.4 mm and 0.1 mm flatter than the first definite apical clearance lens, respectively. Differences between the baseline and post-CL wear for steepest, flattest and average corneal power (ACP) readings, central corneal astigmatism (CCA), maximum tangential curvature (KTag), anterior corneal surface asphericity, anterior corneal surface HOA and thinnest corneal thickness measured with Pentacam were compared.
Results
A statistically significant flattening was found over time on the flattest and steepest simulated keratometry and ACP in apical-touch group (all p < 0.01). A statistically significant reduction in KTag was found in both groups after contact lens wear (all p < 0.05). Significant reduction was found over time in CCA (p = 0.001) and anterior corneal asphericity in both groups (p < 0.001). Thickness at the thinnest corneal point increased significantly after CL wear (p < 0.0001). Coma-like and total HOA root mean square (RMS) error were significantly reduced following CL wearing in both fitting approaches (all p < 0.05).
Conclusion
Short-term rigid gas-permeable CL wear flattens the anterior cornea, increases the thinnest corneal thickness and reduces anterior surface HOA in keratoconus subjects. Apical-touch was associated with greater corneal flattening in comparison to three-point-touch lens wear.
Keywords: Cornea, Keratoconus, Contact lenses
Resumen
Objetivo
Evaluar los cambios en la topografía corneal anterior y las aberraciones de alto orden (HOA) a los 14 días de uso de lentes de contacto rígidas permeables al gas (RGP) en pacientes con queratocono, comparando dos tipos diferentes de adaptación.
Métodos
Se incluyó en el estudio a treinta y un sujetos con queratocono (50 ojos), sin historia previa de uso de lentes de contacto. A los sujetos se les aplicó aleatoriamente un procedimiento de adaptación de toque apical o de tres puntos. Radio base (BOZR) de la lente fue de 0,4 mm, y 0,1 mm más plano que las primeras lentes que proporcionaban claridad apical, respectivamente. Se compararon las diferencias entre la visita de inicio y tras el uso de las lentes, de las mediciones de potencia corneal media, en el meridiano más plano y más curvo, el astigmatismo central corneal (CCA), la curvatura tangencial máxima (KTag), la asfericidad de la superficie corneal anterior, las HOA de la superficie corneal anterior y el grosor corneal más fino, utilizando el sistema Pentacam.
Resultados
Se encontró un aplanamiento estadísticamente significativo en el tiempo, de las lecturas queratométricas más plana y más curva así como de la potencia media de la córnea, en el grupo de toque apical (todos p < 0,01). Se detectó una reducción estadísticamente significativa de la KTag en ambos grupos tras el uso de lentes de contacto (todas las p < 0,05). Se observó una reducción significativa en el tiempo del CCA (p = 0,001) y de la asfericidad corneal anterior en ambos grupos (p < 0,001). El grosor en el punto corneal más fino se incrementó considerablemente tras el uso de las lentes (p < 0,0001). Se redujeron considerablemente el coma y el error cuadrático medio asociado a las HOA tras el uso de las lentes de contacto con ambos procedimientos de adaptación (p < 0,05).
Conclusión
El uso de lentes de contacto rígidas permeables al gas aplana la córnea anterior, incrementa el espesor del punto más fino de la córnea, y reduce las HOA de la superficie anterior en pacientes con queratocono. La adaptación de toque apical está asociada a un mayor aplanamiento de la córnea en comparación con la adaptación tres puntos.
Palabras clave: Córnea, Queratocono, Lentes de contacto
Introduction
Corneal rigid gas-permeable (RGP) contact lenses still represent the most common and successful management option for mild to moderate cases of keratoconus because these lenses can mask relatively high levels of irregular astigmatism and thus substantially improve visual acuity.1 Additionally, most keratoconus subjects report wearing these lenses comfortably throughout the day.1,2
Three fitting approaches have been described to fit corneal RGP in keratoconus: (1) apical-touch (lens bears on corneal apex), (2) three-point-touch (lens’ bearing is shared between corneal apex and mid periphery), and (3) apical-clearance (lens bears on mid periphery without apical-touch).3
The use of corneal RGP contact lenses has been shown to induce topographical changes on the cornea in normal control subjects4,5 as well as in subjects with keratoconus.6 In normal subjects, corneal curvature changes observed following RGP contact lens wear are related to the type of contact lens worn and the number of years of lens wear.5 It has been reported that apical-touch fitting causes central corneal flattening in keratoconus,7 whereas apical-clearance fitting causes central corneal steepening,8 which could be confounded with the normal progression of keratoconus disease, so apical-clearance fitting approach is not normally used. Zadnik and Mutti9 previously discussed that apical-touch fitting of RGP lenses might ‘mold’ the keratoconic cornea by exerting pressure on the cone apex, thereby forcing the anterior surface to conform with the RGP lens’ back surface. Hwang et al. have reported RGP contact lens wear fitted with three-point-touch fitting approach in keratoconus subjects caused corneal flattening after two years of wear.2 More recently, Jinabhai and co-workers reported that both visual acuity and thickness at the thinnest corneal point decreased and corneal curvature and corneal higher-order aberrations (HOA) increased after ceasing RGP contact lens wear for 1 week in keratoconus subjects who had been wearing these lenses, mostly fitted with the apical-touch fitting approach, for an average of 7 years.10 Therefore, corneal curvature, shape, thickness and anterior surface higher-order aberrations are altered following RGP lens wear in keratoconus subjects who have been wearing corneal RGP contact lens for a long period of time. However, to the best of our knowledge, no previous studies have reported corneal changes induced by a short period of corneal RGP lens wear in neophyte contact lens wearers with keratoconus in a clinical context. Those changes might have implications in the lens-to-cornea relationship, lens parameters and lens power prescribed. To clarify this question it is necessary to know whether corneal changes observed after short periods of time within the initial period of fitting and adaptation are similar to the changes reported by other authors. Thus, the present study assessed changes on the anterior corneal surface induced by RGP lenses fitted according two different approaches over a period of 14 days. This time of contact lenses adaptation was decided because subjects were neophyte contact lens wearers. As it is known, some subjects experienced some discomfort when they begin to wear RGP contact lenses and it takes longer for them to be able to wear lenses 8 or more hours a day. In order to be sure that subjects were wearing contact lenses at least 8 h a day, we decided to give them two weeks to get used to contact lenses and wearing them at least 8 h a day before to acquire a new topography.
Materials and methods
Subjects with keratoconus and no previous history of contact lens wear were included in the study. Comprehensive optometric and ophthalmic examinations were performed in all subjects including the assessment of uncorrected and corrected logMAR visual acuities, anterior segment biomicroscopy, fundus examination, and keratometry. In addition, a corneal topographic examination was performed using the Pentacam Eye Scanner (Software version 1.16.r:23, Oculus Inc., Wetzlar, Germany). All topographic examinations were taken by the same examiner (M R-J). The Pentacam system is based on a rotation Sheimpflug camera that can take 12–50 single captures to reconstruct a 3D anterior segment image. In the present study, anterior segment Pentacam examinations were produced with 25 single captures within 2 s. The results obtained with Pentacam were checked under the device's quality specification window; only the correct measurements (i.e. “quality specifications” reads OK) were accepted; if the comment was marked yellow or red, the examination was repeated. As it has been previously reported that the Pentacam instrument provides high sensitivity and specificity in keratoconus detection,11,12 as well as high reproducibility and repeatability in measuring corneal thickness13,14 and corneal power15 a single Pentacam examination was acquired for each eye.
Keratoconus diagnosis was performed according to the keratoconus severity score described by the CLEK study group.16 The keratoconus grading was based on average central corneal power (ACP) and HOA Root Mean Square error (RMS) as mild (ACP ≤ 52.00 D or RMS > 1.50, ≤3.50), moderate (ACP > 52.00 D, ≤56.00 D, or RMS > 3.50, ≤5.75) and severe (ACP > 5600 D or RMS > 5.75) The worst of the two variables (i.e. ACP or RMS) carries the greater weight to select the appropriate grade.11 Eyes with a previous history of acute corneal hydrops, corneal surgery or any other ocular disease were excluded from the study. All subjects were older than 18 years of age. Informed consent was obtained from all subjects prior to the start of all experimental work and data collection. The study protocol followed the Tenets of the Declaration of Helsinki and was approved by the Institutional Ethical Committee Review Board of MGR Doctores ophthalmology clinic and the scientific committee of the School of Sciences at the University of Minho.
All contact lenses used in the study were standard Rose K2 lenses manufactured in tisilfocon A material (Menicon Z, Menicon Co. Ltd., Nagoya, Japan). In subjects with bilateral keratoconus, lens fitting was performed on both eyes using the same fitting approach.
Fitting method
Following manufacturer's recommendations, the first trial lens’ BOZR was selected 0.20 mm steeper than the average central keratometry and fitted on the eye. Enough time to stop reflex tearing caused by contact lens was allowed, and then sodium fluorescein was instilled for fitting assessment (Haag-Streit, Koeniz, Switzerland). Then, the lens’ BOZR was flattened (i.e. increased) or steepened (i.e. decreased) in 0.10 mm steps until the first definite apical clearance lens (FDACL) was found following the methodology previously described by the CLEK Study Group.17 Subsequently, subjects were randomly allocated to either the apical-touch or three-point-touch fitting groups, and lenses with BOZR 0.40 mm and 0.10 mm flatter than the FDACL, respectively, were fitted (Fig. 1) accordingly to a method previously described by the authors.18 Once the subjects were randomly allocated to a group (apical-touch three-point touch), the selected RGP lens was inserted on the eye. Following 30–60 min after lens insertion, the overall diameter and edge lift were assessed to ensure the lens was well centered and showed a fluorescein band of 0.5–0.7 mm in width along the lens edge. Once an acceptable trial lens fit was achieved, the lens was ordered from the manufacturer, and subjects were rescheduled for a dispensing visit. At the dispensing visit, corneal topography was performed in all subjects prior to lens insertion. Subsequently, subjects were trained in procedures for insertion, removal and cleaning/disinfection of contact lenses, and instructed to wear their contact lenses for 2–4 h a day, increasing 1–2 h for each following day until reaching at least 8 h of continuous wearing time. Subjects were scheduled for visits after 1, 7, and 14 days of contact lens wear. Subjects were required to attend the follow-up visits wearing their lenses. A new topography over the naked eye was taken following 14 days of contact lens wear. This topography was taken within 1 min after RGP lens removal.
Figure 1.
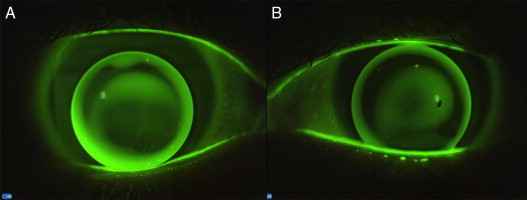
Contact lens fitting fluorescein patterns showing: (A) apical-touch fitting approach and (B) three-point-touch fitting approach.
All measurements reported are from the anterior corneal surface. Differences between baseline and 14-days of RGP lens wear in maximum and minimum simulated keratometry (Steepest SimK and Flattest SimK, respectively), average corneal power, maximum tangential curvature, central corneal astigmatism, anterior corneal surface asphericity for an 8 mm chord diameter and in the thinnest corneal thickness were compared between fitting approaches. Additionally, differences between groups following contact lens wear were also assessed in anterior corneal surface HOA coefficients (3rd to 6th order) and total HOA root mean square (RMS). The corresponding RMS error values were evaluated for the following types of optical aberrations: HOA from the 3rd- to 6th-order Zernike terms inclusive; spherical-like aberrations for the 4th and 6th order Zernike terms; coma-like aberrations for the 3rd and 5th order Zernike terms; and secondary astigmatism aberrations for the 4th and 6th order Zernike terms. Despite Pentacam is capable to measure until the 10th Zernike term, the analysis of corneal aberrations is normally undertaken until 6th term.10,19 All corneal HOA were calculated for a 6.0 mm pupil diameter.19
Statistical analysis
In subjects with bilateral keratoconus, contact lens fitting was performed on both eyes using the same fitting approach. So, the randomization of fitting approach was undertaken on subjects instead of eyes. Despite keratoconus is normally defined as a bilateral and asymmetric condition,20,21 and although many previous reports have used data from both eyes in keratoconus for statistical analysis,1,2,7–9 we followed recent recommendations of Karakosta et al.22 and Armstrong RA.23 to elucidate whether data form both eyes could be use as within-subjects factor. An Intraclass Correlation test was carried out to compare data from the most and less advanced keratoconus eyes of subjects with bilateral keratoconus. All studied parameters showed a weak correlation (all ICC r0 < 0.5). Thus, in subjects with bilateral keratoconus, data from both eyes were treated as within-subject factor.22,23 Normality test were performed for all data collected using the Shapiro–Wilk test with a level of significance of 5%. All normally distributed data were analyzed using 1-way repeated-measures analysis of variance (RM-ANOVA). Fitting approach (i.e. apical-touch vs. three-point-touch) was designated as the factor of interest and study visits (i.e. baseline vs. 14 days) as the repeated measure. Equality of variances and sphericity were tested using the Levene and Mauchly tests, respectively, to select appropriate p-values. Non-parametric variables were evaluated using Wilcoxon signed-rank test for each group separately, and Mann–Whitney U test for comparisons between groups. Non-continuous variables were assessed with the Chi-square test. Statistical analyses were performed using SPSS software (version 15.0, SPSS Inc., Chicago, IL, USA). The level of statistical significance was taken as 5%.
Results
Thirty-one subjects (50 eyes) with keratoconus were included in the study. Sixteen subjects (25 eyes) and 15 subjects (25 eyes) were fitted with an apical-touch fitting approach and with a three-point-touch fitting approach, respectively.
Grade of severity did not show statistically significant differences between groups either at baseline or over the follow-up period (all p > 0.05) (Table 1). However, the KSS range decreased in apical-touch group after contact lens wear (Table 1).
Table 1.
Severity of the groups based on the Keratoconus Severity Score.
| KSS | Baseline | Day Fortieth | ||||
|---|---|---|---|---|---|---|
| Apical-Touch | Three-point-touch | p-Valuea | Apical-touch | Three-point-touch | p-Value* | |
| Mild | 15 | 21 | 0.115 | 20 | 21 | 0.713 |
| Moderate | 8 | 4 | 5 | 4 | ||
| Severe | 2 | 0 | 0 | 0 | ||
Chi-square test. KSS: Keratoconus Severity Score range.
The flattest SimK was found to be flatter following CL wear in the apical-touch group (p = 0.030), but no significant differences were found in the three-point-touch group over time or between groups either at baseline or after 14 days of CL wear (all p > 0.05) (Table 2). The steepest SimK was found to be flatter following contact lens wear in comparison to baseline in apical-touch group (p < 0.0001), but no significant differences were found in the three-point-touch group or between groups either at baseline or after the follow-up period (all p > 0.05) (Table 2). Average corneal power was found to be significantly flatter following contact lens wear in comparison to baseline in apical-touch group (p = 0.003), but no statistically significant differences were found in three-point-touch group over time or between groups at any of the study visits (all p > 0.05) (Table 2). A statistically significant difference in maximum tangential curvature power was found between groups at baseline (p = 0.026) but not after 14 days of CL wear (p = 0.118). The maximum tangential curvature power was significant reduced with 14 days of contact lens wear in comparison to baseline in both groups (both p < 0.001) (Table 2).
Table 2.
Comparison of the flattest, steepest and average corneal power and maximum tangential keratometry.
| Measurements (D) | Apical-touch | Three-point-touch | Comparison between groups pb |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 14 days | Dif. | pa | Baseline | 14 days | Dif. | pa | Baseline | 14 days | |
| Flattest SimK | 46.61 ± 3.41 | 46.31 ± 2.86 | 0.29 | 0.030 | 45.88 ± | 45.92 ± 3.23 | −0.04 | 0.190 | 0.665 | 0.662 |
| Steepest SimK | 50.65 ± 4.24 | 49.79 ± 3.57 | 0.77 | <0.0001 | 49.43 ± 3.60 | 49.13 ± 3.28 | 0.30 | 0.010 | 0.399 | 0.607 |
| ACP | 48.53 ± 3.73 | 47.98 ± 3.11 | 0.51 | 0.003 | 47.56 ± 3.18 | 47.46 ± 3.16 | 0.10 | 0.227 | 0.372 | 0.535 |
| KTag | 56.79 ± 4.90 | 54.56 ± 4.28 | 1.8 | <0.0001 | 53.68 ± 3.81 | 52.61 ± 3.37 | 1.07 | 0.001 | 0.026 | 0.118 |
Wilcoxon signed rank test.
Mann–Whitney U test. Dif: difference; D: diopters; SimK: simulated keratometry; ACP: average corneal power; KTag: maximum tangential curvature.
Contact lens wear induced a statistically significant reduction in central corneal astigmatism in comparison to baseline in both groups (RM-ANOVA, test p < 0.0001, Table 3). However, no statistically significant differences were found between groups in central corneal astigmatism (p = 0.808) or in the time*group interaction (p = 0.176, Table 3).
Table 3.
Comparison of central corneal astigmatism and corneal asphericity for apical-touch and three-point-touch fitting approaches. (RM-ANOVA test).
| Apical-touch | Three-point-touch | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 14 days | Dif. | Baseline | 14 days | Dif. | Time | Group | Time * group | |
| CCA (D) | 3.60 ± 2.04 | 3.28 ± 1.76 | 0.32 | 3.90 ± 1.58 | 3.21 ± 1.54 | 0.69 | <0.0001 | 0.808 | 0.176 |
| Corneal asphericity | −0.87 ± 0.63 | −0.72 ± 0.46 | 0.15 | −0.70 ± 0.37 | −0.64 ± 0.35 | 0.06 | <0.0001 | 0.337 | 0.114 |
CCA: central corneal astigmatism. D: diopters. RM-ANOVA: repeated measures analysis of variance.
Corneal asphericity was found to be significantly reduced following contact lens wear (RM-ANOVA test, p < 0.0001), but no significant differences were found between groups (p = 0.337) or in the time * group interaction (p = 0.114) (Table 3).
The thickness at the thinnest point was significant thinner in the apical-touch group in comparison to the three-point-touch group at both baseline and after 14 days of CL wear (RM-ANOVA test, p = 0.010). A statistically significant increase in thickness at the thinnest corneal point was found over time (p < 0.0001), but no statistically significant differences were found for the time * group interaction (p = 0.134) (Fig. 2).
Figure 2.
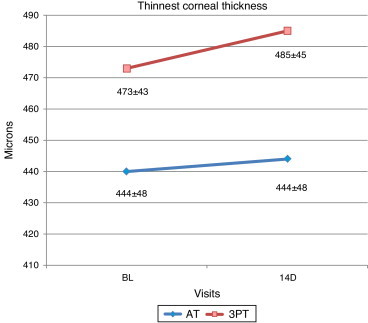
Comparison of the Thinnest Corneal Thickness between both fitting approaches. BL: Baseline; AT: apical-touch fitting approach; 3PT: three-point-touch fitting approach.
No statistically significant differences were found in spherical-like anterior corneal aberration over time in any of the groups (Wilcoxon signed rank test all p > 0.05) or between groups at any visit (Mann–Whitney U test all p > 0.05) (Fig. 3). Statistically significant reduction in secondary astigmatism aberration in apical-touch group and in coma-like aberration and in higher-order RMS in both groups was found following contact lens wear in comparison to baseline (Wilcoxon test all p < 0.05) (Fig. 3). However, no significant differences were found between groups at any visit in secondary astigmatism, coma-like or higher-order RMS anterior corneal aberrations (Mann–Whitney U test all p > 0.05) (Fig. 3).
Figure 3.
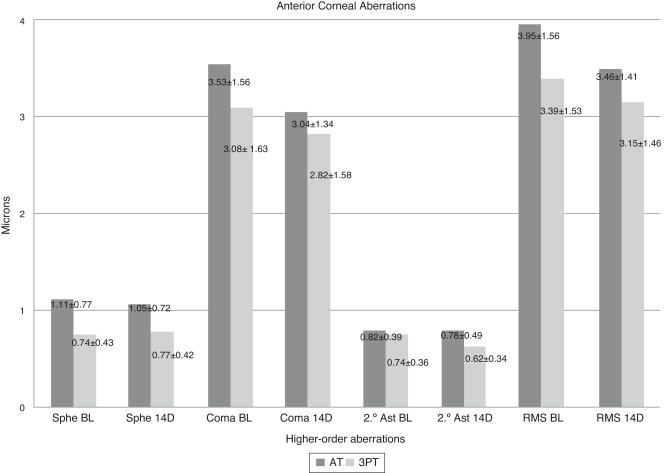
Analysis of anterior corneal surface higher-order aberrations for both fitting approaches. Sphe: spherical-like aberration; 2° Ast: secondary astigmatism; RMS: root mean square error; BL: baseline; AT: apical-touch fitting approach; 3PT: three-point-touch fitting approach.
Discussion
To the best of our knowledge, this is the first study to assess short-term corneal changes caused by apical-touch and three-point-touch RGP contact lens fittings approaches in neophyte contact lens wearers with keratoconus. As expected, this study found RGP contact lens wear to induce central corneal flattening. In the apical-touch group, significant anterior corneal surface flattening was found on average corneal power. This flattening was greater in the steepest in comparison to the flattest corneal meridian, which is in agreement with previous reports.10,24 This is favorable to a reduction in corneal toricity and can be attributed to how RGP lenses settle on eyes with keratoconus. Rigid gas-permeable contact lenses tend to move toward the direction of the steepest (and more elevated) axis leading to increased lens’ bearing and thus greater flattening on this corneal meridian. In the three-point-touch group, although these changes were not statistically significant, the steepest corneal meridian flattened and the flattest meridian steepened, which is in agreement with a previous report.24 A significant flattening in the maximum tangential curvature was also found in both groups following RGP lens wear, that was greater in the apical-touch group in comparison to the three-point-touch group. The flattening in maximum tangential curvature was found to be greater, in magnitude, than the flattening in average corneal power. This is attributed to greater lens’ bearing on the cone apex in comparison to other corneal locations. In the present study, anterior corneal surface flattening was found to be greater in apical-touch group in comparison to the three-point-touch group. This greater reduction in anterior corneal surface curvature in apical-touch group caused the improvement on the KSS staging in this group. This reduction in corneal curvature with RGP contact lens wear could be misinterpreted as an improvement on keratoconus staging, but once the subject discontinues contact lens wear, corneal curvature increases.10,26
We found that central corneal astigmatism was reduced with contact lens wear and this is attributed to the fact that the steepest meridian flattened more than the flattest meridian in both groups after contact lens wear. A greater, not statistically significant but clinically significant, reduction of corneal astigmatism was found with the three-point-touch fitting approach compared to the apical-touch fitting approach. The amount of central corneal astigmatism reduction in three-point-touch group was 0.69 D. Hwang et al. found a reduction in central corneal astigmatism of 0.70 D after two years of RGP contact lens wear in keratoconus subjects fitted with three-point-touch fitting approach.2 In the three-point-touch approach, lens’ bearing on the cone apex tends to be slight and it mainly occurs over the steepest and more elevated corneal axis, which may imply lens clearance over the flattest corneal axis. It has been reported apical-clearance fitting to cause corneal steepening,8 so the flattest axis in three-point-touch approach is likely to remain unchanged or becomes steeper.24
Corneal asphericity was also found to reduce with contact lens wear and this might be also related to the corneal flattening induced by contact lens wear. This corneal asphericity reduction with RGP contact lens wear in keratoconus was previously reported.10 A flattening of the mean central curvature reduces the difference between central and peripheral corneal curvatures thus reducing corneal asphericity.25 Clinically greater reduction in corneal asphericity was found in apical-touch group in comparison to three-point-touch group, which is presumably attributed with the greater corneal curvature flattening in the apical-touch group in comparison to the three-point-touch group.
The significant difference found between groups in thinnest corneal thickness is likely to be related to baseline differences between groups in thickness despite randomization of subjects into the two different groups. Interestingly, an increase in thickness at the thinnest point was found following contact lens wear. This finding is in agreement with Jinabhai et al. who reported a decrease in thinnest corneal thickness after discontinuation of RGP contact lens wear for 1-week in long-term contact lens wearers with keratoconus in two previous studies.10,26 More recently, Romero-Jiménez et al. found greater thickness at the thinnest corneal point in a group of keratoconus subjects who had been wearing RGP lenses for at least six months compared with a control group of non-contact lens wearers with keratoconus.27 Thinnest corneal thickness increase with RGP contact lens wearing might be the result of lens-induced corneal inflammation from mechanical effect. The latter increase in thickness was present since subjects were initially fitted with contact lenses and lasted as long as subjects wore the lenses, suggesting that contact lens wear induces a slight and chronic inflammation of the ocular surface. The increasing in thinnest corneal thickness was found to be greater in three-point-touch group in comparison to apical-touch group. This might be caused because in apical-touch group the pressure of the lens over the corneal epithelium is greater than in three-point-touch group, which lead to a greater reduction of corneal epithelium layer masking the possible local corneal inflammation caused by RGP contact lens wearing. Despite keratoconus has been classically described in the literature as a non-inflammatory disease, recent studies have shown it is accompanied by an increase of pro-inflammatory cytokines in the tears in comparison to normal subjecs,28 with the inflammatory response being even greater with contact lens wear.29 The mechanical rubbing of the RGP lens over the cornea might cause a subtle inflammatory response on the cornea leading to increased corneal thickness. However, studies should be conducted to corroborate the latter.
The reduction in anterior surface corneal aberrations found following RGP lens wear is attributed to the corneal flattening induced by lens wear. In addition, the reduction of higher-order corneal aberrations was greater in the apical-touch group, in comparison to three-point-touch group, a finding in agreement with a previous report which found that the flatter the BOZR, the greater the reduction in higher-order ocular aberrations.30
In conclusion, our study shows RGP contact lens wear to flatten the anterior cornea, to reduce corneal asphericity and corneal stigmatism, and to reduce anterior corneal surface higher-order aberrations in keratoconus subjects after a short period of wear. The greater contact lens bearing, the greater corneal flattening. Three-point-touch fitting approach causes a greater reduction in central corneal astigmatism in comparison to apical-touch. In addition, RGP contact lens wear might cause a local and slight chronic corneal inflammation whose clinical relevance should be ascertained. Changes found on anterior corneal surface with short period of RGP contact lens wear are clinically relevant in terms of corneal curvature flattening, especially in apical-touch fitting approach, because they could be misinterpreted as a keratoconus improvement. On the other hand, it is necessary to evaluate whether changes on anterior corneal surface observed after a short period of time are maintained or they evolve along the time.
Differences found between apical-touch and three-point-touch fitting approaches after a short period of RGP contact lens wear on corneal surface are not clinically relevant, except on central corneal curvature. Therefore, is not possible to state that one of the RGP contact lens fitting approach evaluated is better than the other in terms of corneal impact.
Conflict of interest and source of funding
Miguel Romero-Jiménez is undertaking a PhD partly funded by Menicon Co. Ltd. at the Clinical & Experimental Optometry Research Lab, Center of Physics, University of Minho, Braga, Portugal. Jacinto Santodomingo-Rubido is a full-time employee of Menicon Co. Ltd.
All contact lenses and maintenance solutions used in the present work were provided by Menicon Co. Ltd. without cost for the subjects.
References
- 1.Zadnik K., Barr J.T., Edrington T.B. Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study. Invest Ophthalmol Vis Sci. 1998;39:2537–2546. [PubMed] [Google Scholar]
- 2.Hwang J.S., Wiee W.R., Kim M.K. Effects of multicurve RGP contact lens use on topographic changes in keratoconus. Korean J Ophthalmol. 2010;24:201–216. doi: 10.3341/kjo.2010.24.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leung K.K. RPG fitting philosophies for keratoconus. Clin Exp Optom. 1999;82:230–235. doi: 10.1111/j.1444-0938.1999.tb06653.x. [DOI] [PubMed] [Google Scholar]
- 4.Braun D.A., Anderson Penno E.E. Effect of contact lens wear on central corneal thickness measurements. J Cataract Refract Surg. 2003;29:1319–1322. doi: 10.1016/s0886-3350(03)00230-x. [DOI] [PubMed] [Google Scholar]
- 5.Wang X., McCulley J., Bowman R. Time to resolution of contact lens induced corneal warpage prior to refractive surgery. Eye Contact Lens. 2002;28:169–171. doi: 10.1097/01.ICL.0000018042.02034.AB. [DOI] [PubMed] [Google Scholar]
- 6.Szczotka L.B., Rabinowitz Y.S., Yang H. Influence of contact lens wear on the corneal topography of keratoconus. CLAO J. 1996;22:270–273. [PubMed] [Google Scholar]
- 7.Zadnik K., Barr J.T., Steger-May K. Comparison of flat and steep rigid contact lens fitting methods in keratoconus. Optom Vis Sci. 2005;82:1014–1021. doi: 10.1097/01.opx.0000192349.11525.de. [DOI] [PubMed] [Google Scholar]
- 8.Gundel R.E., Libassi D.P., Zadnik K. Feasibility of fitting contact lenses with apical clearance in keratoconus. Optom Vis Sci. 1996;73:729–732. doi: 10.1097/00006324-199612000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Zadnik K., Mutti D.O. Contact lens fitting relation and visual acuity in keratoconus. Am J Optom Physiol Opt. 1987;64:698–702. doi: 10.1097/00006324-198709000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Jinabhai A., O’Donnell C., Radhakrishanan H. Changes in refraction, ocular aberrations, and corneal structure after suspending rigid gas-permeable contact lens wear in keratoconus. Cornea. 2012;31:500–508. doi: 10.1097/ICO.0b013e31820f777b. [DOI] [PubMed] [Google Scholar]
- 11.De Sanctis U., Loiacono C., Richiardi L., Turco D., Mutani B., Grignolo F.M. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology. 2008;115:1534–1539. doi: 10.1016/j.ophtha.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 12.Miháltz K., Kovács I., Takács A., Nagy Z.Z. Evaluation of keratometric, pachymetric, and elevation parameters of keratoconic corneas with Pentacam. Cornea. 2009;28:976–980. doi: 10.1097/ICO.0b013e31819e34de. [DOI] [PubMed] [Google Scholar]
- 13.De Sanctis U., Missolungi A., Mutani B., Richiardi L., Grignolo F.M. Reproducibility and repeatability of central corneal thickness measurement in keratoconus using the rotating Scheimpflug camera and ultrasound pachymetry. Am J Ophthalmol. 2007;144:712–718. doi: 10.1016/j.ajo.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Ucakhan O.O., Ozkan M., Kanpolat A. Corneal thickness measurements in normal and keratoconic eyes: pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J Cataract Refract Surg. 2006;32:970–977. doi: 10.1016/j.jcrs.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 15.Kawamorita T., Uozato H., Kamiya K. Repeatability, reproducibility, and agreement characteristics of rotating Scheimpflug photography and scanning-slit corneal topography for corneal power measurement. J Cataract Refract Surg. 2009;35:127–133. doi: 10.1016/j.jcrs.2008.10.019. [DOI] [PubMed] [Google Scholar]
- 16.McMahon T.T., Szczotka-Flynn L., Barr J.T. A new method for grading the severity of keratoconus: the keratoconus severity score (KSS) Cornea. 2006;25:794–799. doi: 10.1097/01.ico.0000226359.26678.d1. [DOI] [PubMed] [Google Scholar]
- 17.Edrington T.B., Barr J.T., Zadnik K. Standardized rigid contact lens fitting protocol for keratoconus. Optom Vis Sci. 1996;73:369–375. doi: 10.1097/00006324-199606000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Romero-Jiménez M., Santodomingo-Rubido J., González-Méijome J.M. An assessment of the optimal lens fit rate in keratoconus subjects using three-point-touch and apical touch fitting approaches with Rose K2 lens. Eye Contact Lens. 2013;39:269–272. doi: 10.1097/ICL.0b013e318295b4f4. [DOI] [PubMed] [Google Scholar]
- 19.Romero-Jiménez M., Santodomingo-Rubido J., Flores-Rodríguez P. Which soft contact lens power is better for piggyback fitting in keratoconus? Contact Lens Ant Eye. 2013;46:45–48. doi: 10.1016/j.clae.2012.10.070. [DOI] [PubMed] [Google Scholar]
- 20.Zadnik K., Steger-May K., Fink B.A. Between eye asymmetry in keratoconus. Cornea. 2002;21:671–679. doi: 10.1097/00003226-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Chopra I., Jain A.K. Between eye asymmetry in keratoconus in an Indian population. Clin Exp Optom. 2005;88:146–152. doi: 10.1111/j.1444-0938.2005.tb06687.x. [DOI] [PubMed] [Google Scholar]
- 22.Karakosta A., Vassilaki M., Plainis S., Elfaal N.H., Tsilimbaris M., Moschandreas J. Choice of analytic approaches for eye-specific outcomes: one eye or two. Am J Opthalmol. 2012;153:571–579. doi: 10.1016/j.ajo.2011.08.032. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong R.A. Statistical guidelines for the analysis of data obtained from one or both eyes. Ophthalmic Physiol Opt. 2013;33:7–14. doi: 10.1111/opo.12009. [DOI] [PubMed] [Google Scholar]
- 24.Lee J.L., Kim M.K. Clinical performance and fitting characteristics with a multicurve lens for keratoconus. Eye Contact Lens. 2004;30:20–24. doi: 10.1097/01.ICL.0000095230.24618.03. [DOI] [PubMed] [Google Scholar]
- 25.Lam A., Douthwaite W. Derivation of corneal flattening factor, p-value. Ophthalmic Physiol Opt. 1994;14:423–427. [PubMed] [Google Scholar]
- 26.Jinabhai A., Radhakrishanan H., O’Donnell C. Corneal changes after suspending contact lens wear in early pellucid marginal corneal degeneration and moderate keratoconus. Eye Contact Lens. 2011;37:99–105. doi: 10.1097/ICL.0b013e31820592b1. [DOI] [PubMed] [Google Scholar]
- 27.Romero-Jiménez M., Santodomingo-Rubido J., González-Méijome J.M. The thinnest, steepest, and maximum elevation corneal locations in non-contact and contact lens wearers in keratoconus. Cornea. 2013;32:332–337. doi: 10.1097/ICO.0b013e318259c98a. [DOI] [PubMed] [Google Scholar]
- 28.Lema I., Durán J.A. Inflammatory molecules in the tears of patients with keratoconus. Ophthalmology. 2005;112:654–659. doi: 10.1016/j.ophtha.2004.11.050. [DOI] [PubMed] [Google Scholar]
- 29.Lema I., Durán J.A., Ruiz C. Inflammatory response to contact lenses in patients with keratoconus compared with myopic subjects. Cornea. 2008;27:758–763. doi: 10.1097/ICO.0b013e31816a3591. [DOI] [PubMed] [Google Scholar]
- 30.Jinabhai A., Radnakrishnan H., O’Donnell C. Visual acuity and ocular aberrations with different rigid gas permeable lens fitting in keratoconus. Eye Contact Lens. 2010;36:233–237. doi: 10.1097/ICL.0b013e3181e52dd1. [DOI] [PubMed] [Google Scholar]


